Eye
1/222
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
223 Terms
Structures in the external eye
Bony orbit
Extraocular muscles
Superior and inferior oblique
Lavatory palpebrae (eyelid)
Fat
Conjunctiva
External Eye
Bony orbit
Cavity in the skull in which the eye and appendages sit
Prevents mechanical injury
External Eye
Extraocular muscles
Muscles that control eye movement
Allows the eye to move up, down, left, right and rotate
There are 6 extraocular muscles:
Superior rectus
Inferior rectus
Lateral rectus
Medial rectus
External Eye
Extraocular muscles
Superior rectus
Inferior rectus
Medial rectus
Lateral rectus
Superior rectus » moves eye upwards
Inferior rectus » moves eye downwards
Medial rectus » moves eye toward the nose
Lateral rectus » moves eye away from the nose
External Eye
Extraocular muscles
Superior and inferior oblique
Counteract head movement - so keep vision stable when your head tilts to the side
Superior oblique: rotates the top of the eye towards the nose, helps stabilise vision when the head tilts to the opposite side
Inferior oblique: rotates the top of the eye away from the nose, helps stabilise vision when the head tilts to its own side
External Eye
Levator palpebrae (eyelid)
Protects and lubricates the eye
External Eye
Fat
Surrounds eye within the bony orbit
Functions:
Allows smooth movement of eye muscles
Acts as a lubricant so eye can move around
External Eye
Conjuctiva
Thin mucus membrane covering the sclera
Folds and joins the inner lining of the upper and lower eyelids » forms a bag-like structure called conjunctival sac
Lubricates the eye with mucus and tears
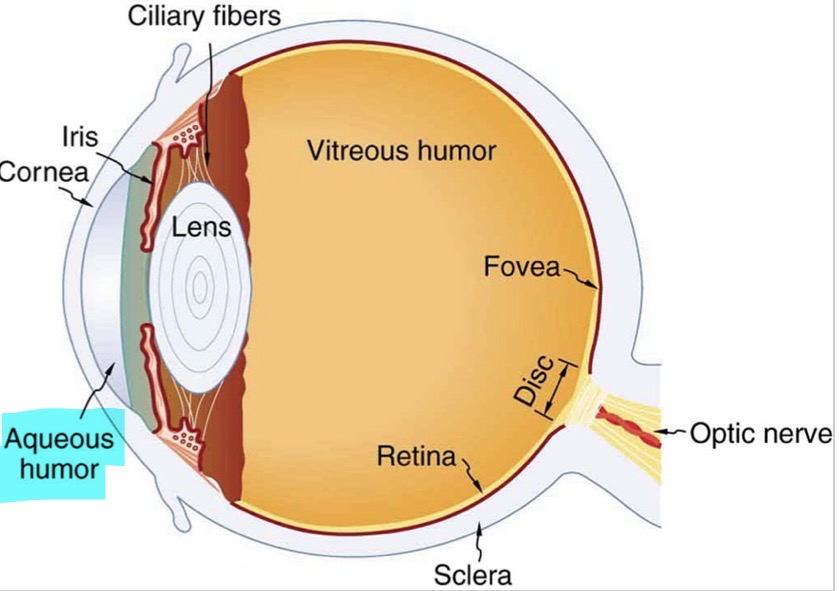
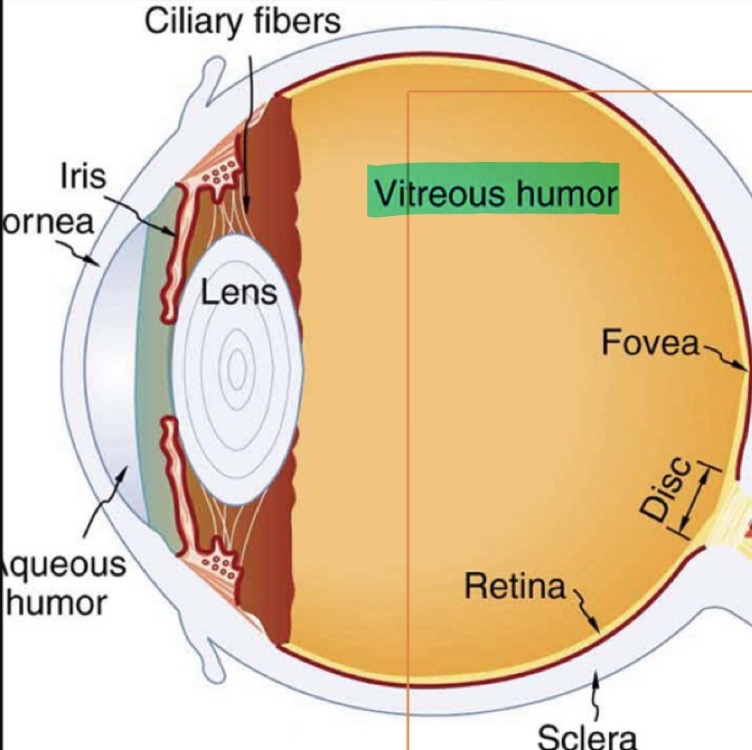
Label the overall structure of the eye
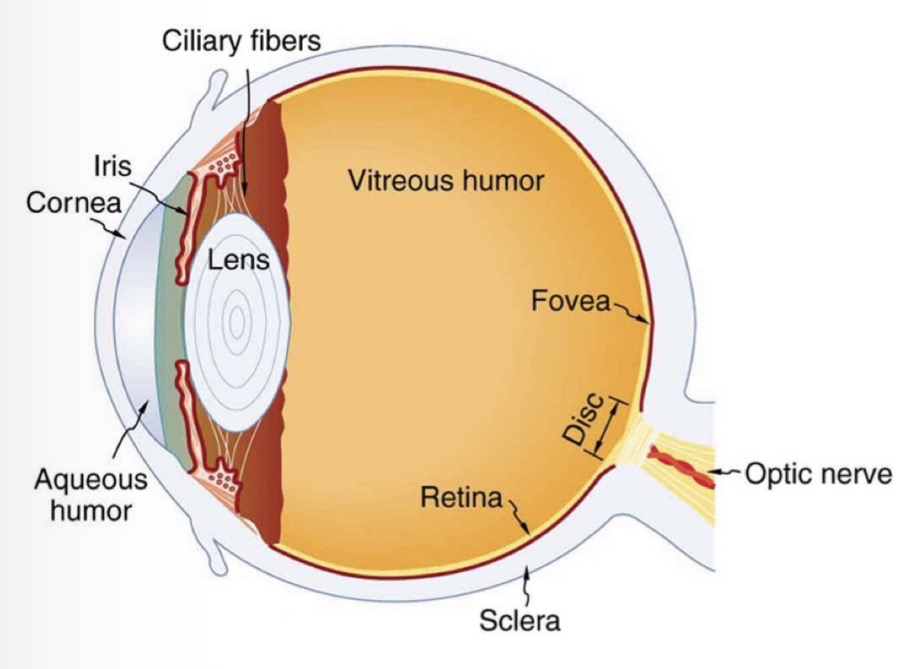
2 chambers of the eye
Anterior chamber » front of the eye
Posterior chamber » back of the eye
Anterior Chamber
Structures in the anterior chamber of the eye
Sclera
Cornea
Iris
Lens
Aqueous humour
Anterior Chamber
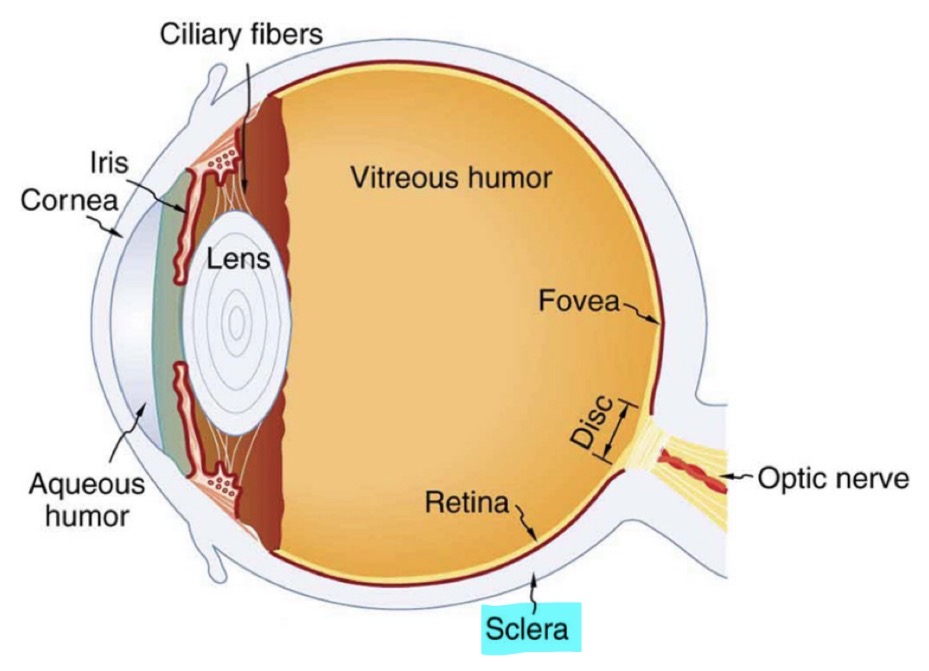
Sclera
‘White of the eye’
Protective function
Made up of non-uniform collagen and elastic fibres
Extraoccular muscles are attached to the eye via the sclera
Anterior Chamber
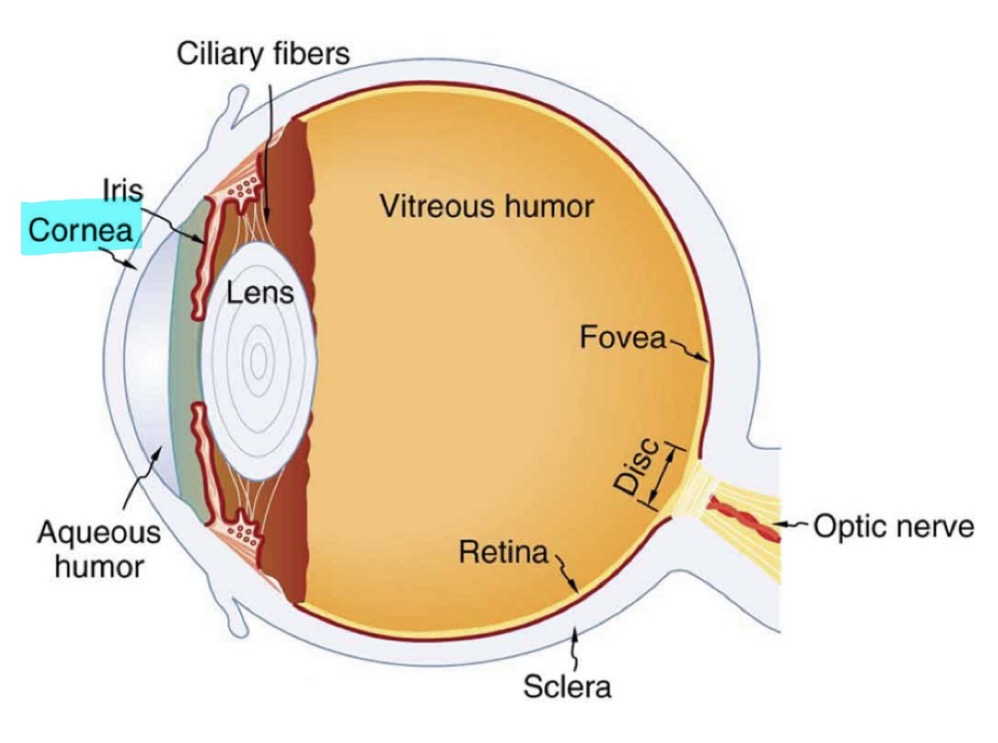
Cornea
Continuous with the sclera
Transparent with no blood vessels
Major refractive structure of the eye - bends light entering the eye
Responsible for 2/3 of the eye’s total refractive power
Anterior Chamber
Cornea
Why does the cornea refract light when it enters the eye
Light changes direction when it moves from one medium to another as it changes speed
Anterior Chamber
Cornea
Even thought it accounts for most of the eye’s focusing power, the corneas focus is fixed. Why is this?
The corneas focus is fixed because the cornea cannot change its shape
Therefore, it cannot change its refractive power
Anterior Chamber
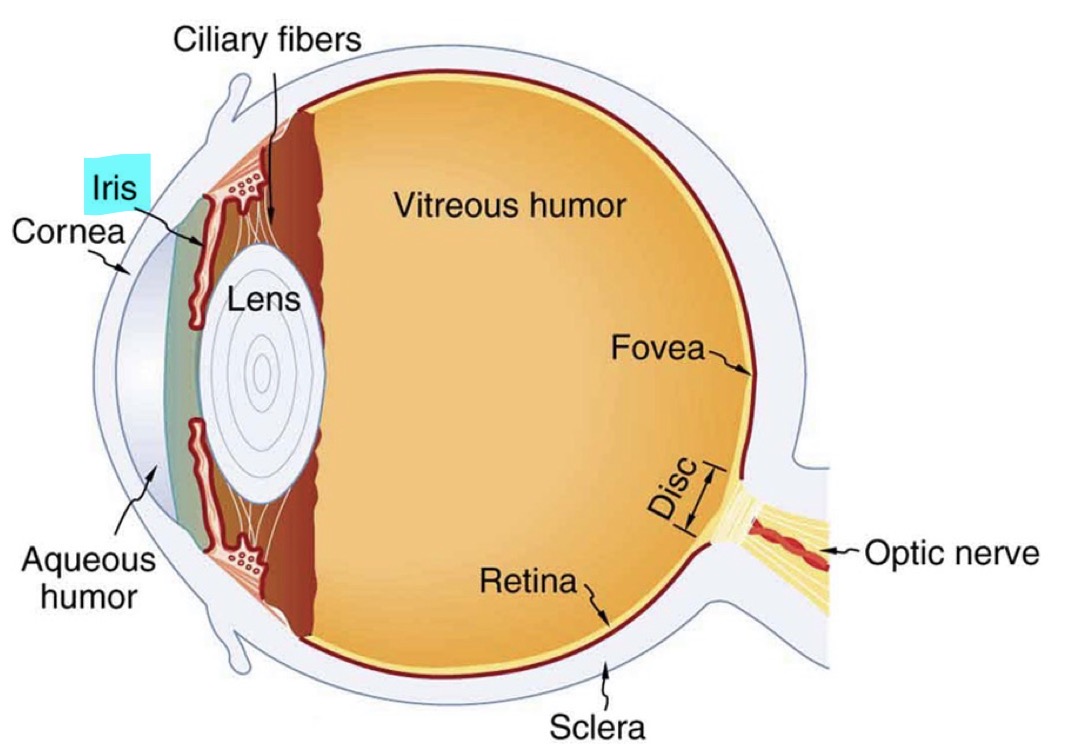
Iris
Gives the eye colour » depending on melanin content
Controls light levels in the eye via the pupil
The iris contains 2 muscles which control pupil size ;
Sphincter muscle
Around the edge of the pupil
Bright light causes the sphincter muscle to contract causing the pupil to constrict
Dilator muscle
Run through the iris radially (like spokes on a wheel)
Dim lighting causes the dilator muscle to contract causing the pupil to dilate
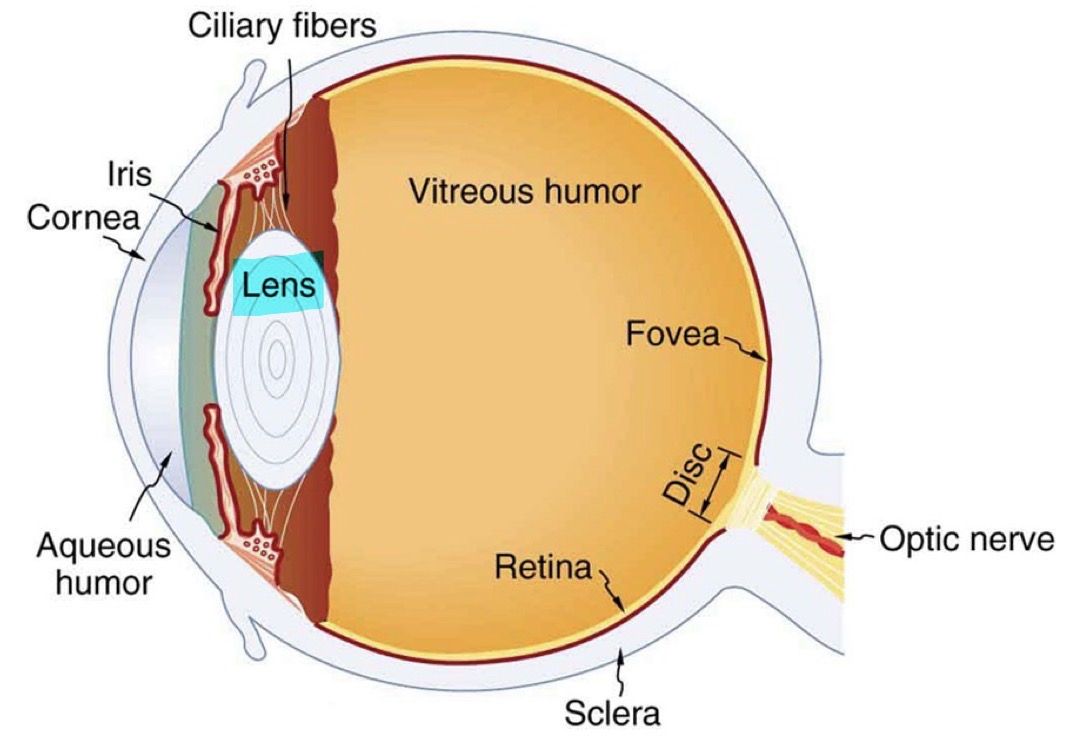
Anterior Chamber
Lens
Transparent
Biconvex structure - 2 outward-curving surfaces
Refracts light to focus it on the retina
Makes up the remaining 1/3 of the total refractive power of the eye
Unlike with the cornea, the focus is not fixed
This is because the lens can change shape to focus on images at various distances - accommodation
Anterior Chamber
Lens
How does the lens change shape
The ciliary muscles relax and contract, causing the lens to become thicker or thinner
Anterior Chamber
Lens
Shape of the lens when object is closer
Lens is thicker as needs to bend light more
Anterior Chamber
Lens
Shape of the lens when object is further away
Lens is thinner as doesn’t need to bend light as much
Anterior Chamber
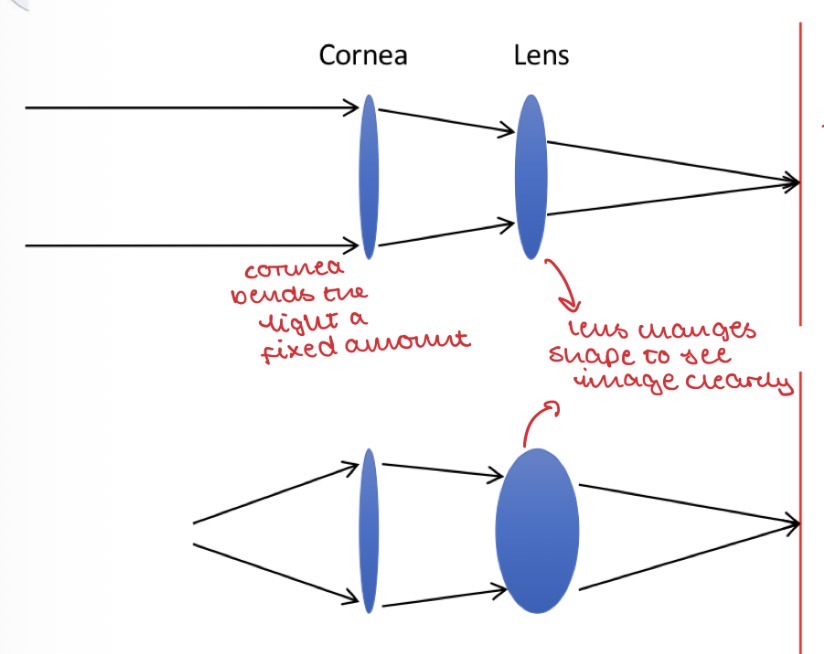
Summary of the refraction of the light by the cornea and lens
Both refract light entering the eye
The cornea makes up 2/3 of the eyes total refractive power, the lens makes up 1/3
When light enters the eye, the cornea bends the light a fixed amount (as it is unable to change shape)
The lens then changes shape to focus the light on the retina » allows us to see the image more clearly
So both work together to refract light to focus it on the retina
Anterior Chamber
Aqueous humour
Clear, watery fluid that is bordered by the cornea and the lens
Similar to the blood plasma but has a low concentration of proteins
Provides nutrients to the cornea and lens
Gives the eye shape
Maintains the intraocular pressure
Anterior Chamber
Aqueous humour
Production and drainage of aqueous humour AKA how does aqueous humour end up in the anterior chamber?
Aqueous humour is continuously produced and drained:
It is secreted from the epithelial cells of the ciliary body behind the iris
It migrates into the anterior chamber by flowing between the iris and the lens
At the same time as the aqueous humour is being produced, it is being drained:
It is drained through the pores of the trabecular meshwork
It passes into the Canal of Schlemm, then into veins of the orbit via the episcleral vein
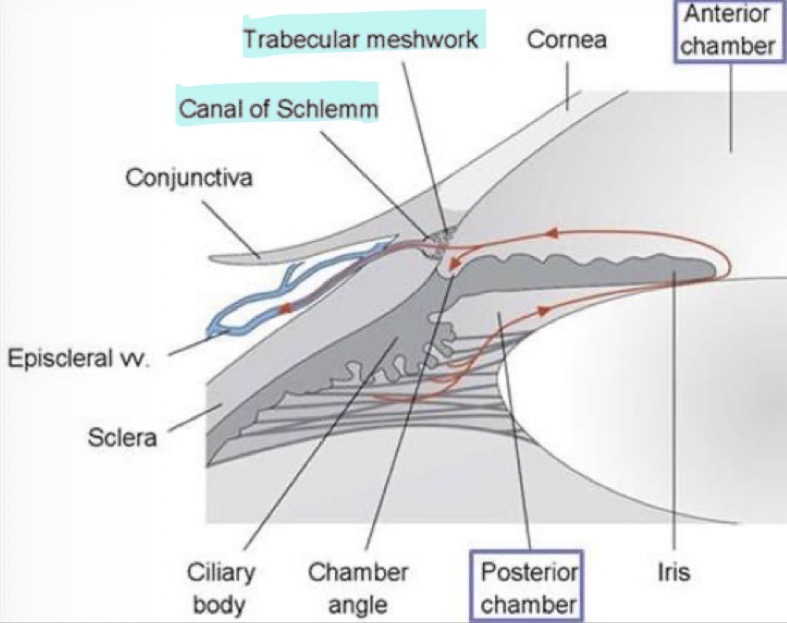
Anterior Chamber
Aqueous humour
What happens if there are problems with production or drainage of aqueous humour?
This will change intraocular pressure:
If production > drainage = fluid builds up = IOP rises
If production < drainage = fluid is drained faster than it is made = IOP drops
Intraocular pressure is only stable when production = drainage
Posterior Chamber
Structures in the posterior chamber of the eye
Vitreous humour
Retina
Posterior Chamber
Vitreous humour
Bordered by the lens and the retina
More gelatinous than the aqueous humour - made of water and collagen
Not continuously produced and drained like aqueous humour - it is stagnant
Helps maintain eye structure at the back of the eye and pushes retina back in place
Posterior Chamber
Vitreous humour
What happens to the vitreous humour with age?
The electrostatic forces that keep the collagen fibres apart diminish
So the vitreous humour becomes more watery
This causes it to move away from the retina
Posterior Chamber
Retina
Light-sensitive tissue that lines the back of the eye
Covers 65% of the interior surface of the eye
Contains rods and cones - photosensitive cells which convert light into signals that are carried to the brain by the optic nerve
Rods function in dim light and provide black and white vision
Cones function in the daytime and provide colour vision
Posterior Chamber
Retina
By looking at the retina, how can doctors see if there are any problems with the CNS?
The retina is the only part of the CNS that can be seen externally
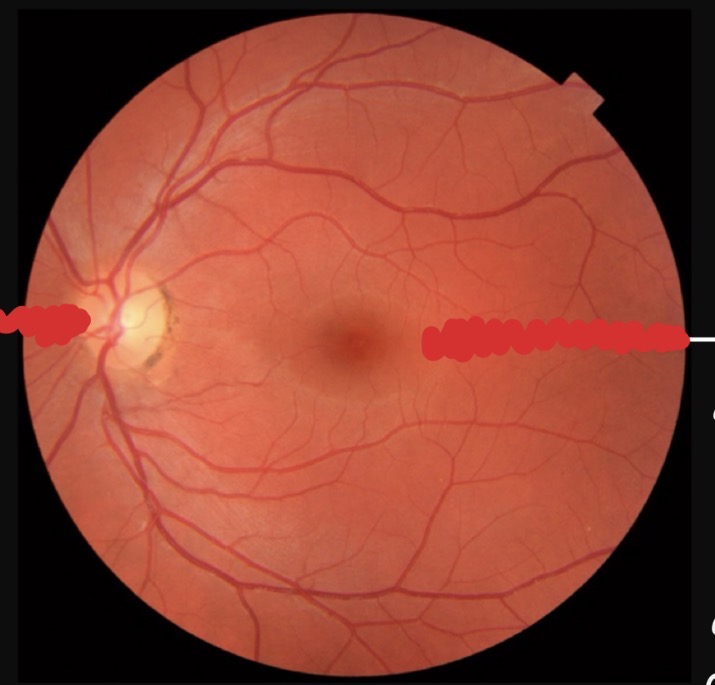
Posterior Chamber
Retina
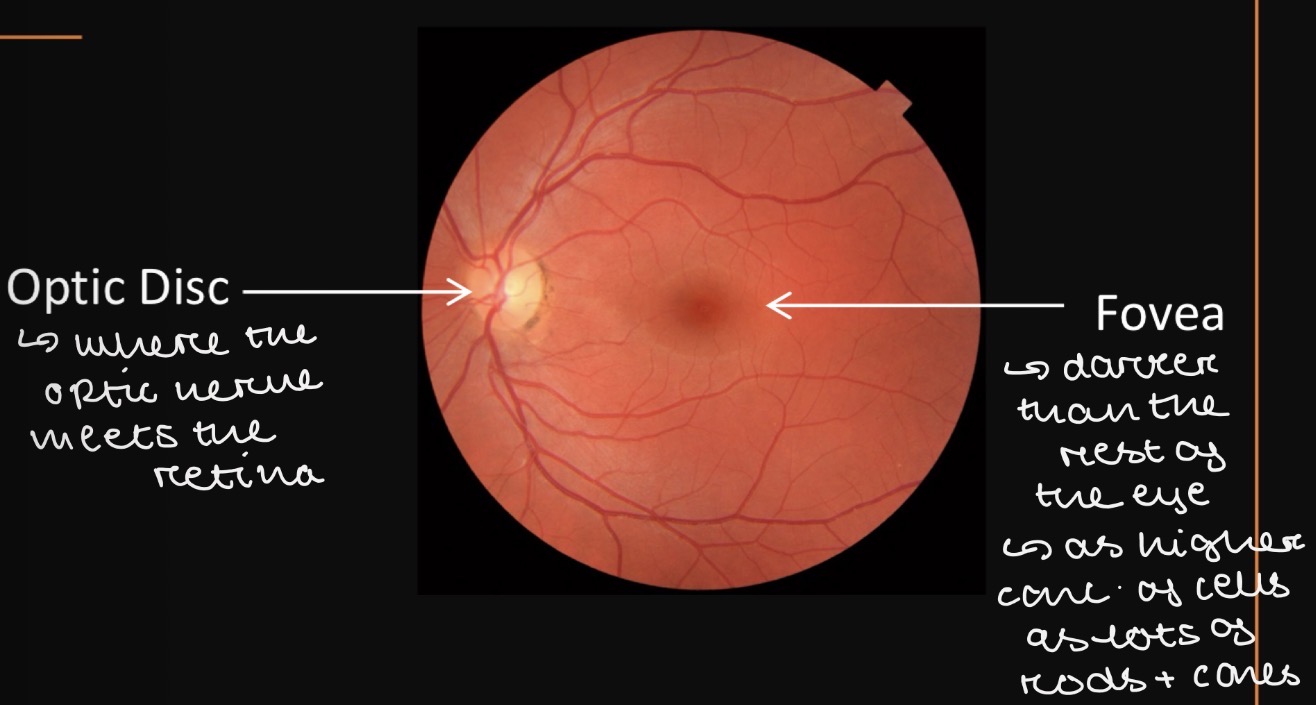
Label the optic disc and the fovea and describe their function
Optic disc » where the optic nerve meets the retina
Fovea » darker than the rest of the retina as high concentration of rod and cone cells
Drainage systems of the eye
Aqueous humour » drains into the systemic uveoscleral circulation
Aqueous humour » drains into the trabecular meshwork then the Schlemm’s canal
Vitreous humour » drains via diffusion into the anterior chamber
Posterior route » movement of fluid from the retina across the blood-retinal barrier into the choroid circulation
Drug pathways in the eye
Trans-corneal route
Transport across the cornea
Most common route to aqueous humour
Blood-retinal barrier
Drugs can cross the BRB to reach the retina
The BRB prevents drugs/toxins in the blood from entering the posterior eye » so difficult for drugs to enter
Intravitreal delivery route
Injection into the vitreous humour
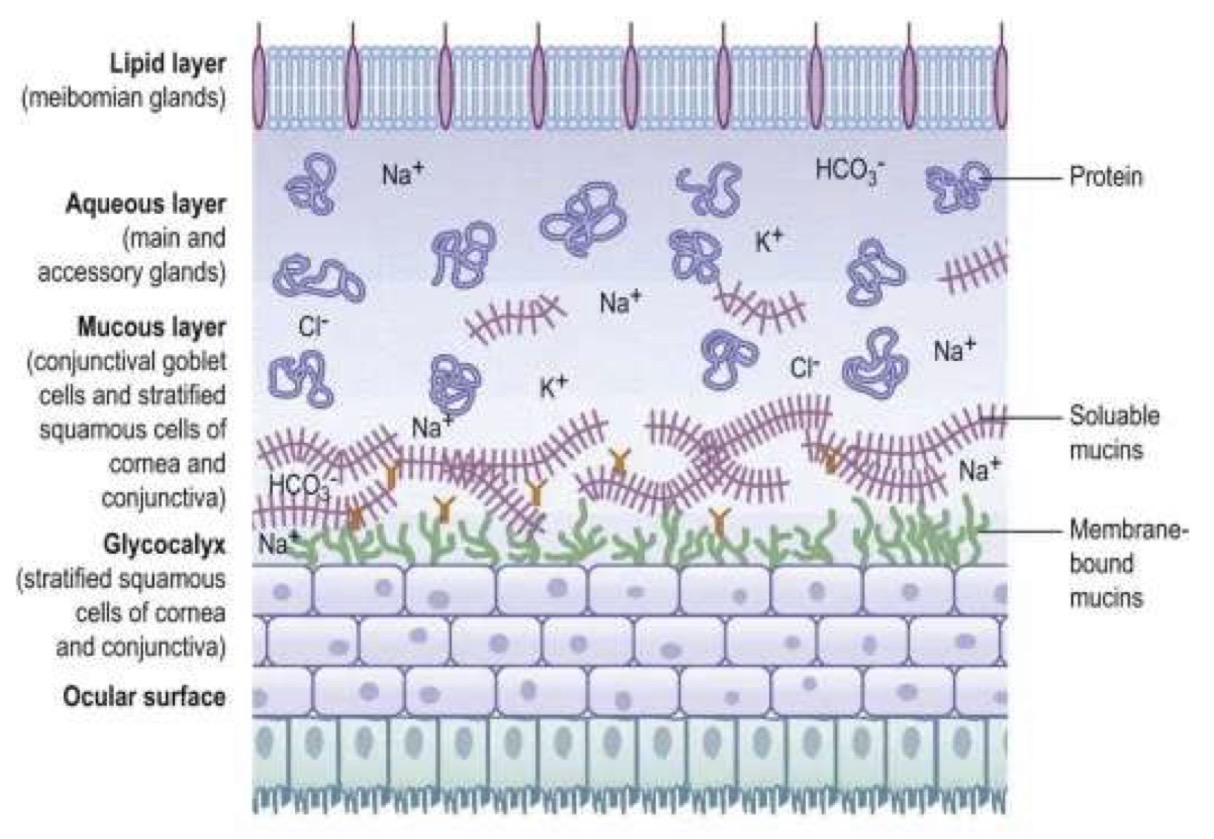
Tear Film
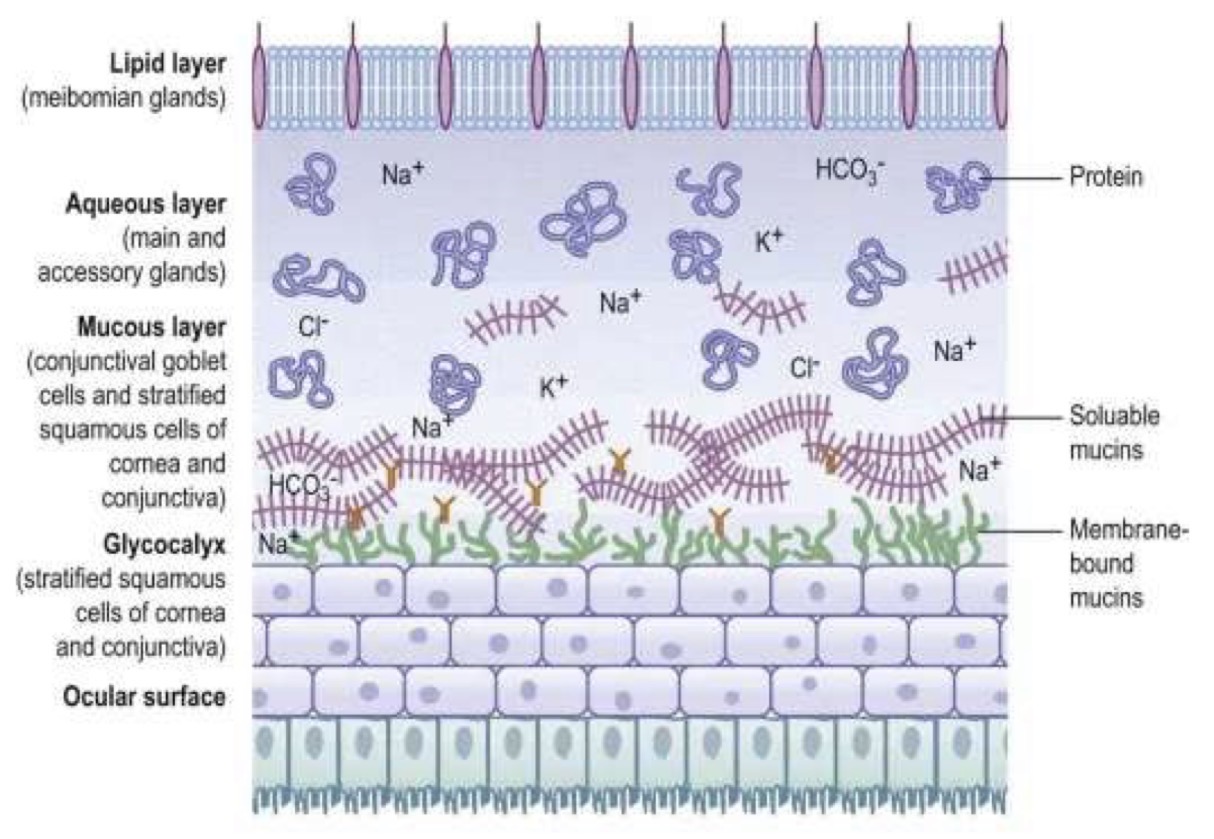
What are the 3 main layers of the tear film?
Lipid layer
Muco-aqueous (aqueous layer)
Mucous layer + Glycocalyx
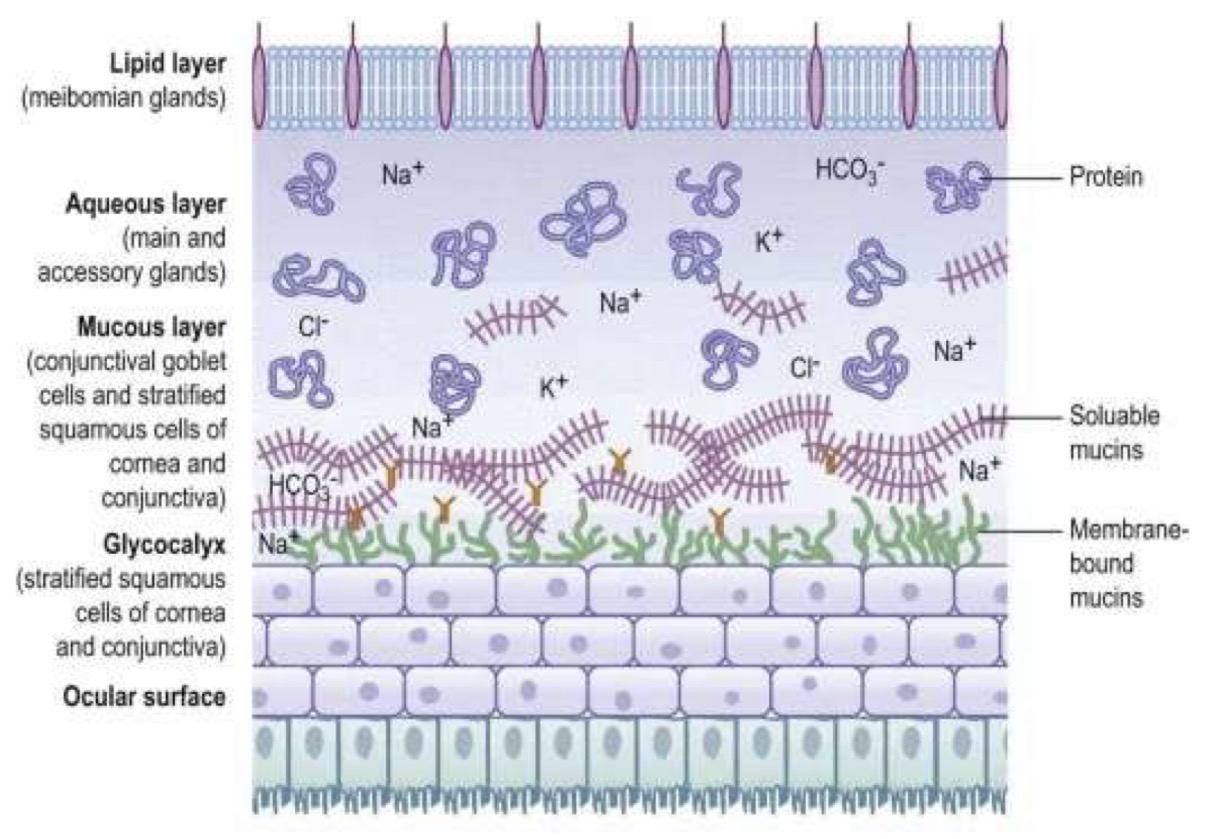
Tear Film
Which glands produce the lipid layer of the tear film?
What is the lipid layer composed of?
What is the main function of the lipid layer?
Produced by: Meibomian glands located in the eyelids
Composed of: sterol esters, waxes and fatty acids
Functions: The lipid layer reduces water evaporation from the surface of the eye
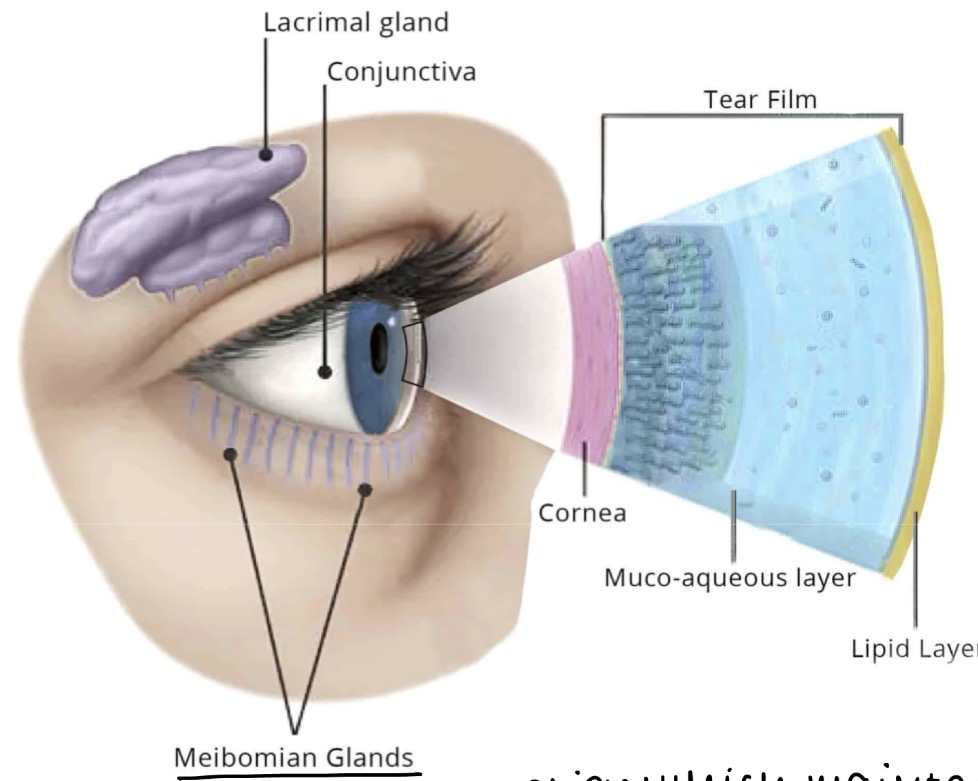
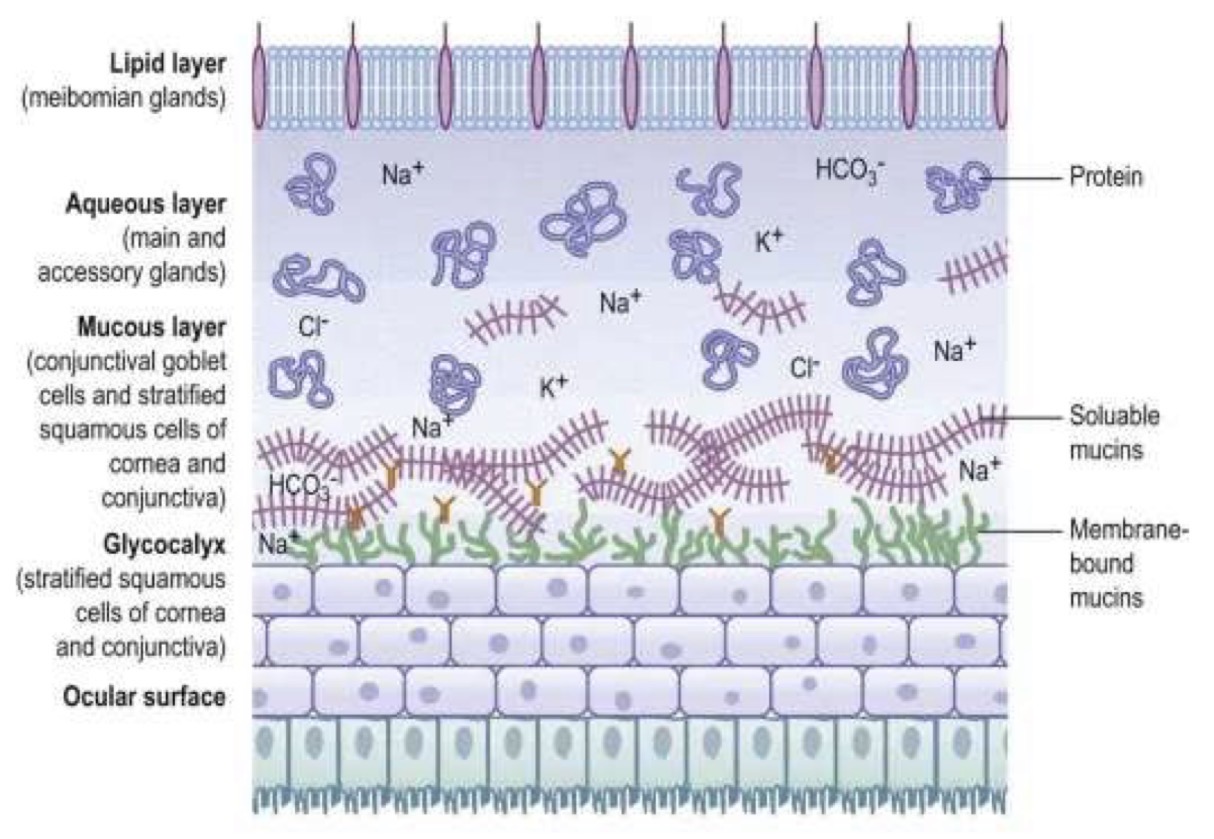
Tear Film
What produces the aqueous layer of the tear film?
What is the aqueous layer composed of?
Produced by: The lacrimal gland and accessory glands
Composed of:
Dissolved ions e.g HCO3-, Na+, K+, Cl-
Proteins
Lubricants
Soluble mucins produced by goblet cells
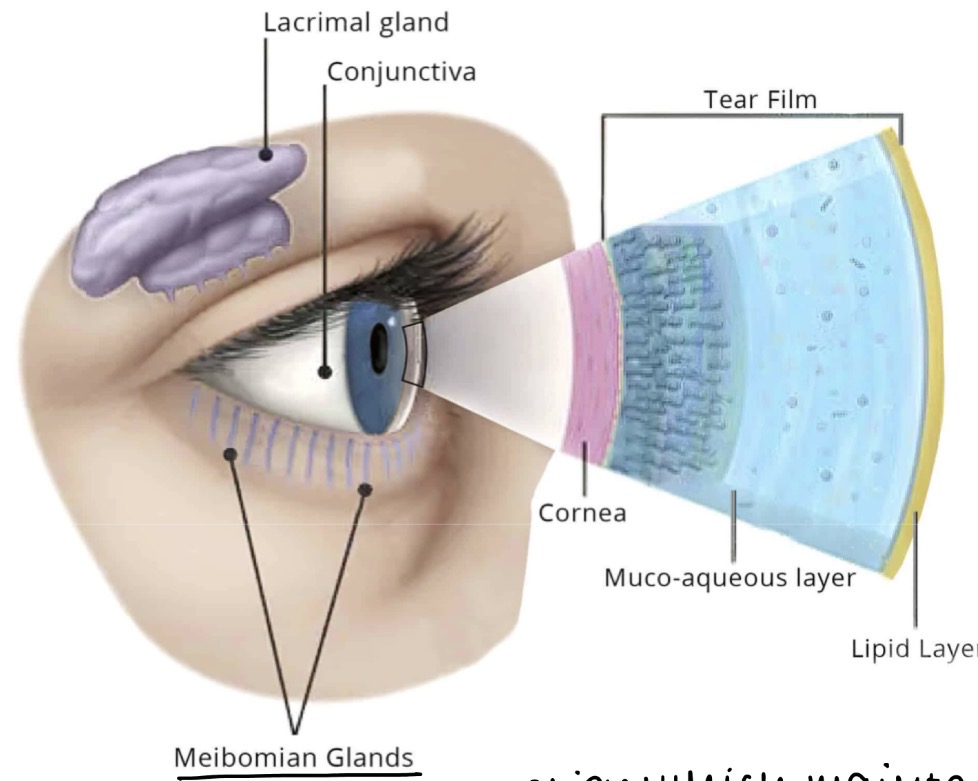
Tear Film
What do the lacrimal glands secrete that make up the bulk of the aqueous layer of the tear film?
the lacrimal fluid (tear fluid)
Tear Film
What is the average viscosity of lacrimal fluid and what contributes to it?
About 3cp
The protein content of lacrimal fluid increases its viscosity
Tear Fluid
What type of fluid is lacrimal fluid in terms of Rheology and what does this mean?
Pseudoplastic (shear-thinning)
As force is applied, viscosity decreases, allowing the lacrimal fluid to spread more easily over the surface of the eye
Tear Film
What produces the mucus layer in the tear film
What is the function of the mucus layer?
Produced by: Conjunctival goblet cells
Function: stabilises the tear film and helps maintain a slippery surface on the eye
Tear Film
What is the glycocalyx and where is it located?
A layer of membrane-bound mucins
Located on stratified squamous cells of the cornea and conjunctiva
Why are tears considered a major barrier in ocular drug delivery?
Because they cause significant pre-corneal drug loss
This reduces the amount of drug available for corneal absorption
What are the 2 main causes of pre-corneal drug loss?
Tear turnover and drainage
Systemic absorption via the nasolacrimal duct
How does tear turnover reduce drug concentration?
causes dilution of the drug as fresh tears continuously replace the tear film
What is the normal tear volume of the eye?
7 uL
What is the tear turnover rate?
1.2 uL/min
What is the maximum volume the tear film can hold?
What is the typical volume of one eye drop?
Why does this mean that most of an eye drop ends up on the cheek?
Max volume of tear film: 30uL
Volume of eye drop: 50uL
Tear volume is already 7uL
So tear volume + eye drop volume = 57uL
This exceeds the maximum tear film volume of 30uL leading to overflow and drainage
How much tear fluid is displaced with each blink?
about 10uL
Why does blinking increase drug loss?
Blinking spreads and clears out 10uL of tear fluid
This pushes excess volume into drainage pathways
In addition to just falling down your cheek, what happens to excess tear volume in the eye?
Cleared by the naso-lacrimal apparatus
Role of the nasolacrimal duct?
drains tears into the nose
What triggers drainage through the nasolacrimal apparatus?
a reflex reaction to excess tear volume
Where do tears drained by the nasolacrimal duct ultimately go?
into the GI tract after passing through the nose
Why can you sometimes taste eye drops
The drug drains through the nasolacrimal duct
Into the nose
Then into the GI tract
This allows it to reach taste receptors
What is a clinical implication of drainage of drug-containing tears into the GI tract?
Potential systemic absorption of the drug
What is the most significant barrier to ocular drug administration?
the cornea
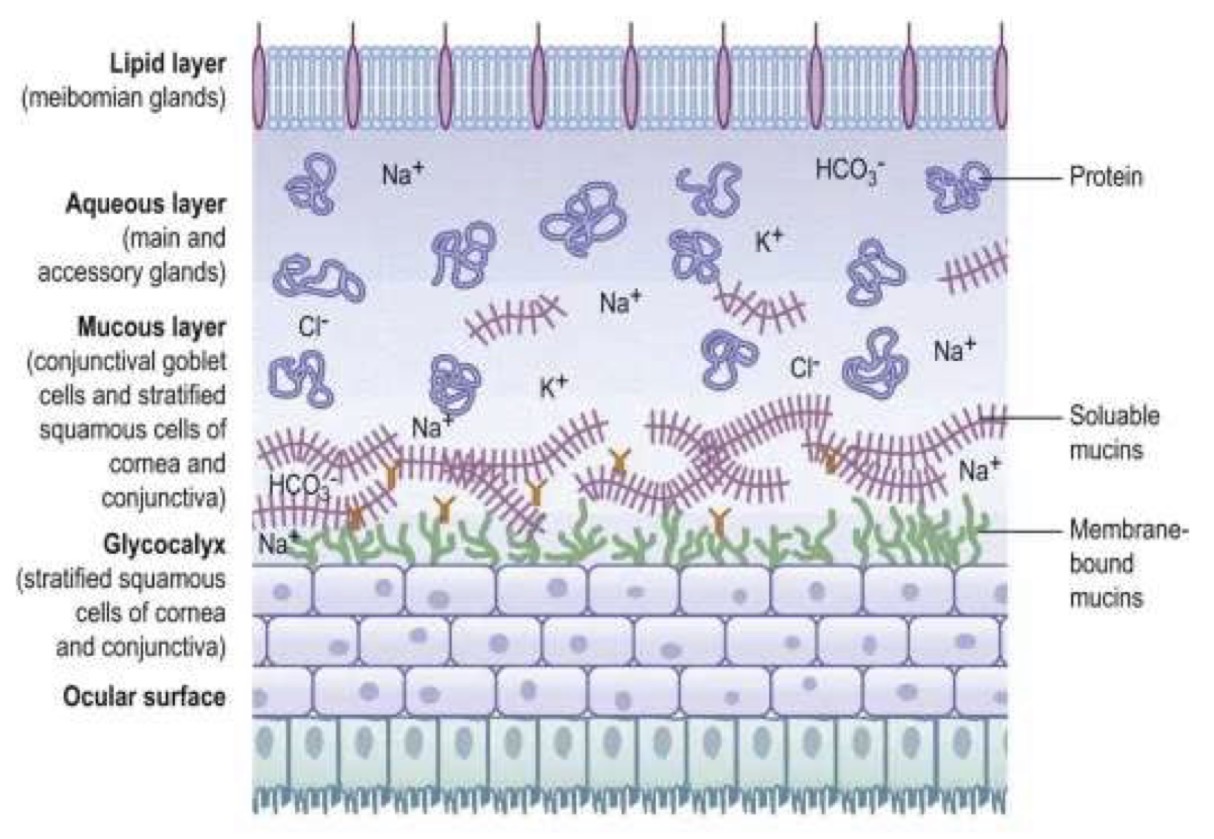
Structures of the Cornea
Describe the structures of the cornea
Epithelium
5 - 6 layers
500 - 100um
Hydrophobic barrier
Bowman’s membrane layer
8 - 12um irreplaceable collagen layer
Acts as a basement layer for the epithelium
Unlike the Descemet’s membrane, is not regenerative
Stroma
Provides most of the corneal thickness (90%)
80% water, 20% collagen + polysaccharides
Descemet’s Membrane
6um
High tensile strength
Regenerative » repairs itself if damaged
Endothelium
Regulates stromal hydration
Supplies nutrients
Structures of the Cornea
What may happen if the surface of the cornea is scratched?
Bowman’s membrane unable to regenerate
Scar tissue may form
Causes blurred vision
How does the cornea act as a barrier?
Epithelium
Barrier to water (hydrophobic), microbes and xenobiotics - prevents them from entering the eye through tight junctions
Tight junctions
Very restrictive
Prevents tear fluid from penetrating the cornea » this maintains osmotic pressure
Pros and ons of topical ocular delivery
Pros:
Convenient route
By-passes 1st pass metabolism
Cons:
Very inefficient - only 1-5% of the total dose reaches the aqueous humour
What are the 3 main barriers that reduce drug permeation in topical ocular delivery?
Nasolacrimal drainage
Conjunctival absorption into systemic circulation
Corneal barrier
Ocular Metabolism
What phases of metabolism occur in ocular tissue?
Where does metabolism occur?
What enzymes are involved
Both Phase I and Phase II metabolism occur in ocular tissue
Occurs in:
Ciliary body
Most active in the Retinal Pigment Epithelium (RPE)
Enzymes:
Esterases are abundant
However, weak expression of CYP450s
Prodrugs
What is a prodrug
an inactive form of a drug which becomes activated when metabolised in the body
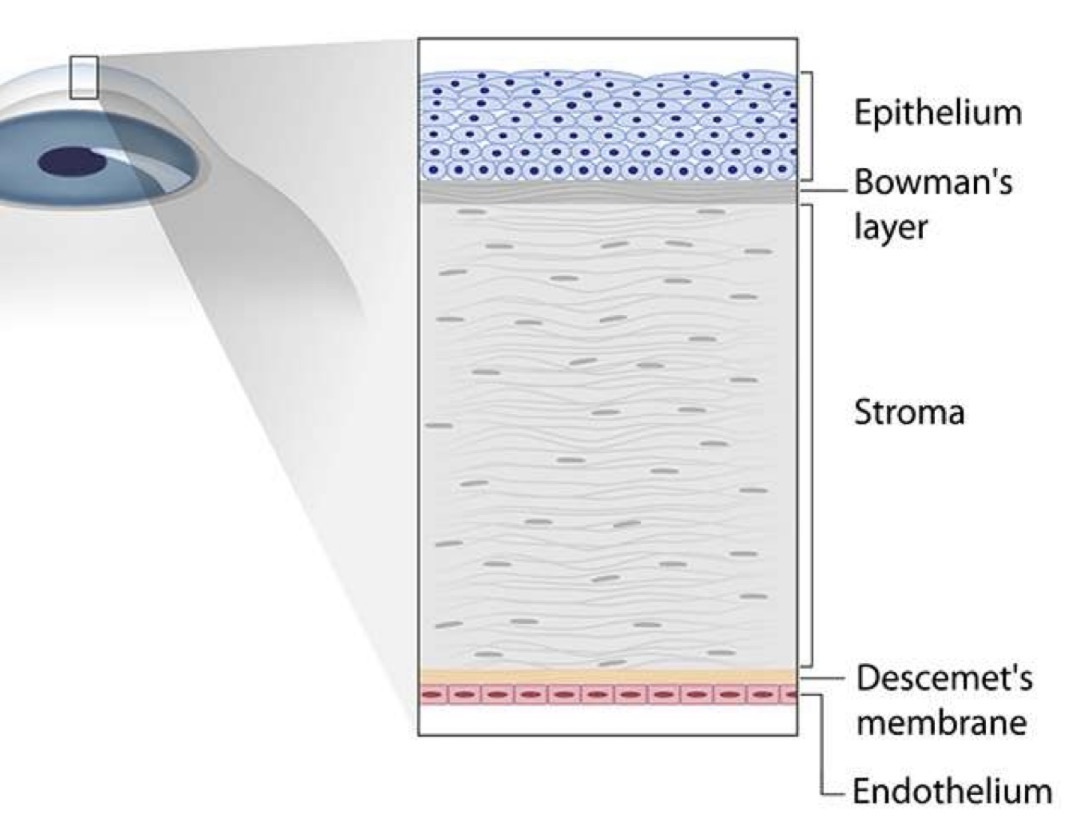
Prodrugs
Why might prodrugs be used in ocular drug delivery?
If formulation cannot improve delivery, the development of a prodrug is used as a last resort to improve delivery
Prodrugs
Major drawback of creating a prodrug
The prodrug form of a drug is a new chemical entity
Therefore, there are regulatory hurdles » must demonstrate safety and efficacy of thee new molecule
Prodrugs
Why do free acids show low corneal permeation at ocular pH?
because they are ionised = so less lipophilic
Prodrugs
How do esters improve drug delivery for corneal permeation?
Increase lipophilicity » so able to enter corneal epithelium
They are cleaved by esterases once inside the eye
Prodrugs
What is an example of a prodrug used in ocular delivery?
Latanoprost » an isopropyl ester of free acid
The addition of the isopropyl group makes it much better at getting into the eye as the polar COOH is masked
This makes it more lipophilic = able to enter corneal epithelium
Prodrugs
What antiviral drugs are available as amino acid prodrugs?
Acyclovir
Ganciclovir
Prodrugs
How do anti-viral amino acid prodrugs enhance corneal uptake?
via the PEPT transporters expressed in the corneal epithelium
Prodrugs
What products are currently in development for prodrug ocular delivery?
Antiviral drugs e.g. ganciclovir, acyclovir
Available as amino acid prodrugs which enhance uptake into the cornea via PEPT transporters
What are the 2 main methods for drug absorption in the eye?
Conjuctival / scleral route (ie. The white of the eye)
Corneal absorption route
Where do we want the drug to be absorbed into?
the anterior chamber
Is the conjunctival / scleral route a good choice for targeting the anterior chamber?
Not really
Poor choice for targeting the anterior chamber (AC)
Instead, it gets absorbed into the SYSTEMIC CIRCULATION
Which route is the best for targeting the anterior chamber?
Corneal absorption route
Corneal Absorption Route
What is the primary barrier in the corneal absorption route?
corneal epithelium
Corneal Absorption Route
What is the lifespan of the corneal epithelium?
7 - 10 day lifespan
Corneal Absorption Route
What are the 3 transport routes across the corneal epithelium?
Paracellular (between cells)
Transcellular (through cells)
Active transport
Corneal Absorption Route
How do the different layers of the cornea affect the absorption of the drug:
Epithelium
Stromal layer
Endothelium
Corneal epithelium
Rate-limiting barrier as:
Hydrophilic drugs cannot easily pass through the corneal epithelium
Drug molecules must be <=1nm to get through the tight junctions
If the corneal epithelium is infected or damaged, this can increase permeability
Stromal layer
Higher permeability
Can slow down lipophilic drugs because they dont dissolve well in the water-rich stroma
Corneal endothelium
Single layer
High permeability
Corneal Absorption Route
What do we have to consider to ensure the drug is able to permeate the layers of the cornea?
Molecular size
Diffusion coefficient
LogP
Corneal Absorption Route
How does molecule size affect corneal absorption?
larger molecules cross cell membranes more slowly than smaller molecules
Corneal Absorption Route
What is the paracelllar pathway in the cornea like?
Restrictive - limits the passage of substances between cells
Corneal Absorption Route
How does the diffusion coefficient affect corneal absorption?
A reduced diffusion coefficient slows the diffusion of larger molecules
Corneal Absorption Route
How are some polar molecules absorbed quickly across the cornea?
active uptake transporters facilitate the fast transport of certain polar molecules
Corneal Absorption Route
What logP range was found optimal for beta blocker corneal permeation?
logP 2 - 3
Higher logP values = unable to pass through the stroma (too lipophilic to dissolve well)
Lower logP values = unable to pass through the epithelium
Blood-retinal barrier
What is it and what is its function?
Protects the retina by preventing drugs in the systemic circulation from entering the eye
Blood-retinal barrier
What structures make up the blood-retinal barrier?
Outer retinal pigment epithelium
Inner endothelium of retinal vessels
Blood-retinal barrier
How do tight junctions in the BRB affect drug transport?
Restrictive - prevent hydrophilic drugs from passing through
Blood-retinal barrier
What transporters exist in the BRB and what do they do?
Efflux transporters e.g. P-glycoprotein » protect the retina from toxins
Uptake transporters e.g. glucose, amino acid transporters » bring in nutrients
Blood-retinal barrier
How does the BRB make systemic delivery of drugs to the retina difficult?
the BRB restricts drug entry and expresses protective efflux transporters
What other ocular route of administration is send when topical delivery is not possible?
Intravitreous injection » however, only used in a hospital setting
Types of formulations for the eye
Liquids
Solutions
Suspensions / emulsions
Semi-solids
Ointments
Gels
Ocular Solutions
Advantages
Cheapest
Easiest to manufacture
Drug is already dissolved so no dissolution step = faster corneal permeation = faster onset
Ocular Solutions
Disadvantages
Have the shortest residence time » thin and less viscous so drained from the eye quickly
Ocular Solutions
What are ocular solutions commonly used for?
Anaesthetics
Diagnostics
Pre-operative drugs like mydriatrics
Ocular Solutions
Which muscarinic antagonist used in ocular solutions causes mydriasis and ciliary muscle paralysis
cyclopentolate
Ocular Solutions
Which Sympathomimetic in ocular solutions is used to induce mydriasis?
Phenylephrine
What formulation can be used to improve the short residence time of ocular solutions?
Ocular suspensions
Ocular Suspensions
Why are some drugs formulated as ocular suspensions instead of solutions?
because they have low aqueous solubility and cannot be dissolved into a solution
Ocular Suspensions
Where do suspended particles collect after administration of an ocular suspensions?
in the ocular cul-de-sac between the eyelid and the eyeball
Ocular Suspensions
How do ocular suspensions provide sustained drug delivery?
The particles collect in the cul-de-sac between the eyelid and the eyeball
The suspended particles gradually dissolve to deliver the drug over a period of time