Common Maternal Complications
1/50
Earn XP
Description and Tags
Vocabulary-style flashcards covering definitions and key concepts from the lecture notes on postpartum hemorrhage and hypertensive disorders in pregnancy.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
Postpartum hemorrhage (PPH)
Excessive bleeding after birth. ACOG defines it as cumulative blood loss >1,000 mL or with signs of hypovolemia; vaginal delivery normal blood loss is <500 mL, but bleeding of any amount can be PPH.
early vs late post partum hemorrhage
early is within 24
late is 24-48 hours
Four Ts (causes of PPH)
Tone (uterine atony) (the uterus is boggy) THE MOST COMMON ISSUE
Trauma (lacerations hematomas, inversion, rupture)
Tissue (retained placenta or invasive placenta)
Thrombin (coagulopathies)
what do you do with the blood
quantify it (to keep track of blood loss)
1ml of blood is 1gram of weight
keep even wet gauze
Uterine atony
Lack of uterine muscle tone leading to heavy postpartum bleeding; the primary and most common cause of PPH.
BIG BOGGY UTERUS
what causes the uterus to end up boggy or struggle to tighten back up
big baby
more than 1 baby pregnancy
too much amniotic fluid
infection of the amniotic fluid or uterus
prolonged labor
retained placenta
more than 4 vaginal births
episiotomy
hematoma
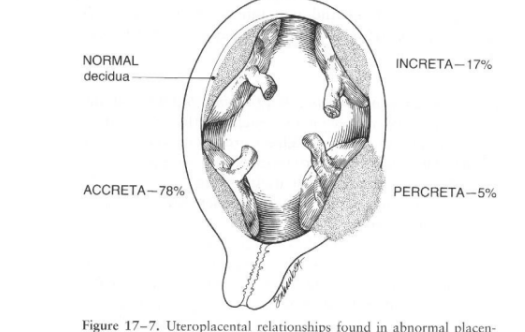
Tissue (in the context of PPH)
Retained placental tissue or placenta accreta / increta/ percreta causing ongoing bleeding.
Thrombin (coagulopathy)
Disorders of coagulation that contribute to PPH (bleeding due to impaired clotting).
Risk factor: magnesium sulfate
Magnesium therapy in preeclampsia can contribute to uterine atony and bleeding risk.
Risk factor: coagulopathy
Bleeding disorder that worsens postpartum hemorrhage.
Risk factor: cesarean birth (urgent/emergent)
Cesarean delivery increases risk of PPH compared with vaginal birth.
Risk factor: uterine inversion
Turned inside out uterus after delivery; a cause of heavy bleeding requiring immediate management.
Assessment finding of post partum hemorhage: lochia
Postpartum uterine bleeding discharge; monitor for color, amount, and clots
the clots bigger than a quarter
Assessment finding: Systemic
Tachycardia: Elevated heart rate that may accompany hemorrhage.
Hypotension: Low blood pressure indicating possible shock from bleeding.
Oliguria: Low urine output, a sign of reduced perfusion in hemorrhage.
Cool clammy skin
post partum hemorrhage secondary signs
womens bodies have so much blood that systemic signs such as low blood pressure would not show up till things get really bad
Blood loss thresholds (PPH signs)
1000 mL: significant hemorrhage by ACOG criteria;
higher volumes correlate with worsening clinical signs (e.g., 1500–2500+ mL associated with progressive shock).
subinvolution
• Delayed return of enlarged puerperal corpus to normal size and function
• Common with secondary or late PPH
•Causes
• Retained placenta
• Infection
• Malposition
• Myomas
• Gestational trophoblastic disease
symptoms of subinvolution
• Pelvic discomfort or backache
• Bleeding from an enlarged, boggy, tender uterus
• Lochia does not change from rubra
meidcation for early PPH
Pitocin: 0-40 U in 500/1000 ml crystalloid IV, or 10 units IM
Methergine: can not give to people with hypertension (meth gives you hypertension)
Hemabate: Can not give to people with asthma, they get mad crazy diarrhea as a side effect
Cytotec for ealy PPH
800-100mcg rectally to control hemorrhage and stimulate uterine contractions.
Tranexamic acid (TXA) for early PPH
• Helps decrease blood loss by maintaining blood clots and
preventing the breakdown of fibrin
• 1 gm loading dose of IV TXA over 10 minutes (1 mL/min) upon
diagnosis of excessive blood loss
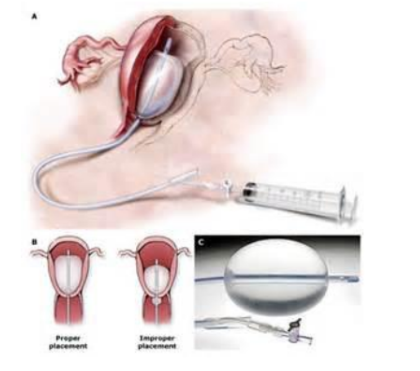
Bakri balloon
Intrauterine balloon tamponade device used to control postpartum hemorrhage; commonly filled with normal saline (e.g., 500 mL) to apply internal pressure and stop bleeding
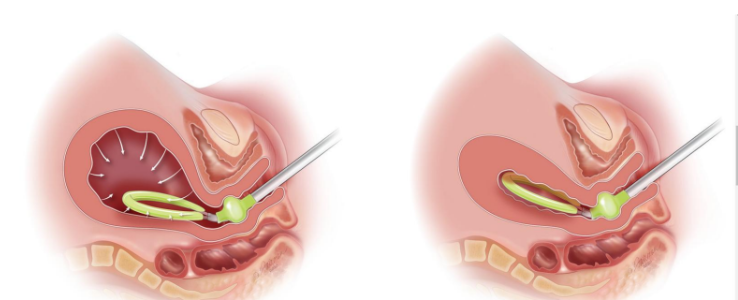
The jada for PPH
is a flexible drainage device designed to control uterine bleeding by providing suction and creating negative pressure which collapses the uterus
made by engineering students
B-Lynch suture
A uterine compression suture technique used surgically to control atony when other measures fail.
OB hemorrhage cart
• Quick access to emergency supplies
• Refrigerator for meds
• Establish necessary items and par levels
• Label drawers/compartments
• Include checklists
• Develop process for checking and restocking
• IV pressure bags
• Sutures for B-lynch and modified B-lynch techniques
• Bakri balloon
• 500 cc fluid for filling
• Bag for drainage collection
• Kerlex roll
• Vaginal pack
nursing management of PPH
• Call for help
• Assess and massage uterus properly
• Ensure 18 G IV, LR with ongoing Pitocin
• Emergency Cart
• Weigh pads; monitor bleeding
• Assess lochia for color, amount, and clots
• Administer medications/ blood/ oxygen
• Monitor vital signs
• Insert Foley
• Assign runner, recorder, CRNA, family liaison
• Collect lab work as ordered
lacerations and hematomas
• Injuries to the labia, perineum, vagina, and cervix
• Hematoma
Cardinal sign is pain not relieved by analgesics
• Lacerations
Bleeding despite firm uterus
Episiotomy laceration degrees
First-degree: skin and vaginal mucosa;
Second-degree: includes perineal muscles;
Third-degree: extends to anal sphincter;
Fourth-degree: extends into rectum itsself and mucosa.
Vulvar/vaginal hematomas
Bleeding into vulvar or vaginal tissues often associated with forceps delivery;
presents with rectal pressure and severe pain.
Uterine inversion management
Discontinue pitocin, call for help, start IV fluids,
Consider what medications you have available to relax uterus, manually inverse uterus;
Retained placental tissue
• Normal separation within 15 min
• 95% separation within 30 min
• Retained placenta
• Not separated within 30 min of start of 3rd stage
Abnormal placental implantation (accreta/increta/percreta)
Placenta adheres to/penetrates the uterus abnormally:
accreta (adhesion to myometrium) A for ADHERE
increta (into myometrium), I for INTO
percreta (attaches through uterus)
question
A nurse is caring for a client 2 hr after a spontaneous vaginal
birth and the client has saturated two perineal pads with blood
in a 30-min period. Which of the following is the priority nursing
intervention at this time?
• Palpate the client’s fundus
activity
4 causes: Tone, trauma, tissue, thrombin
Which of the 4 t’s the most common cause of PPH: tone
Name 3 risk factors: big baby, multiple babies, long labor, too much amniotic fluid, infection
3 medications used: pitocin, hemabate, methergine
3 nurisng interventions for hemorrhage: fundal massgae, start IV, call for help, weighing blood, getting hemorrhage cart
4 types of hypertension
Chronic Hypertension–CHTN
Gestational Hypertension-GHTN
Preeclampsia- (AKA Pre-e or older slang term was ‘Toxemia’)
Preeclampsia with severe features
Eclampsia
why is hypertension bad in pregnancy
Narrowed blood vessels
Placental insufficiency/ restricted blood flow/ poorly oxygenated uterus
Oligohydramnios = low amniotic fluid
IUGR, Small for gestational age baby
Chronic hypertension (CHTN) in pregnancy
• Present BEFORE pregnancy
May or may not be diagnosed already
• 140s/90s typical
• If new onset HTN develops prior to 20 weeks, it is chronic hypertension.
• No protein in the urine
• Increased BPs remain high 12 weeks after birth
Gestational hypertension (GHTN)
New-onset hypertension after 20 weeks of gestation without proteinuria or severe features; resolves postpartum.
• HTN with BP >140s/90s
• 2 occasions, 4 hours apart
Preeclampsia
HTN that develops >20 weeks
• Hypertension 140s/90s with
• Proteinuria in a urine specimen- 300+ mg in a 24 hr specimen, Or 0.3+ protein/creatinine ratio spot check
• Resolves by 12 weeks postpartum
Common risk factors
• Multifetal gestation
• History of preeclampsia
• Chronic hypertension
• Preexisting diabetes and/or thrombophilias
• Women with a new partner
• Paternal factors
2% to 7% of healthy pregnancies
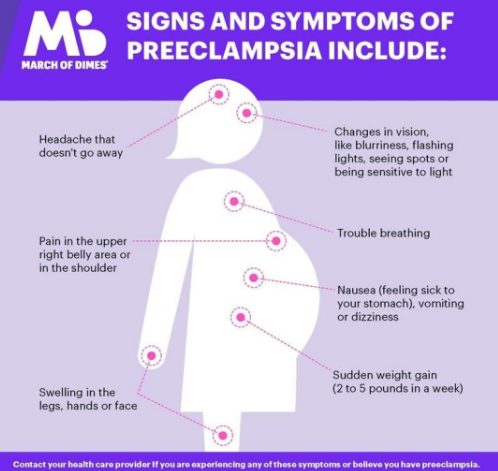
signs of preclampsia
headache that doesnt go away
trouble breathing
swelling in legs, hand, face
nausea
sudden wieght gain of 2-5 pounds
changes in vision, blurriness, flashing lights seeing spots
Preeclampsia with severe features
Hypertension 160+/110+ and Proteinuria with one or
more:
o Thrombocytopenia
o Impaired liver function (do LFTS)
o New onset renal insufficiency (decreased GFR check labs)
o Pulmonary edema
swelling all over the body not just legs or arms
o New onset cerebral disturbance (severe headache)
o New onset of visual disturbances
• Increased risk of placental abruption, IUGR, and stillbirth
• Resolves by 12 weeks postpartum
Eclampsia
• Seizure activity or coma (definitive)
• No history of preexisting (seizure-related) disorder
• Eclamptic seizures can occur before, during, or after birth
• Due to cerebral edema or cerebral hemorrhage
• Possible placental abruption
interprofessional care
• High-risk patients can receive low-dose aspirin in 1st trimester
• Accurate BP’s at Clinic visits
Assess for
• HTN
• Edema / large sudden weight gain
• DTR’s/clonus
• Proteinuria
• Symptoms of severe features
gestational hypertension and pre-e care management
Maternal and fetal assessment done at home
• NST, BPP weekly
• Fetal Movement Counts (4 or more in 1 hr)
o Amnioic fluid index and Eestimated fetal weight
o Labs weekly (liver, urine, kidney (BUN, creatinine, GFR), CBC
o BP twice/week
o Daily weights, did they gain like 5 pounds in one day
Regular diet with adequate protein
pre e with severe features
• Inpatient management
Meds – Mag sulfate, antihypertensives, and betamethasone (if <34 weeks) helps mature babies lungs when they early
Goal BP is like 140/90 not 120/80
• Continuous fetal monitoring
• Careful VS, Strict I/Os, careful assessment
• Bed rest, rails up, quiet darkened room
After Mag, inpatient expectant management versus delivery
• 37 weeks+ gestation = delivery
• 34-37 weeks-determine how ‘bad’ is the PreE, do we need to consider delivery
Magnesium sulfate therapy- High risk medication alert
Goal is to lower risk for seizure activity
• Keep mom pregnant just a little longer + Neuro benefit to baby (less risk for cerebral palsy)
• Double-check system
• 4-6g over 15-30 min loading dose, then 2g per hour until 24 hours after delivery
o Maintain serum level 4-7 mEq/L
• Educate: PT will feel nauseated, malaise, warm, flushed, diaphoretic, and sedated
• Excreted by kidneys (check renal function closely)
Magnesium sulfate toxicity monitoring
• Hourly Mag toxicity checks
o Foley with urimeter (atleast 30ml per hour)
o Respiratory Rate! if toxic level will be less than 12
o Reflexes/DTRs, they will have hyperreflxia, if absent too much magnesium sulfate
• Discontinue if no DTRs, slurred speech, poor respiratory rate, cardiac symptoms
• Calcium Gluconate available!!
Magnesium toxicity
• TOXIC WHEN SERUM LEVELS ARE TOO HIGH:
• Monitor VS, Q30 minutes to hourly
• Monitor for RR<12 breaths/minute
• Hourly I&O’s, need UO>30 ml/hr
• Monitor for signs of end organ damage
• Monitor DTR’s and clonus
Antidote: Calcium Gluconate
seizure activity
Pad side rails for all patients at risk for seizures
• Call for help! Do not leave the bedside
• Protect airway - Turn to side
• Time the seizure
After seizure
o Administer O2 – pulse ox
o Suction as needed
o IV, foley, mag sulfate, monitor VS and fetus, stat labs, emergency meds available (hydralazine, labetalol, nifedipine, calcium gluconate),
Consider a stat delivery
Interventions
• Control of Blood Pressure
• Antihypertensive medications are indicated when the systolic BP exceeds 160 mm Hg or the diastolic BP exceeds 110 mm Hg
Postpartum care
• Vital signs, intake and output, DTRs, level of consciousness
• Magnesium sulfate infusion is continued after birth for seizure prophylaxis as ordered, usually for 24 hours
Future health care
• Significant risk of developing preeclampsia in a future pregnancy (women with severe features)
• Increased risk for developing chronic hypertension and cardiovascular disease later in life
• Educate clients on lifestyle changes
Aspirin for preeclampsia prevention
Low-dose aspirin in the first trimester for high-risk patients to reduce the risk of developing preeclampsia.