Chapter 26- Assessment of high-risk pregnancy
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
53 Terms
Categories of risk factors for high-risk pregnancies
biophysical, psychosocial sociodemographic, and environmental
Biophysical factors
Genetic- defective genes, transmissible inherited disorders and chromosomal anomalies, multiple gestation, large fetal size, and ABO incompability
Nutritional status- young age, three pregnancies in the previous 2 years, tobacco, alcohol, or drug use, inadequate dietary intake because of chronic illness or food fads, history of bariatric surgery, inadqueate or excessive weight gain, and hematocrit value less than 33%
Medical and obstetric disorders- complications of current and past pregnancies, obstetric-related illnesses, and pregnancy losses
Psychosocial factors
Smoking
Caffeine (more than 200 mg of caffeine daily→increased risk for giving birth to infants with intrauterine growth restriction)
Alcohol
Drugs
Psychologic status
Sociodemographic factors
Low income
Lack of prenatal care
Age
Adolescents
Mature women
Parity
Marital status
Social determinants of health
Ethnicity
Environmental factors
Infections
Radiation
Chemicals ex. mercury and lead
Therapeutic drugs
Illicit drugs
Industrial pollutants
Cigarette smoke
Stress
Diet
Paternal exposure to mutagenic agents in the workplace (increased risk for miscarriage)
Two goals of antepartum testing
Identify fetuses at risk for injury caused by acute or chronic interruption of oxygenation so that permanent injury or death might be prevented
Identify appropriately oxygenated fetuses so that unnecessary intervention can be avoided
Monitoring usually begins by 32-34 weeks of gestation
Common maternal and fetal indications for antepartum testing
Diabetes
Hypertension
Preeclampsia
Systemic lupus erythematosus
Renal disease
Cyanotic heart disease
Fetal growth restriction
Oligohydramnios
Late term or postterm gestation
Previous stillbirth
Decreased fetal movement
Daily fetal movement count (DFMC) (kick count)
Decreased fetal activity is noted in response to hypoxemia
One recommendation is to count once a day/60 minutes
Other common recs 2-3 times daily (after meals or before bedtime) for 2 hours or until 10 movements are counted
or all fetal movements in a 12-hour period each day until a min of 10 movements are counted
counting starts around 28 weeks
When a pregnant woman reports decreased fetal activity, a nonstress test is usually performed
Note- fetal movements are not usually present during the fetal sleep cycle, reduced temporarily if the woman is taking meds that depress the CNS, drinking alcohol, or smoking. Obesity decreases perception of fetal movements and the ability of the woman to count them. Fetal kicks DO NOT decrease as the woman nears term
2D ultrasound
The image produced includes only two dimensions (length and width), so it appears flat.
The image is viewed in black, white, or shades of gray.
• This is the standard medical scan used in pregnancy.
3D ultrasound
The image is usually displayed in sepia tones rather than in black and white.
This scan can be used for diagnostic or management purposes. Viewing certain anomalies using a 3D scan provides further information that assists in planning for care at birth and for the neonate. These images are also often requested by pregnant women and families simply for their own enjoyment.
4D ultrasound
The images produced are recorded and played back in succession. As the image is continuously updated, the fetus is viewed in real time.
Transvaginal ultrasound
Probe inserted in vagina
Does not require that the woman have a full bladder
Useful in obese women whose thick abdominal layers cannot be penetrated with an abdominal approach
Optionally used in the first trimester to detect ectopic pregnancies, monitor the developing embryo, help identify abnormalities, and help establish gestational age
In some instances, it may be used along with abdominal scanning to evaluate for preterm labor in second- and third-trimester pregnancies
Abdominal ultrasound
More useful after the first trimester, when the uterus becomes an abdominal organ
Woman should have full bladder to displace the uterus upward to provide better image of the fetus
Standard (basic) ultrasonography exam (1)
done most frequently and can be performed by ultrasonographers or other health care professionals.
In the second and third trimesters, a standard exam is used to evaluate fetal presentation, amniotic fluid volume (AFV), cardiac activity, placental position, fetal growth parameters, and the number of fetuses.
Also used to perform an anatomic survey of the fetus.
Limited ultrasonography exam (2)
determine specific piece of information about the pregnancy ex. identifying fetal presentation during labor or estimating AFV
Usually performed by the woman’s obstetric health care provider in the office or clinic or in the labor and birth unit
Specialized (detailed) or targeted ultrasonography exam (3)
done when suspect woman is carrying an anatomically or physiologically abnormal fetus.
Indications include abnormal history or lab findings or abnormal results of a previous standard or limited ultrasound exam.
Highly trained and experienced personnel do these exams
First trimester- major uses of ultrasound during pregnancy
Confirm pregnancy
Confirm viability
Determine gestational age
Rule out ectopic pregnancy
Detect multiple gestation
Determine cause of vagina bleeding
Visualization during chorionic villus sampling
Detect maternal abnormalities such as bicornuate uterus, ovarian cysts, fibroids
Second trimester- major uses of ultrasound during pregnancy
Establish or confirm dates
Confirm viability
Detect polyhydramnios, oligohydramnios
Detect congenital anomalies
Detect IUGR
Assess placental location
Visualization during amniocentesis
Evaluate for preterm labor
Third trimester- major uses of ultrasound during pregnancy
Confirm gestational age
Confirm viability
Detect macrosomia
Detect congenital anomalies
Detect IUGR
Determine fetal position
Detect placenta previa or placental abruption
Visualization during amniocentesis, external version
Biophysical profile
Amniotic fluid volume assessment
Doppler flow studies
Detect placental maturity
Evaluate for preterm labor
Fetal heart activity
can be demonstrated by about 6 weeks using transvaginal ultrasound
Fetus in favorable position→good views of the fetal cardiac anatomy using transvaginal ultrasound by 13 weeks
Fetal death can be confirmed by lack of heart motion along with presence of fetal scalp edema and maceration and overlap of the cranial bones
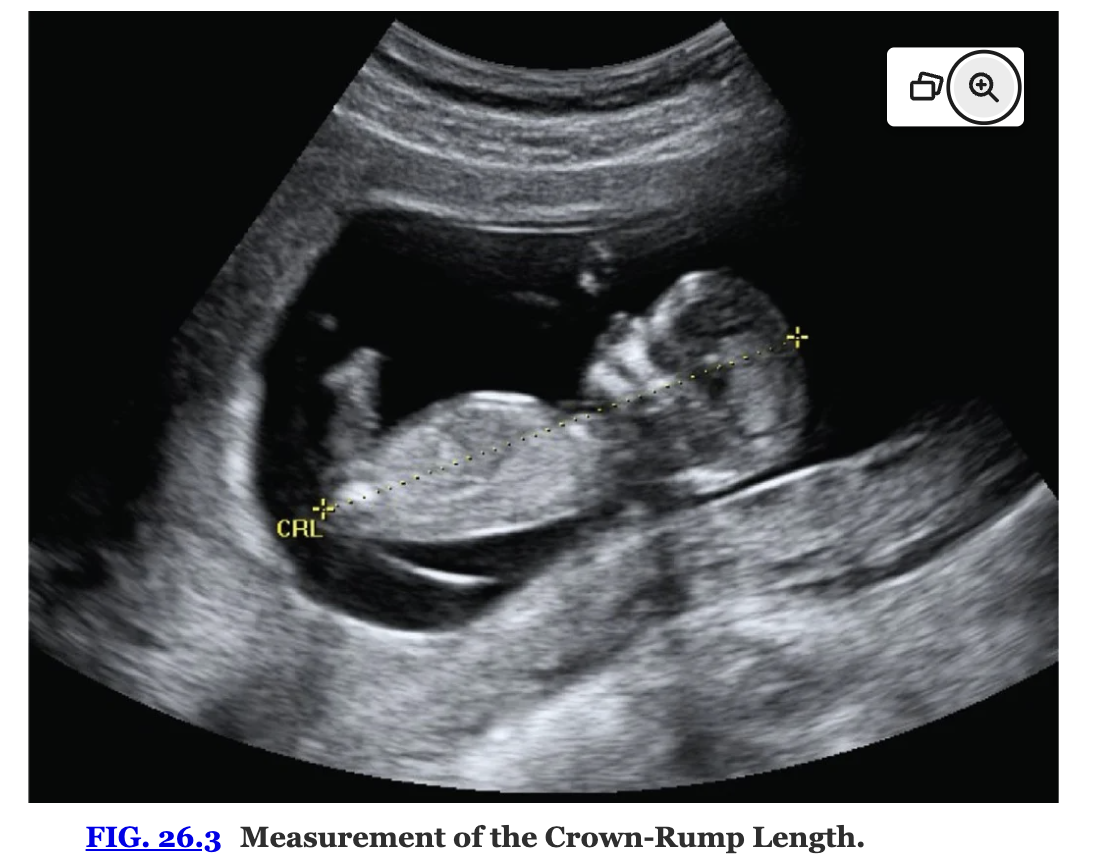
Gestational age by ultrasound
indicated for situations such as uncertainty regarding the date of the last normal menstrual period, recent discontinuation of oral contraceptives, a bleeding episode during the first trimester, uterine size that does not correlate with dates, and other high-risk conditions
Either the maximum embryo length or the crown-rump length is used during the first trimester to measure the early embryo
After the first trimester, the biparietal diameter (BPD), head circumference, abdominal circumference, and femur length are measured instead.
Fetal growth
Conditions that require ultrasound assessment of fetal growth include poor maternal weight gain or pattern of weight gain, previous pregnancy with intrauterine growth restriction (IUGR), chronic infections, substance use (e.g., tobacco, alcohol), maternal diabetes, hypertension, multifetal pregnancy, and other medical or surgical complications
IUGR may be symmetric (the fetus is small in all parameters) or asymmetric (head and body growth do not match)
Symmetric IUGR reflects a chronic or long-standing insult and may be caused by low genetic growth potential, intrauterine infection, chromosomal anomaly, maternal undernutrition, or heavy smoking.
Asymmetric growth suggests an acute or late-occurring deprivation such as placental insufficiency resulting from hypertension, renal disease, or cardiovascular disease.
Reduced fetal growth is still one of the most frequent conditions associated with stillbirth
Nuchal translucency (NT) screening
measurement of fluid in the nape of the fetal neck between 10 and 14 weeks of gestation to identify possible fetal abnormalities
A fluid collection greater than 3 mm is considered abnormal. When combined with abnormal maternal serum marker levels, elevated NT indicates a possible increased risk of certain chromosomal abnormalities in the fetus including trisomies 13, 18, and 21.
An elevated NT alone indicates an increased risk for isolated anomalies such as congenital heart defects, abdominal wall defects, and diaphragmatic hernia. If the NT is abnormal, a targeted ultrasound scan and possibly fetal echocardiography in the second trimester should be offered
Placental position
pattern of uterine and placental growth and the fullness of the maternal bladder influence the apparent location of the placenta by ultrasonography
After 16 weeks of gestation, if the edge of the placenta ends at least 2 cm from the cervix, the placental location is considered normal.
If the placental edge is less than 2 cm from the cervix, repeated ultrasound scans should be performed as pregnancy progresses until the placenta moves well away from the cervical os or it becomes clear that the previa will persist.
At least 90% of placentas identified earlier in pregnancy as previa, or low lying, ultimately resolve by the third trimester
Doppler blood flow analysis
uses systolic/diastolic flow ratios and resistance indices to estimate blood flow in various arteries.
indication of fetal adaptation and reserve
vessels most often studied are the fetal umbilical and middle cerebral arteries and the maternal uterine arteries
Severe restriction of umbilical artery blood flow as indicated by absent or reservered flow during diastole has been associated with fetal growth restriction
Significantly increased peak systolic velocity in the middle cerebral artery has been found to predict moderate to severe fetal anemia.
Abnormal maternal uterine artery Doppler waveforms have been used to predict fetal growth restriction
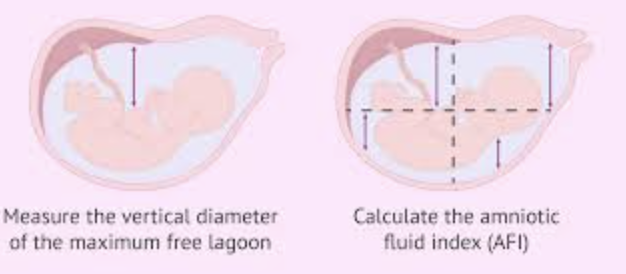
Oligohydramnios
decreased amniotic fluid
Subjective determinants include a fundal height that is small for gestational age and a fetus that is easily palpated
An objective criterion of decreased AFV is met if the max vertical pocket of amniotic fluid is < 2 cm
An AFI of <5 indicates this
Associated with congenital anomalies ex. renal agenesis (Potter syndrome), prelabor rupture of membranes, and severe IUGR
Polyhydramnios
increased amniotic fluid
Subjective criteria: fundal height that is large for gestational age and a fetus that cannot be easily palpated or that is ballotable
Objectively defined: pockets of amniotic fluid >8 cm
AFI is >25 cm
Associated with GI and CNS congenital anomalies, twin-to-twin transfusion syndrome, infections, and placental abnormalities
Amniotic fluid index (AFI)
vertical depths (in centimeters) of the largest pocket of amniotic fluid in all four quadrants surrounding the maternal umbilicus are totaled
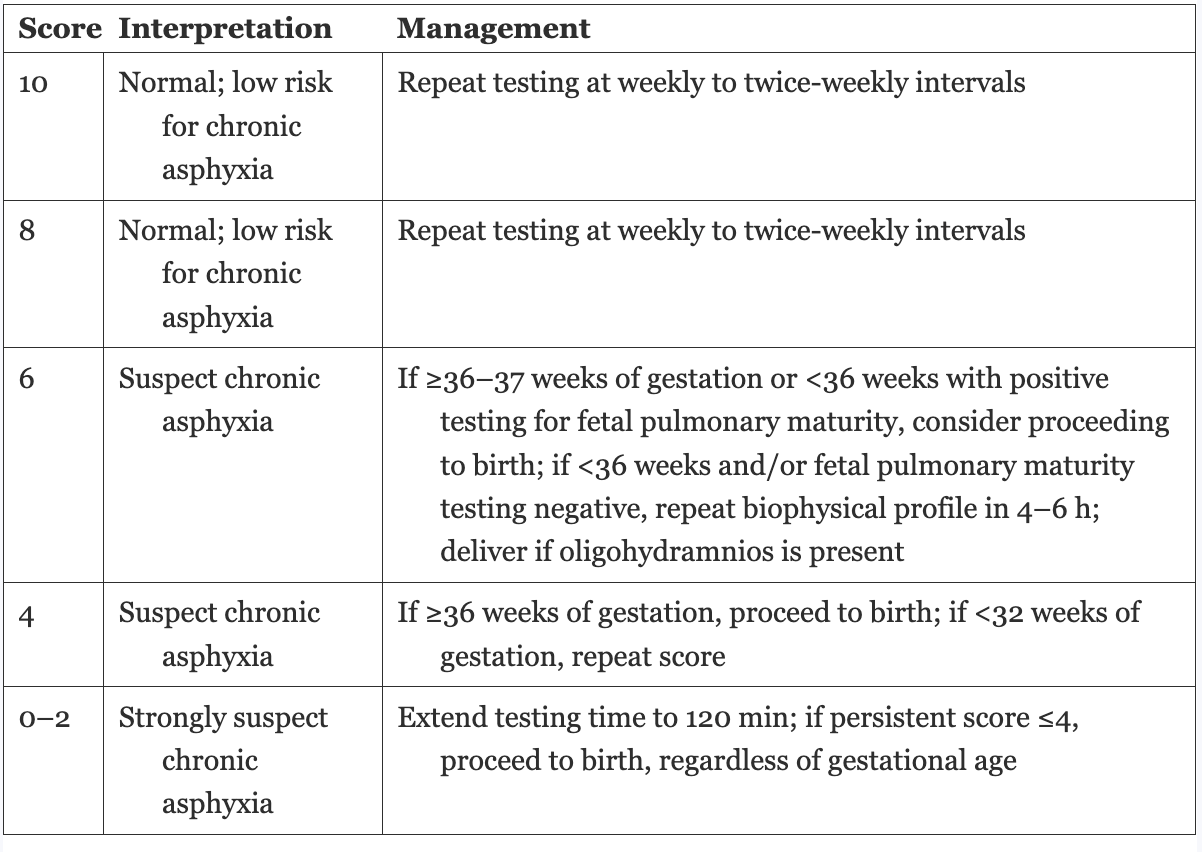
Biophysical profile (BPP)
noninvasive dynamic assessment of a fetus that is based on acute and chronic markers of fetal disease.
Includes AFV, FBM (fetal breathing movements), fetal movements, and fetal tone determined by ultrasound and fetal heart rate reactivity determined by the means of the nonstress test (NST)
FHR reactivity, FBMs, fetal movement, and fetal tone reflect the current CNS status
AFV demonstrates the adequacy of placental function over a longer period of time
The BPP is used frequently in the late second trimester and the third trimester because it is a reliable predictor of fetal well-being.
A BPP of 8 or 10 with a normal AFV is the desired test result.
Advantages of the test include excellent sensitivity, a low false-negative rate, and improved detection of fetal structural anomalies.
A limitation of the test is that if the fetus is in a quiet sleep state, the BPP can require a long period of observation.
Biophysical profile management
Modified biophysical profile (mBPP)
being used increasingly as a way to shorten the testing time required for the complete BPP by assessing the components that are most predictive of perinatal outcome.
Desired test results are a reactive NST and a single deepest vertical pocket of amniotic fluid that is more than 2 cm
Magnetic resonance imaging (MRI)
MRI is noninvasive and can provide images in multiple planes, but no interference occurs from skeletal, fatty, or gas-filled structures, and imaging of deep pelvic structures does not require a full bladder.
evaluate fetal structure (CNS, thorax, abdomen, genitourinary tract, musculoskeletal system) and overall growth, the placenta (position, density, and presence of gestational trophoblastic disease), and the quantity of amniotic fluid
Maternal structures (uterus, cervix, adnexa, and pelvis); the biochemical status (pH, adenosine triphosphate content) of tissues and organs; and soft tissue, metabolic, or functional anomalies can also be evaluated.
Biochemical assessment
Involves biologic examination ex. chrromosomes in exfoliated cells and chemical determinations
Procedures used to obtain the needed specimens include: amniocentesis, PUBS, CVS, and maternal blood sampling
Based on the test results, women may consider having an induced abortion
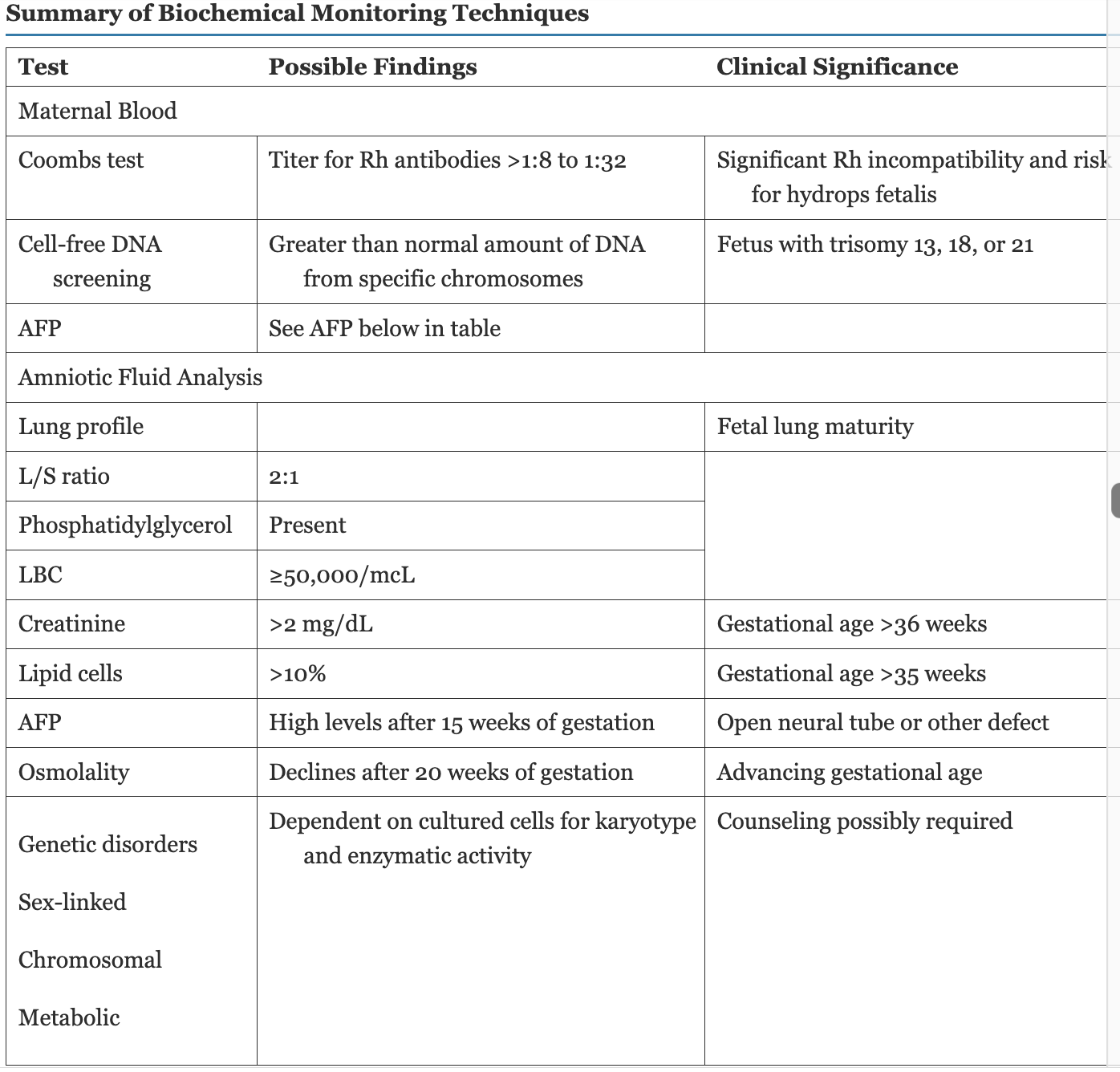
Summary of biochemical monitoring techniques
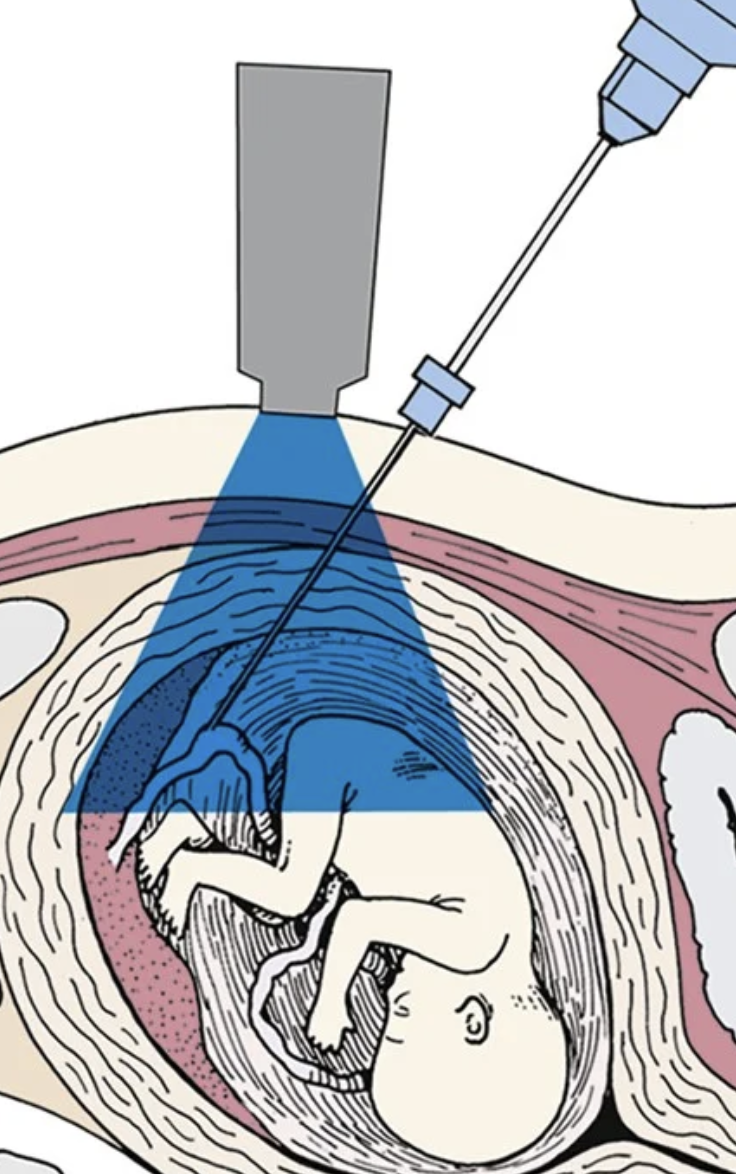
Amniocentesis
usually at or after 15 weeks to obtain amniotic fluid which contains fetal cells
a needle is inserted transabdominally into the uterus and amniotic fluid is withdrawn into a syringe.
should be avoided performing before 13-14 weeks→ higher risk for pregnancy loss, amniotic fluid leakage, and fetal talipes equinovarus (clubfoot)
Indications- prenatal diagnosis of genetic disorders or congenital anomalies (neural tube defects [NTDs] in particular), assessment of pulmonary maturity, and (very rarely) diagnosis of fetal hemolytic disease.
Because of the possibility of fetomaternal hemorrhage, administering Rh0(D) immune globulin to the woman who is Rh negative is standard practice after an amniocentesis.
![<ul><li><p>usually <strong>at or after 15 weeks</strong> to obtain amniotic fluid which contains fetal cells</p></li><li><p>a <u>needle is inserted transabdominally into the uterus</u> and amniotic fluid is withdrawn into a syringe.</p></li><li><p><strong>should be avoided performing before 13-14 weeks</strong>→ higher risk for pregnancy loss, amniotic fluid leakage, and fetal talipes equinovarus (clubfoot)</p></li><li><p><u>Indications-</u> prenatal diagnosis of genetic disorders or congenital anomalies (neural tube defects [NTDs] in particular), assessment of pulmonary maturity, and (very rarely) diagnosis of fetal hemolytic disease.</p></li><li><p>Because of the possibility of fetomaternal hemorrhage, administering <strong>Rh0(D) immune globuli</strong>n to the woman who is <u>Rh negative</u> is standard practice after an amniocentesis.</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/24fb4ec7-0599-484c-b735-22dc88987a7b.png)
Risks for having a child with a genetic disorder
• Older maternal age (35 years of age or older)
• Older paternal age (there is no consensus, but usually considered to be 40 to 50 years of age)
• Parents who are affected by or are carriers of genetic disorders including sickle cell anemia, Tay-Sachs disease, and cystic fibrosis
• Women with a prior child with a structural birth defect or with a structural fetal defect identified by ultrasound during their current pregnancy
• Women with a prior child with a chromosomal abnormality
Chorionic villus sampling
earlier diagnosis and rapid results
When performed after the first trimester, the procedure is better known as placental biopsy
Indications for CVS are similar to those for amniocentesis, although CVS cannot be used for maternal serum marker screening because no fluid is obtained.
CVS can be performed between 10 and 13 weeks of gestation and involves the removal of a small tissue specimen from the placenta. This tissue reflects the genetic makeup of the fetus.
Transcervically or transabdominally
Because of the possibility of fetomaternal hemorrhage, women who are Rh negative should receive Rh0(D) immune globulin after CVS to prevent red cell alloisoimmunization
Noninvasive prenatal testing (NIPT)
obtaining a blood sample from the pregnant woman, NIPT decreases the possible risks to the fetus associated with amniocentesis and CVS.
NIPT is able to separate fetal deoxyribonucleic acid (DNA) found in the maternal blood sample and analyze it to identify chromosomal abnormalities including trisomy 13, trisomy 18, and trisomy 21 and sex chromosome disorders
Percutaneous umbilical blood sampling (PUBS) (cordocentesis)
direct access to the fetal circulation during the 2nd and 3rd trimester
Can be used for fetal blood sampling and transfusion
The most common genetic indication for the use of PUBS is the evaluation of mosaic results found on amniocentesis or CVS, when a sample of fetal blood is required to determine the specific mutation.
PUBS is also used to assess for fetal anemia, infection, and thrombocytopenia. Bleeding from the cord puncture site and fetal-maternal bleeding are the most common complications of the procedure.
Transient fetal bradycardia can also occur.
Maternal serum Alpha-fetoprotein (MSAFP)
Screening tool for NTDs (neural tube defects) in pregnancy
Risk factors of NTD: history of this disorder in a prior pregnancy, folic acid deficiency, pregestational diabetes, and teratogen exposure (e.g., valproic acid [Depakote], carbamazepine [Tegretol])
performed between 15-20 weeks, with 16-18 weeks being ideal
AFP is produced in the fetal gastrointestinal tract and liver, and increasing levels are detectable in the serum of pregnant women beginning at 7 weeks of gestation.
Amniotic fluid AFP measurement is DIAGNOSTIC for NTD, while MSAFP is a SCREENING tool only.
Multiple marker screens first-trimester screening to detect trisomy 21
11-14 weeks of gestation
two maternal biochemical markers, pregnancy-associated plasma protein A (PAPP-A) and human chorionic gonadotropin (hCG) or the free beta-human chorionic gonadotropin (β-hCG) subunit, and evaluation of fetal NT.
In the presence of a fetus with trisomy 21, hCG levels and the NT measurement are higher than normal in the first trimester, whereas PAPP-A levels are lower than normal.
First-trimester screening using PAPP-A and hCG or β-hCG levels has been shown to be as accurate for detecting fetuses with trisomy 21 as quadruple screening in the second trimester
When used as a single marker, NT detects 70% of fetuses with trisomy 21.
The nasal bone cannot be identified on ultrasound in about one-third to one-quarter of fetuses who have trisomy 21
ADAM 12 (biochemical marker)
8-10 weeks
glycoprotein that is synthesized by the placenta and secreted throughout the pregnancy
Decreased levels of ADAM 12 are found in women carrying a fetus with trisomy 21
Multiple market screens second trimester
quadruple marker or quad test, used to screen for fetuses with trisomy 21 and 18.
15-21 weeks
measures the levels of four maternal serum markers: MSAFP, unconjugated estriol, hCG, and dimeric inhibin A
In the presence of a fetus with trisomy 21, MSAFP and unconjugated estriol levels are lower, whereas hCG and inhibin levels are elevated. Low MSAFP, unconjugated estriol, and hCG values are associated with trisomy 18
Coombs test
screening tool for Rh alloisoimmunization
If the maternal titer for Rh antibodies is greater than 1:8 to 1:32, it is considered critical because those values are associated with a significant risk for hydrops fetalis.
can also detect other antibodies that may place the fetus at risk for incompatibility with maternal antigens.
Cell-free DNA (cfDNA)
screening test for aneuploidy
performed using a sample of maternal blood
Maternal plasma contains small fragments of cfDNA, resulting from the breakdown of both maternal and fetal cells.
The test cannot actually distinguish fetal from maternal DNA, but it can accurately predict the fetal status by measuring the amount of cfDNA circulating in maternal blood and comparing it with known standards.
If the fetus has a normal karyotype, the amount of DNA is consistent with the known standard for the normal amount. However, if more than the expected amount of chromosome 21 DNA, for example, is detected, it can then be assumed that the fetus is contributing the extra amount and therefore has trisomy 21.
Not accurate <10 weeks
Less sensitive for women who are obese
Antepartum assessment using electronic fetal monitoring
First- and second-trimester antepartum assessment is directed primarily at the diagnosis of fetal anomalies.
The goal of third-trimester testing is to determine whether the intrauterine environment continues to support the fetus.
Maternal assessment of fetal movement is often used as a first-line screening test for fetal well-being
When electronic fetal monitoring and ultrasound are used for antepartum fetal evaluation, the NST and the mBPP are the primary tests performed.
The complete BPP and the contraction stress test (CST) are used for follow-up evaluation in clients who have a persistently nonreactive NST or abnormal mBPP score.
Traditionally, testing has begun at 32 to 34 weeks of gestation (earlier testing for women with multiple high-risk conditions). Once or twice weekly testing done
Nonstress test (NST)
normal fetus produces characteristic heart rate patterns in response to fetal movement, uterine contractions, or stimulation. Most fetuses who do not produce a reactive (normal) test result are not compromised. They simply fail to exhibit accelerations of the FHR during the testing period, usually because they are in a quiet sleep state.
Disadvantages include the requirement for twice-weekly testing, a high false-positive rate, and a low false-negative rate, although higher than is achieved with th
attempt to increase fetal activity by manually stimulating the fetus or having the woman drink orange juice to increase her blood sugar level.
Vibroacoustic stimulation (VAS) is often used to change the fetal state from quiet to active sleep if the initial NST result is nonreactive
Interpretation of NST
results either reactive or nonreactive
reactive- normal. two accelerations in a 20-min period. each lasting at least 15 second and peaking at least 15 beats/min above the baseline (before 32 weeks, 10s/10 beats/min)
nonreactive-test does not demo at two qualifying accelerations within a 20- min window. requires further evaluation. often extended for 20 mins. VAS may be used. If not met after 40 mins, CST or BPP should be performed.
Once NST initiated, usually repeated once or twice weekly for the remained of the pregnancy
Contraction stress test (CST) or oxytocin challenge test (OCT)
graded stress test of the fetus
Identify the jeopardized fetus that was stable at rest but showed evidence of compromise after stress.
Uterine contractions decrease uterine blood flow and placental perfusion. If this decrease is sufficient to produce hypoxia in the fetus, a deceleration in FHR results.
In a healthy fetoplacental unit, uterine contractions do not usually produce late decelerations, whereas if interrupted oxygenation is present, contractions produce late decelerations.
The CST provides an earlier warning of fetal compromise than the NST and produces fewer false-positive results.
should not be performed in clients who are at high risk for preterm labor, including women with prelabor rupture of membranes, multiple gestation, and cervical insufficiency. Also placenta previa, previous classical incision for cesarean birth or other uterine surgery
Nipple-stimulated contraction test
In one approach the woman applies warm, moist washcloths to both breasts for several minutes. She is then asked to massage one nipple for 10 minutes. Massaging the nipple causes a release of oxytocin from the posterior pituitary gland.
An alternative approach is for her to massage one nipple through her clothes for 2 minutes, rest for 5 minutes, and repeat the cycles of massage and rest as necessary to achieve adequate uterine activity. When adequate contractions or hyperstimulation (defined as uterine contractions lasting more than 90 seconds, or five or more contractions in 10 minutes) occur, stimulation should be stopped.
Oxytocin-stimulated contraction test
Exogenous oxytocin also can be used to stimulate uterine contractions.
An intravenous (IV) infusion is begun, and a dilute solution of oxytocin (e.g., 30 units in 500 mL of fluid) is infused into the tubing of the main IV line through a piggyback port and delivered by an infusion pump to ensure an accurate dose.
One method of oxytocin infusion is to begin at 0.5 milliunits/min and double the dose every 20 minutes until three uterine contractions of moderate intensity, each lasting 40 to 60 seconds, are observed within a 10-minute period.
These criteria for contractions were selected to approximate the stress experienced by the fetus during the first stage of labor
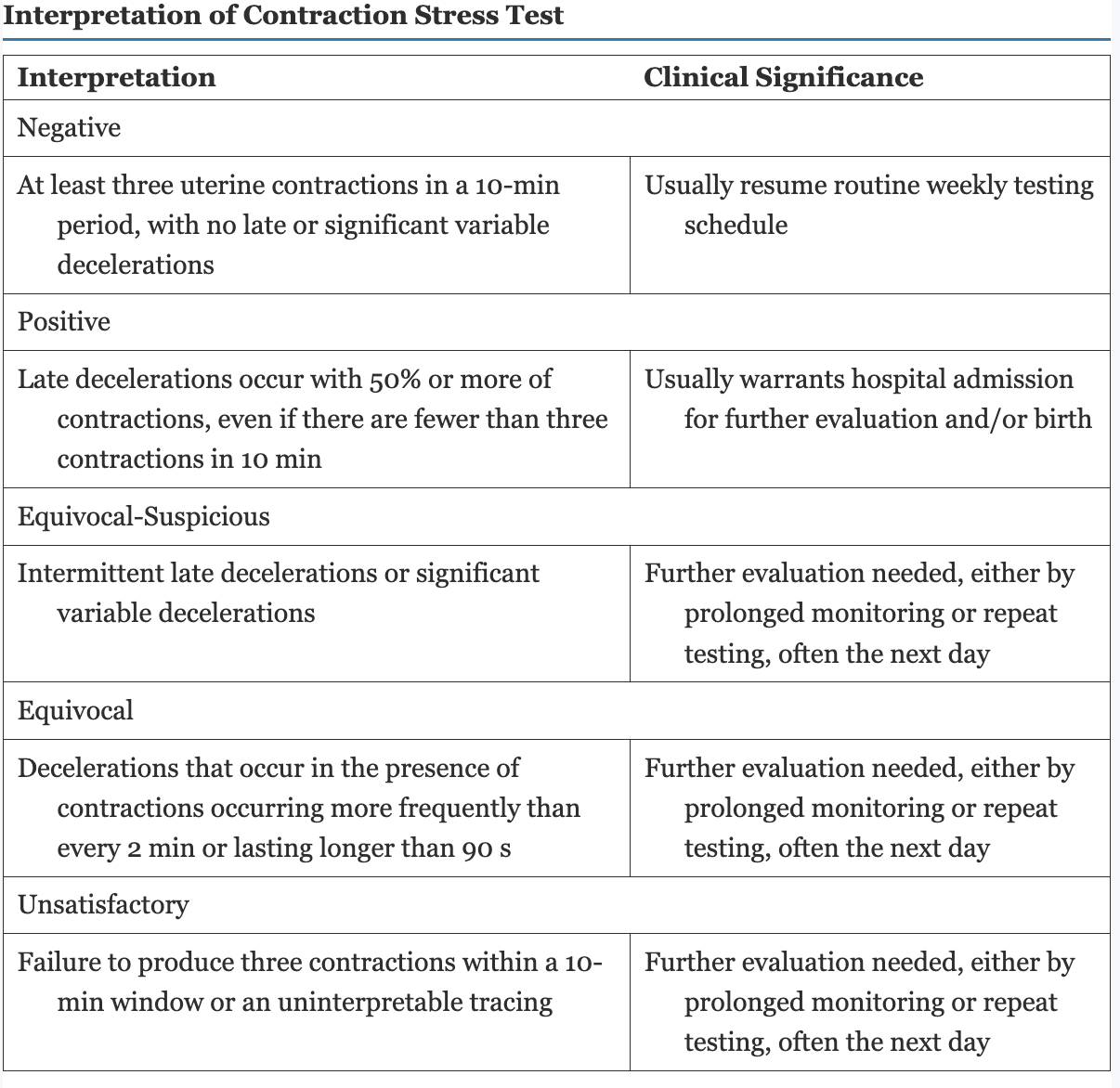
Interpretation of CST
CST results are negative, positive, equivocal-suspicious, equivocal, or unsatisfactory.
If no late decelerations are observed with the contractions, the findings are considered negative.
Repetitive late decelerations render the test results positive
The desired CST result is negative
Positive results have been associated with intrauterine fetal death, late FHR decels in labor, low 5-min APGAR scores, IUGR, and meconium-stained amniotic fluid
Unsatisfactory, suspicious, and equivocal tests require further evaluation either by prolonged monitoring or repeat testing often the following day.
Interpretation of contraction stress test table