Lecture 14: Psychiatric disorders and schiz.
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
How do you prove that psychiatric disorders are more than illnesses?
Biological bases, real ligitimate thing
Ppl w mental illness are not fundamentally different. They’re just in general tend to lie toward the extreme end of the spectrum. So the brain operates in an usual way, but just has abnormally high or low level of smth
Socially defined
By defining who is hyperactive/hypoactive in smth is socially constructed
Evolving. (Who considered as schizophrenic in 1980 vs. 2025. )
Boundaries somewhat arbitrary
We’re categorizing indv differently
e.g. Schizoaffective disorder
A constellation of symptoms: DSM is not interested in CAUSE, but focuses heavily on diagnosing symptoms)
Polytreatment as the norm: Like mood modulators for BPD, and so on
3 things considered mental disorders before
Masturbation (19th)
Drapetomania: “Mental illness” of trying to escape from slaveowners
Homosexuality (until removed from DSM in 1970s)
Implications:
Any of these categorizations are necessary to gonna intersect our idea of what’s acceptable and normal
All kids are gonna be impulsive, have level of hyperactive
Are equivalent disorders found around the world?
To some extent, yes
E.g. schizophrenia, bipolar, depression
But there are cultural disparities (nature of behavioral manifestation)
Also “culturally-bound disorders”: Disorders that are categorized, but don’t clearly show up across cultures in a universal way
Culturally-bound disorders
Disorders that are categorized, but don’t clearly show up across cultures in a universal way
E.g. koro (Chinese – men think that genitalia retracting into their abdomen), windigo (Canada, the desire to eat human flesh, like carnibolism), anorexia nervosa (withholding food on your self, manifest in Western culture due to thin body ideal)
Doesn’t mean anorexia isn’t real, but just hard to spot from diff manifestations across cultures
How are brain differences the norms (3)
Differences in brains of control vs. ADHD, for example. You’ll see statistically significant differences. But also differences in classical music lovers vs. heavy metal music lovers. You’ll still see statistically significant difference between their brains!
It means that without any behavioral data, it’s very hard to interpret the meaningfulness of these brain diffs. Brain diff between two doesn’t mean one of them is diseased
Differences will be observed between virtually all groups of individuals with the right tools
Implication: We only have a really statistically weak neuroimaging tools
Currently, imaging is far too insufficient for diagnosis
Implication: There’s no tool to measure such chemical imbalance
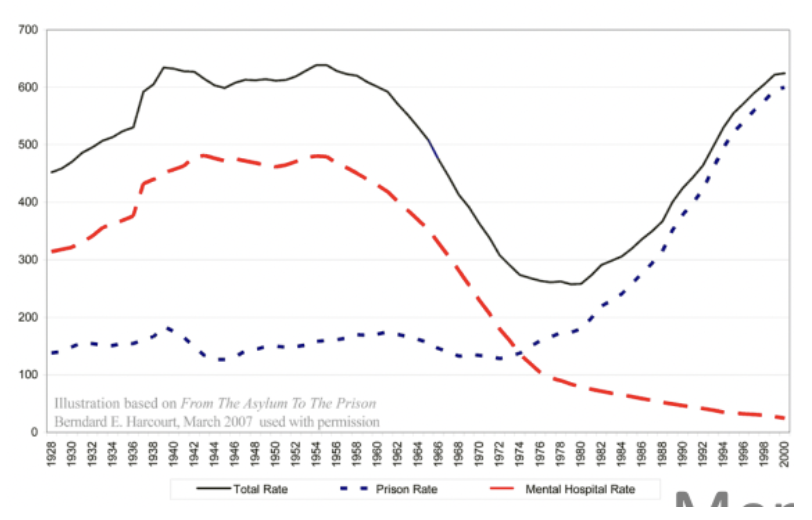
Deinstitutionalization
The process of reducing the population of long-term psychiatric hospitals by providing community-based care instead.
Previously: Sanatorium, asylum, in-patient care. Huge shame on ppl w mental health issues. There was a tour for random ppl to look around in these hospitals and looked at those ppl w mental health issues like they’re visiting a zoo.
→ Balloon theory
Balloon theory
This theory suggests that as mental health institutions closed, those individuals often ended up in homelessness or the prison system.
Rise in homelessness, prison, and decrease in mental hospital rate.
Are People With Psychological Disorders Dangerous?
Mental disorders rarely lead to violence and clinical prediction of violence is unreliable
Those with mental disorders are disproportionately more often the victims of crime than those non-mentally ill (including murders)
Psychosis is NOT psychopathy
Psychosis is not dangerous, it’s linked to schizophrenia. Means losing in touch with reality (hallucination, delusion, depersonalization)
Psychopathy much higher likelihood to commit crimes (Studies found that judges and surgeons have slightly higher trait of psychopathy)
All kinds of DSM and DSM threshold
DSM-I (1952) and II (1968): psychodynamic-heavy (primary organized around Freud’s fucked up ideas, and homosexuality)
DSM-III (1980): Spitzer’s vision, exhaustive, So many categories (216 small categories)
DSM-IV (1994): (900 pages) This version stays for so long cuz ppl who made these DSMs have financial conflicts of interest with pharmaceutical companies. They made it less transparent → weren’t allowed to make DSM-V
DSM-V (2013): NDAs (legally literate so clinicians can communicate), rewrites, a “living document”
Much more flexible
Exhaustive classification system for every possible mental disorder
DSM threshold: False positive and negative over and underdiagnosis (you have to have the certain amount of symptoms to get diagnosed as a mental illness
4 purposes of DSM-V
To guide treatment choices. (even though schiz varies for every individual)
To allow clinicians to communicate.
To please insurance companies who require a concrete diagnosis.
To permit research (via categorization to look for common underlying conditions)
Schizophrenia DSM-V: A
2+ of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated). One must be (1), (2), or (3):
Delusions
Hallucinations
Disorganized speech (e.g., frequent derailment or incoherence)
Grossly disorganized or catatonic behaviour
Negative symptoms (i.e., diminished emotional expression or avolition)
Do positive or negative symptoms happen first?
Positive symptoms manifest first before negative symptoms
We question if negative symptoms are side effects of the medication, but found that even ppl who don’t take meds still manifest negative symptoms
Schizophrenia DSM-V: B
For a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas, such as work, interpersonal relations, or selfcare, is markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, there is failure to achieve expected level of interpersonal, academic, or occupational functioning)
Schizophrenia DSM-V: C
Continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms.
During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or by two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences).
Prodromal period
The early, often subtle, phase where symptoms are beginning to emerge but haven't reached full psychosis.
Residual period
This phase follows the active phase of psychosis and is characterized by a return of symptoms that were more prominent during the active phase, but at a lower intensity
Schizophrenia DSM-V: D & E
D. Schizoaffective disorders (bipolar I, depression with mania) have been ruled out (psychosis — hallucinations, delusions, disorganized thinking — is not primarily explained by mood problems)
E. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition
Positive symptoms
Increase in how you exp the world (delusion, hallucination, repetitive movements)
Negative symptoms
Decrease in how you exp the world: decrease in spontaneous speech, motivation, pleasure, etc.
Cognitive symptoms
Deficits in working memory, doing abstract work, interpersonal cues and relationships
Mood symptoms
Cheerful or sad in the way, simultaneous diagnosed to have major depressive disorders
Schiz stats
Prevalence: 0.5-1.5%, slightly more common in men
Onset: teens to early 30s
Unemployment, poverty, homelessness common
What it doesn’t look like: Dissociative identity disorder (DID)
Relative risk is relatively high (genetic)
Heritability gaps: There’s no “schizophrenia gene,”
Psychostimulants and cannabis use are small, but may dig out the underlying cause, most likely due to environmental causes
Brain changes in schizophrenia
Widespread decreased gray matter (related to negative symptoms – loss of synapses and brain tissue), sometimes abnormal white matter
Enlarged ventricles (loss of tissue → fill up the space with fluid)
Seen through DTI
Affects parietal lobe the earliest: (which is not related to dopamine producing at all!) related to like contralateral neglect, or diff ways to see the world, which can be seen in schizophrenia
Why ppl say schiz is a neurodevelopmental disease: Structural (3)
Some types of interneurons (i.e. GABA) are missing (impaired balance between excitation and inhibition – changing between signal and noise)
Hippocampus: atypical layering structure, atypical neuronal shape
Prefrontal cortex (PFC):
Fewer dendritic spines on pyramidal neurons
Fewer GABAergic interneurons (fewer inhibition)
Why ppl say schiz is a neurodevelopmental disease: Functional
Hypofrontality (hypoactive – less active than normal in frontal cortex) – frontal and temporal lobes (incl. hippocampus), dysfunctional dopamine neurotransmission (pre- and post-synaptic), probably much more
Best considered a neurodevelopmental disorder
Non-pharmacological treatments
There are few non-pharmacological treatments that are useful during the acute phases of schizophrenia.
Cognitive-behavioural therapy (CBT) can be valuable for positive and negative symptoms when combined with pharmacological interventions.
Insight therapies and counselling: useful when the individual has been stabilized on medications: Help with any co-existent mood or anxiety disorder, support as they deal with the difficulties of integrating themselves back into society
Pharmacological treatment (antipsychotic drugs)
The most common treatments are pharmacological: anti-psychotic drugs (aka neuroleptics) and are beneficial for positive symptoms!
Negative symptoms are not treatable by any drugs
Discovery of neuroleptics
In 1950, a surgeon noticed that the administration of chlorpromazine to his patients to counteract swelling had a calming effect.
He subsequently suggested that it might have a calming effect on difficult-to-handle patients with psychosis
Subsequent research showed that, after being administered for a period of 2-3 weeks, it alleviated the symptoms of psychosis in many patients (in surprising number of patients)
Sciz medication is dopamine D2R antagonists
Dopamine theory of schizophrenia
The theory that schizophrenia is caused by too much activity at receptors for the neurotransmitter dopamine.
Schiz drugs are dopamine D2R antagonists
4 findings dopamine theory was based on
PD brains have super low dopamine, and antipsychotic drugs (for schiz) produce symptoms that are similar to PD.
Drugs that increase dopamine levels (e.g., amphetamine, cocaine) produce positive symptoms of schizophrenia (e.g. hallucination, feels smth crawling under skin)
The efficacy of an antipsychotic drug is correlated with the degree to which it blocks activity at dopamine receptors. Low dose of psychostimulant (<1mg) is beneficial enough.
Ppl w schiz have hypersensitive/higher-than-usual dopamine release
The more dopamine released, the more changes in positive symptoms
Changes on BOTH postsynaptic and presynaptic side
Criticisms of problems with the dopamine theory
The newer “atypical” antipsychotic drugs produce a wide variety of changes in the brain (so it targets more than just dopamine) and were just as good as traditional antipsychotics (proving that it’s not just about dopamine that makes psychosis — positive symptoms)
They’re just as good and just as bad. (They’re stil dopamine antagonist drugs)
It takes 2-3 weeks for antipsychotic drugs to work, yet their effects on dopamine receptor activity are immediate.
Not just changing dopamine level, but with this duration of waiting time, it prolly changes so many regions in your brain, maybe midbrain, or just invasive to other areas
MOST patients show NO benefit to the first antipsychotic they are given.
Glutamate hypofunction theory
Dysfunction of glutamate NMDA receptors on GABAergic interneurons leads to a decrease in GABAergic transmission. (Glutamate and GABA dysfunction theory)
Fewer GABA interneurons (esp in the PFC), and these interneurons are more likely to have dysfunctional NMDAR on them →
Dysfunctional NMDAR lead to altering the balance of Glutamate and GABA (excitation and inhibition balance) which leads to the problems like positive symptoms
Glutamate hypofunction theory’s evidence to support (5)
Post-mortem brains show fewer glutamate receptors in schiz vs. control
Glutamate antagonists like phencyclidine (PCP) and ketamine can mimic symptoms and cognitive problems of schiz
NMDAR co-agonists (e.g. glycine, d-serine)(activated, like strengthen LTP) provide small improvement
Heavy cannabis use → remove some of NMDAR (mimics “hypofrontality” — weakens executive functions)(and this is why cannabis MAYBE a risk factor of schiz)
CB1 (cannabinoid receptors, activated by THC) receptor activation causes CB1-NMDAR internalization(NMDAR removed from synapse → stop working)
Basically means that heavy cannbis use → remove NMDAR → less gluta → weird exci and inhi balance
Glutamate hypofunction theory’
Positive symptoms can’t be treated by glutamatergic medication. But helps with negative symptoms
Evidence that makes us question if schizophrenia could be an autoimmune disorder (2)
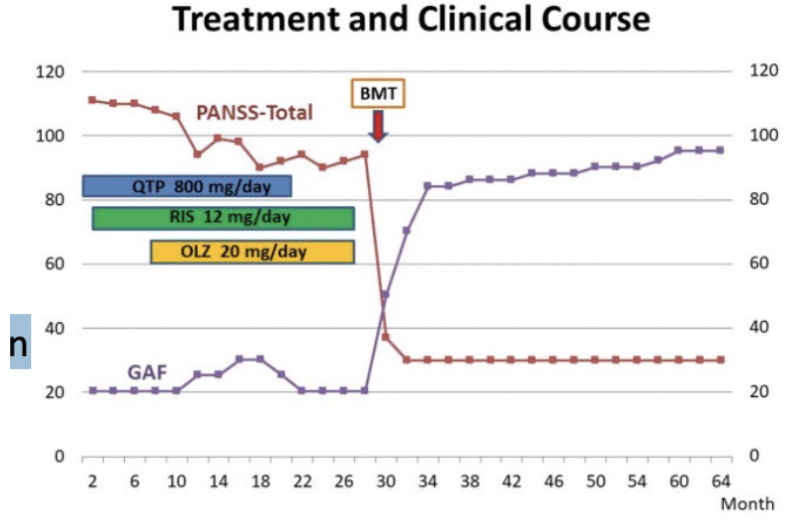
Bone marrow transplant (BMT) “cured” schizophrenia! (Miyaoka et al. 2017)
Another BMT “caused” schizophrenia (used bone from his sibling who has schiz
Possible explanations of why schiz might be autoimmune disorder (3)
Hypothesis: BMT restores microglia function
Autoimmune disorders more prevalent in schizophrenia
NMDAR attacks immune system when it’s not supposed to