APPROACH TO CANINE INFECTIOUS DISEASES
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms
2 PRIMARY METHODS FOR DIAGNOSING
INFECTIOUS DISEASES
• Detection of the organism
• Detection of antibodies against the organism
• CPV, aka ___________
• Targets rapidly dividing cells in the _______
• <2 weeks – ______________
• Liver, kidney, heart, vessel, bone marrow, intestine, lungs
• 3 – 8 weeks – _______
• Death after 5 months – from __________
Parvoviral enteritis
intestine
generalized; virus-induced necrosis in tissues rapidly dividing cells
myocarditis
myocardial scarring and conduction failure
PATHOPHYSIOLOGY of CPV
• Viral entry → oropharynx & lymphoid
organs → Viremia → Tissue tropism
(radiomimetic) → Viral shedding
• Intestinal damage (crypts)
• Bacterial colonization
• Endotoxic shock
> Hypothermia
> DIC
> Jaundice
GROSS PATHOLOGY
• Lymphoid depletion and thymic
involution
• Mesenteric lymphadenomegaly
• Coagulative lymphadenitis
• Flaccid, segmentally reddened
intestine with serositis (generally
limited to small intestine)
• Intestinal contents: brown to red
brown and fluid with fibrinous
exudate (with or without
hemorrhage)
CPV
HISTOPATHOLOGY
• Villous atrophy secondary to crypt
cell destruction
• Necrotic crypt epithelial cells
• Basophilic intranuclear inclusion
bodies in enterocytes and
lymphocytes (early infection)
CPV
HISTOPATHOLOGY
• Thickened alveolar walls +
inflammatory cells →
interstitial
pneumonia/pulmonary
edema & congestion
• Lymphocytic myocarditis,
recruitment of macrophages
admixed with neutrophils
• Hepatic congestion with
engorged vascular and
sinusoids dilatation
CPV
PATHOLOGICAL SEQUELA of CPV
• Dehydration
• Sepsis
• Acidosis/electrolyte imbalances
ISOLATED BACTERIA FROM FECES (Zheng, Y. et al,
2018)
• Shigella
• Peptoclostridium
• Peptostreptococcus
• Streptococcus
• Fusobacterium
TREATMENT
• Supportive
• Fluids
• Multivitamins
• Symptomatic
• Antiemetic
• Anti-hemorrhagic
• Antimicrobials
RECOMMENDED TREATMENT for CPV
• Crystalloid + Colloid (if with signs of oncotic compromise)
• LRS as primary fluid of choice
• Canine shock dose of 80-90 mL/kg – split in consecutive boluses of 15 – 20 mL/kg given over 15 minutes until improvement of the perfusion
is achieved
• >20 mEq/L potassium hydrochloride (should not exceed 0.5
mEq/kg/h)
• Antibiotics
• Ampicillin, Cefoxitin, Enrofloxacin
• Aminoglycoside (if well-hydrated)
CONTROL AND PREVENTION
• Immunization with MLV CPV2 at ____ weeks of age (for protection)
• Immunization with MLV CPV2 for adults (hyperimmunization of adults → minimized viral shedding)
• Disinfection
6
• Subacute systemic disease
with high mortality in dogs
and other carnivores
worldwide
• Single stranded RNA virus,
family Paramyxoviridae
• Outbreaks in shelter facilities
• High morbidity and mortality
• Rapid spread
CANINE DISTEMPER VIRUS
TRANSMISSION
• Oronasal exposure
• Aerosol via coughing and sneezing
• Viral shedding (days 4 to 7)
• Hematogenous spread --> epithelial cells and CNS tissues
• Contagious up to 3 months
CANINE DISTEMPER VIRUS
PATHOGENESIS of CANINE DISTEMPER VIRUS
• Replication in macrophages and
monocytes:
-
-
-
• Multisystemic infection of the
epithelial cells
• Peak virion reproduction _____ days post
infection
• Viremia → Systemic spread of virus to
different organs
-
-
-
• Tonsils
• URT epithelium
• Regional lymph nodes
4
• Fever
• Lymphocytic apoptosis → Lymphopenia
• Immunosuppression
CNS PATHOLOGY
• Viral injury & inflammatory
cytokines
• Macrophage activation and
release of inflammatory
cytokines
• Destruction and demyelination of
CNS cells
CANINE DISTEMPER VIRUS
CLINICAL SIGNS
• Asymptomatic to mild (older, with
partial immunity)
• Fever
• Lethargy
• Anorexia
• Dehydration
• Hyperkeratosis
• Serous to mucopurulent oculonasal
discharge
• Viral pneumonia with secondary
bacterial infection
• Vomiting & mucoid to hemorrhagic
diarrhea
• Neurologic sign
CANINE DISTEMPER VIRUS
DIAGNOSIS
• No pathognomonic signs (difficult to diagnose based on symptoms)
• Poor vaccination history
• CBC – lymphopenia as most consistent abnormality
• Biochemical profile
• Cerebrospinal fluid
• ELISA
• RT-PCR
• Necropsy & histopathology
• Culture & SensitivitY
CANINE DISTEMPER VIRUS
TREATMENT FOR CDV
• Supportive
• Parenteral fluids (vomiting & severe diarrhea)
• Antibiotics (bacterial bronchopneumonia and other infection)
• Doxycycline
• Broad-spectrum bactericidal
• Steroid
• Dexamethasone (to control CNS edema)
• Anticonvulsant
• Diazepam (0.25 to 1 mg/kg IV PRN)
• Phenobarbital (2.2 to 8 mg/kg PO BID)
• Levetiracetam (20 mg/kg PO TID)
• Cause of infectious canine hepatitis
• Non-enveloped, double stranded DNA
• Protected with vaccination
CANINE ADENOVIRUS TYPE 1
TRANSMISSION
• Oronasal exposure (body secretions, excretions & environmental
fomites)
• Not airborne
• Viral shedding during acute infection
• Urine as most important source of infection
CANINE ADENOVIRUS TYPE 1
PATHOGENESIS
• Lymphoid tissues of tonsils and regional lymph nodes
• Viremia (3 to 4 days post-infection)
• Infection of other tissues
• Cytopathic effect (liver, eyes, kidney)
• Vascular damage and hemorrhage (from endothelial infection)
• Hepatic necrosis (depends on the level of antiviral antibody)
CANINE ADENOVIRUS TYPE 1
CLINICAL SIGNS
• Corneal edema and anterior uveitis
• Fever, depression, lethargy
• Abdominal discomfort
• Mucus membrane pallor
• Inflammation of the tonsil
• Pharynx with tonsillar and cervical
lymph node enlargement
• Ascites & hepatomegaly
• Laryngitis, tracheitis, pneumonia,
coughing, vomiting & diarrhea
CANINE ADENOVIRUS TYPE 1
OTHER CLINICAL SIGNS
• Petechial and ecchymotic hemorrhages & epistaxis (from coagulation
abnormalities)
• Icterus (uncommon)
• Neurologic signs secondary to hepatic encephalopathy or CNS
infection
• Supported by elevation in serum bile acid and ammonia
CANINE ADENOVIRUS TYPE 1
DIAGNOSIS
• Presenting signs
• Evidence of hepatic disease with poor vaccination history
• CBC
• Thrombocytopenia and bleeding disorder (in the setting of DIC)
• PCR
• Blood chemistry profile
• Elevated ALP, ALT
• Bleeding profile
• Prolonged aPTT and PT
CANINE ADENOVIRUS TYPE 1
TREATMENT OF CAV TYPE 1
• Supportive care
• Liver tonic (i.e. Liv 52, Samylin®, S-adenosylmethionine [Denamarin®])
• Management of clinical signs and complications
• Intravenous fluid
• Blood transfusion
• To address complications of hemorrhage and DIC
• Lactulose
• To address neurologic signs → reduction of concentrations of encephalotoxins
Longest-known infectious diseases in human history
• Has 7 serotypes (6 are transmitted by bats)
• Humans and nearly all animals are susceptible
• 100% fatal if clinical signs appeared
RABIES
TRANSMISSION
• dogs as the main reservoir host
• Mainly predominant in areas of Africa,
Asia, and Central and South America
• Transmission is mainly through
infected saliva
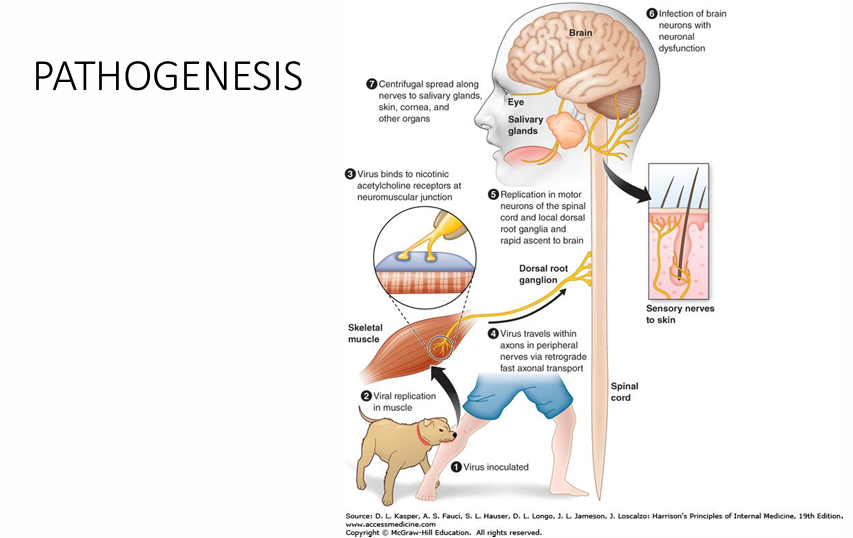
• Replicates in muscles, and ascend via
PNS/CNS
• Shedding: Saliva
RABIES
RABIES
CLINICAL SIGNS
•______
• 2-3 months but may vary from 1 week
to 1 year (6 months on the average)
• _________-
• Starts with the first appearance of
symptoms
• When the virus enters the CNS and
begins to cause damage
• Occurs usually from 2 to 10 days (on the
average) post-inoculation
Incubation Period
Prodromal Period
CLINICAL MANIFESTATIONS IN HUMANS
• Acute Neurologic Period
• Duration is 2 to 10 days that may ensue death due to irreversible neuronal
damages
• Occurs in 2 forms: Furious and Paralytic
• _______- hyperactivity, excitable behavior, hydrophobia, aerophobia; death
secondary to cardiorespiratory arrest
• _______ - 20% of the total number of human cases; paralytic muscles
(begins at the site of bite/scratch); progression from comatose to death
Furious
Paralytic
DIAGNOSIS
• ANIMALS
• Post-mortem
examination
•___________
• Gold standard
• Brain tissue tested with
fluorescent labelled
antirabies Ab
• Ab directed at
nucleoprotein componenT
Direct fluorescent
antibody test
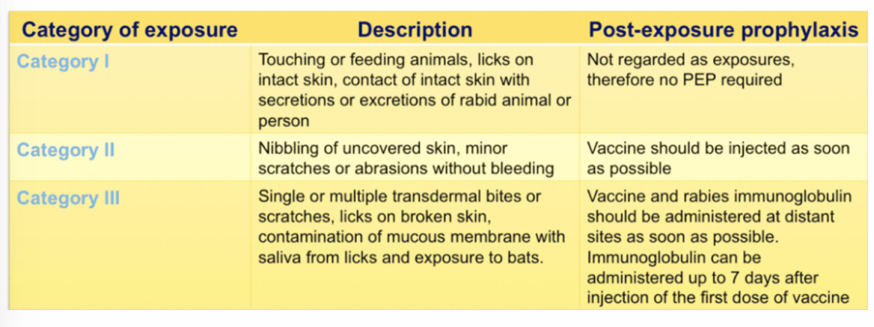
RABIES POST-EXPOSURE PROPHYLAXIS MODALITIES
ss RNA, Paramyoviridae family
Most commonly associated with CIRD
Acute Respiratory Signs
Part of core or specific kennel cough vaccine
Canine Parainfluenza Virus (CPiV)
non-enveloped ds DNA, Adenoviridae family
seldom isolated from dogs with CIRD in Europe (possibly due to vaccination)
Confirmatory test:_____
Canine Adenovirus 2 (CAV-2)
PCR
enveloped ds dna, Herpesviridiae
higher prevelance in kenneled dogs vs household
with secondary role in CIRD
activated by more virulent respiratory pathogens
Canine Herpesvirus 1 (CHV-1)
once considered as a component of CIRD
but now a multi-systemic morbilivirus causing fatal disease
incidence reduced in areas with widely practiced vaccination
CDV
ss RNA betacoronavirus genus of Coronaviridae
closely related to bovine coronavirus and human coronavirus
genetically and serologically distinct from canine coronavirus (enteric)
2nd most prevelent in CIRD
Canine Respiratory Coronavirus (CRCoV)
ss RNA, orthomyxoviridae family, H3N8
closely related to equine influenze virus H3N8
2007, South korea, avian influenza H3N2 associated with outbreaks of respiratory disease in kenneled dogs
development of more pathogenic H3N1 CIV
Risk: Genetic drift and genetic shift
Canine Influenza Virus (CIV)
gram negative, aerobic coccobacillus
normal inhabitant of canine URT
secondary pathogen
80% of dogs with acute respiratory distress
most common: Co infection with CPiV
Bordetella bronchioseptica
gram-positive coccus
sporadic disease in kenneled and racing dogs
Beta hemolytic (complete hemolysis), Lancefield group C bacterium
Chronic nasal discharge rhinitis
Acute hemorrhagic, fibrinosuppurative and sometimes fatal bronchopneumonia
Streptococcus equi subsp. Zooepidemicus
Clinical signs
cough
decrease in appetite
anorexia
usually BA and afebrile on presentation
DIagnosis
HIstory
physical exam
tracheal sensitivity
Diagnostic tests
can be deferred or excluded if mild
CBC/electrolytes
left shift neutrophilia
radiograph
culture sensitivity
PCR
Treatment for respiratory ds.
Antitussive
HYdrocodone - 0.25 mg/kg PO TID - QID PRN
Expectorant
Guaifenesin 3-5 mg/kg PO TID -QID PRN
Antihistamine
Dipenhydramine 2 mg/kg PO BID PRN
Antibiotic
Doxycycline 5-10 mg/kg PO BID 14-21 days
Amoxiclav - 13.75 - 20 mg/kg PO BID 7-21 days
TMPS for Bordetella
Fluoroquinolones for Mycoplasma
Treatment for respiratory ds. Critical care
Steroids/ anti-inflammatory
Opioid
Morphine 0.3 mg/kg IV PRN
Indicated for ARDS (acute respiratory distress syndrome)
Supportive
fluid support
oxygen
multivitamins