Cell Bio 3 - final
1/140
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
141 Terms
Two essential physiologic functions necessary for life:
(hint: role of the lungs)
Breathing
Circulation
A person may live for several days without liver kidney or higher brain function, but without breathing and circulation you will die in about _________
5 minutes.
- Exchange of respiratory gases between the cells of an organism and its environment
External respiration
Lungs are (mostly) concerned with external respiration.
- Utilization of O2 in cellular metabolism
Internal respiration
(more w/ liver)
what are some non-respirtory func. of the lungs?
•Phonation
•Provide reservoir for blood for left ventricle
•Filters circulation (clots via DVT, and cancers can get trapped in lungs)
•Have angiotensin converting enzyme (ACE) —> RAAS system
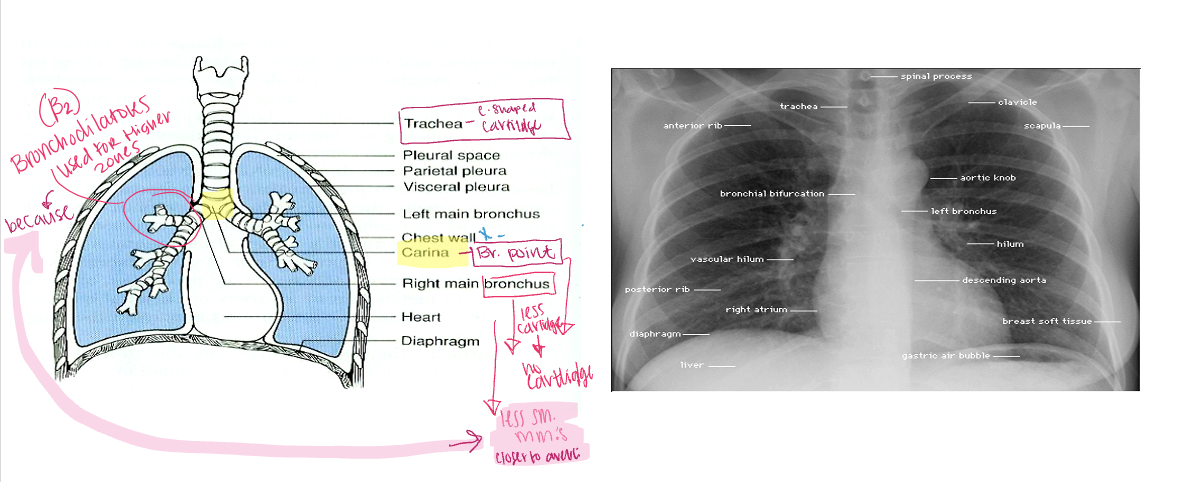
(visceral//partetal) pleura?
Adheres to the lung surface
Visceral
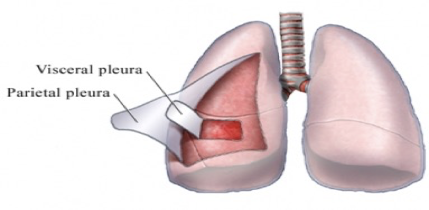
(visceral//partetal) pleura?
•Adjacent to chest wall
•Pleural space- can be filled with air (pneumothorax)
•Fluid (pleural effusion)
•Blood (hemothorax)
Parietal
(note: •Encases visceral pleura)
friction rub in the lungs
Pleurisy - inflammation of pleura
space b/t visceral//partetal pleura
pleural space — little friction
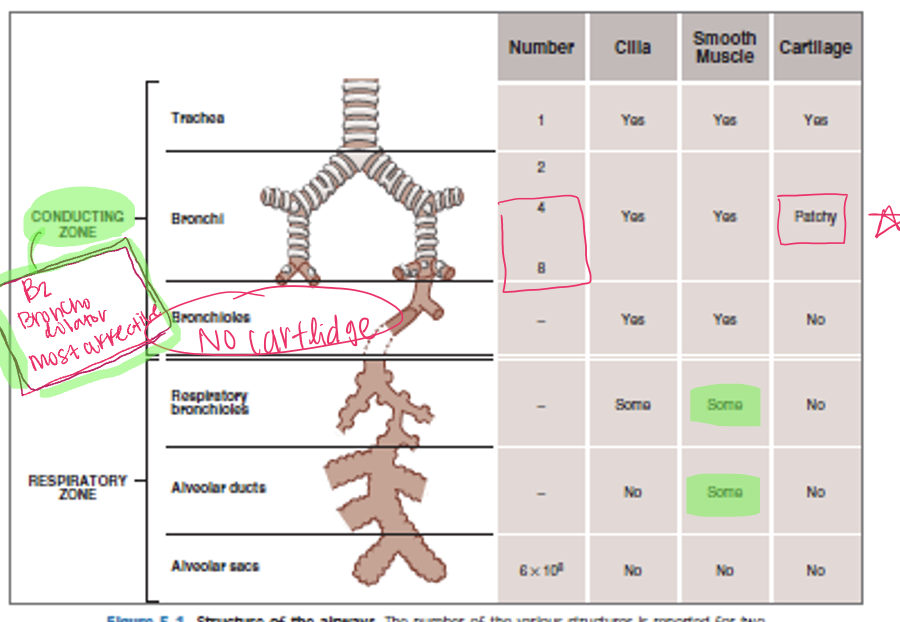
(Upper / lower )respiratory?
Columnar epithelium
Ciliated cells
Goblet cells
Conduction zone**
Warms and humidifies air
Deposition of particles
Mucociliary clearance
upper
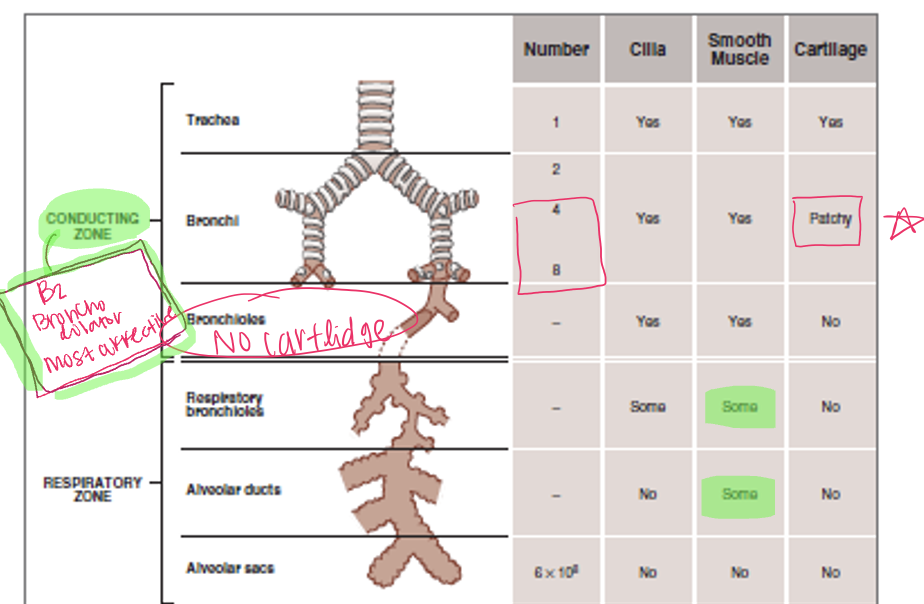
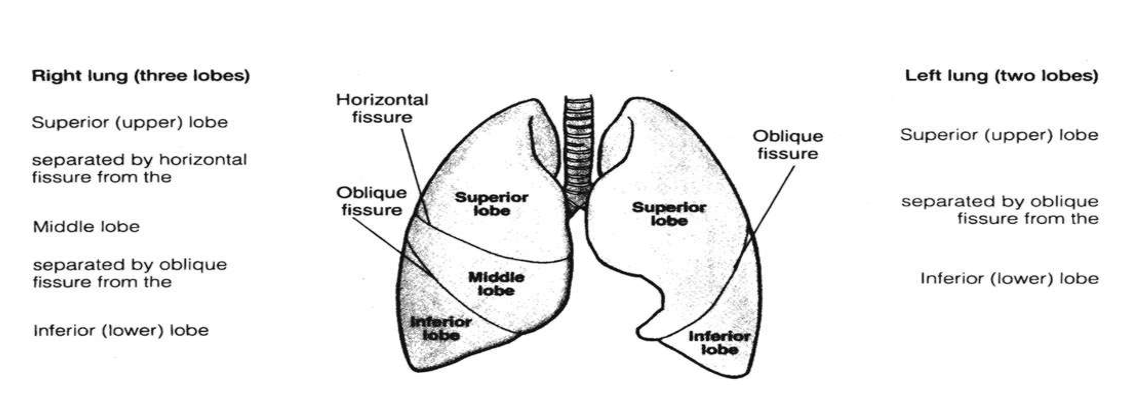
(Upper // Lower) respiratory?
Specialized respiratory epithelium
Single cells barrier between air and blood
Respiratory zone
Large surface area for gas exchange (respiratory bronchioles, alveolar ducts, alveoli)
Lower
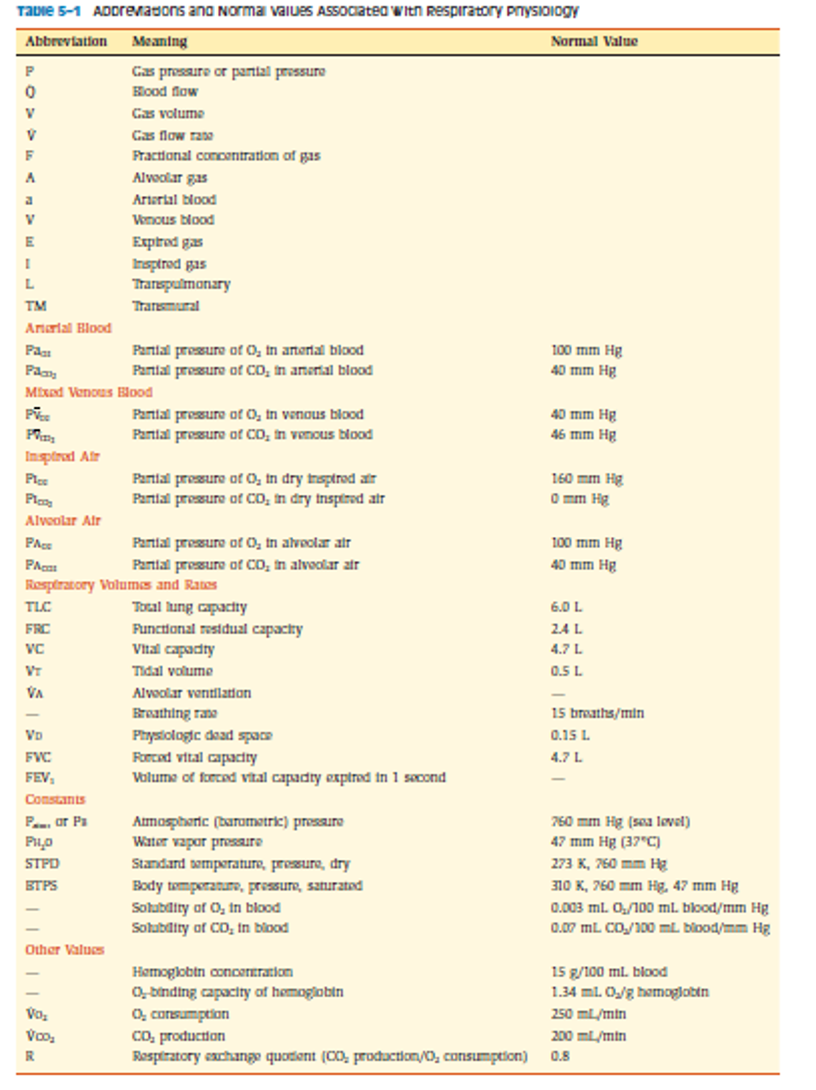
- gas pressure exerted by air (as temp increases, so does velocity of particle movement and pressure)
•Atmospheric (barometric) pressure
—
•Standard atmospheric pressure (760 mm Hg at sea level)
•At 18,000 feet (760 X 0.5 mm Hg )
•At 36,000 feet (760 X 0.25 mm Hg)
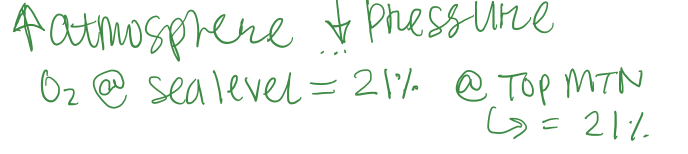
In the water, barometric pressure increases (about 1 atm per 33 ft)
the rate at which gas enters or leaves the lung (hyper/hypo ventilation).
•Ventilation (rate) -
- a state of reduced carbon dioxide in the blood.
•Hypocapnia - a state of reduced carbon dioxide in the blood.
vs.
•Hypercapnia - a condition where there is too much carbon dioxide (CO2) in the blood.
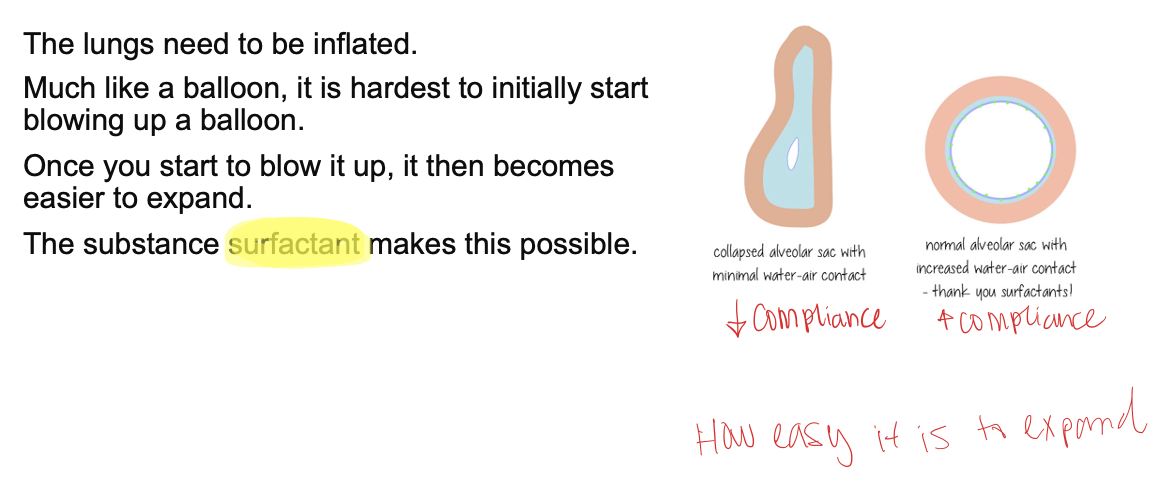
- how easily a structure can be stretched (change in volume/change in pressure).
•Compliance - (distensibility)
- retractive (recoil) force generated by distension.
•Elastance
normal, unlabored ventilation, sometimes known as quiet breathing or resting respiration. In eupnea, expiration is an entirely passive process, employing the elastic recoil of the lungs.
•Eupnea -
medical term for abnormally shallow breathing or slow respiratory rate. This differs from apnea in that there remains some flow of air.
•Hypopnea - medical term for abnormally shallow breathing or slow respiratory rate. This differs from apnea in that there remains some flow of air.
vs.
Hyperpnea is when the increased breathing is required to meet demand, as during and following exercise or when the body lacks oxygen.
may also occur as a result of sepsis, and is usually a sign of the beginning of refractory sepsis.
depth & rate
- the movement of individual molecules from a higher concentration to an area of lower concentration by random movement.
•Diffusion
- function of molecular weight (inversely related to sq. root of MW), absolute temp, and solubility.
•Diffusion coefficient (D)
difficult or labored breathing; shortness of breath
(does not necessarily mean something is wrong).
•Dyspnea -
- (oxygen saturation) (SO2) measures the percentage of hemoglobin binding sites in the bloodstream occupied by oxygen.
Now when we say “O2 sats” (—> pulse ox) we are talking about hemoglobin binding to oxygen. Normally one hemoglobin can bind four oxygen molecules but can also bind carbon monoxide. (can be tricked by CO)
•Hemoglobin saturation
– a deficiency in the concentration of oxygen in arterial blood (PaO2 is low).
•Hypoxemia
—
notes:
•Hypoxia - inadequate supply of oxygen to body tissues.
•Hypoxemia is one cause of hypoxia but not the only cause.
- the ability for a given substance, the solute, to dissolve in a solvent (higher solubility = increased rate of diffusion)
•Solubility
—
notes:
•Solubility coefficient - a constant for each gas that equates to the partial pressure
•CO2 is 24x more soluble than O2.
•Helium is fairly insoluble.
what are the Walker sign and Steinberg sign?
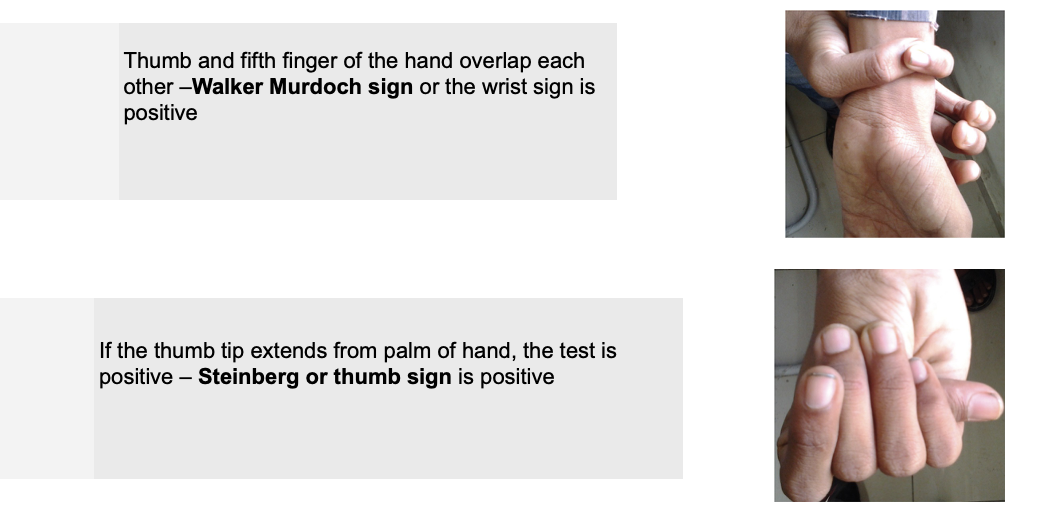
(thinking marfans)
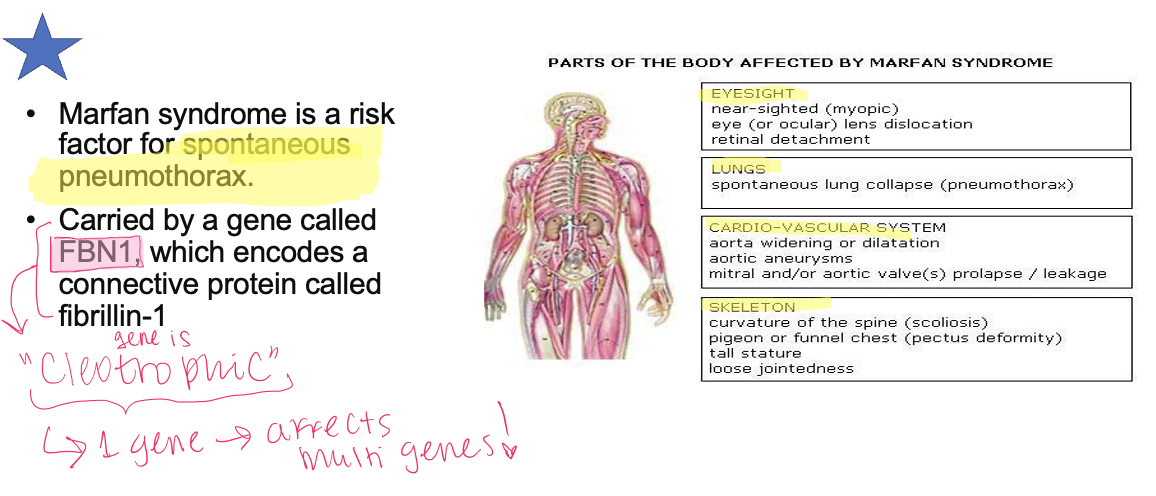
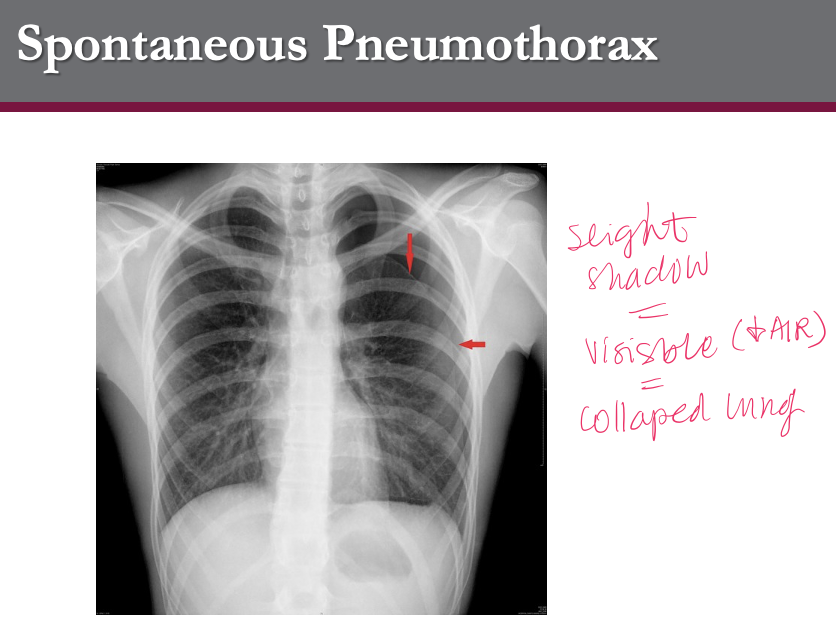
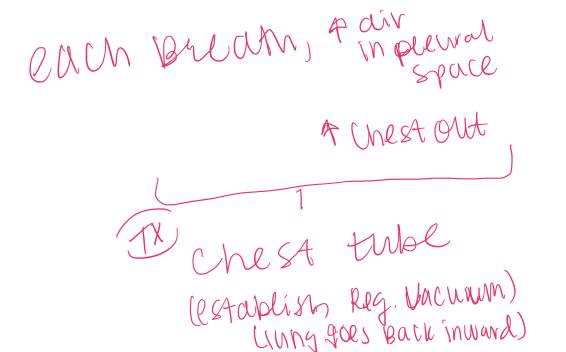
is a potential medical emergency caused by accumulation of air or gas in the pleural cavity, occurring as a result of disease or injury.
the chest wall will spring outward and the lungs will collapse inward
Pneumothorax, or collapsed lung,
Breathing begins by negative pressure allowing air to flow into the nasal passages and though the turbinates.
There are sniff receptors and irritant receptors
that cause you to stop inhaling if they sense something is toxic;
they can also cause you to cough or sneeze.
This is important because the type I pneumocytes in alveoli are very sensitive to toxins, etc.
Board e.g. A fire fighter is coughing/wheezing after battling a blaze. They may give you other clues. Now you may think that this is due to CO inhalation
but it is really due to irritation of his airways. (cough, sneeze)
Irritation, with allergens or with other toxins like smoke may induce bronchoconstriction.
1.Bronchoconstriction
—> activation of the parasympathetic nervous system!!!
Postganglionic parasympathetic fibers will release acetylcholine next to the Reissessen muscle, a smooth muscle layer surrounding the bronchi.
These smooth muscle cells have M3 type muscarinic receptors on their membrane.
The activation of these receptors by ACh will activate an intracellular Gq protein,
that in turn will activate the PLC pathway,
that will end in an increase of intracellular calcium concentrations
and therefore contraction of the smooth muscle cell.
The muscle contraction will cause the diameter of the bronchus to decrease, therefore increasing its resistance.
●
2. Bronchoconstriction is defined as the narrowing of the airways in the lungs (bronchi and bronchioles).
Air flow in air passages can get restricted due to 3 factors:
-a spasmodic state of the smooth muscles in bronchi and bronchioles
- an inflammation of the airways
- excessive production of mucous due to an allergic reaction or irritation caused by mechanical friction of air (due to shear stress), overcooling or drying of airways.
Bronchoconstriction is common in people with respiratory problems:
Such as asthma, COPD, and cystic fibrosis.
_______ coated in mucus, periciliary fluid and surfactant
•Keeps surface moist
•Traps small particles
•Decreases surface tension
•Ciliated epithelium (about 200 cilia per cell) beat at 10-20x/sec towards the pharynx.
•Respiratory passages
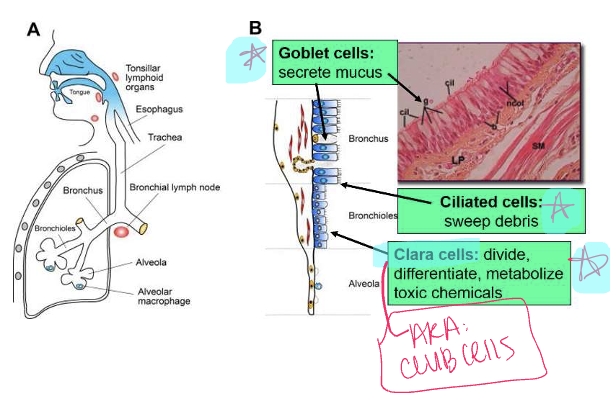
Cells in the Respiratory Zone:
•Thin, elongated
•95% of alveolar surface
•Gas exchange
•Type I Cells
•Cells in the Respiratory Zone:
Cuboidal
•2% of alveolar surface
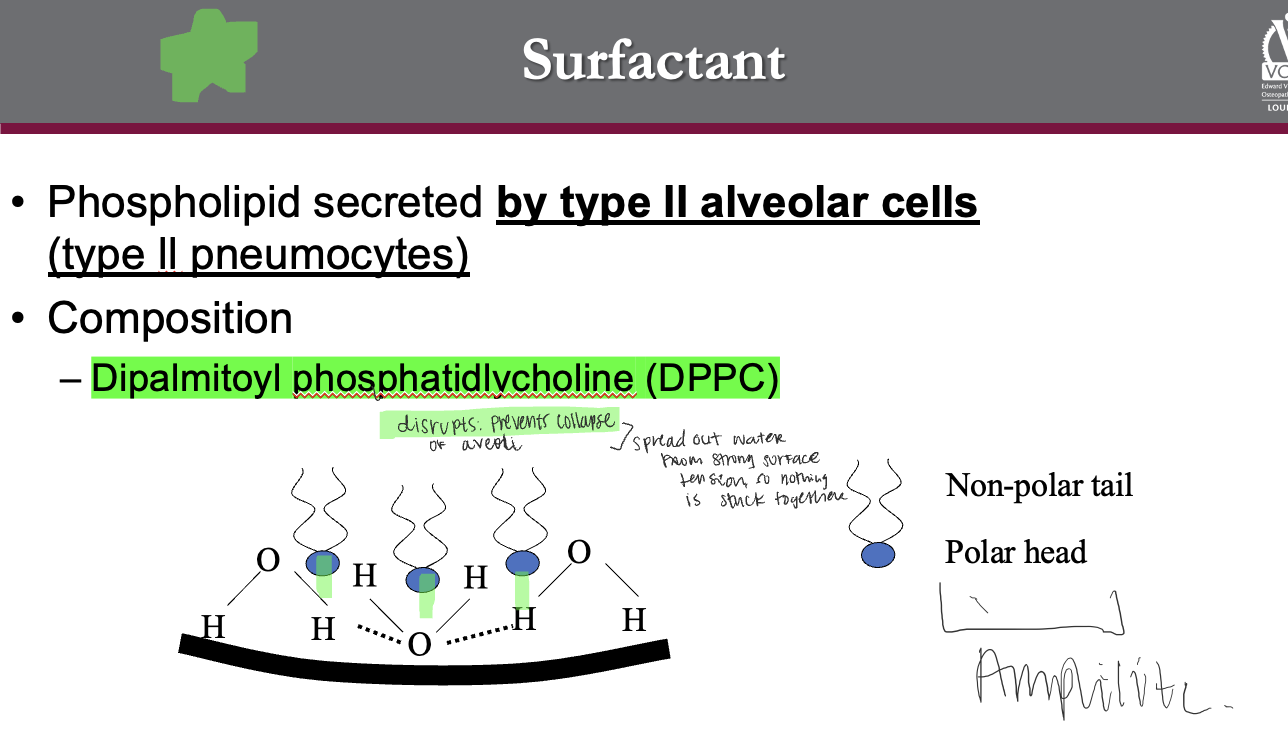
•Secretes surfactant
•Progenitor of Type I cells —> stem cells*
•Type II Cells
Cells in the Respiratory Zone:
•Throughout the airways
•Associated with nerves
•Type III (Brush) Cells
Cells in the Respiratory Zone:
•Kill bacteria
•Produce cytokines and ROS
•ROS can be toxic to Type II cells & inhibit surfactant (incr. edema)
—> can lead to lung collapse*
•Alveolar macrophages (scavengers of surface)
def. Cl transport —> def. Na transport —> affects water !!!
coughing, copious phlegm production. Problem-bacteria that normally inhabit the thick mucus grow out of control and cause pneumonia.
Staphylococcus aureus (kids)
Haemophilus influenzae,
Pseudomonas aeruginosa (adults)a
^^are the three most common organisms causing lung infections in disease*
-autosomal recessive disease.
-is most common among Caucasians and Ashkenazi Jews; .
Cystic Fibrosis
•Mutation in cystic fibrosis transmembrane conductance regulator (CFTR).
•Chloride channel defect in sweat duct causes increased Na and Chloride concentration in sweat (sweat test)
•In airway, CF patients have decreased chloride secretion and increased sodium and water reabsorption leading to dehydration of the mucus layer coating epithelial cells.
•Decreased mucociliary action
•Mucus plugging of airways

•Inspiration is [passive // active]
and regulated by?
Inspiration is ACTIVE:
Brain stem —>
respiratory centers —> Neural impulses —>
stimulate diaphragm and intercostal muscles —> lowers pressure (allows air in!)
•Expiration is [passive // active]
•and is regulated how?
Expiration is PASSIVE————— NRecoil of lungs
mechanoreceptors in the chest wall and lung
chemoreceptors located at the
bifurcation of carotid artery
ventrolateral surface of the brainstem
extra notes for understanding:
1. Peripheral Chemoreceptors
Location: Carotid bodies at the bifurcation of the carotid arteries (and also the aortic bodies).
Function: Sensitive to low oxygen (hypoxemia), high CO₂, and low pH.
Role in breathing: Send signals to the respiratory centers to increase ventilation when oxygen is low or CO₂/pH is abnormal.
2. Central Chemoreceptors
Location: On the ventrolateral surface of the medulla oblongata (part of the brainstem).
Function: Sensitive primarily to CO₂ levels (via pH changes in cerebrospinal fluid).
Role in breathing: Stimulate increased ventilation in response to elevated CO₂.
Regarding Expiration:
Expiration is typically a passive process at rest but becomes active during exertion or respiratory distress.
The respiratory centers in the brainstem (medulla and pons), including areas near the central chemoreceptors, modulate the activity of expiratory muscles.
In summary:
Bifurcation of the carotid artery → Peripheral chemoreceptors (carotid bodies)
Ventrolateral surface of the brainstem → Central chemoreceptors
these are mm’s of inspiration or expiration:
SCM
Scalenes (ant./mid/post.)
parasternal intercartilagenous mm’s
external intercostals
diaphragm — contracts & lowers*
—
inspiration
everything is expanding to incr. volume , (decr. pressure —> neg pressure)
high to low
outside air —> to inside
In inspiration the diaphram is ….
contracting and lowering.
these are mm’s of inspiration or expiration:
internal intercoastals
(except: parasternal intercartilagenous mm’s)
abdom. mm’s
rectus adom.
external or internal oblique
transverse adbom.
expiration!
NOTE: expiration = passive
(+) of these mm’s = PATHOLOGIC —> resp. distress! (bad)
—
normal exhale:
neg pressure —> pos. pressure (decr. vol)
HIGH TO LOW
inside body —> outside of body (passive)
what neuromusclar disease is this?
•Antigenic mimicry at Nodes of Ranvier
-Na channels are blocked — no ap
•Inflammation of myelin leading to conduction block and muscle paralysis
lowers activation of diaphram —> incr. SOB
(less contraction during inhale)
•Guillain-Barre syndrome
•Autoimmune response against acetylcholine receptors
•Muscle weakness can impair movement of the chest wall and result in respiratory failure even though mechanical properties are normal
tx w/ Ache inhibitors
•Myasthenia gravis
Compliance of the lung is ________ correlated with their elastic properties or elastance
Compliance of the lung is inversely correlated with their elastic properties or elastance
—
notes:
•The lungs have a springiness to them. They want to contract.
•The chest wall wants to pull out.
•Compliance is the distensibility of the system.
Lungs stay inflated due to
surfactant !
Respiratory Distress Syndrome
is a common lung disorder in premature infants.
• fact, nearly all infants born before ______ of pregnancy develop RDS.
•
RDS might be an early phase of bronchopulmonary dysplasia (BPD).
•Infants who develop BPD usually have fewer healthy air sacs and tiny blood vessels in their lungs.
Both the air sacs and the tiny blood vessels that support them are needed to breathe well.
usually develops in the first 24 hours after birth.
before: 28 weeks
_________
is characterized by inflammation and scarring in the lungs.
More specifically, the high pressures of oxygen delivery result in necrotizing bronchiolitis and alveolar septal injury, further compromising oxygenation of blood.
usually have fewer healthy air sacs and tiny blood vessels in their lungs.
Both the air sacs and the tiny blood vessels that support them are needed to breathe well.
•bronchopulmonary dysplasia (BPD).
•A leakage of protein rich fluid into alveolar lining.
•Respiratory distress syndrome of newborns, seen in premature infants.
(Cause: deficiency of pulmonary surfactant).
•Pink, fibrin-rich hyaline membranes lining small and collapsed alveolar spaces and necrotic debris mainly within the respiratory bronchioles, alveolar ducts and unopened alveoli.
•Hyaline membrane: compacted plasma exudates and cellular debris.
(sticky n stuck ☹ )
Hyaline Membrane Disease
(ARDS) —> acute resp. distress syndrome
what are the 2 biggest problems with RDS
1.Thickened membranes make gas exchange difficult
—> (develop hypoxemia and cyanosis).
2.Hyaline membranes are sticky and will increase collapse of membrane so you can’t keep them open.
-
note:
•Multiple things can also cause this - sepsis, infection, shock, hypersensitivity, drugs and others.
•Need to have positive end expiratory pressure (PEEP) to keep this open.
how do you prevent total collapes in ARDS?
•Need to have positive end expiratory pressure (PEEP) to keep this open.
there are characteristics of ???
mostly births at <28 weeks
Difficulty breathing at birth (or within an hour)
High inflating pressure required (PEEP)
Inability to hold residual air on exhalation*
Rapid, shallow respiration at onset (60-120 breaths/min)
Cyanosis, unresponsive to O2 therapy*
Due to lack of surfactant
In normal lungs at the end of exhalation, a small amount of residual gas remains in the lung sacs, —> the alveoli
Without surfactant, these alveoli fully deflate at the end of each exhalation and are difficult to reopen in order to fill with air during the next breath.
Poor aeration of lung fields is termed "atelectasis"
Respiratory Distress Syndrome (RDS) AKA Hyaline Membrane Disease (HMD)
= DECR. COMPLIANCE
=
Lecithin/sphingomyelin ratio (L/S ratio)
The ratio of lecithin to sphingomyelin concentration in the amniotic fluid
Used to predict the degree of pulmonary maturity of the fetus and thus the risk of respiratory distress syndrome (RDS) if the fetus is delivered prematurely
•A ratio of > 2:1 (L/S) is considered mature
•28-30 weeks’ gestation: _______ Lecithin and ______sphingomyelin
•30-32 weeks’ gestation:_______ Lecithin and ______sphingomyelin
•> 32 weeks’ gestation: _______ Lecithin and ______sphingomyelin
-34-40WKS — MATURE LUNGS 🙂
•28-30 weeks’ gestation: lower Lecithin and higher sphingomyelin
•30-32 weeks’ gestation: EQUAL
•> 32 weeks’ gestation: higher (increasing w/ ea. wk) Lecithin and decresing (lower)sphingomyelin
-34-40WKS — MATURE LUNGS 🙂
•Cortisol induces s
Surfactant production.
(can give sortisol to expecting mothers who will have premature labor)
•Infants of a ______ mother may develop RDS
(despite a mature L/S ratio due to deficient or delayed surfactant production)
• & why?
diabetic mother
•Fetal hyperinsulinism may adversely affect lung maturation by decreasing the action of cortisol.
•
•In a child with RDS, the infant will have:
increased recoil: (lungs have tendency to get smaller),
decreased compliance (harder to open),
collapse of lung (atelectasis), and pulmonary edema.
Chronic fetal stress can have what affect on surfactant production?
accelerates surfactant production allowing for a mature L/S ratio in premature infants.
what is being described(?)
In the lungs, hysteresis describes the difference between the inflation and deflation curves (inhale vs exhale) of the lung when plotting volume versus pressure (a pressure-volume loop). That is:
At the same pressure, the lung volume during inspiration is less than during expiration.
This creates a looped curve rather than a single line.
due to air/liquid interface (surface tension) in aveoli —> takes longer to deflate and wont fully deflate (collapse)
this alters the pressure/volume curve
•Surfactant lets the alveoli stay open just a second longer to allow gas exchange (diffusion from pressure changes) and changes the work done during the breathing cycle.
Pulmonary Hysteresis:
(^critical role in gas exhange!)
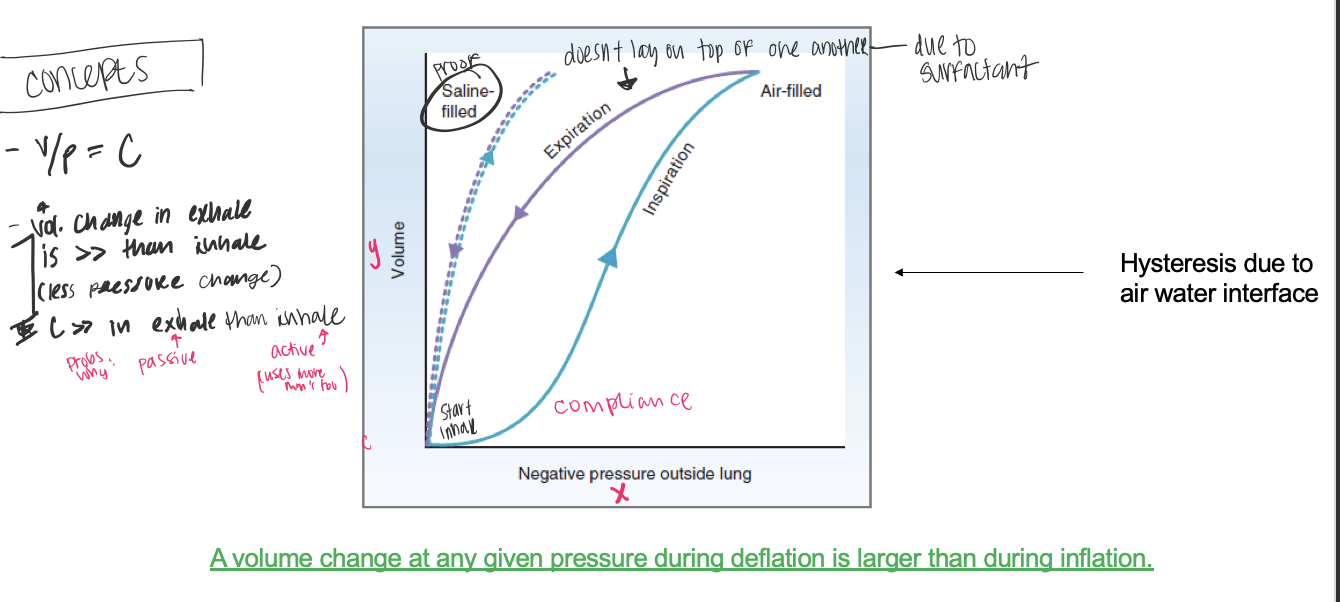
name the 3 main 🔹 Causes of Pulmonary Hysteresis: 🔹
Surfactant behavior:
Pulmonary surfactant reduces surface tension more effectively during deflation (expiration), making the alveoli stay open longer and allowing greater volume for a given pressure.Recruitment/derecruitment of alveoli:
Some alveoli only open (recruit) at higher pressures during inspiration and remain open during expiration until very low pressures.Tissue elasticity:
Elastic components (like collagen and elastin) show viscoelastic properties, contributing to the difference in inflation and deflation dynamics.
Pressure Volume Curves and Hysteresis
A volume change at any given pressure during deflation (exhale) is (larger/smaller) than during inflation (inhale)
larger!
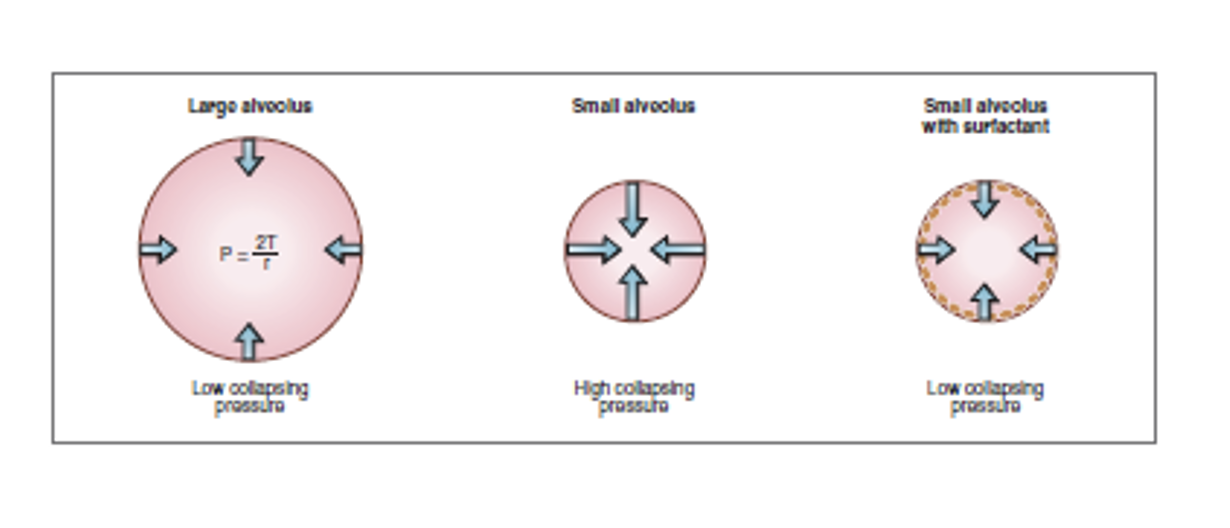
Normally alveoli would collapse due to attraction of water molecules at an air-water interface.
but it does not do this due to….
KNOW THIS FOREVER 🙂
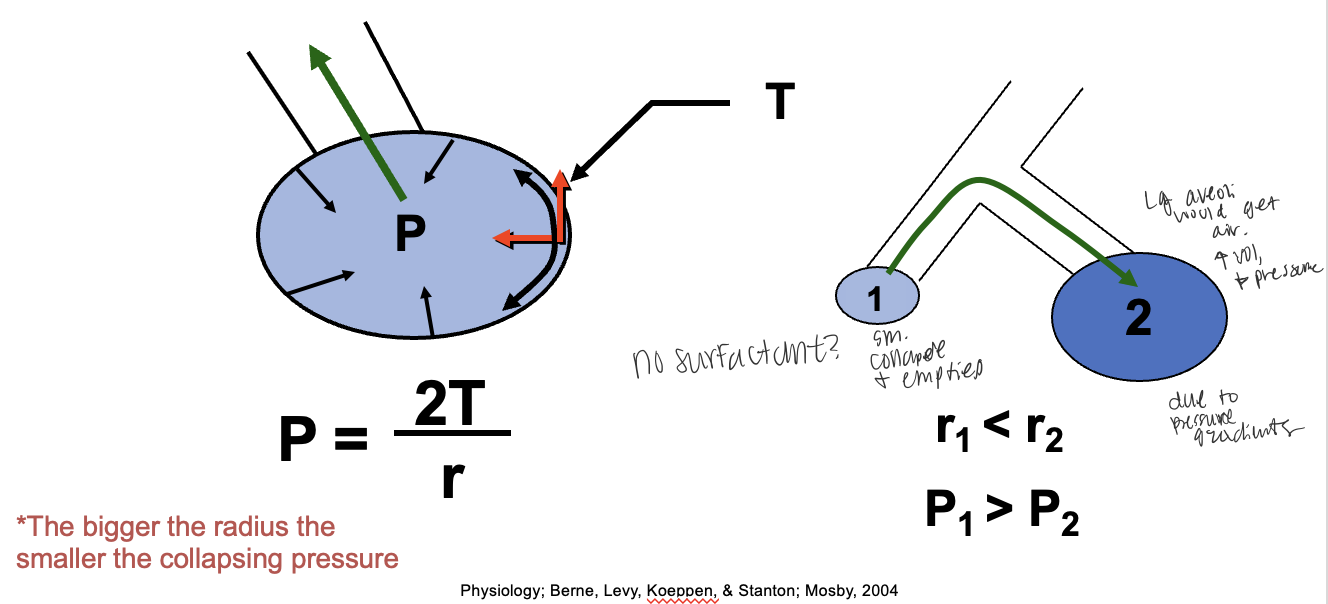
Collapsing Pressure is Greatest in [Small/medium/large] Alveoli
small alveoli
notes:
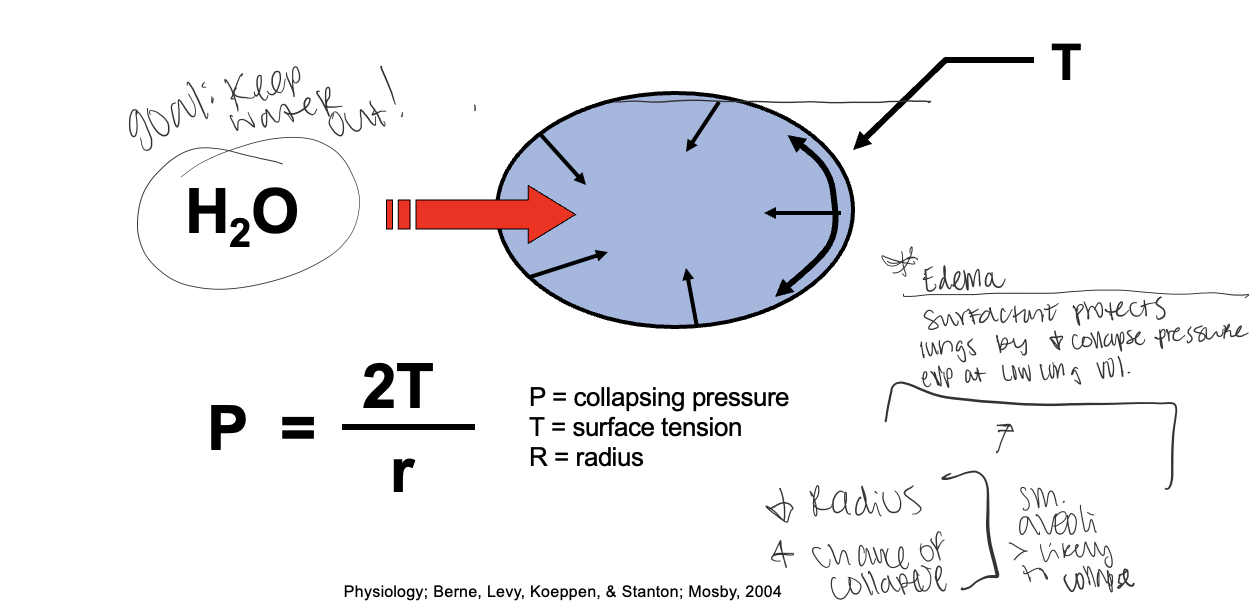
Surface tension is also a concern in alveolar edema.
The attractive force of the water molecules at an air-liquid interface exerts an inward force on the alveolar surface that tends to close the alveoli.
This same inward force acts to pull water into the alveoli from the alveolar capillaries and interstitial space —→ inducing alveolar edema.
Pressure developed by surface tension is inversely proportional to the radius of the alveoli,
therefore the tendency for water to move into the alveoli is greatest in small alveoli.
Surfactant protects against edema formation in alveoli,
particularly at low lung volumes by decreasing collapsing pressure.
In infant respiratory distress syndrome, the lack of surfactant leads to alveolar edema.
describe the law of Laplace when talking about surfactant in the lungs:
The bigger the radius the ……..
The bigger the radius the —→ smaller the collapsing pressure
extra notes:
Collapsing pressure - (Law of LaPlace)-
The pressure that develops is related to the radius of curvature of the bubble surface.
Thus, the larger (radius) the bubble, the lower the internal pressure due to surface tension.
. The pressure is directly related to the surface tension divided by the radius of the bubble.
(For a sphere with only one surface, such as an air bubble in water, the equation is P=2T/r)
. In the absence of surfactant, the smaller alveoli would exhibit a higher pressure due to surface tension than the larger alveoli, and the pressure gradients would result in the smaller alveoli emptying into larger alveoli.
Now- why are some alveoli smaller and some are larger?
—> has to deal with gravity and the other alveoli.
In infant respiratory distress syndrome, the lack of surfactant leads to alveolar edema.
NAME THE FIVE MAIN FUNC’S OF SURFACTANT
Reduces surface tension
Facilitates opening of alveoli
Increases lung compliance
Prevents atelectasis (collapse of alveoli at low lung volumes)
Reduces capillary filtration forces (alveolar edema) Remember Pc and πc (keeps alveoli from letting water in)
^STARLING FORCES
explain the role of type II pneumocytess and lamellar bodies
Type II cells found in alveoli —> produces surfactant. & makes type I cells!
Type II cells contain multiple mitochondria, which is indicative of the amount of metabolic activity in this cell type, and vesicles with concentric layers.
the vesicles =The lamellar body = preformed surfactant,
which is released onto the alveolar surface following stimulation of the Type II cells
by stretch of the alveolar wall, or various neurohumoral mediators, including b-adrenergic agonists.
When released, the contents of the lamellar bodies form tubular myelin,
which is acted upon by the surfactant Apoproteins to spread across the alveolar surface to form the surfactant layer.
LESS SURFACTANT, MORE EDEMA, HIGHER COLLAPSE RISK
•Hyaline membrane disease (aka ARDS) - leakage of protein rich fluid into alveoli
•Decreases gas exchange and increases surface tension, collapsing forces
The lungs try to minimize the work needed to extract oxygen from the atmosphere to provide it to tissue.
big concepts:
First, the harder the lungs/chest wall have to work to ventilate, the more work is done. -
If we have fibrosis or really floppy lungs, more work is needed for them to perform correctly.
Second, if you have areas that have a lot of oxygen tension but don’t have good pressure difference, then the oxygen in the lungs doesn’t make it to the tissue.
— It is wasted.
Also, if you have an area of the lungs that gets really good blood flow, but the oxygen levels are low, then the blood traveling to that area of the lungs is also wasted.
—> So, the lungs try to optimize the most air flow with the most perfusion.
GOAL: MAX O2 IN, MAX CO2 OUT w/ little as poss. work
Lungs and chest wall will work together to allow max exchange
—
what are some things that would affect exchange?
•Dead space (too much dead space not good)
•Compliance/elastance (lungs too floppy or stiff) - affect work/gas exchange
•Decreased area of diffusion (Fick’s law)
•Fluid in the lungs (pneumonia)
•Perfusion problems (blood clot)
•Not enough difference in pressure/volume
{Restrictive / obstructive} lungs
lungs do NOT want to open, inhibits air in*
fibrosis, (Too Stiff – Can’t Stretch)
—
Occupational and environmental exposures
Sarcoidosis*
Drugs
Radiation
Connective tissue or collagen diseases such as rheumatoid arthritis and systemic sclerosis*
Genetic/familial
Restrictive !!
{Restrictive / obstructive} lungs
Emphysema (Too Floppy – Can’t Contract) — inhibits air leaving!
•Cigarette smoking (centrilobular)
Alpha-1 Antitrypsin deficiency (panacinar)
breaksdown elastin —> decr. surface area in lungd
- Air pollution
obstructive
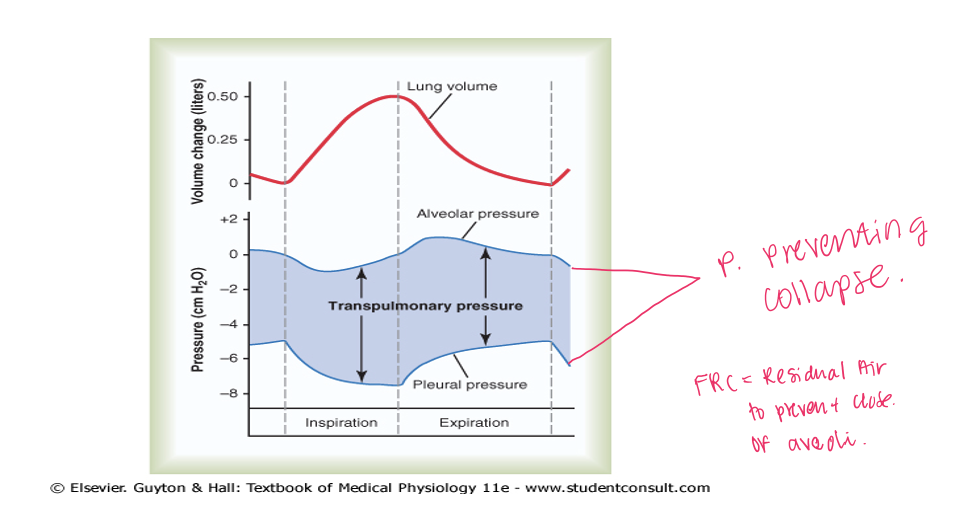
Opposing Recoil of Lung and Chest Wall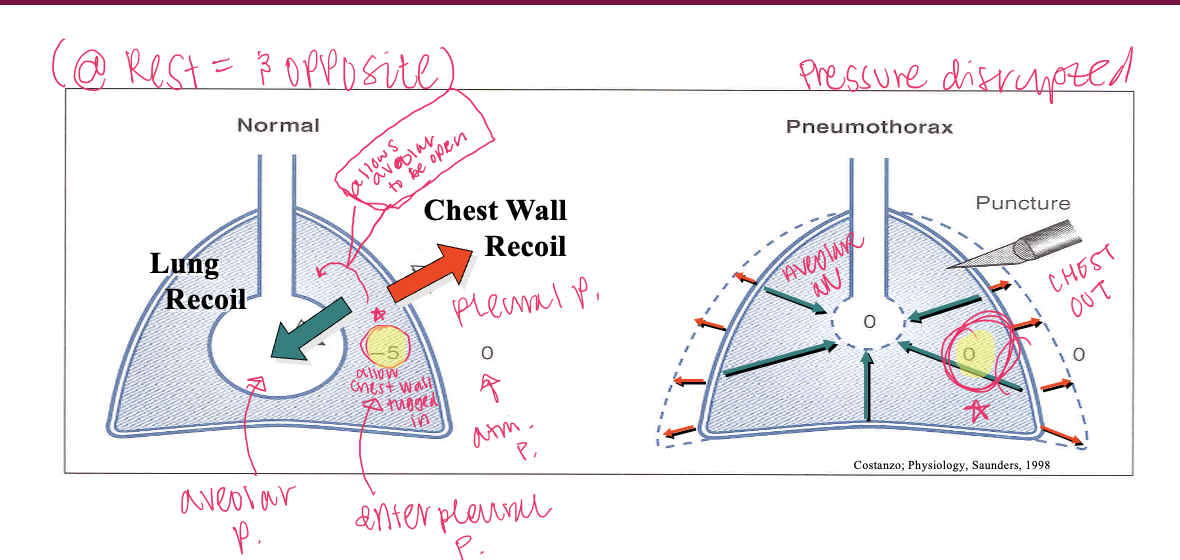
Lung tissue contains collagen, elastin, and smooth muscle fibers that cause it to recoil inward, whereas the chest wall has a tendency to spring outward
(I.e., the recoil force of the chest wall at rest is outward).
The combination of these two forces acting on the closed intrapleural space generates a negative pleural pressure of approximately –3 to -8 mm Hg.
At FRC, the outward directed force of the chest wall is balanced by the inward directed recoil force of the lung tissue.
- -
If the chest wall is breached, as in the case of a pneumothorax, the intrapleural space is open to the atmosphere.
The chest wall no longer opposes the lung recoil, and the lung collapses.
Another way to think of this is that pleural space represents a vacuum that functionally connects the lung and chest wall.
With a pneumothorax, the vacuum no longer exists, so the lung deflate and the chest wall recoils outward.
Under these conditions, activation of inspiratory muscles pulls air into the pleural space instead of the airways.
Pressures on the Lung/Chest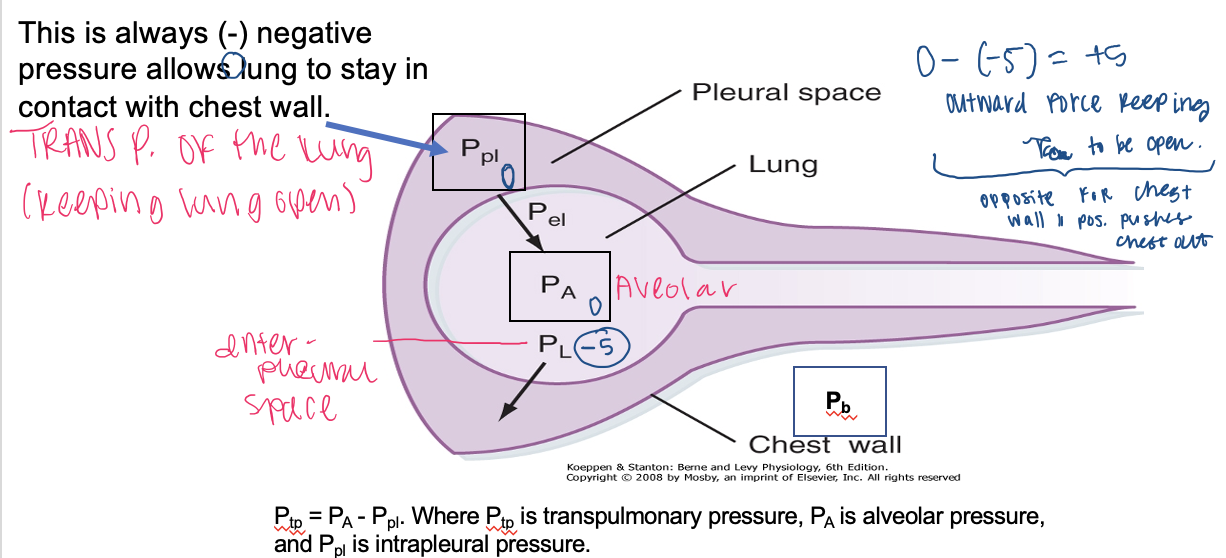
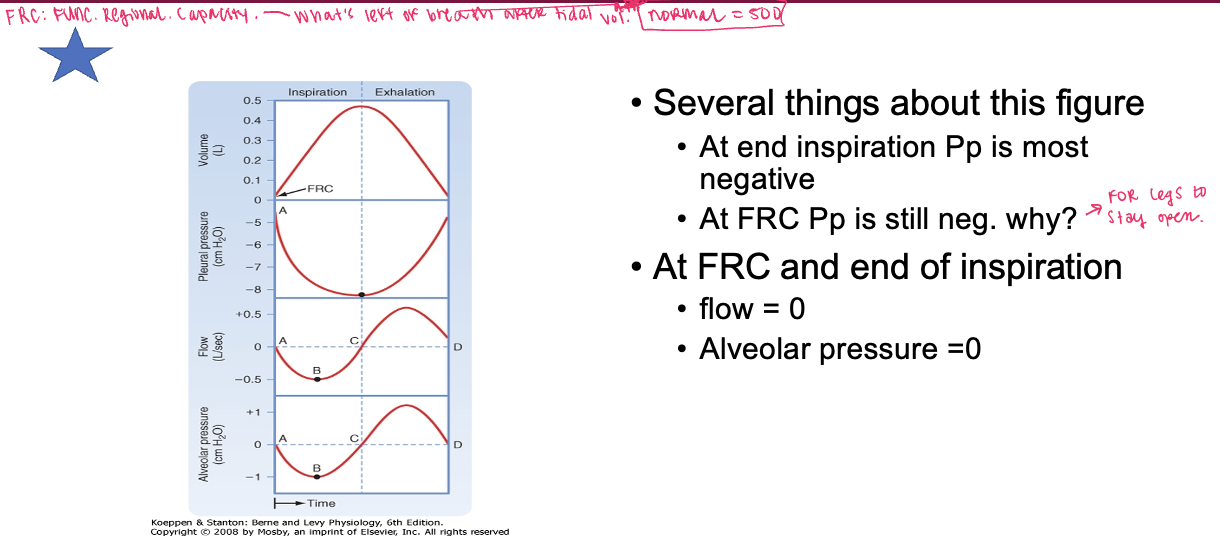
Inspiration is to the left of the vertical dotted line
exhalation is to the right.
Positive (relative to atmosphere) pressures are above the horizontal dotted line and negative pressure are below.
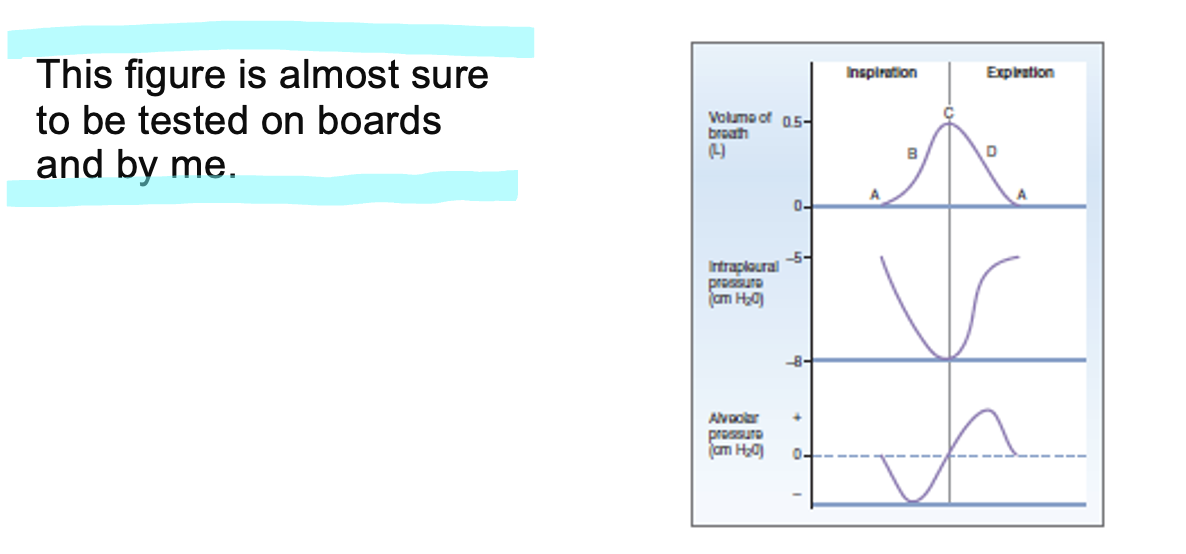
Volume & pressure changes
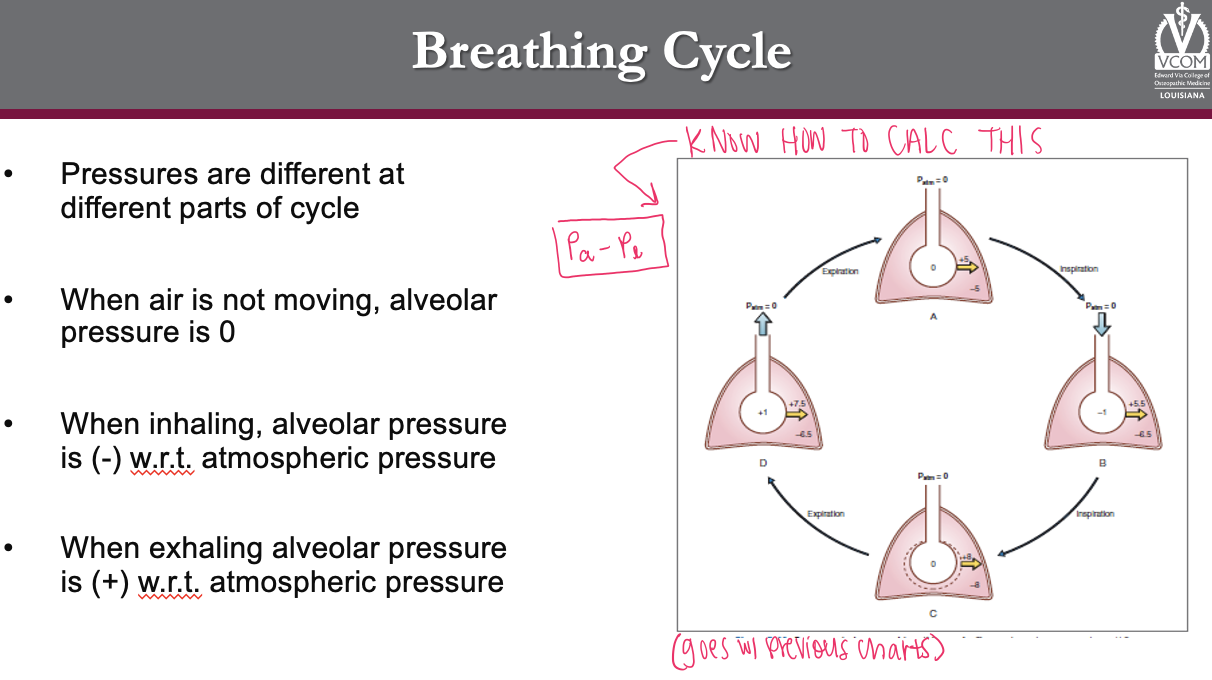
Wrt = with respect to
. Things to remember-
PA is alveolar pressure- this is relative to atmospheric pressure.
Pleural pressure (Ppl)) is normally negative
-why? Because it is the difference between the lungs wanting to contract and the chest wall wanting to spring out.
So, we have an equation Ptp (or transpulmonary pressure) will be negative cause
Ptp= (alveolar pressure –pleural pressure.)
Gas moves in and out of the lungs along pressure gradients.
When we describe pressure changes, they are relative to ambient atmospheric pressure (Patm).
A pressure of 1 cm H2O is equal to 0.74 mmHg (or 1 mmHg=1.36 cm H20)
At sea level atmospheric pressure Patm is equal to 760 mm Hg.
In the middle of an inspiration the pressure in the alveoli becomes -2 cm Hg.
This means 2 cm below atmospheric pressure (i.e. 760-2(0.74) mmHg.
Alveolar pressure is the sum of pleural pressure and elastic recoil pressure.
-
Transpulmonary pressure is the difference between pleural pressure and alveolar pressure.
Alveolar pressure (PA) pressure within the alveoli of the lungs
(it rises and falls but eventually becomes equal to atmospheric pressure)
Pressure in the intrapleural space (Ppl) pressure in the fluid in the space between lung and chest wall.
This pressure also fluctuates with breathing (however it is normally 5 to 6 cm H2O below pressure in alveoli.
It is negative to both atmospheric and alveolar pressure.
Barometric pressure (Pb)
Elastic recoil (Pel)
Transmural lung pressure (PL, pressure across the lung wall)
is the difference between alveolar pressure (PA) and pressure in the pleural space (Ppl).
PL=PA-Ppl
(this is the distending pressure that keeps the lungs from collapsing.
An increase in this pressure is responsible for inflating the lungs during inspiration.
Transmural chest wall pressure
(PW, pressure across the chest wall) is the difference in pressure between the pleural space (Ppl) and the atmosphere(Pb).
PW=Ppl-Pb
The Respiratory Cycle
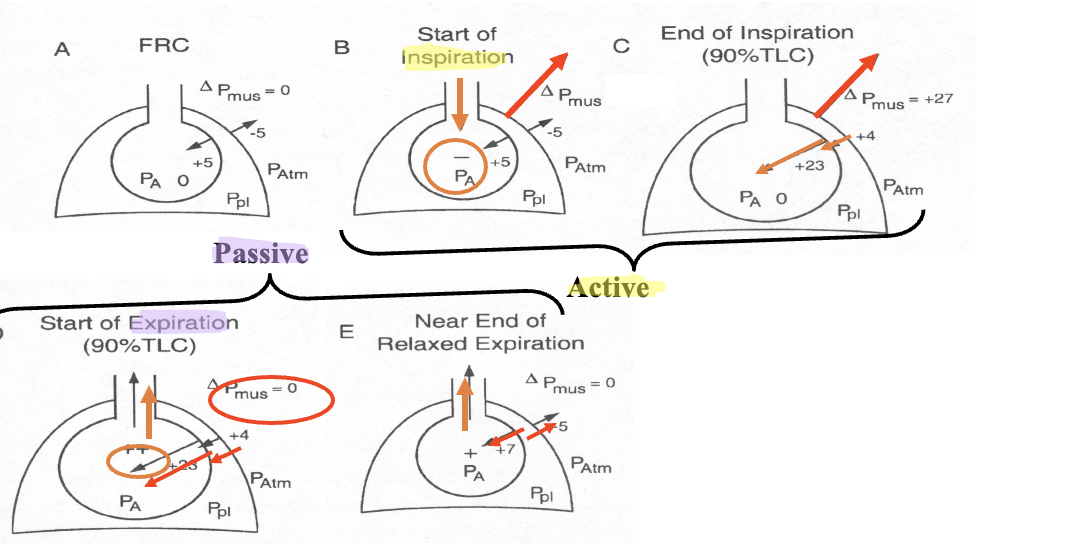
In normal resting breathing, inspiration is the active phase.
A.At FRC, the inward elastic recoil of the lung balances the outward recoil of the chest wall.
B.Inspiration is initiated when the diaphragm and accessory muscle of the chest wall contract. The diaphragm, pulls down, and the rib cage is pulled up and out. The force of the muscle contraction in this figure is expressed as the amount of pressure that force can develop (27 cm H2O of outward pressure). Since the total outward directed force (DPmus + PW) is greater than the inward recoil force (PL), the lungs inflate are pulled open. The increased pleural pressure acts on the surface of the lung, and the resulting force is transmitted through the lung tissue to the alveolar walls. The alveoli are thereby pulled open. A negative pressure is generated in the alveoli, and air is pulled in.
C.As the lungs expand, the inward directed lung recoil increases due to stretching of the lung tissue. In addition, the chest wall recoil is reduced, and eventually reverses. When the sum of the lung recoil and chest wall recoil equals the outward pressure generated by the muscle, inspiration stops.
D.When the inspiratory muscles relax, the combined inward recoil of the chest wall and lung tissue moves the chest wall inward. The alveoli are compressed, and a positive alveolar pressure is generated, which drives air out of the lungs.
E.During expiration, the inward recoil of the lung tissue is greater than the outward recoil of the chest wall, and so the chest wall is pulled inward. As the chest wall is compressed, an outward recoil force develops that opposes the inward recoil of the lung.
F.When the inward recoil of the lung and outward recoil of the chest wall are balanced, expiration stops.
●
Note the convention: A force that acts to increase alveolar pressure results in a positive pressure.
(Elastic recoil of the lung is a positive pressure)
A force that acts to decrease alveolar pressure results in negative pressure.
(Contraction of inspiratory muscles is a negative pressure)
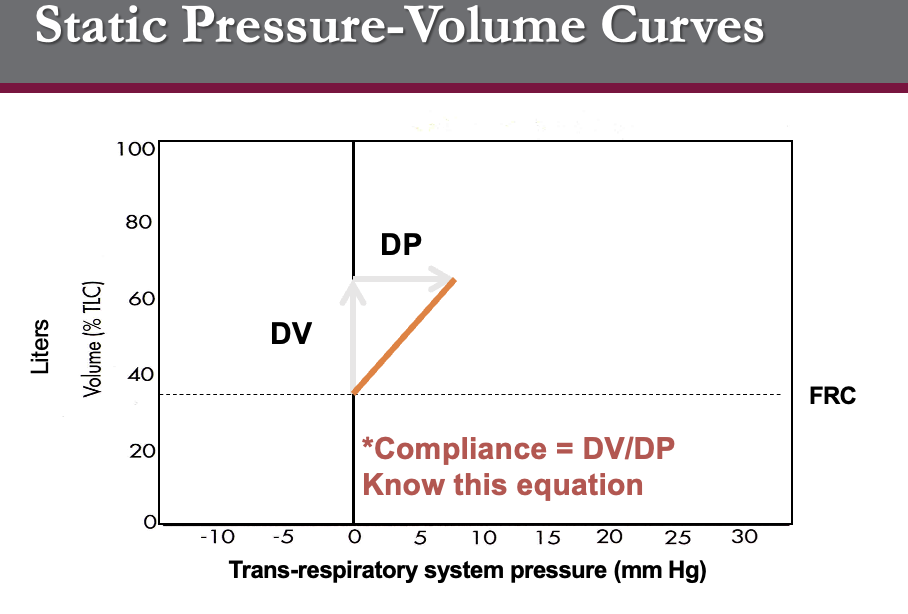
Compliance = change in volume /change in pressure
Compliance = DV/DP
Compliance represents the slope of the curve.
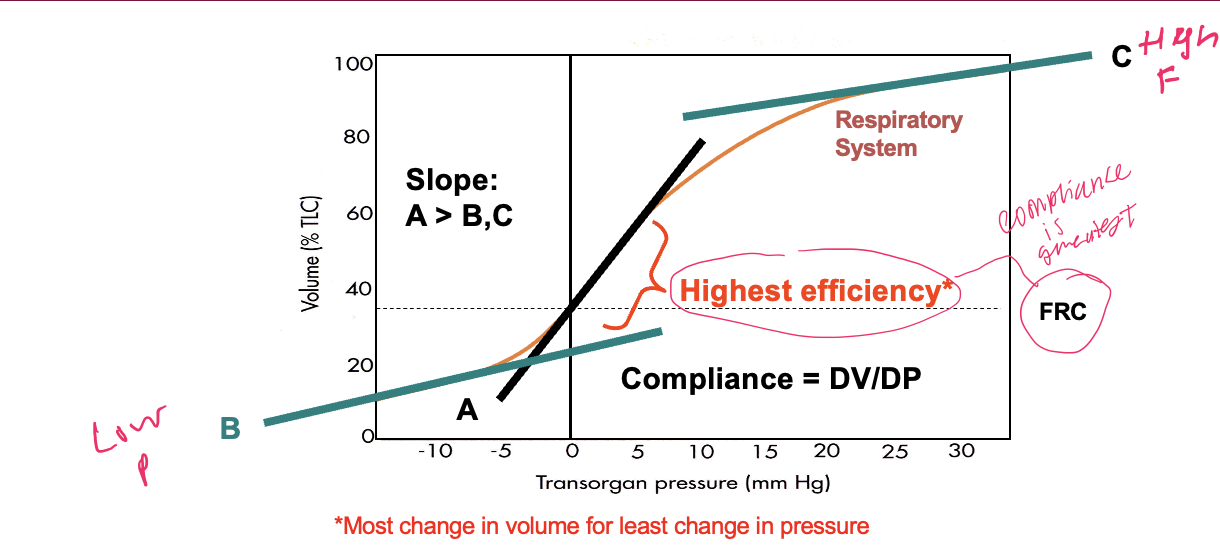
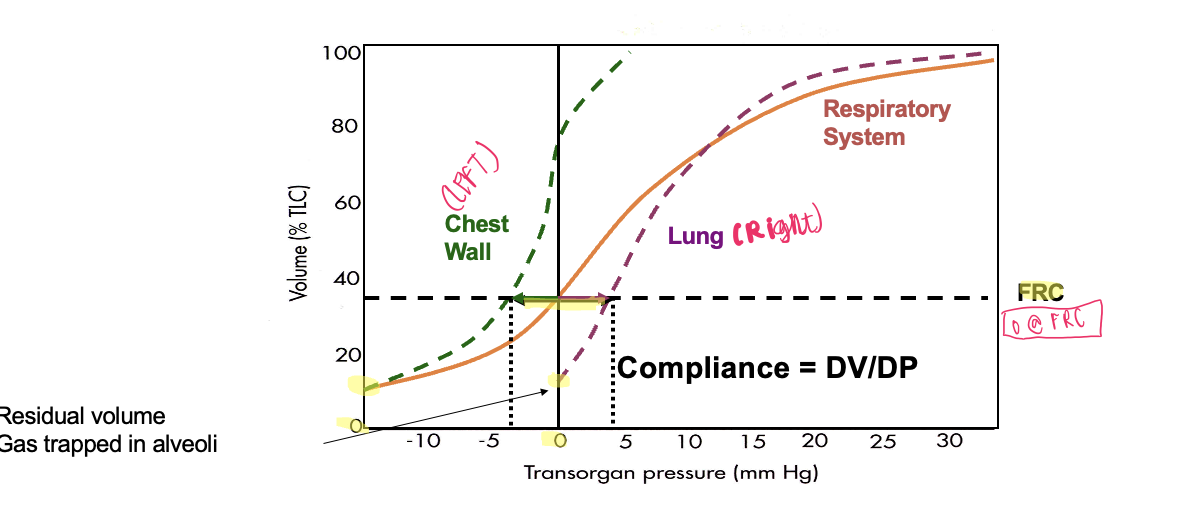
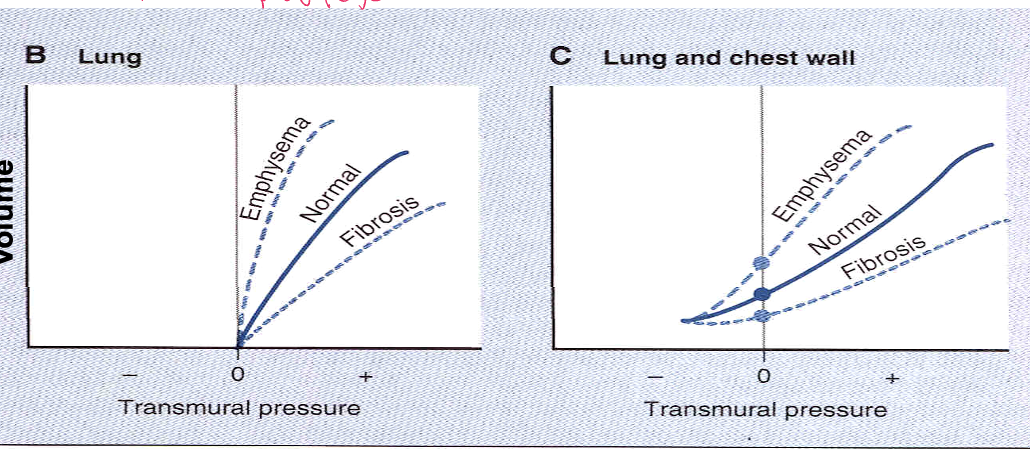
Disease states influence the compliance/elastance of the lungs, which is reflected in the shape of the pressure volume curves.
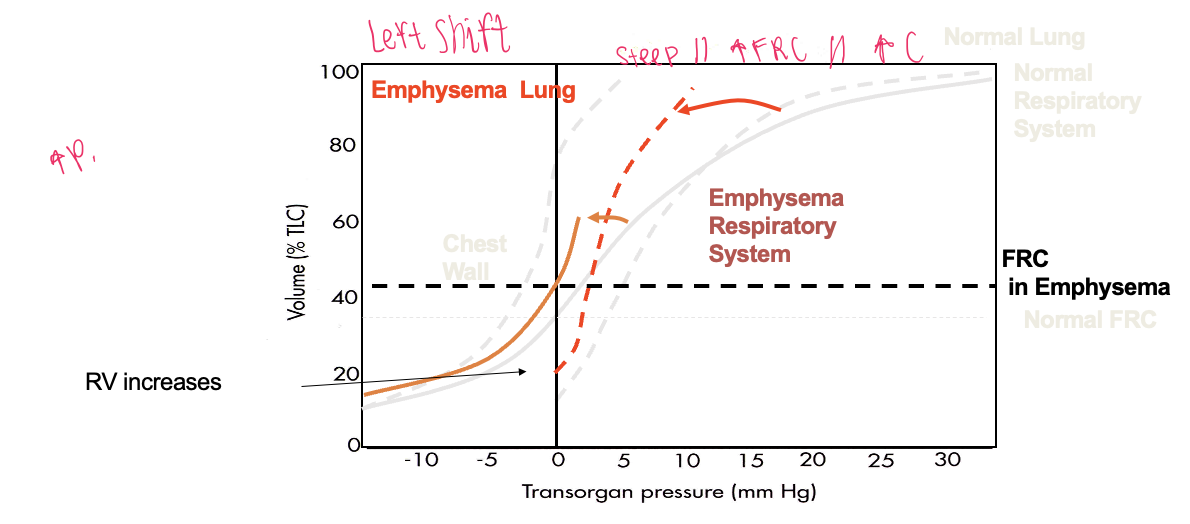
In emphysema,
lung tissue is destroyed by proteases,
—> increases the compliance and reduces the elastance of the lungs.
This causes the lungs to inflate easily, but the recoil force that normally drives exhalation is reduced.
In these subjects, the outward chest wall recoil is acting upon a smaller inwardly directed lung recoil, and the subjects exhibit an increased FRC.
Inspiratory capacity is therefore reduced.
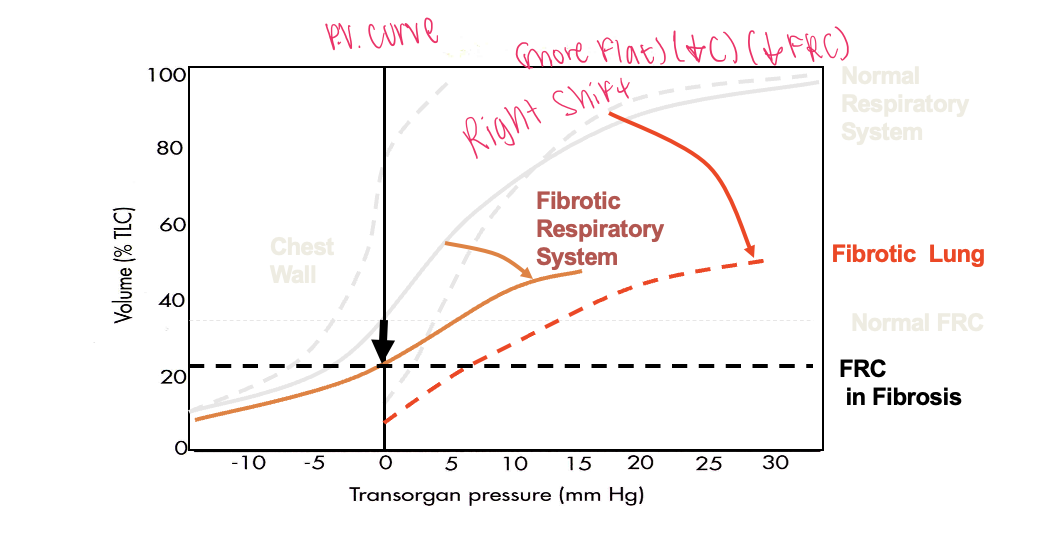
Fibrosis,
or deposition of elastin and collagen in the lungs,
increases the stiffness of the lungs (i.e., reduces compliance and increases elastance).
The inward recoil of the lungs is increased relative to the chest wall outward recoil;
FRC is reduced;
and additional force is required to expand the lungs.
OXYGEN FACTS:
Why does O2 need Hb?
oxygen has limited solubility in liquid so it needs Hb).
========
•Red blood cells are packed with the protein hemoglobin (Hb).
Oxygen binding to hemoglobin is needed to transport oxygen to tissues
-
•Hemoglobin variations (thalassemia) or hematocrit (% RBC) - too high or too low is problematic.
•Oxygen moves in and out of cells/body by diffusion (down a concentration/pressure gradient).
•Barometric pressure is important in climbing a mountain and trying to breathe.
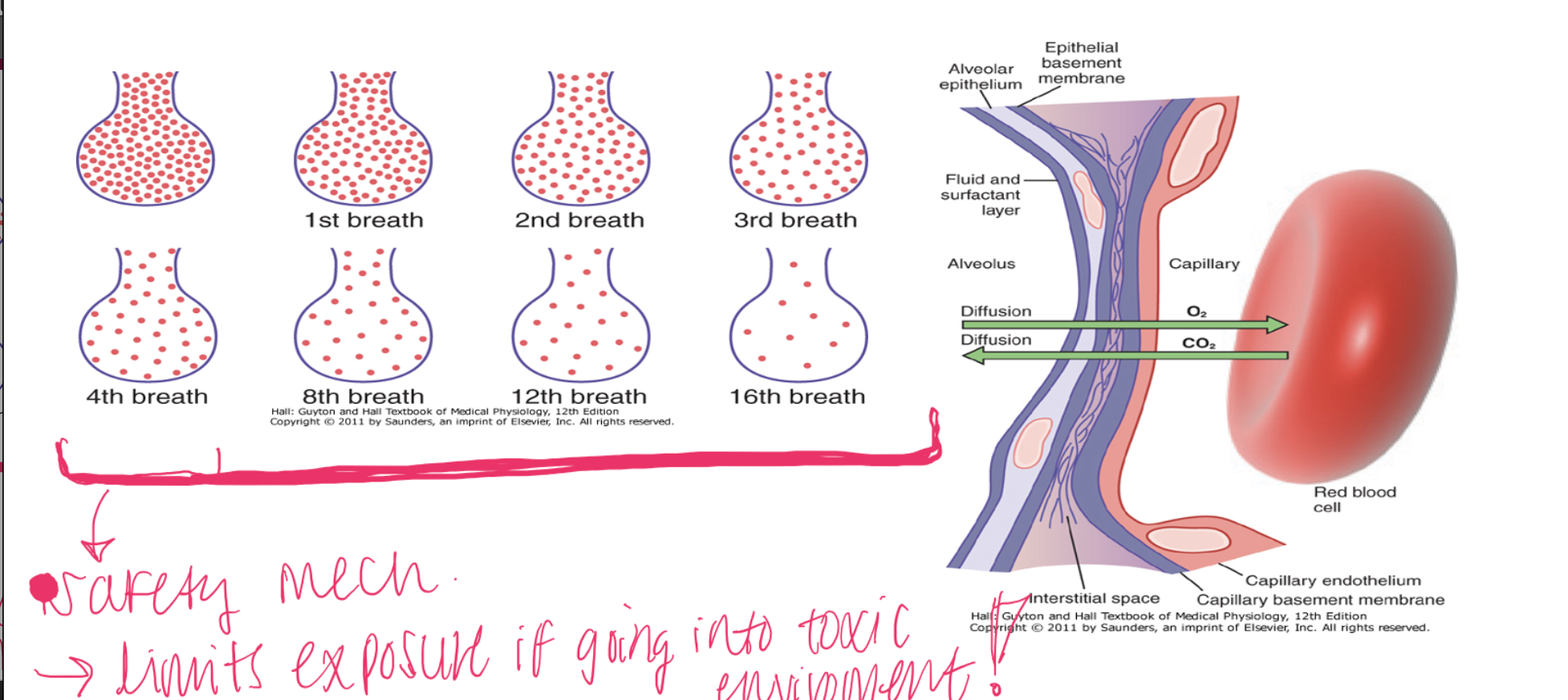
explain this
we only breathe in/out about 1/7th of our aveoli —> protects us from toxins in the air
and
it takes about 16th breaths
{Hemoglobin // Myoglobin]
•Oxygen transport protein in the RBCs.
•Blood chemistry affects hemoglobin oxygen binding properties.
•Oxygen is not very soluble, so we bind it to hemoglobin to transport it through the bloodstream.
Has 4 chains, each chain can bind one O2 (so each Hb can bind 4 O2
Hemoglobin
know terms:
Other forms
A – Normal (α2β2)
F – Fetal (α2γ2 affinity>HbA)
Carbaminohemoglobin (CO2-Hb) (Carries 20% CO2 )
Carboxyhemoglobin (CO-Hb)
Methemoglobin (Fe3+-Hb)
S – Sickle Valine substitution for Glutamic acid Position 6 on β chain polymerizes, particularly at low O2 levels
{Hemoglobin // Myoglobin]
Stores oxygen in muscle for emergency use
Reserve for O2
Higher in slow twitch muscles
Not normal in circulation (lysis of cells) can lead to kidney damage
Bind 1 O2
Myoglobin
extra notes:
•Damaged muscle tissue (rhabdomyolysis)
•Released myoglobin (filtered by the kidneys) causes acute renal failure.
uric acid production —> chrystals
concern with statins
can block kidney tubules
•Myoglobin is a sensitive marker for muscle injury (can be marker for heart attack in patients with chest pain).
Myoglobin has low specificity for acute myocardial infarction (AMI)
CK-MB, cTnT, ECG, and clinical signs should of course be taken into account to make the diagnosis
function of the lungs is to take oxygen from the atmosphere as a gas and put it into a liquid environment (blood).
& CO2 (in the blood) from cellular metabolism and transport it back into the atmosphere.
This is done by three main principles —-
1.
2.
3.
changes in pressure,
change in concentration,
chnage in solubility.
notes:
As we go through oxygen/CO2 transport, we are really talking about gas transport.
It always will occur by diffusion and down a concentration gradient.
note: (CO2 is more soluble than oxygen).
Helium has a very low solubility,
Each gas exerts a partial pressure on the overall atmosphere.
the total barometric pressure at sea level is 760 mmHg and gases each exert a partial pressure to make that total of 760 mm Hg.
, once a gas is bound to a substance (like oxygen being bound to Hb) it does not exert a partial pressure anymore.
Red blood cells timeline
in the womb:
first week —
middle trimester —
last month —
(birth - till puberty)
—
after pubery —
first week — Yolk sac
Middle trimester — Fetal liver
(also spleen/lymph nodes)
•Last month –From the bone marrow
—
•After puberty only from rib, sternum, and vertebra
notes:
and vise verse for kidney/live examples^
both have a direct affect on RBC // Hb’s
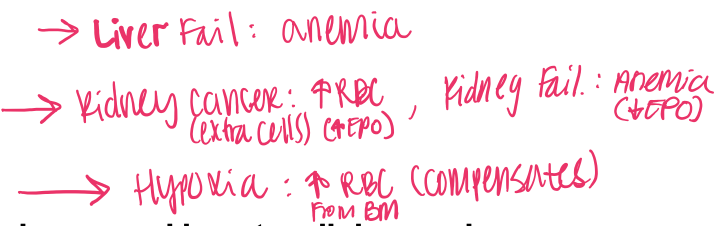
RBC production is induced by production of
erythropoietin by the kidney
e.g. kidney failre —> likely to be hypoxic or low Hb because EPO output will be too low
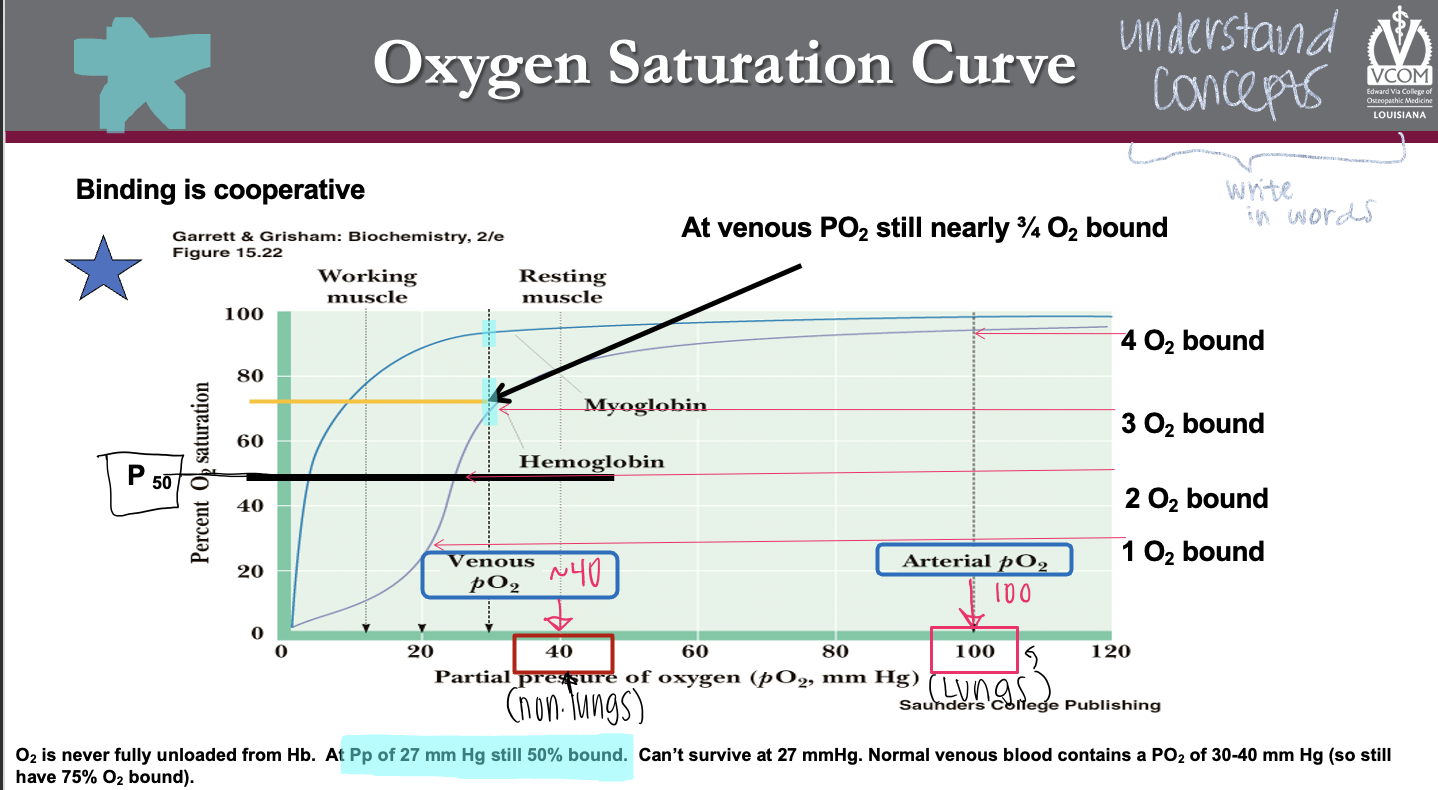
at 100mmHg (arterial pO2) lungs have offloaded O2 into blood
Hb is 100% bounded (4O2)
—> now looking at venous pO2
=40mmHg
75% post devilvery
—> which means Hb is only delivered to about 25% of the tissues
(3/4 Hb chains has O2 bounded in the blood)
at P50 = 27mmHg = 50% bounded
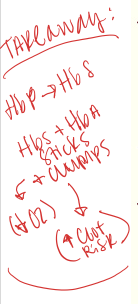
A single amino acid change on the surface of Hb β chain (Hb S) changes shape of Hb
Causes Hb (S) to stick to Hb (A) and form large aggregates (clumps). Happens more so in low pH
As Hb falls out of solution inside red blood cell cell takes on a sickle shape.
Aggregated Hb is a poor O2 transporter.
Sickled cells clog small capillaries, blocking blood flow in tissues.
(can cause ishemic injury)
Sickle-cell Anemia
•Form of the oxygen-carrying protein hemoglobin, in which the iron in the heme group is in the Fe3+ (ferric) state, not the Fe2+ (ferrous) of normal hemoglobin.
•Normally only 1% in normal person
•cannot carry oxygen.
It is a bluish chocolate-brown in color (term cyanosis-blue color).
•The NADH-dependent enzyme
methemoglobin reductase is responsible for converting methemoglobin back to hemoglobin.
Methemoglobin
used to tx cynanide posioning! ***
Amyl nitrite is administered to treat cyanide poisoning.
It works by converting hemoglobin to methemoglobin
which allows for the binding of cyanide and the formation of non-toxic
—> cyanomethemoglobin.
________ is administered to treat cyanide poisoning.
(& how does it work?)
Amyl nitrite
It works by converting hemoglobin to methemoglobin
which allows for the binding of cyanide and the formation of non-toxic
—> cyanomethemoglobin.
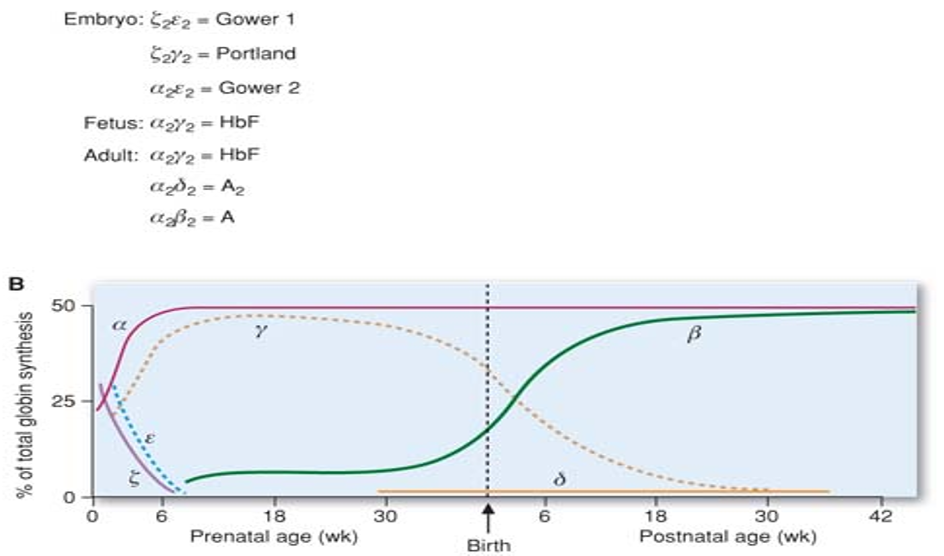
•Different subunits have slightly different structure, slightly different O2 binding properties, based on developmental stage of fetus and O2 demands.
•
•α always present
•
•γ major second subunit during development (HbF α2γ2), quickly replaced by β after birth (HbA α2β2).
•
•HbF has higher affinity for oxygen than HbA (this is how fetus can get O2).
^^ KNOW THIS
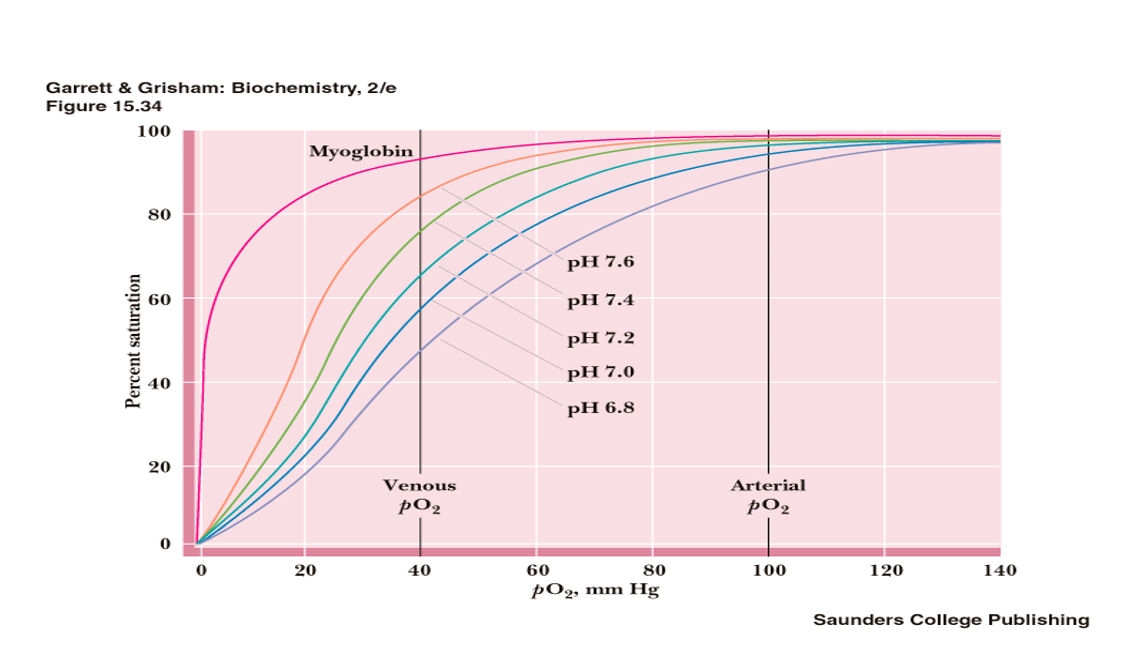
5 Factors that Modify Hb O2 Binding Affinity
•Blood pH
•CO2 levels
•2,3-bisphosphoglycerate
•Temperature
•Hb chain composition
(HbF has higher affinity for O2) this helps the fetus get more oxygen from the mother.
If you incr. CO2 or increase H protons (decreasing pH) (IN THE TISSUES)
what do we see on a graph
hint: the Bohr effect!!
we see a right shift!!
Hb has a lower O2 affinity
(THE OPPOSITE OCCURS IN THE LUNGS)
(note: myoglobin is unaffected)
2,3-BPG is present in human red blood cells and binds with greater affinity to….
deoxy or oxy Hb????
deoxygenated hemoglobin»
-- It interacts with deoxygenated hemoglobin Beta subunits by decreasing their affinity for oxygen,
so it allosterically promotes the release of the remaining oxygen molecules bound to the hemoglobin,
—> enhancing the ability of RBCs to release oxygen near tissues that need it most.
That’s the reason why 2,3-BPG works as an allosteric effector.
(note: Fetal Hb doesnt have this, so it has a HIGHER affinity for O2)
—
note: •in the absence of 2,3-BPG, oxygen binding to Hb follows a rectangular hyperbola.
•The sigmoid binding curve is only observed in the presence of 2,3-BPG. !!!!
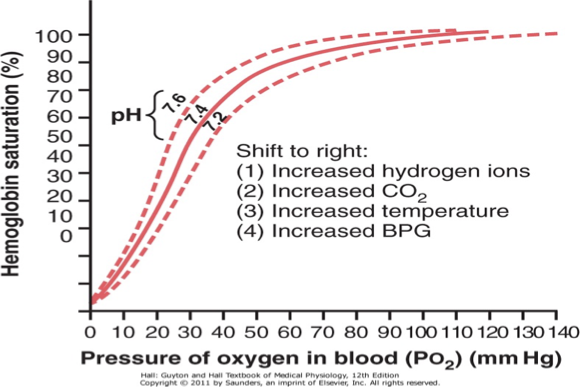
note:
Now for increased temperature, you just have to remember when things get hotter they come apart. So when you exercise you can create heat and increase unloading O2 to working muscles.

The flow rates for CO2 and O2 are shown for 1 L of blood.
The CO2 production to O2 consumption is the respiratory exchange ratio, R, which at rest is ________
^IN USA ***
approx. 0.8.
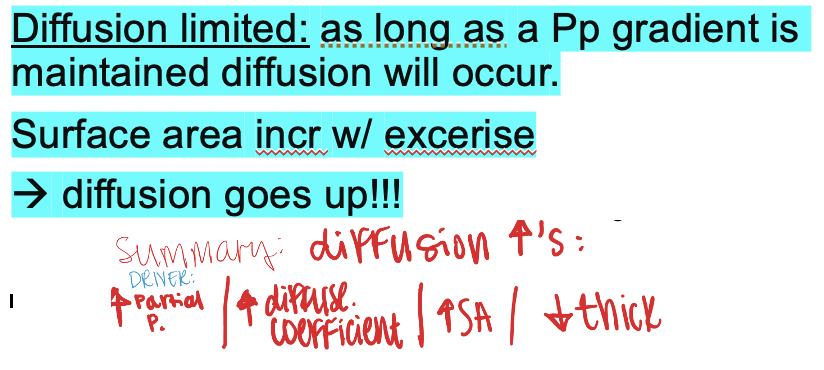
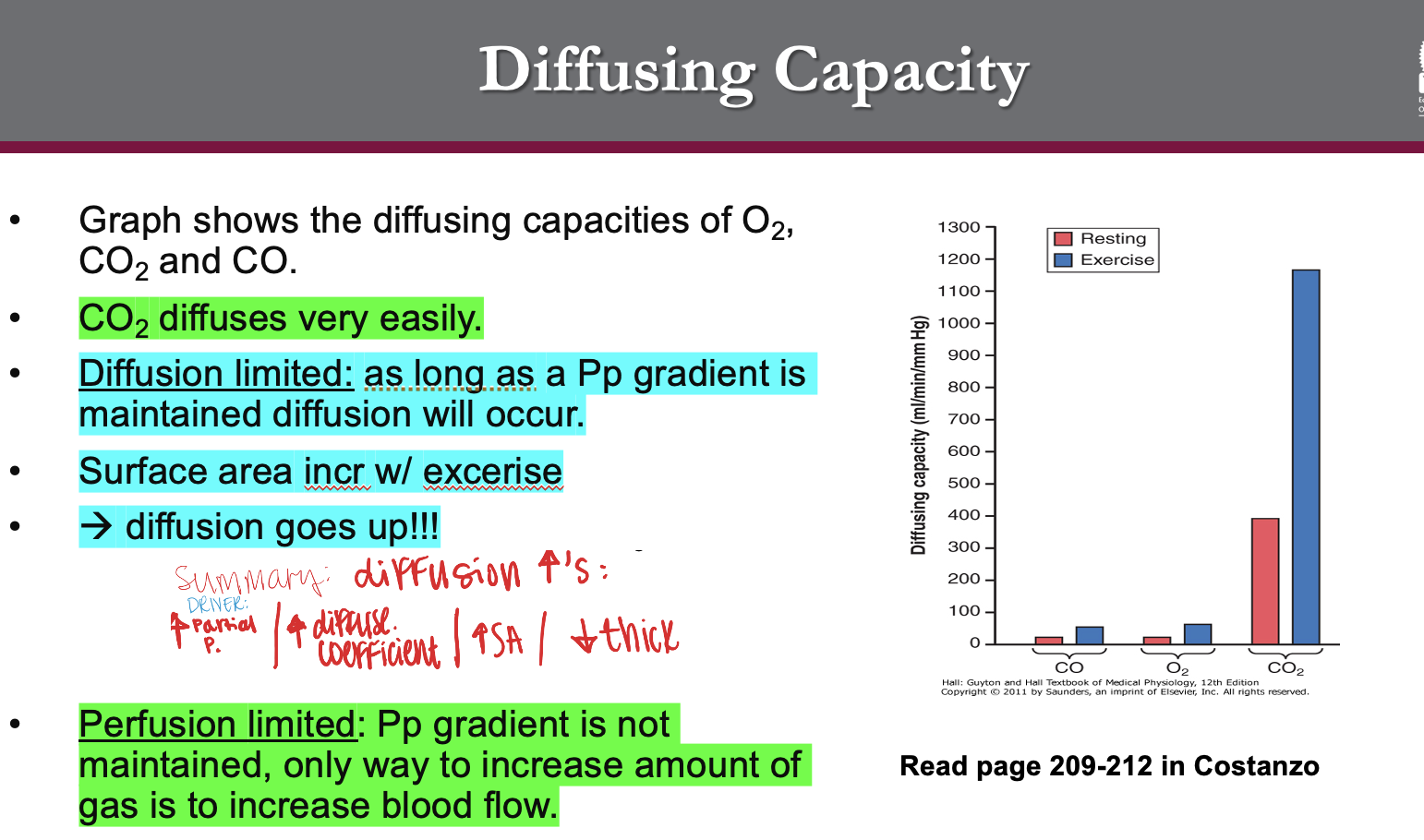
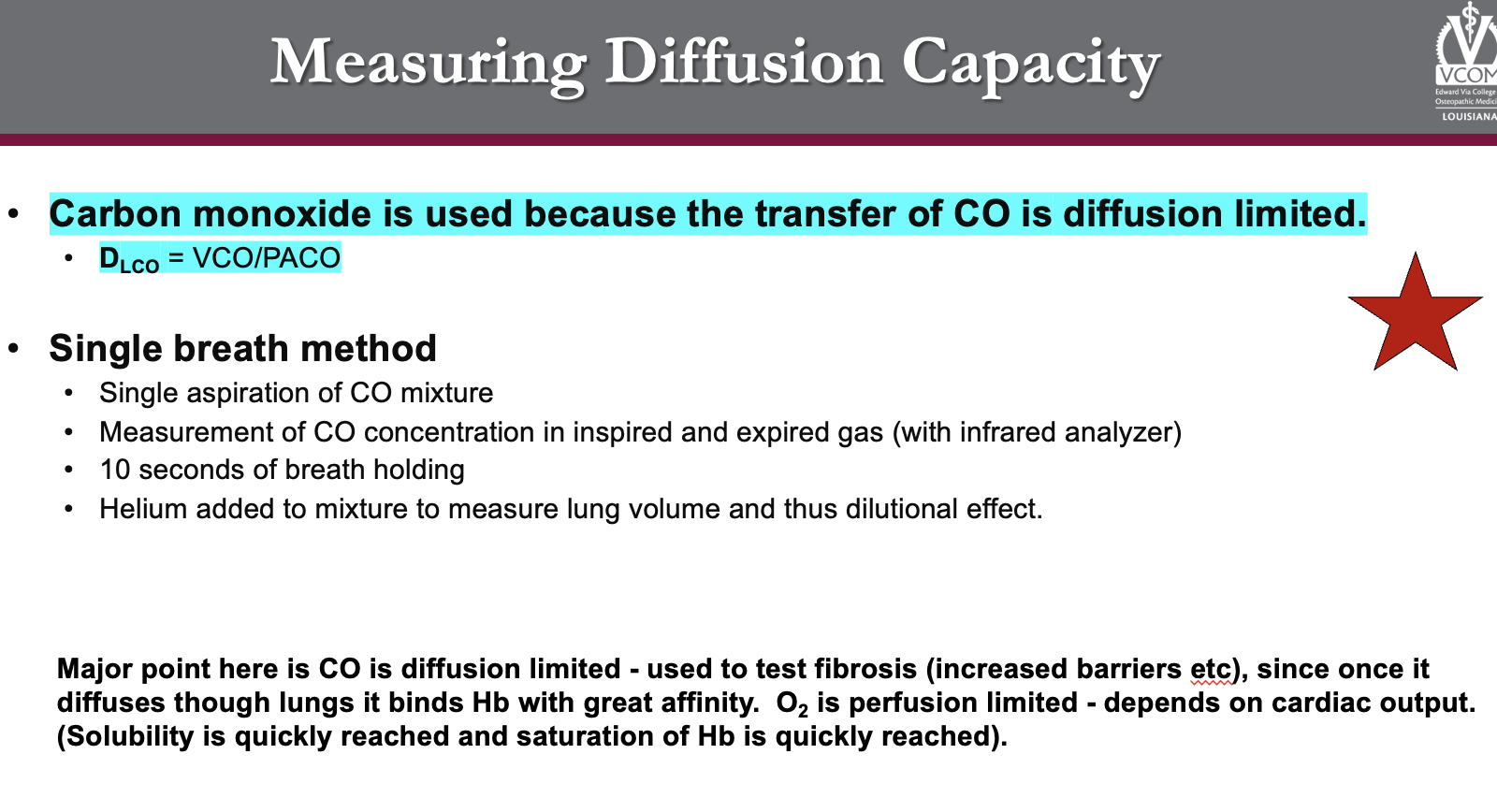
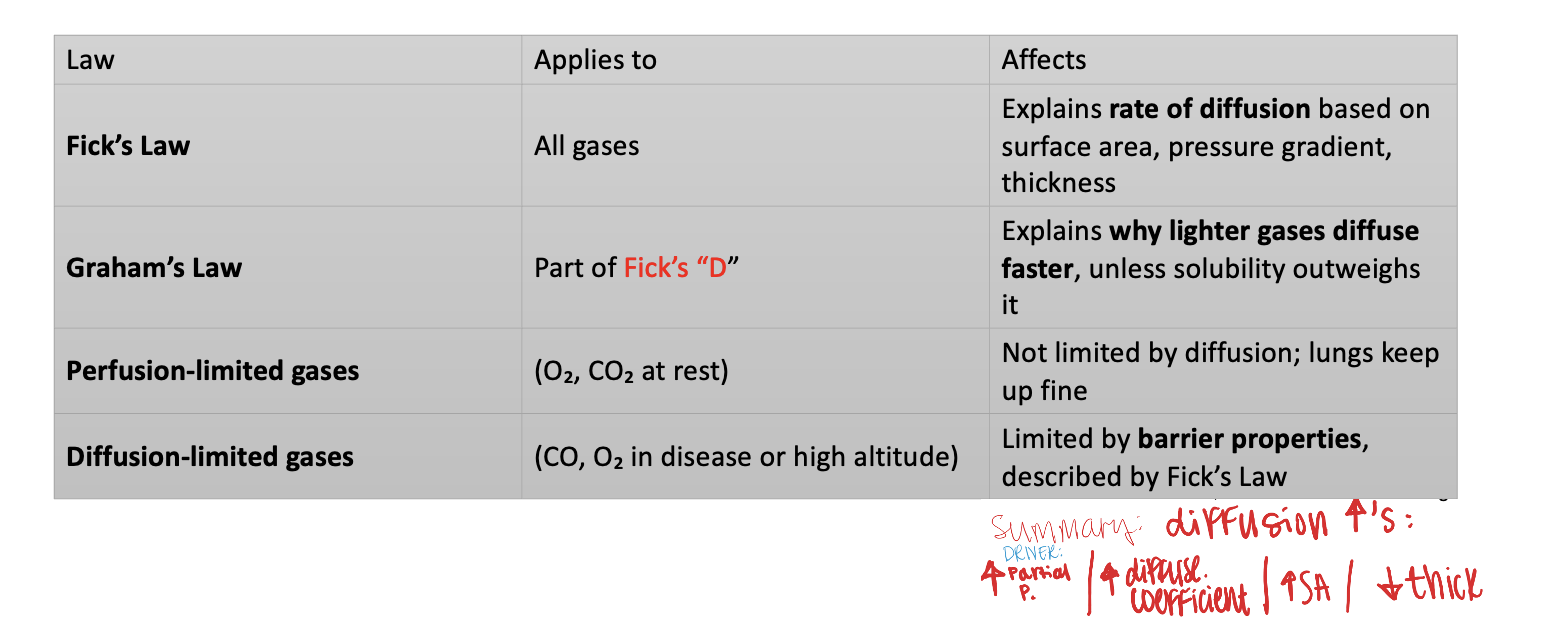
•The rate of diffusion is directly proportional to the solubility coefficient of the gas and inversely proportional to the square root of its molecular weight.
•CO2 diffuses 20x faster than O2.
Graham’s law
(incr. solubility, incr diffusion rate; lower molecular weight, higher diffusion rate.)
The diffusion of a gas across a sheet to tissue is directly related to the:
surface area, diffusion constant of the specific gas, and the partial pressure difference.
Fick’s law
•Diffusion is directly proportional to the driving force, diffusion coefficient, and the surface area. It is inversely proportional to the thickness of the membrane.
•Driving force (partial pressure differences of the gases)
•Diffusion coefficient – depends on molecular weight and solubility
•Thickness of membrane; more mucus means longer distance to travel.
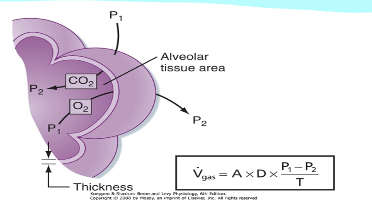

V = flow
A = surface area for exchange
increase in exercise,,,,,,, decrease in emphysema
T = thickness of the membrane
Increases in fibrosis
D = diffusion constant
P1 - P2 = partial pressure gradient
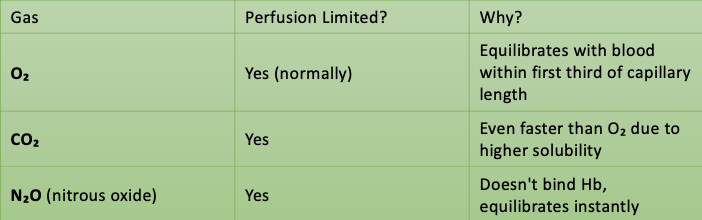
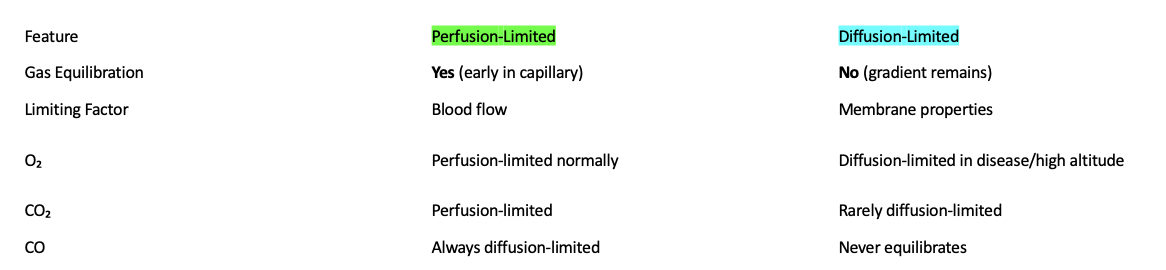
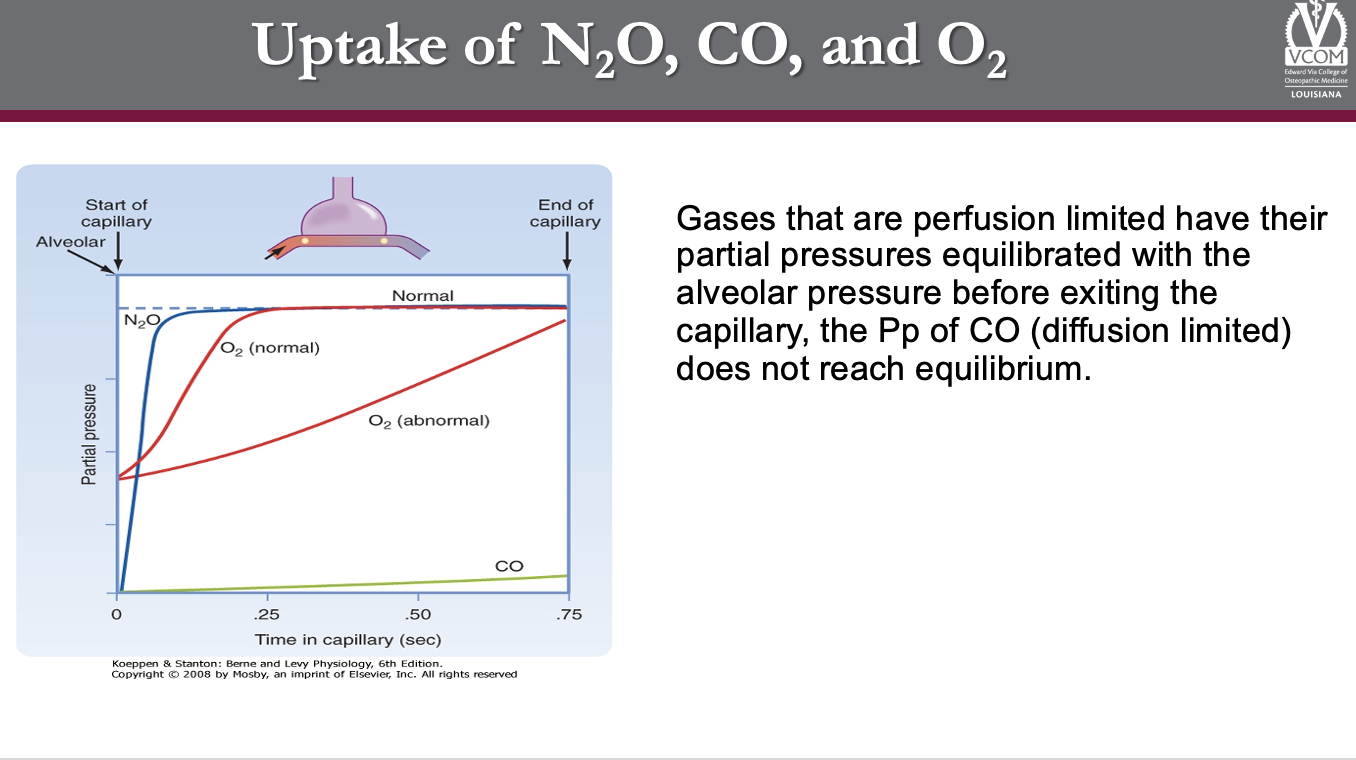
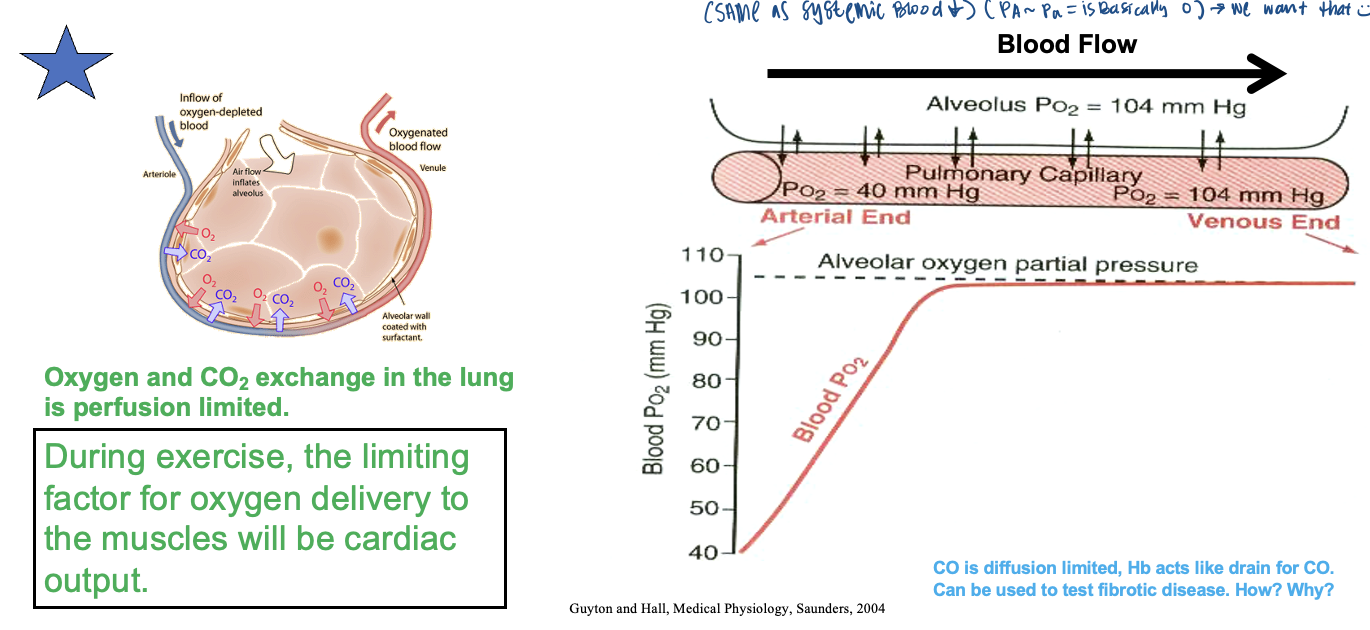
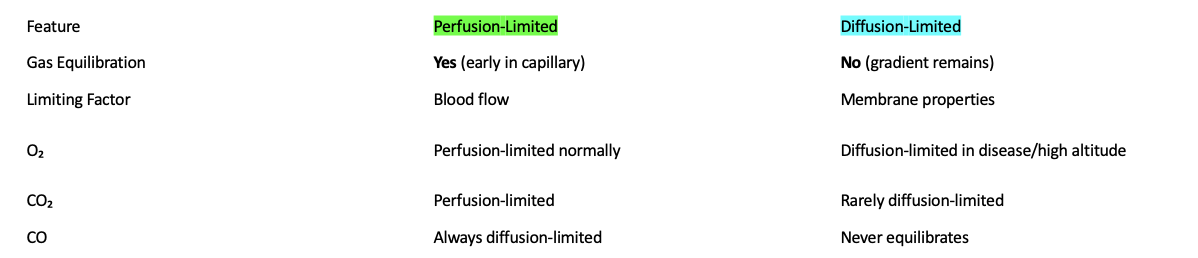
Perfusion or diffusion limited gases??
•Definition: Gas equilibrates quickly between alveoli and blood.
•The amount transferred is limited by blood flow (perfusion).
•More blood flow → more gas uptake.
Perfusion-Limited Gases (e.g., O₂, CO₂, N₂O)
notes for undertsanding:
Different gases have different solubility factors, and some are insoluble.
Gases that are insoluble in the blood do not chemically combine with proteins in the blood and equilibrate rapidly between alveolar gas and blood.
The diffusion of insoluble gases between alveolar/ blood is considered perfusion limited
because of the partial pressures of gas leaving the capillary has reached equilibrium with alveolar gas and is limited by the amount of blood perfusion in the alveolus.
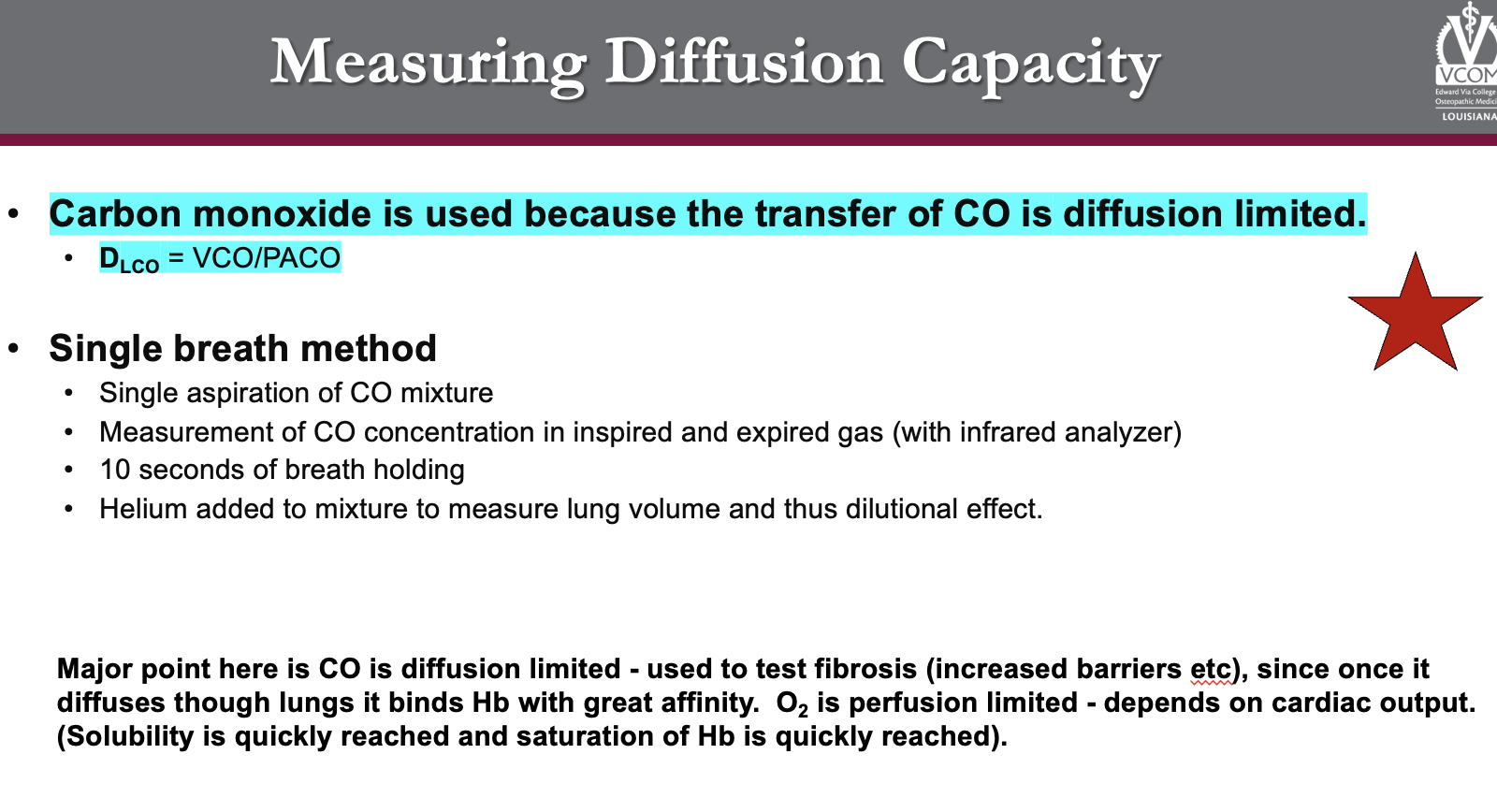
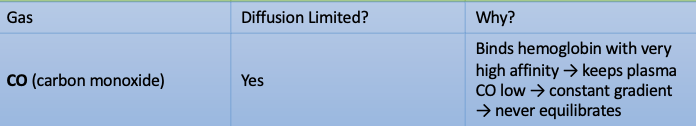
In contrast, a diffusion limited gas such as CO has low solubility in the alveolar capillary membrane but high solubility in the blood because of its high affinity for hemoglobin.
The high affinity for CO with Hb enables large amounts of CO to be taken up in the blood with little or no appreciable increase in its partial pressure.
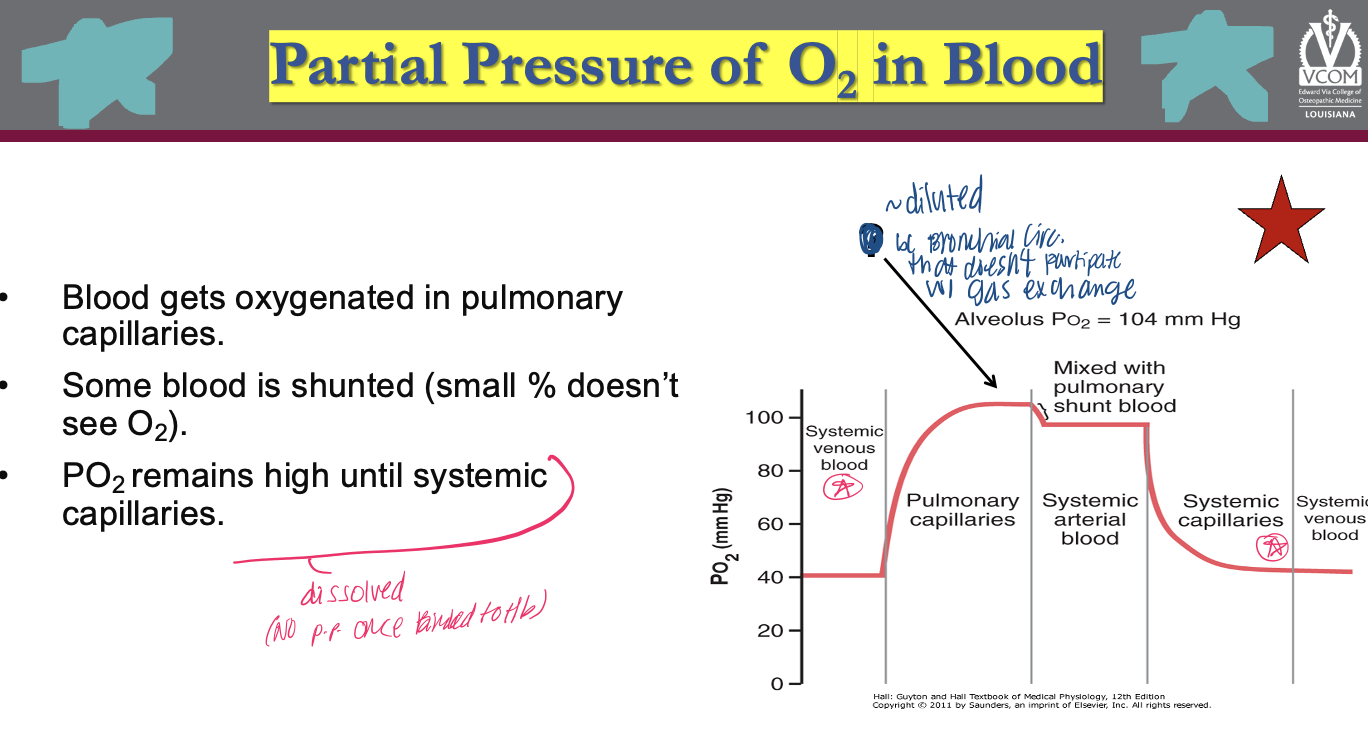
Blood enters the arterial end of the pulmonary capillary at a PO2 of 40 mm Hg, whereas alveolar PAO2 is approximately 100 mm Hg.
As the blood passes along the capillary, O2 diffuses across the blood gas barrier and dissolves in the plasma, increasing the plasma PO2 until it equals PAO2.
Under normal conditions, equilibration occurs before the midpoint of the capillary.
In other words, all the O2 that will bind the Hb happens at the beginning of the capillary system,
—> so if you increase perfusion during exercise, you will generally still bind nearly all of your Hb with O2.
If you increase in perfusion, you do NOT compromise PaO2.
So, in exercise (the limiting factor for oxygen delivery to the muscles will be cardiac output).
•Definition: Gas does not equilibrate between alveoli & blood
during the time it spends in the capillary.
•Limited by how fast it can diffuse across the alveolar membrane.
More blood flow doesn’t help, because the barrier (not flow) is the bottleneck
Diffusion-Limited Gases (e.g., CO)
During exercise, the limiting factor for oxygen delivery to the muscles will be ______
cardiac output.
notes for undertsanding:
Different gases have different solubility factors, and some are insoluble.
Gases that are insoluble in the blood do not chemically combine with proteins in the blood and equilibrate rapidly between alveolar gas and blood.
The diffusion of insoluble gases between alveolar/ blood is considered perfusion limited
because of the partial pressures of gas leaving the capillary has reached equilibrium with alveolar gas and is limited by the amount of blood perfusion in the alveolus.
In contrast, a diffusion limited gas such as CO has low solubility in the alveolar capillary membrane but high solubility in the blood because of its high affinity for hemoglobin.
The high affinity for CO with Hb enables large amounts of CO to be taken up in the blood with little or no appreciable increase in its partial pressure.
Blood enters the arterial end of the pulmonary capillary at a PO2 of 40 mm Hg, whereas alveolar PAO2 is approximately 100 mm Hg.
As the blood passes along the capillary, O2 diffuses across the blood gas barrier and dissolves in the plasma, increasing the plasma PO2 until it equals PAO2.
Under normal conditions, equilibration occurs before the midpoint of the capillary.
In other words, all the O2 that will bind the Hb happens at the beginning of the capillary system,
—> so if you increase perfusion during exercise, you will generally still bind nearly all of your Hb with O2.
If you increase in perfusion, you do NOT compromise PaO2.
So, in exercise (the limiting factor for oxygen delivery to the muscles will be cardiac output).
Concept | Meaning |
|---|---|
O₂ binds Hb fast | Happens early in pulmonary capillary (first ⅓) |
Exercise = faster flow | Less time in capillary, but still enough for full O₂ loading |
PaO₂ remains normal | Because lungs aren’t the limiting factor |
Limiting factor = cardiac output | How much oxygenated blood reaches muscles |
What Limits O₂ Delivery During Exercise?
✅ Not the lungs.
✅ Not PaO₂ (remains normal or even rises slightly).
🚴 The limiting factor is:
Cardiac output — how much oxygenated blood you can send to the muscles per minute.
This is why trained athletes develop:
Larger stroke volume
Higher cardiac output
More capillaries and mitochondria in muscle
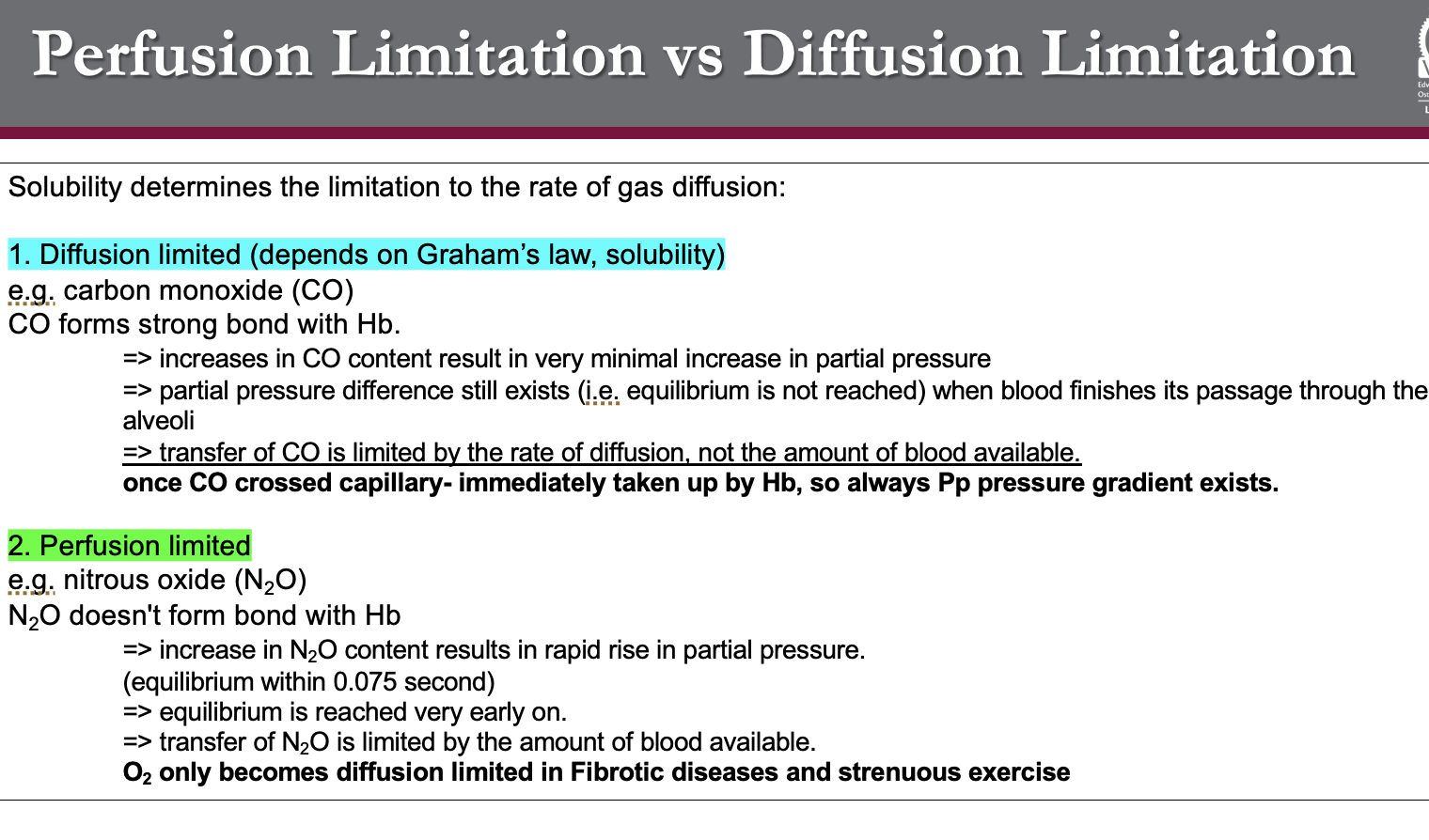
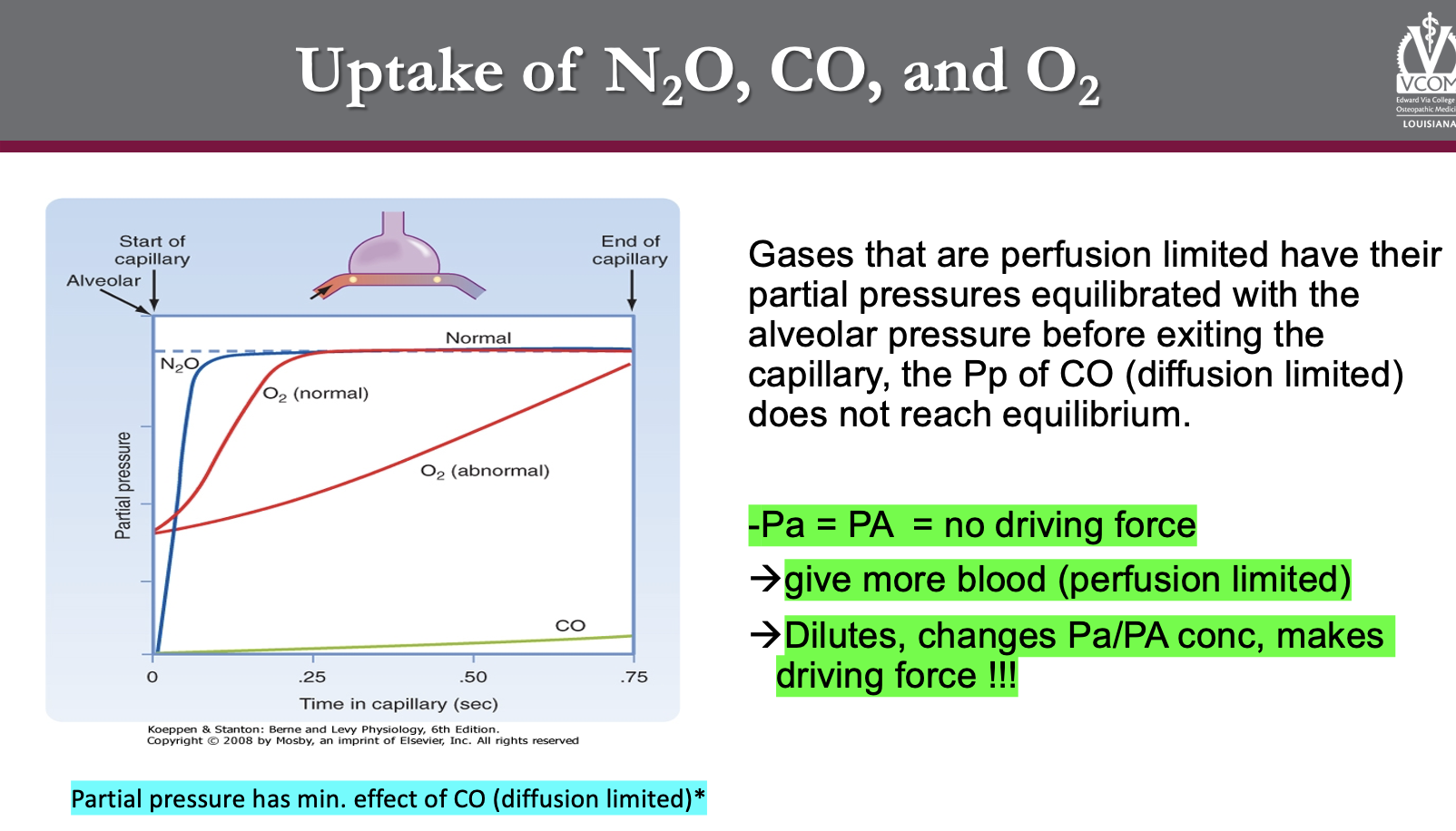
N2O does not bind any Hb so it reaches equilibrium pretty quick, because it diffuses pretty easily so the only way to get more N2O in the blood is to remove the saturated blood (so we say N2O is perfusion limited).
O2 normally is perfusion limited due to Hb getting saturated pretty quickly.
CO is diffusion limited since once it get across it quickly binds the Hb more effectively than O2 and will never reach saturation until all the Hb is bound.
In this case, you are probably dead.
key point for gas laws:
Oxygen Transport in Blood in 2 Forms
•About 20% volume or 20 mL of O2 per 100 mL of blood (exists in two forms).
form 1 —?
form 2 —?
•Form 1 - 0.3% is dissolved (CONSTANT!!)
•Dissolved in blood is related to Pp of O2 and solubility
(solubility of O2 in blood is 0.003 mL O2/100 mL blood)
-
•Form 2 - Amount carried by Hb 99.7%
•Depends on concentration and saturation
•Normal Hb concentration 13-15 g/100 ml blood
Is increased in polycythemia - does not affect PO2
(more rbc’s)
Is decreased in anemia
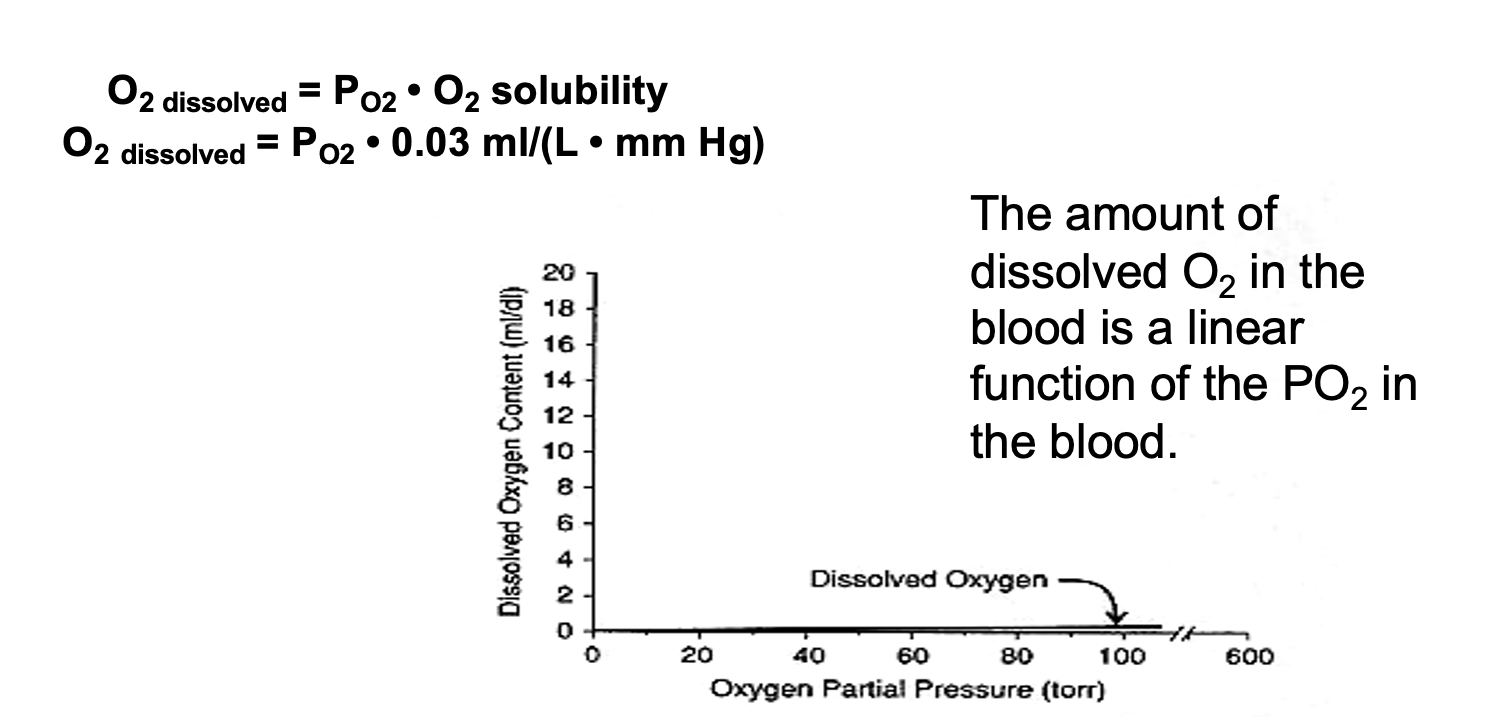
Incre. In either
= incr. in O2 dissolved
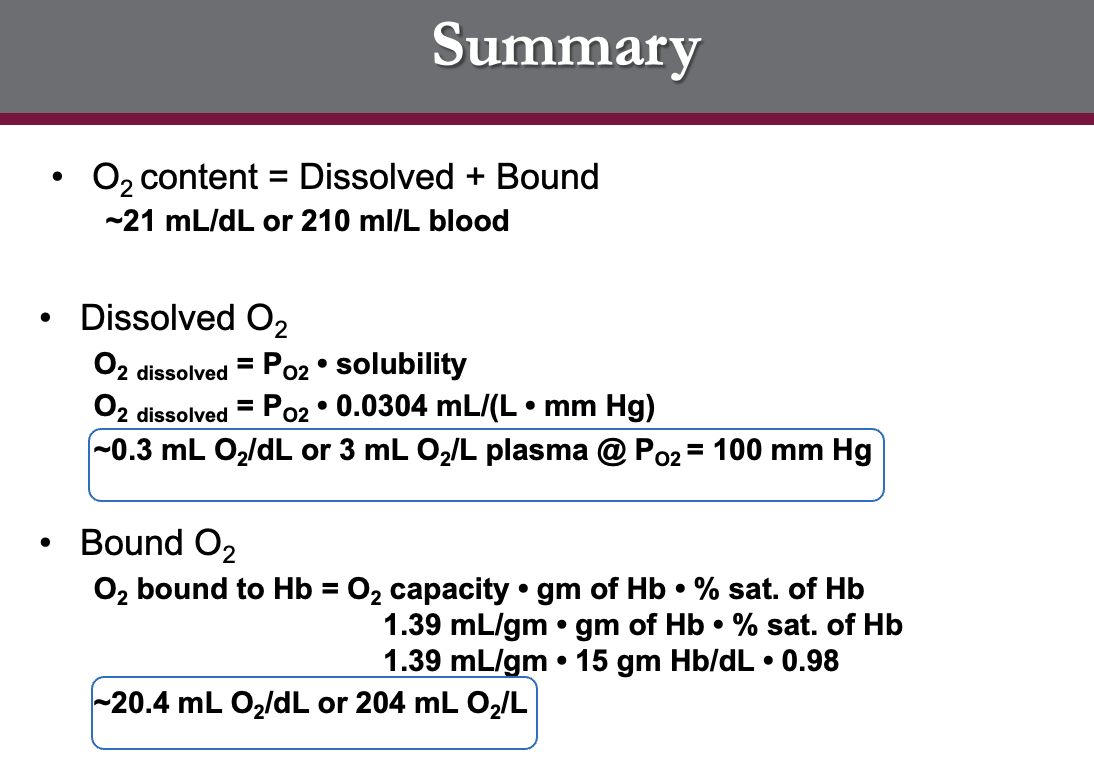
So actually little O2 is dissolved in blood, most of O2 is bound to Hb.
If O2 is bound to Hb then it does not exert a partial pressure.
Oxygen Dissociation Curve
what affect to the graph will these have if increased?
Temperature
PCO2
Acidity
2,3-Diphosphoglycerate (2,3-DPG)
if increased:
Temperature ——— incr. P50, right shift
PCO2————————— incr. P50, right shift
Acidity ————————-incr. P50, right shift
2,3-Diphosphoglycerate (2,3-DPG) —— incr. right shift
•In polycythemia OR anemia,????
, total O2 will increase but dissolved O2 will remain the same (so PO2 will not be affected).
•
Polycythemia
anemia
, total O2 will DECREASE but dissolved O2 will remain the same (so PO2 will not be affected).
—
- does not affect PO2 — because its only affecting Hb for the most part!!
•Form 2 - Amount carried by Hb 99.7%
•Depends on concentration and saturation
•Normal Hb concentration 13-15 g/100 ml blood
Is increased in polycythemia - does not affect PO2
(more rbc’s)
Is decreased in anemia - does not affect PO2
total amount (or concentration) of O2 in the blood, including free and bound forms
-
A. Dissolved O2
B. Hb or O2 saturation
C. Arterial O2 saturation (SaO2)
D. O2 content (or concentration)
O2 content (or concentration)
amount of O2 in solution as defined by the PO2 and O2 solubility
-
A. Dissolved O2
B. Hb or O2 saturation
C. Arterial O2 saturation (SaO2)
D. O2 content (or concentration)
Dissolved O2
amount of O2 bound to Hb as a percentage of the total O2 binding capacity of Hb in a blood sample
- A. Dissolved O2
B. Hb or O2 saturation
C. Arterial O2 saturation (SaO2)
D. O2 content (or concentration)
Hb or O2 saturation