M6: S5: the Small intestine
1/56
Earn XP
Description and Tags
• Describe the mechanisms responsible for the digestion of carbohydrates, protein, and fat. • Describe how carbohydrates, protein, and fats are absorbed. • Understand segmentation as a mechanism of motility. • Describe the anatomical features of the small intestine that make it an ideal location for absorption.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
Describe the mechanisms responsible for the digestion of carbohydrates, protein, and fat.
Describe how carbohydrates, protein, and fats are absorbed.
Understand segmentation as a mechanism of motility.
Describe the anatomical features of the small intestine that make it an ideal location for absorption.
Describe the mechanisms responsible for the digestion of carbohydrates, protein, and fat.
Describe how carbohydrates, protein, and fats are absorbed.
Understand segmentation as a mechanism of motility.
Describe the anatomical features of the small intestine that make it an ideal location for absorption.
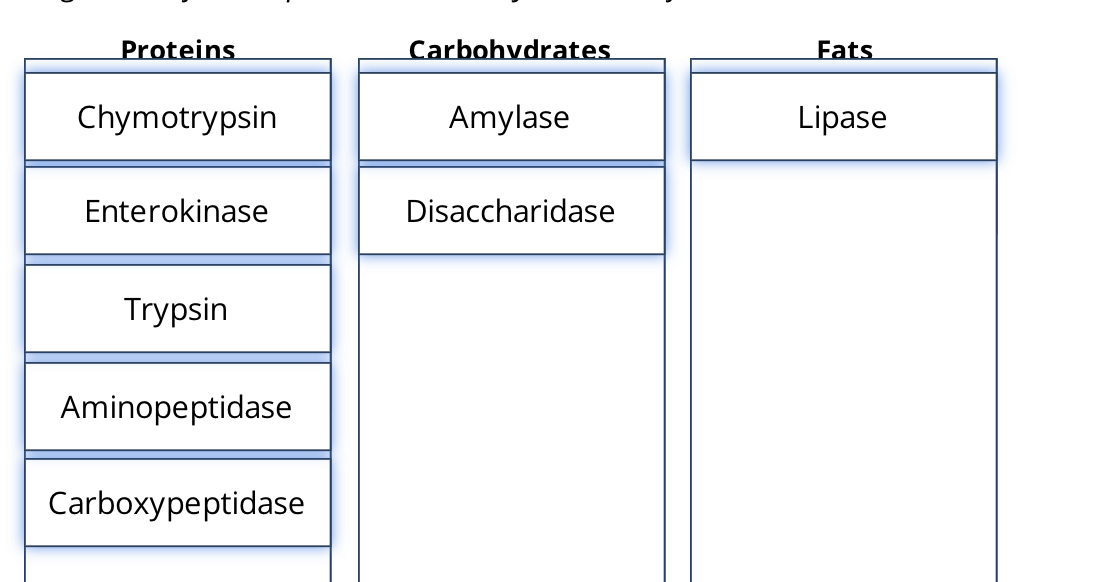
where is the small instine anatomaically
between the stomach and the large intestine
where does the majoirty of digestion occur
in the small instestine
what are the different parts of the small instestine
Duodenum
Jejunum
iileum
T or F: the movement in the small intestine is peristaltic
F: the movement is not peristalitic. The term for motility in the small intestine is segmentation, which both mixes and slowly propels the chyme.
what kind of movement in the small intestine
The term for motility in the small intestine is segmentation, which both mixes and slowly propels the chyme.
what is is the migrating motility complex
This motility consists of weak peristaltic waves that are sustained for only short distances before dying out. They start at the stomach and slowly move their way down the intestine. Its purpose is to move any remnants of the previous meal, any mucosal debris, and any bacteria forward towards the colon. When the peristaltic waves reach the end of the ileum, they start again at the beginning of the duodenum.
when most of the meal ha been absorbed the segmentation contractions end and are replaced by what?
When most of the meal has been absorbed, the segmentation contractions end and are replaced by the migrating motility complex.
T or F: no intestinal enzymes are secreted into the small instine lumen
T” digestion is here is the result of pancreatic enzymes, however there are some intestinal enzymes that are membrane bound and not secreted into the lumen
what do the exocrine glands in the small instine secrete
mucus
what does mucus in the small insestine do?
it provides lubrication and protection and lots of H2O for the hydrolytic reactions carried out by the digestive enzymes
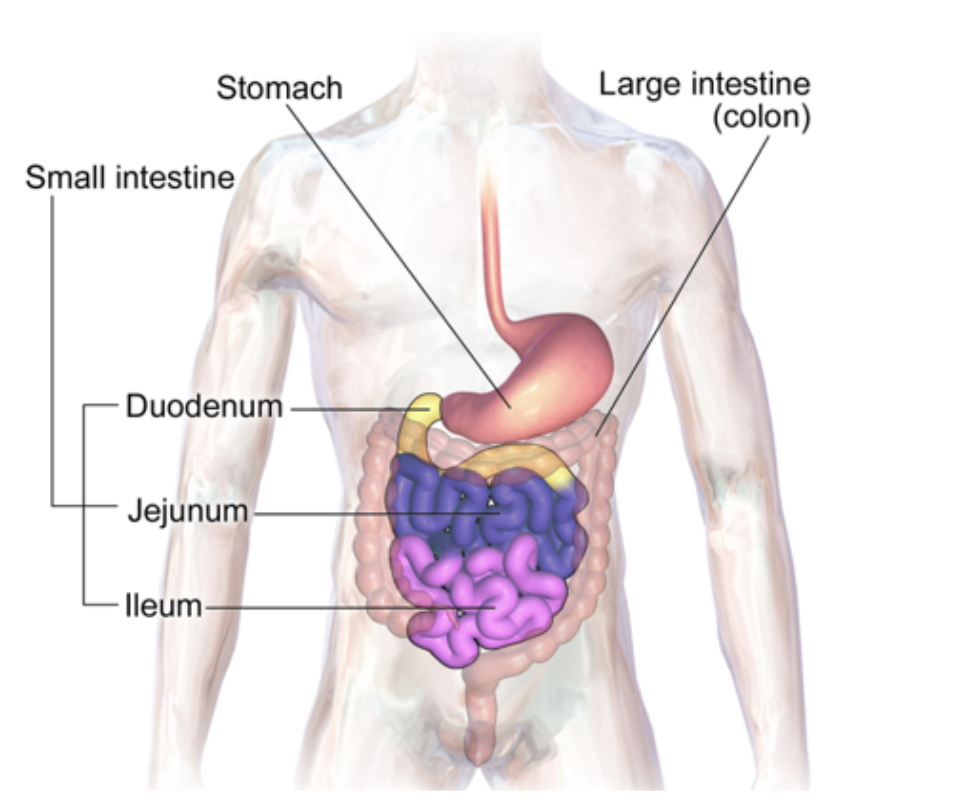
the lumincal surface of the small intestine has small hair-like prjections called what and what do they do
microvilli that form the brush border which aids in the process of absorption.
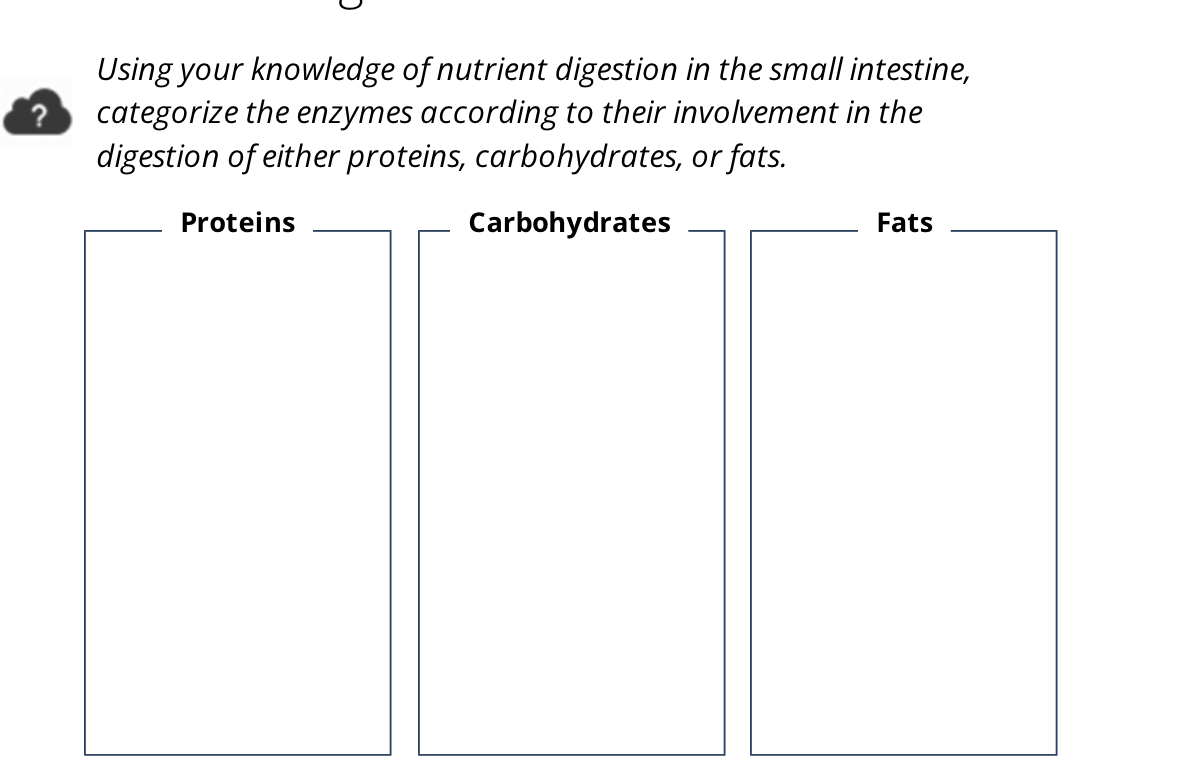
The brush border contains membrane-bound enzymes which are categorized into three classes what are they?
enterokinases, disaccharidases, aminopeptidases
what is the brush border
the lumen-facing epithelial surface of cells which bears closely packed microvilli and hydrolytic enzymes, and is thus present on cells which specialise in absorption
a person with lactose intolerance lack the disaccahridase lactase. What does this cause?
In persons with lactose intolerance, they lack the disaccharidase lactase so they are unable to break down lactose. The undigested lactose both causes an osmotic gradient so more water enters the lumen, and provides a substrate for large intestine bacteria that can break lactose down while releasing COz and methane.
The excess fluids and gases can cause cramping and diarrhoea.
what does enterokinases do
enterokinases can convert pancreatic trypsinogen to trypsin
what does disaccharidases do
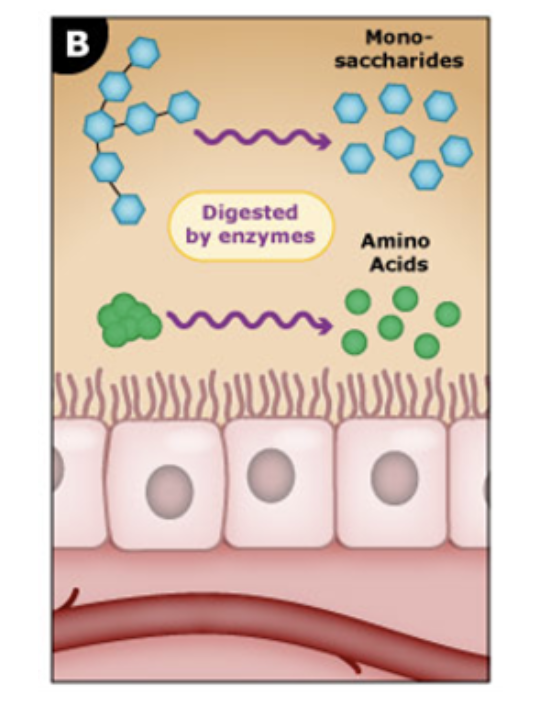
disaccharidases complete carbohydrate digestion by hydrolyzing disaccarides (maltose, sucrose, lactose) into monosaccharies
what does aminopeptidases do
hydrolyze small peptide fragements into individaul amino acids
what is the ileum vital for absorption of
Vitamin B12 and bile salts
where are does most of the absorption done of carbohydrates, proteins, fats, electrolytes, vitamins, as well as the majority of water?
Almost all absorption occurs in the duodenum and jejunum with little occurring in the ileum.
what compounds are regulated with excess being excreted int he feces
calcium and iron
these are broken down into
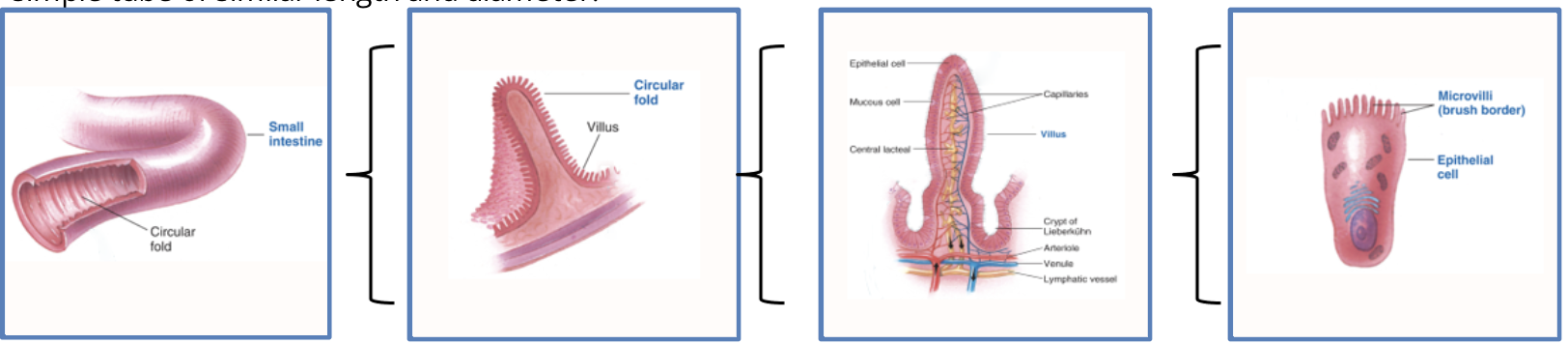
T or F: The structure of the small intestine is such that it increases the surface area 600 fold more than a simple tube of similar length and diameter.
T
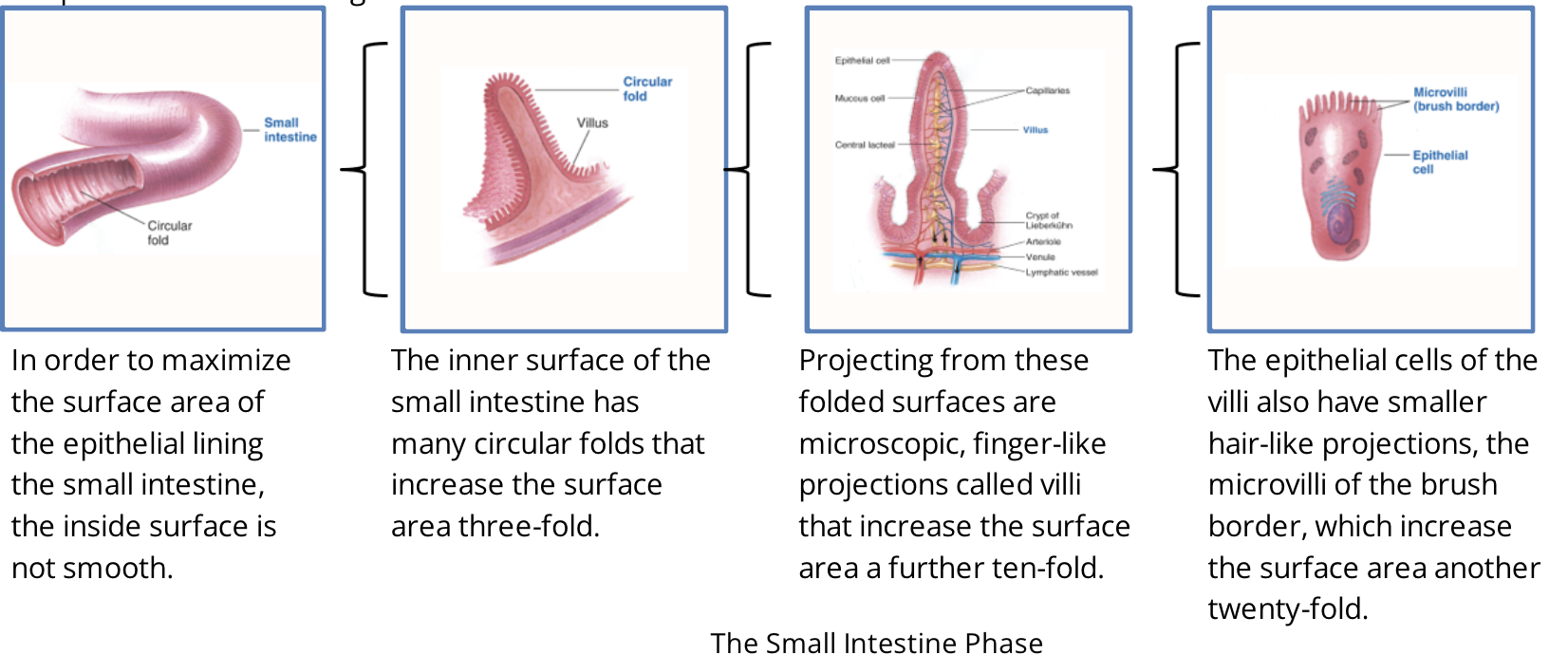
how are ways the small instine maximzes the SA
the SA of the epithial linning of the small intesine is not smooth
has folds increase the surface area 3 fold
from the folds has finger like projections called vili that increase the surface area a further ten-fold
the vili has smaller hair-like projections (microvili of the brush vorder) which increases the SA another 20 fold
T or F: Chemical digestion and nutrient absorption are essentially finished by the time food residue leaves the small intestine and enters the cecum.
T
how can sodium be absorbed in the small instine passively or activly
passively or activly : Sodium can be absorbed both passively and actively. Chloride follows sodium due to the electrical gradient and water follows sodium due to the osmotic gradient.
Chloride follows sodium due to the ——— gradient and water follows sodium due to the ——- gradient.
Chloride follows sodium due to the electrical gradient and water follows sodium due to the osmotic gradient.
how is sodium passivily absorbed in the small insestine
In the presence of an appropriate electrochemical gradient, sodium can passively move down this gradient into the interstitial fluid by moving between intestinal epithelial cells through leaky tight junctions.
how is sodium activily absorbed in the small insestine
Movement of sodium through cells requires active transport. It can passively cross the luminal membrane through sodium channels or cotransported with either glucose or amino acids. Once inside an epithelial cell, sodium is actively pumped out across the basolateral membrane into the interstitial fluid where it diffuses into the capillaries.
T or F:Movement of sodium through cells requires active transport.
T
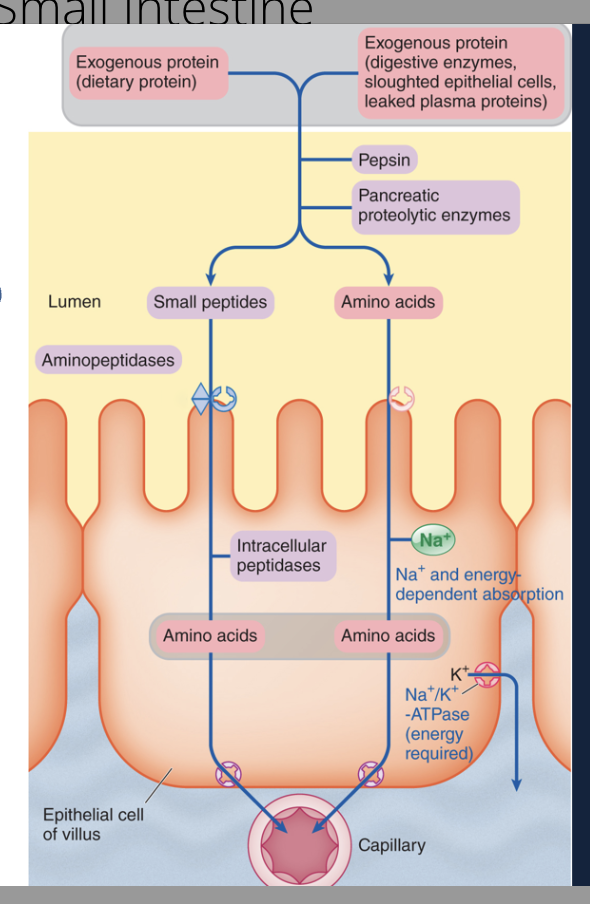
What are exogenous proteins?
Exogenous proteins are proteins that originate or are introduced from outside of an organism or cell, as opposed to being produced naturally within it.
what are the three sources of exogenous proteins that need to be abosrbed and digested
digestive enzymes are all proteins and need to absorbed
proteins from epithelial mucosal cells that have been sloughed off
plasma proteins tht normally leak from the capillaries into the digestive tract lumen
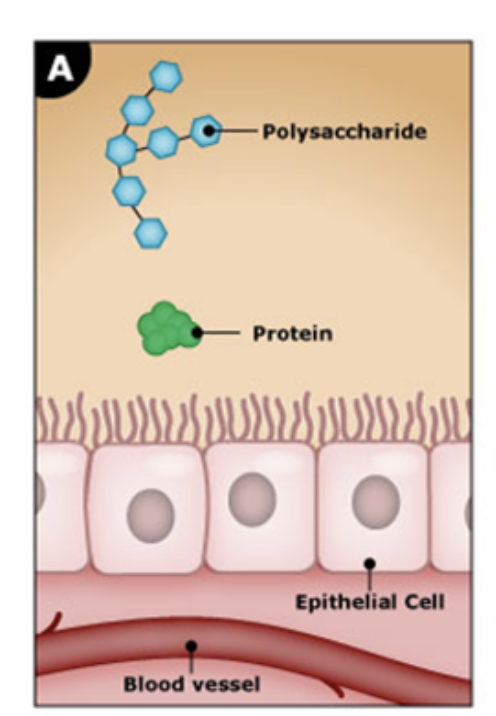
Protein from these three sources exogenous proteins alone can account for up to 40 g. Regardless the source of the proteins, they are all broken down into individual amino acids and small peptides for absorption. how are they absorbed
These are absorbed by secondary active transport, similar to glucose and galactose. Small peptides have a different carrier and are broken down both by the brush border aminopeptidases as well as intracellular peptidases. Amino acids move out across the basolateral membrane and into the blood.
how are carbhydrates absorbed as what and active or passive
as monosaccharides active transport by sodium monsaccharide cotransport or sodium-independent facilitated diffusion
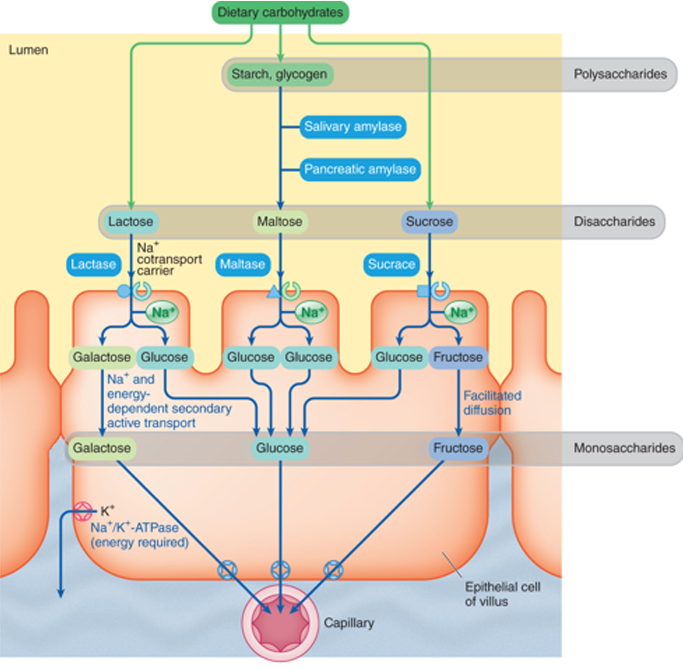
what is the preferences for monosacchairde absorption
Galactose
Glucose
Fructose
how is glucose transported for absorption
Galactose is transported first and can be absorbed by secondary active transport. Basolateral Na*-K† pumps require energy and bring Na* into the epithelial cells. This Na* is then used by cotransport carries to bring glucose and galactose into the epithelial cell.
Once concentrated inside, galactose moves down its concentration gradient across the basolateral membrane and into the blood.
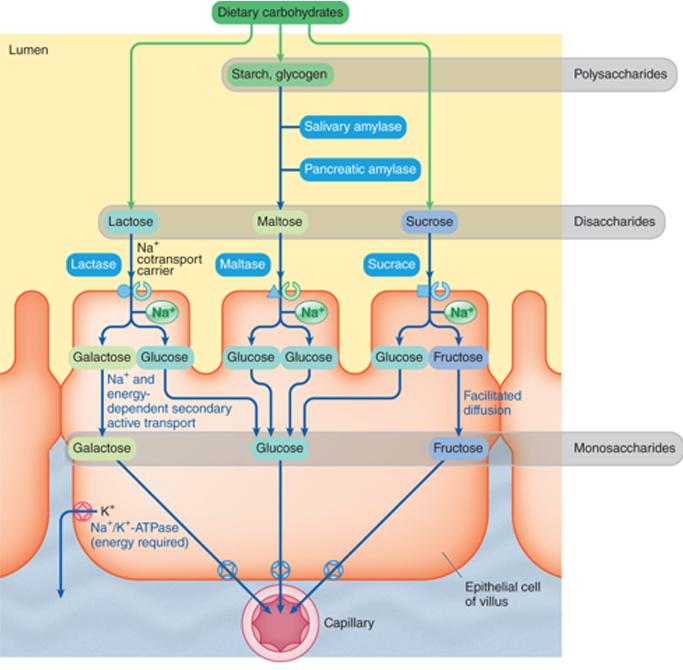
how is glucose transported for absorption
Glucose is transported second and, very similar to galactose, can be absorbed by secondary active transport. Just as in the case of galactose transport, basolateral Na*-K+ pumps require energy and bring Nat into the epithelial cells. This Nat is then used by cotransport carries to bring glucose and galactose into the epithelial cell. Once concentrated inside, glucose moves down its concentration gradient across the basolateral membrane and into the blood.
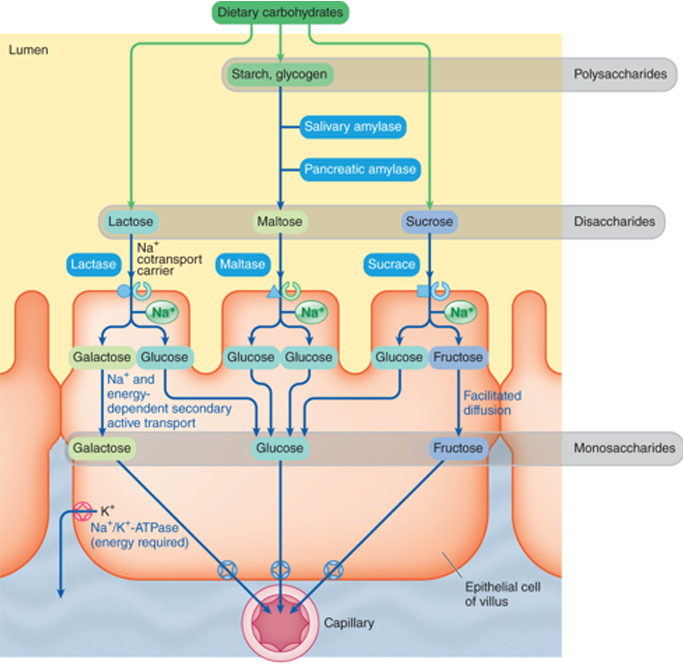
how is frucoste transported for absorbtion
Fructose is transported last and is transported by facilitated diffusion. (passive transport)

what are the four steps of fats that are absorbed by the small intestine
Recall that bile salts emulsify fats and that pancreatic lipases digest the triglycerides into monoglyceride and
fatty acids within fat droplets.
When the micelles reach the luminal membrane of the epithelial cells, monoglycerides and fatty acids can diffuse from the micelles into the epithelial cells. The micelles then return to the chyme to pick up more triglycerides. This process repeats along the length of the small intestine until all fat is absorbed. In the terminal ileum, the bile salts themselves are reabsorbed by active transport.
Once inside epithelial cells, the monoglycerides and free fatty acids are converted back into triglycerides. The triglycerides are attracted to each other and form lipid droplets and get coated with a layer of lipoprotein to make the fat droplets water soluble. In this form they are called chylomicrons.
Chylomicrons leave the endothelial cells by exocytosis. Because capillaries have basement membranes, chylomicrons cannot directly enter them. Instead, the chylomicrons are taken up into the lymphatic system before being delivered to the blood.
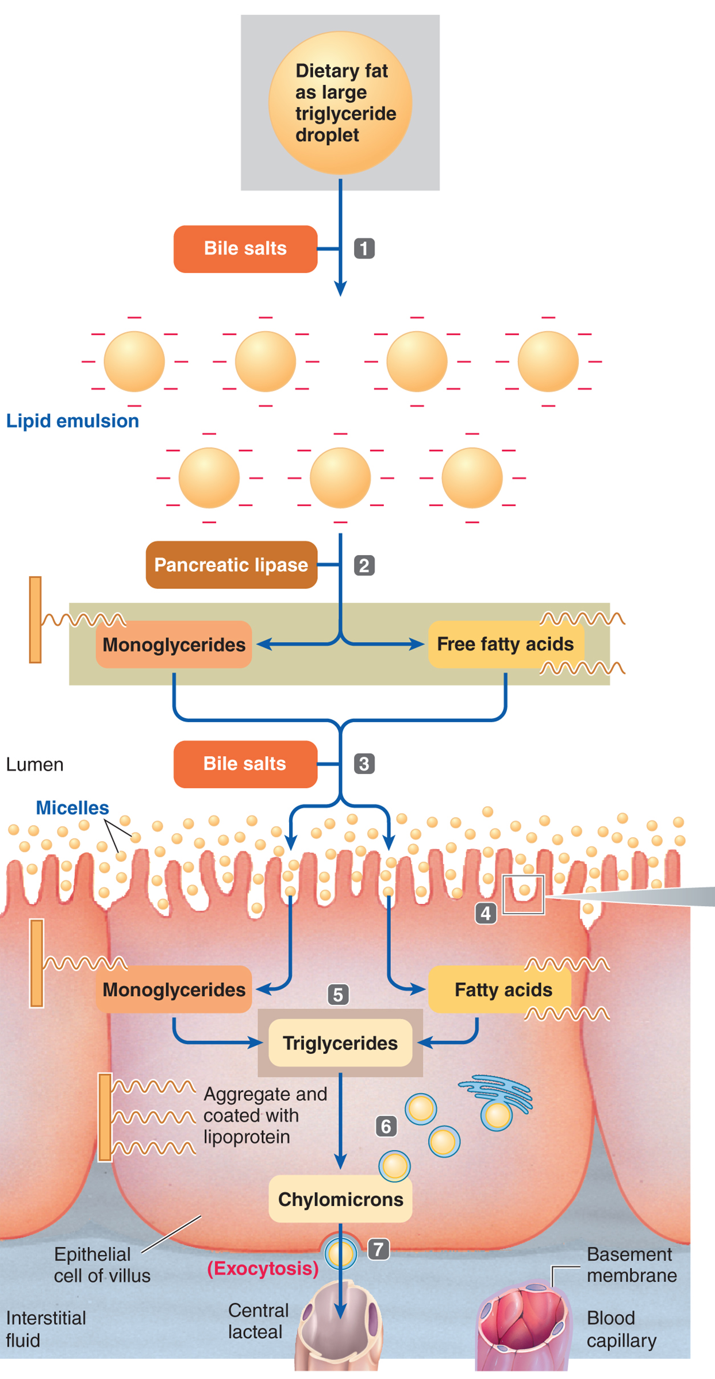
are biles salts reabsored activly or passivly
active in the ileum
Chylomicrons leave the endothelial cells by
exocytosis.
what are Chylomicrons
Once inside epithelial cells, the monoglycerides and free fatty acids are converted back into triglycerides. The triglycerides are attracted to each other and form lipid droplets and get coated with a layer of lipoprotein to make the fat droplets water soluble. In this form they are called chylomicrons.
T or F: Chylomicrons leave the endothelial cells by exocytosis. Because capillaries have basement membranes, chylomicrons cannot directly enter them. Instead, the chylomicrons are taken up into the lymphatic system before being delivered to the blood.
T
what mineral is essential for the production of haemglobin
iron
the amount of iron absrobed is dependent on what
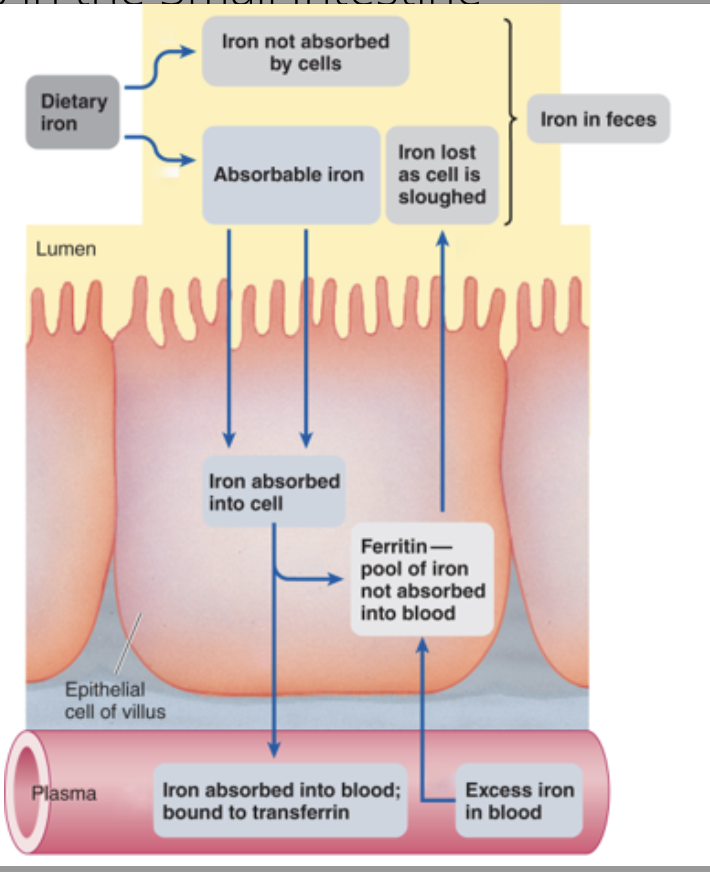
its state
Ferrous iron (Fe2+) is more readily absorbed than ferric iron (Fe3+). Only a portion of ingested iron is in the right form to be absorbed.
what state of iron is more readily absorbed
Ferrous iron (Fe2+) is more readily absorbed than ferric iron (Fe3+). Only a portion of ingested iron is in the right form to be absorbed.
Dietary iron that is absorbed into the small intestine epithelial cells and is immediately needed for red blood cells production, is transferred into the blood.
Once inside the epithelial cell, iron has two fates. what are they
If it is immediately needed for red blood cell production it is delivered to the blood where it is bound to transferrin for delivery to the bone marrow.
If it is not immediately used it is stored within the epithelial cell in a granular form called ferritin.
if iron is immediately needed for red blood cell production it is delivered to the blood where it is bound to ————- for delivery to the —— ——-.
if iron is immediately needed for red blood cell production it is delivered to the blood where it is bound to transferrin for delivery to the bone marrow.
If iron is not immediately used it is stored within the ——— cell in a granular form called ————.
If iron is not immediately used it is stored within the epthial cell in a granular form called ferritin
what happens when iron levels in the epithelial cells become too high?
iron is secreted into the intestinal lumen
T or F: Any ferritin is also dumped into the lumen when the epithelial cell is sloughed off within three days. All excess iron is excreted in the feces.
T
what is ferritin
grandular form of iron that it is stored as in the epithial cells
what is the second major way next to vomiting that loss water and disrupts body acid-base balance
diarrhoea
what are the three main causes of diarrhoea
dirrhoa can cause what when refering to acid base balance
loss of HCO3- causing metabolic acidosis