Microbio: HIV Life-Cycle
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
what does HIV stand for
human immunodeficiency virus
what is HIV the causative agent for
AIDs (Acquired Immune Deficiency Syndrome)
currently #2 infectious disease killer by a single infecious agent
AIDS
how many people were living with HIV in 2009
33.3 million people world wide
Infection time course of someone infected with HIV/AIDs
Primary Infection: When someone is initially infected, they have high levels of CD4+ T-cells.
CD4+ T-cells number dips due to a rise in the HIV virus RNA .(all of this occurs within a few weeks of getting the infection)
After this DIP in CD4+ T-cells, and rise in HIV virus RNA, at some point, CD4+ T-cells will stabilize & HIV levels will go down and the patient can go into clinical latency at this point which can last for years.
What can Happen after Primary Infection?
During this time the HIV RNA copies per ml.
Plasma drastically increase leading to acute HIV syndrome with wide dissemination of the virus with it seeding in the lymphoid organs.
This also reaches a period of clinical latency which develops into constitutional symptoms, then diseases attacks the body, ultimately leading to death of the individual.
Cell count with AIDS
With AIDS, CD4+ cell count drops to less than 200 cells/ml
The time to death after progression to AIDS is less than 10 months
Clinical Latency
No AIDS, No symptoms, have HIV but immune system is still functioning.
Viral count is low
Can still pass on disease without knowing
Constitutional Symptoms
Virus reactivates
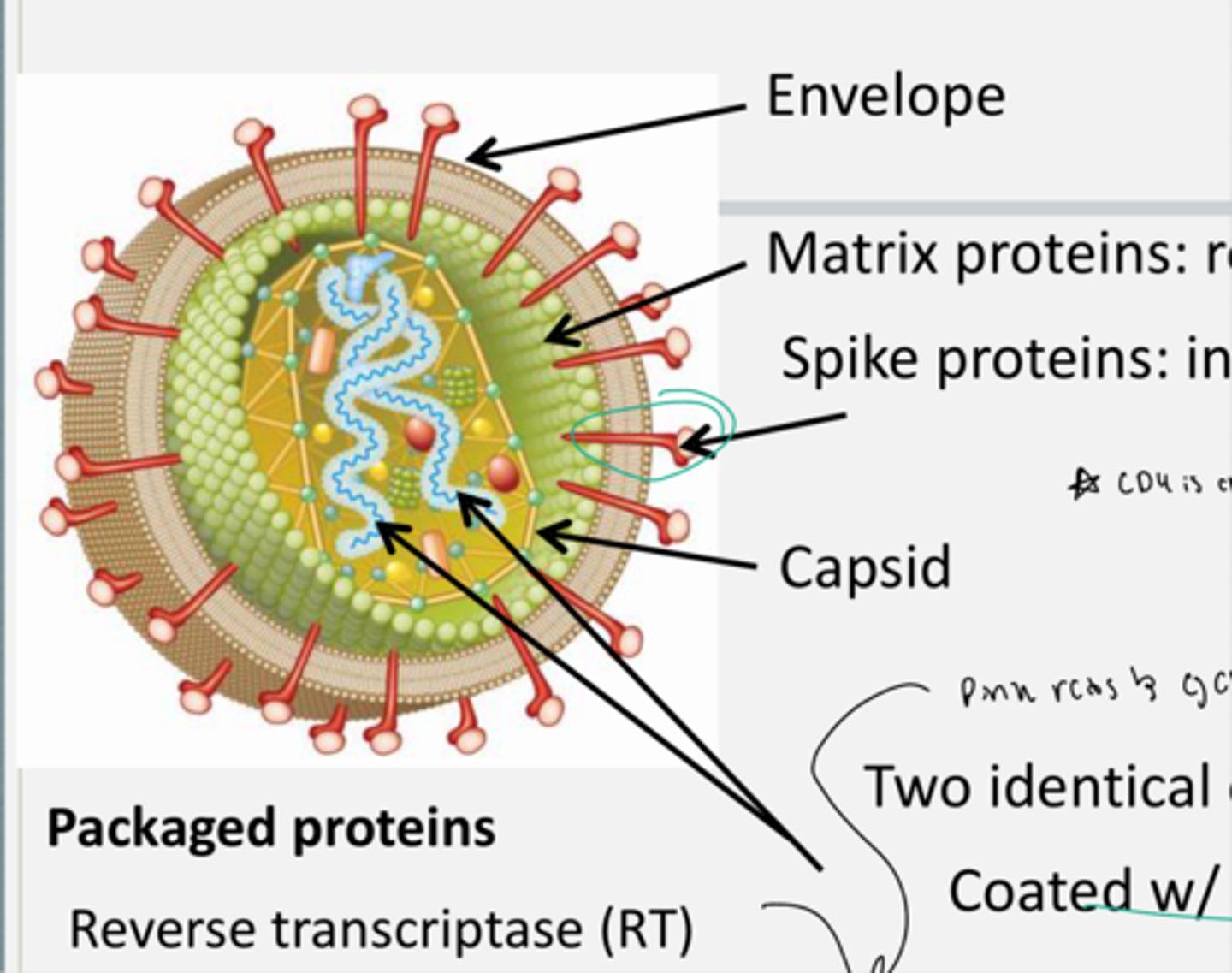
Structure of the HIV virus
HIV virus is enveloped.
It contains Matrix proteins: that reinforce the envelope & strengthen it. Not founf in all viruses
It contains Spike proteins: that interact with the host cell.
It also contains Capsid proteins: encases RNA+Genome.
Its genetic material is in the form of two identical copies of (+) RNA coated with proteins.
it also contains other packaged proteins including a reverse transcriptase (RT), integrase (IN), protease (PR), and additional accessory proteins all of which are needed at certain points in the HIV life cycle.
Structure of the HIV genome
HIV ___ consists of 2 identical copies of + RNA
It contains two LTR (long terminal repeat) regions that circles the genes coding for proteins in the HIV genome.
Within the genome there are
Gag genes: which are transcribed into capsid proteins.
Polymerase(pol) genes: which encodes reverse transcriptase, integrase, and protease.
Envelope(Env) genes: which encode envelope proteins like the spike proteins TM and SU.
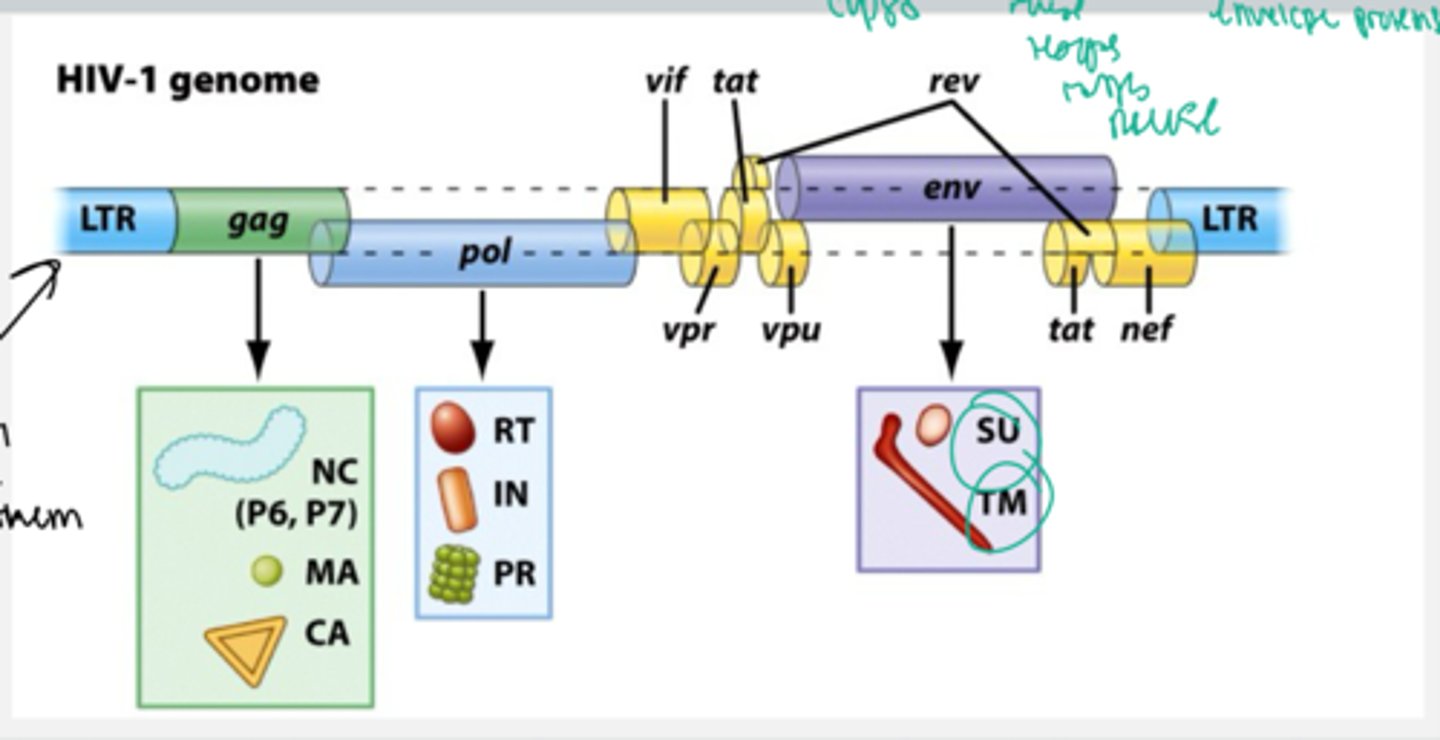
Alternative splicing
___ in the genome expresses accessory proteins which assist in infection (ex. Tat - activates transcription of the viral genome)
Viral proteins translation in the HIV genome
____transcribed/ translated as long polypeptides
Proteases will come and cleave the individual proteins post-translationally into individual proteins from the long polypeptide/cleaves into individual enzymes
thus this is one of the targets in the treatment of HIV
HIV infection between bacteria and mammals
Eukaryotic cells have 1 start and 1 stop codon so they do not have polycistronic mRNA like bacterial cells, thus HIV can only infect mammalian cells. (the CD4+ white blood cells of mammals)
Bacterial cells have polycistronic mRNA so they are not infected by HIV.
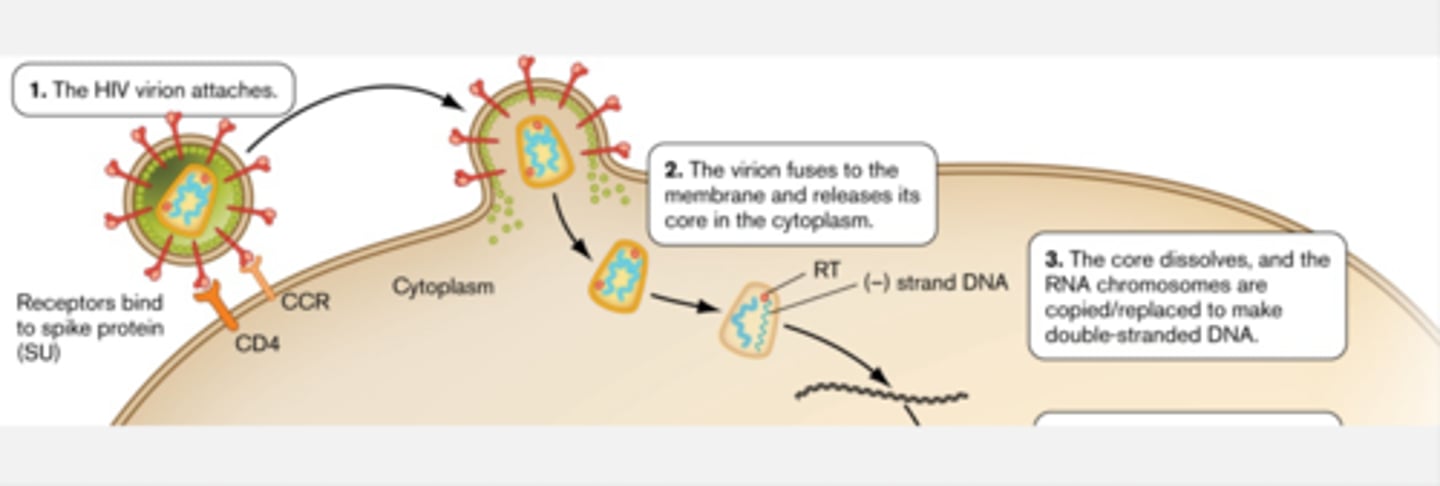
HIV attachment?
The envelope (Env) region of the HIV virus encodes the spike proteins which include TM (transmembrane subunit) and SU (surface subunit).
The viral cell contains the SU and TM as well as a fusion peptide attached to the TM in the viral cell on the cell membrane surface.
The host cell (CD4 white blood cells) contains membrane, the CD4 receptor, and the chemokine receptor CCR5 (co-receptor, but there are different types of co-receptors this is just one type)
HIV spike proteins bind CD4 receptor and chemokine co-receptor. TM subunit goes through conf. change and interacts with host cell mem. through fusion protein. SU subunit interacts with CCR5 and CD4 receptors. All of this allows fusion with host cell.
HIV binds the CD4 receptor together with the chemokine receptor CCR5. CD4 is found on CD4+ T cells (aka helper T cells) of the immune system
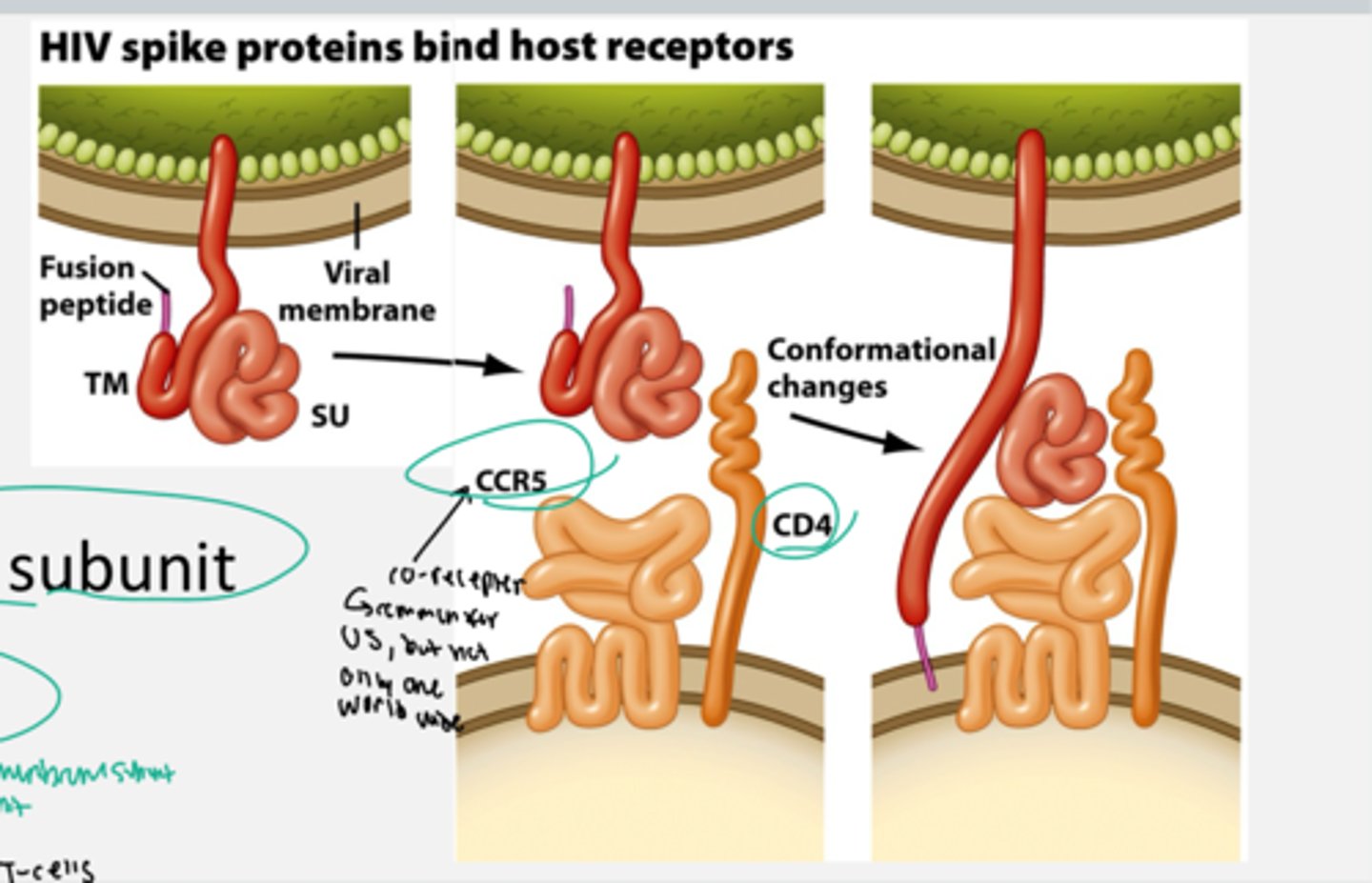
HIV entry into the host cell
The envelope and host membrane fuse together and the HIV core directly enters the cytoplasm of the host cell. HIV core then dissolves and releases its contents.
1. HIV virion attaches: the CD4 and CCR5 receptors on the host cell bind the spike proteins(TM & SU) on HIV
2. The Virion fuses to the membrane and releases its core containing the two identical + RNA copies as well as the other packaged proteins like reverse transcriptase, protease, integrase, and others.
when this happens reverse transcriptase will reverse transcribe a - double stranded strand of DNA from the + strand RNA and releases this strand into the host cell cytoplasm.
3. The core dissolves and the RNA chromosomes are copied/replaced to make double-stranded DNA
HIV Resistance
Individuals who lack a functional CCR5 co-receptor are naturally immune to HIV because the virus cannot enter their cells.
These individuals have a mutated allele that has a 32 bp deletion.The CCR5 delta 32 mutation (deletion). With this deletion, individuals do not make functional CCR5 co-receptors so HIV cannot bind to the CCR5.
In individuals without the mutation, they have one functional copies of CCR5 in each strand of their DNA (2 copies total) = HIV can attach and enter (will produce many CCR5 receptors present on their cell membrane).
In individuals who are heterozygous for the mutation (contain one functional copy and one copy of the CCR5-delta 32 mutation), HIV can still enter, but this will be a delayed process. So they have 1 copy of the mutated allele, so HIV can still get in their cells. But, they will have a delay in the progression of the HIV infection in their body. will only produce a few CCR5 receptors (1 for example)
Individuals who are homozygous for the CCR5 delta 32 deletion mutation do not produce functional CCR5 receptors (thus there are no CCR5 receptors on their cell membrane) and the virus cannot enter their cells.
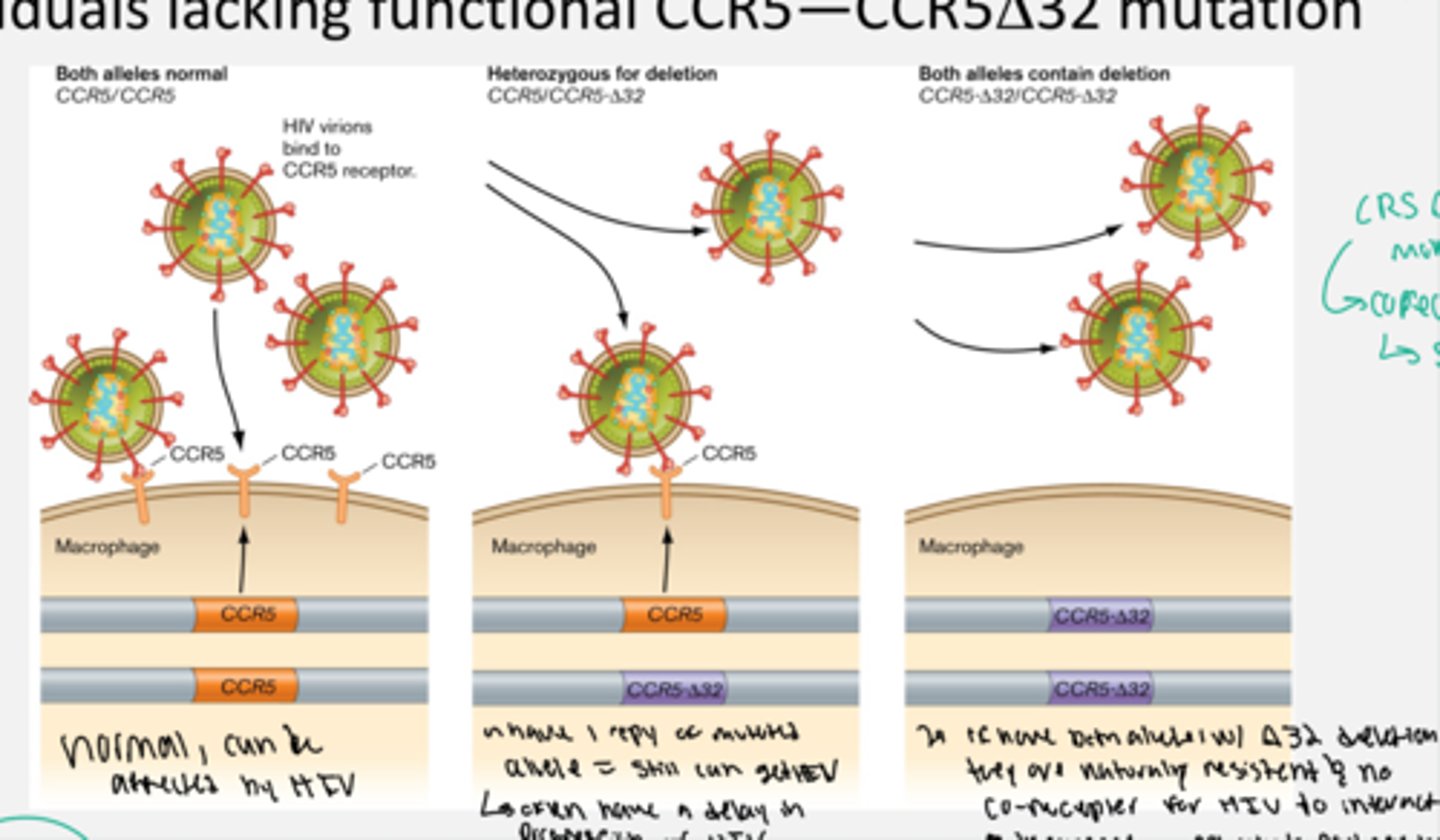
How was the CCR5 delta 32 mutation discovered
Individuals whose partners had HIV and they were exposed via sexual intercourse but the person with the homozygous mutation never got infected because they had the delta 32 mutation
Is CCR5 the only co-receptor for HIV
No, CCR5 is not the only co-receptor for HIV. some HIV strains recognize the CXCR3 receptor instead so people infected with this strain will not be immune.
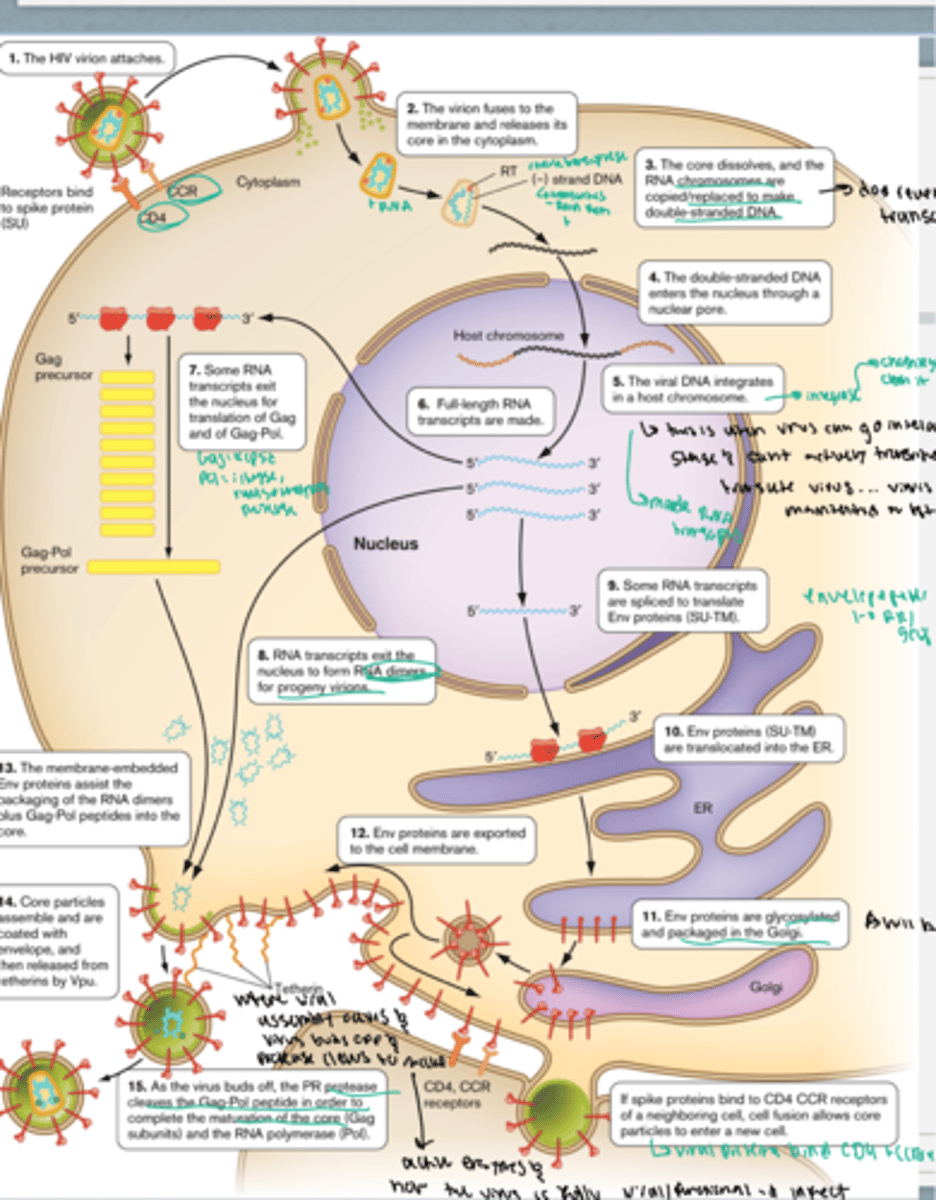
Explain the HIV lifecycle
1. the HIV virion attaches and enters into the host cell by binding with the CD4 and CCR5 receptors with the spike proteins of the virus
2. The virion fuses with the membrane and releases its core into the cytoplasm.
3. The core dissolves and the RNA chromosomes are copied/replaced to make double-stranded DNA using viral reverse transcriptase (transcribes + sense mRNA into double stranded - DNA.
4. The double stranded DNA enters the host nucleus via a nuclear pore.
5. The viral genome uses integrase to integrate itself into the host chromosome. at this point, the virus can go into the latent stage(will end at some point) and cannot actively transcribe or translate the virus. the virus is just maintained in the host genome but is not active.
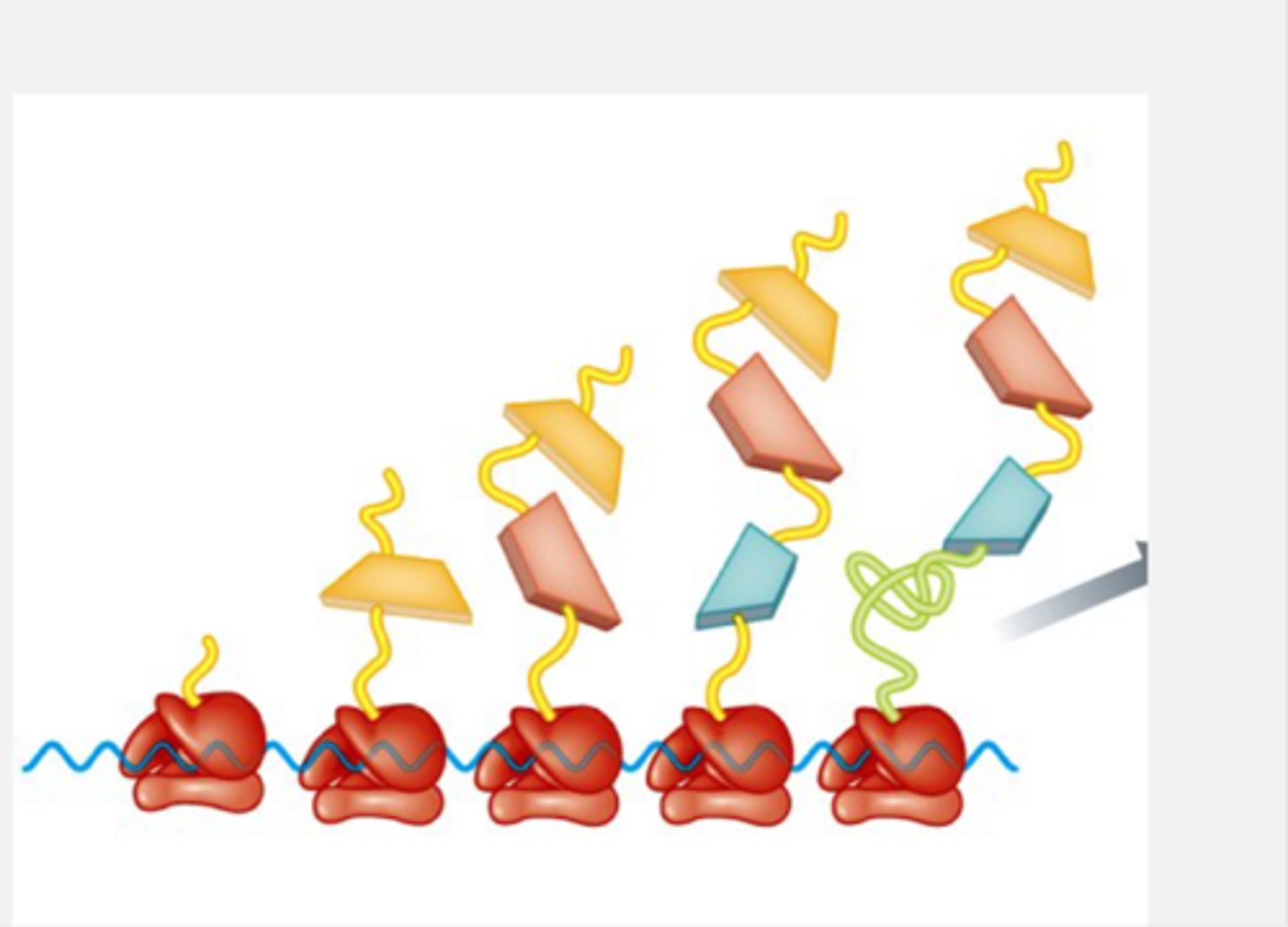
6. Now the full-length RNA transcripts of the host infected DNA are made in the 5' to 3' direction using host RNA polymerase. At this point, the new viral mRNA can take a few different pathways:
- Some RNA transcripts exit the nucleus for translation in the cytoplasm by ribosomes to make the Gag and Gag-Pol proteins.
- Some RNA transcripts exit the nucleus to form RNA dimers for progeny virions(to form new viral proteins)
- Some RNA transcripts are spliced to translate Env proteins (SU-TM) by ribosomes in the cytoplasm. The Env proteins (SU-TM) are translocated into the ER. Then the env proteins are glycosylated and packaged in the Golgi. They are then exported to the cell membrane.
13. Then all of these proteins come together: The membrane embedded Env proteins assist the packaging of the RNA dimers plus Gag-Pol peptides into the core.
14. The core particles assemble and are coated with envelope, and then released from tetherins by Vpu.
15. as the virus buds off, the PR protease cleaves the Gag-Pol peptide in order to complete the maturation of the core (Gag subunits) and the RNA polymerase (Pol).
Why can we develop treatments against HIV
- Because we understand the life-cycle, we have developed effective anti-HIV drugs
What was the first HIV treatment
AZT = the first effective anti-HIV drug
When was AZT developed?
The drug was developed in 1987. First effective treatment. It was originally developed as a potential anti-cancer drug.
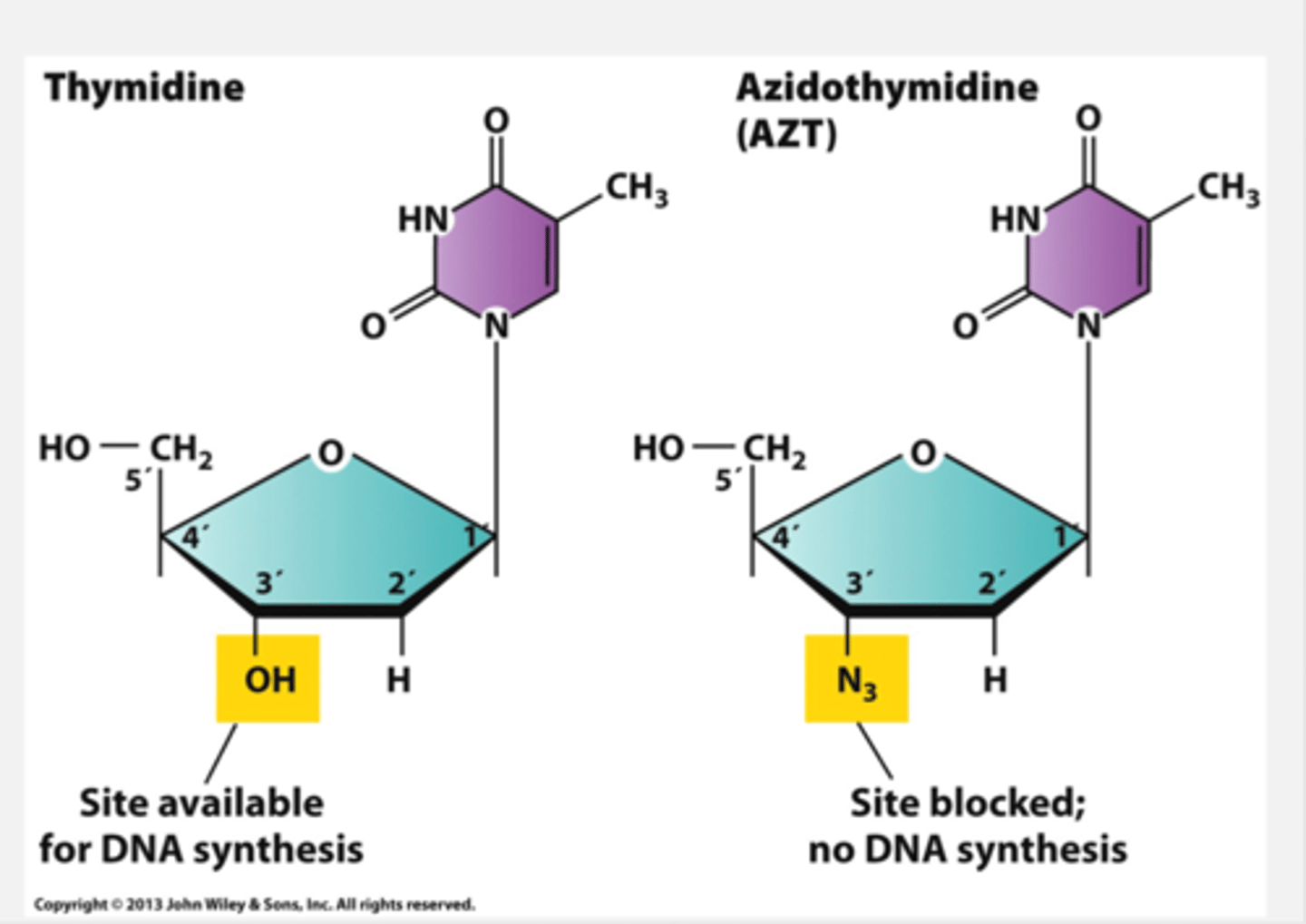
How does AZT work?
The way the medicine works is that human DNA polymerase is more selective than reverse transcriptase found in HIV. So most, but not all of the time it can distinguish AZT from thymidine. Therefore, AZT isn't lethal to us but can have serious side effects because human DNA polymerase can distinguish AZT from thymidine.
On thymidine there is an OH group at the 3' carbon which is available for DNA synthesis. however on AZT, there is an N3 group so the site is blocked at the 3' carbon and no DNA synthesis is possible.
From 1981 - 1987 what were the rates of HIV/AIDs cases and fatalities before AZT was invented.
Cases and fatalities doubled roughly every year
What is the problem with the AZT monotherapy treatment
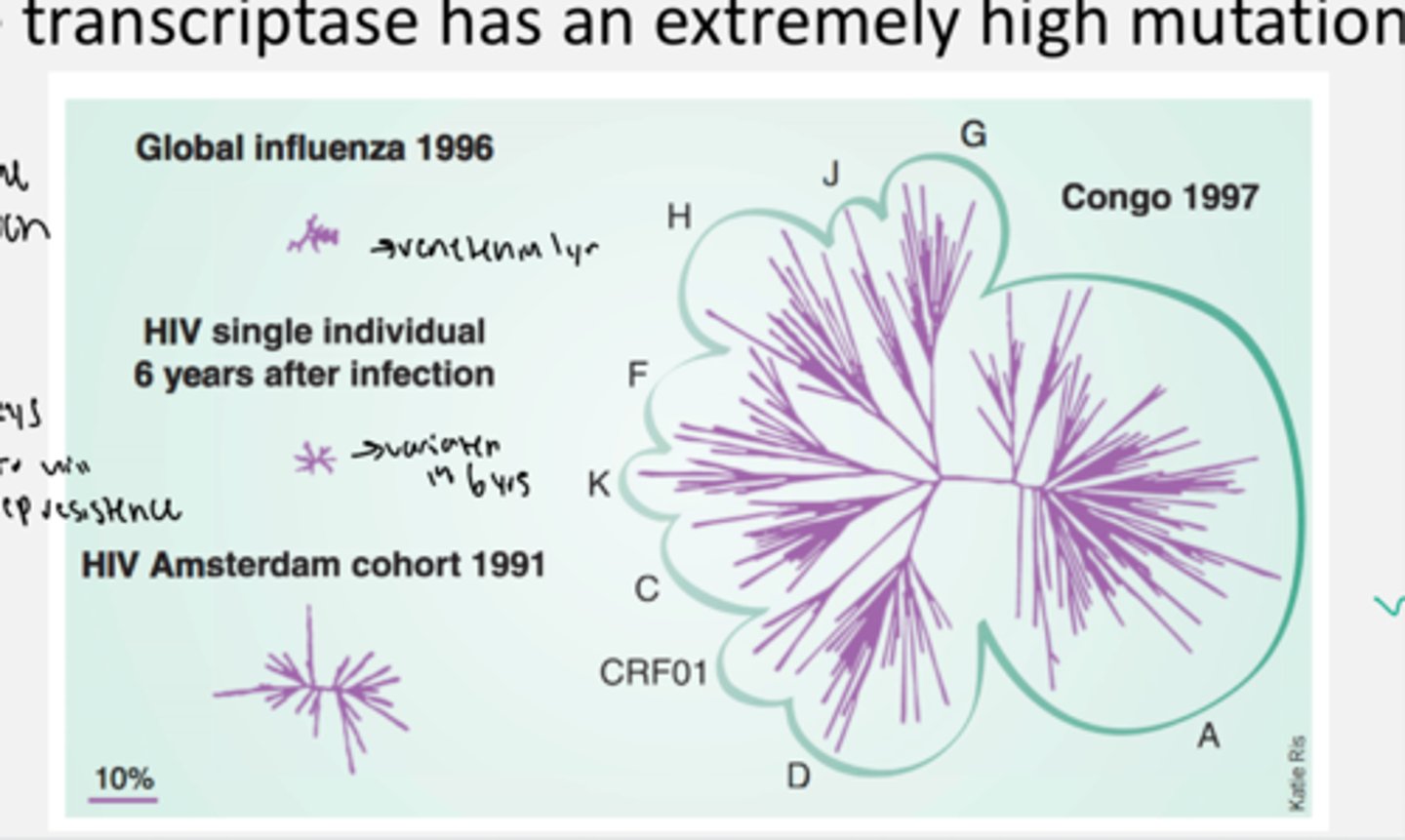
Reverse transcriptase (RT) has an extremely high mutation rate. So, HIV became resistant to AZT very quickly (spoke length on diagram shows the degree of divergence from OG infection).
- High mutation rate also makes developing a vaccine very difficult
What is the new/more effective treatment for HIV
HAART: Highly active antiretroviral therapy
- There are drugs included that inhibit multiple steps of the HIV life cycle
- Triple combination or cocktail therapy
- This makes it more difficult for HIV to become simultaneously resistant to 3 different drugs
it includes protease inhibitors (prevents the virus from cleaving), inludes integrase inhibitors which prevent it from integrating into hist genome, includes reverse trasncirpatse inhibtors so it cannot make - DS DNA from + RNA in the viral genome. It also includes fusion/entry inhibitors that do not lets it attach to the cell/integrate.
How did HAART transform HIV infections
HIV transformed into a treatable, chronic disease in wealthy countries. So in poorer countries the life expectancy with aids was still decreased 20 and 40 year olds dying
what are some problems with the HAART treatment
- There are severe side effects in some patients (ex. diabetes, pancreatitis, lipidystrophy, lactic acidosis, diarrhea)
- Drug resistant HIV strains
In these strains you must optimize treatment and HIV replication is not always completely repressed
- The treatment is expensive and requires complicated medical care (about 20,000 per person/year)
Is HAART a cure
NO HAART is not a cure for HIV. Life-long therapy is required with this drug and viral levels will quickly rebound if the therapy is stopped. So HIV is in the body forever so HAART is needed forever.
Has there been any successful cures for HIV?
Timothy Ray Brown (aka the Berlin patient) was the first and only adult cured of HIV.
- he was HIV positive when he was diagnosed with leukemia
- he had a bone marrow transplant from an individual who was homozygous for the CCR5 delta 32 mutation which cured him. the patient has never had to use HAART since before the trasnplant and has no detectable levels of HIV.