Iron, TIBC, and Copper
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
source and occurrence
n Iron (Fe2+, Ferrous) or (Fe3+, Ferric)
n Vital part of erythroid maturation
n Less than 5 grams total in body
n Found in compounds such as
– Hemoglobin: (2500 mg)
– Myoglobin: (300 mg)
– Enzymes
• Catalase: H2O2 decomposition (300 mg)
• Peroxidase: Oxidation (300 mg)
• Cytochromes: Electron Transfer (300 mg)
• Iron-sulfur: Electron Transfer (300 mg)
free vs bound vs stored
free iron can lead to tissue damage
generation of free radicals by reacting with peroxide
transported in the plasma bound to transferrin
stored as ferritin or hemosiderin
intake requirements
RDA for male is 10 mg/day
for females 15mg/day
~1 mg of iron is lost per day (adults)
due to loss of RBCs and intestinal shedding
in females, the menstrual cycle can drain 30 mg of iron
iron metabolism source
– Majority of circulating iron derived form
destroyed RBCs (recycled)
– Intestinal absorption
– Occurs mainly in the duodenum
– Accounts for only 5-10% of daily iron intake
– Dietary, ferric Fe3+ form
• reduced to the ferrous Fe2+ form to be absorbed
– Diet is usually 10-20 mg/day
iron metabolism transport
n Transferrin (4 mg)
– A singled chained polypeptide formed in the liver
– Transports Iron to normoblasts
n Binds iron in the ferric, Fe3+ state
n Delivers iron to cells with transferrin surface
receptors
n 40 mg of iron is transported daily
storage of iron
n Over 65% of the body iron is in hemoglobin
n Stored in the rest of the body as
– Ferritin and Hemosiderin
ferritin (apoferritin)
n A soluble multi subunit protein shell which
surrounds iron atoms
n Takes up iron in the ferrous, Fe2+ state and
oxidizes it to the ferric state
n 1/3 in the liver
n 1/3 in the bone marrow
n 1/3 in the spleen
n Assesses iron storage
n Assays: Immunoassays
n ↓: Sensitive for the detection of iron deficiency
n ↑: In chronic diseases, infection, inflammation
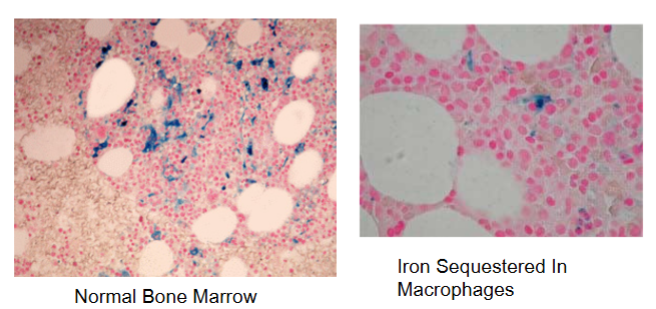
hemosiderin
ferritin which has lost surface tension
is soluble
stains with prussian blue stain
measurement of serum iron
n Specimen Requirements
– SERUM
• do not use EDTA, Potassium oxalate, citrate
– Bind the iron in the specimen
– Avoid hemolyzed serum
n
n Reference Methods:
– AAS
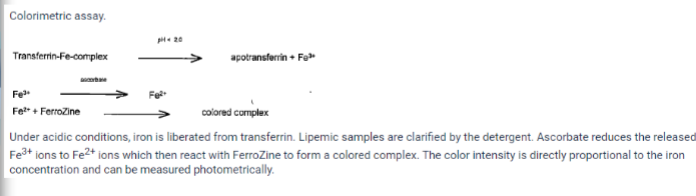
colorimetric methods
n Colorimetric
– Splitting off of Fe3+ from Transferrin by acid;
• HCL, H2SO4, Tricholoroacetic acid (TCA)
– Separation of Fe3+ and protein
– Reduction of Fe3+ Fe2+
• Ascorbic Acid
• Hydrazine
• Thioglycollic acid, Hydroxylamine
– Reaction of Fe2+ with Chromogen
chromogens
– Bathophenanthroline
– Diphenylphenanthroline
– Ferrozine (reference method)
• Method used by Student Lab Instruments
– Tripyridyl triazine (TPZ) pyridylazo dye
measuring iron
the specimen is acidified to release iron from transferrin and reduce Fe3+ to Fe2+ (ferrous iron)
instrumentation methods
n Vitros (Johnson & Johnson)
n Reflectance colorimetry
– 1st layer
• -remove iron from the transferrin by acid
– 2nd layer
• ascorbic acid - Fe3+ Fe2+
– 3rd layer:
• chelate out iron
– 4th layer
• Reagent layer
– Two readings taken-one at 54 seconds and one at
297 seconds
instrument methods: Roche
reference ranges
males - 59-158 ug/dl
female - 37-145 ug/dl
clinical significance of increased serum iron
– Hemolytic anemia
– Sideroblastic anemia
– Primary Hereditary Hemochromatosis
– Iron intoxication
– Iron overload (transfusion)
– Increased Red Cell Destruction
– Ineffective Erythropoiesis
• Following thalassemia
• Lead poisoning
clinical significance of decreased serum iron
n Iron deficiency anemia
– (↓ Hb, Hct, MCV, MCH,
MCHC)
n Inadequate intake
n Chronic Diarrhea
n Malabsorption
n Increased Requirements
n Growth
n Premenopausal Women
n Pregnancy
n Chronic Blood Loss
n Excessive menstruation
n Peptic Ulcer
– Gastritis
n Anemia of Chronic
Diseases
– Infections
– Inflammatory
diseases: SLE, RA
– Malignancies
n Thalassemia
total iron binding capacity (TIBC)
n Reflects Transferrin levels
n Not bound with serum Fe
n Capability of transferrin to binding Fe
n Helpful in the determining cause of iron
deficiency anemia
methodology
n Saturation of transferrin with excess Fe3+
– Ferric ammonium citrate
– Ferric chloride
n Removal of unbound Fe3+
– Precipitation with
• MgCO3
n Centrifuge
n Analyze supernatant for iron
– Measures iron bound to transferrin
n Reaction Sequence for TIBC
– Apotransferrin + free Fe+3 Fe-transferrin + free Fe+3
– Fe-transferrin + Fe+3 + alumina Fe-transferrin +alumina-Fe
n Reference Range 250-450 ug/dl
clinical significance for TIBC increased and decreased levels
n Increased
– Iron deficiency anemia
n Decreased in
– chronic disease
– Infections, inflammation, and malignancy
– Thalassemia
– Hemochromatosis
• Iron storage disease
n Normal in Sideroblastic anemia
percent saturation of transferrin
n Serum iron x 100 = % Saturation
TIBC
n Unsaturated Iron Binding Capacity (UIBC)
n TIBC = UIBC + Serum Iron
n UIBC = TIBC - Serum Iron
n This is latent iron binding capacity
n Only 1/3 of the transferrin binding sites are
normally bound to Fe
plasma ferritin
n Ferritin
– the most sensitive indicator of iron deficiency
n Ferritin levels decline early in anemia and increase
early in chronic diseases
n Methodology
– RIA - Radioimmune Assay
– IRMA - Immunoradiometric assay
– EIA - Enzyme marker
– Flurometric enzyme immunoassay (FPIA-Abbott IMx)
– CHEMILUMINESCENT
n Reference Values for Ferritin
– Male: 15-200 ug/L
– Females: 12-150 ug/L
significance of plasma ferritin levels
n Decreased
– in iron deficiency anemia
n Normal - Increased
– in anemia of chronic disorders and Thalassemia
n Increased
– in Sideroblastic anemia
– Familial Hemochromatosis
laboratory findings in microcytic/hypochromic anemia
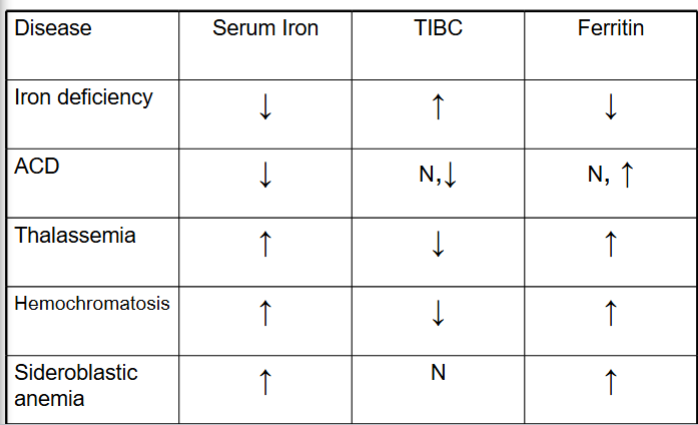
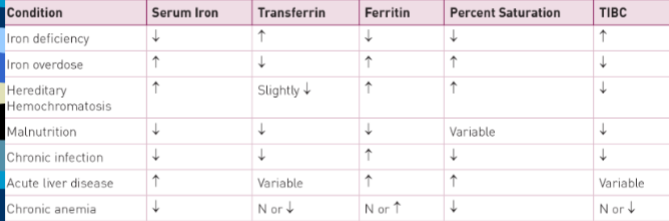
laboratory markers of iron status in several disease states
free erythrocyte protoporphyrin
n Measured by the Zinc Protoporphyrin: Heme ratio or
ZPP/Heme
n Useful in screening for iron deficiency demonstrated
in lead poisoning
n Methodology
– Hematoflurometry
– Hemoglobin is converted to cyanmethemoglobin, measure
light absorbance at 420nm
– Then measure the zinc protoporphyrin at 595 nm
– Reference Values: <80 umol ZPP/mole of heme
– Significance:
• Increased in iron deficiency
copper (functions)
n Function of Copper
• Oxidation reduction reactions
• Involved with the synthesis of hemoglobin
• Formation of collagen
• Maintenance of the myelin sheath skeletal development
• Function of the immune system
• Formation of melanin pigmentation
• Component of
– enzyme superoxide dismutase
– Cytochrome C oxidase
– Tyrosinase
– Ascorbate oxidase
n RDA = 1.5 - 3.0 mg/day
n Transported primarily by ceruloplasmin
measurement of copper
AAS, (flame or electro thermal)
n Reference Values
– Males: 70-140 ug/dl
– Females: 80-155 ug/dl
– Pregnancy: 120-300 ug/dl
– Erythrocytes: 90-150 ug/dl
– Wilsons disease:
• Serum 40-60 ug/dl
• Urine >100 ug/dl
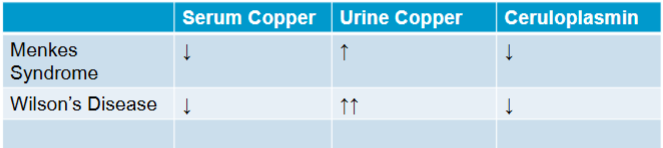
clinical significance of copper
n Deficiency (Rare)
– Wilson’s Disease (Heptolenticular disease)
• Autosomal recessive, ATP-7B gene mutation
• Copper transport is abnormal
• Copper accumulates in the liver, brain, cornea, and
kidney
• Kayser Fleisher rings in the cornea by copper deposition
• Decreased Ceruloplasmin, Increased Urinary copper
– Menke's Steely Hair Syndrome:
• Extreme form of Cu deficiency
• X linked defect in Cu transport and storage
• Decreased ceruloplasmin
– Severe copper deficiency
– Transient deficiencies
• Sprue, nephrosis
increases in copper levels clinical significance
n Addison’s disease
n Hypopituitarism
n Infection
n Lymphoma
n Liver disease
n Pregnancy
n Bronze baby syndrome
– Complication of UV treatment of infants
with jaundice
– Copper-porphyrin conjugates
ceruloplasmin
n Indicator of Copper status
n Function:
– Transport of Copper
– Synthesized in the liver
– An acute phase reactant and involved in the
formation of heme
– Considered an anti-oxidant
measurement of ceruloplasmin
n Colorimetric
– oxidizes a substrate to color change
n Immunoassay
– Immune-Nephelometry
– RID - Radial-Immunodiffusion
– Chemiluminescence
– FLPIA
n Reference Values:
– 15-60 mg/dl
– (excretion is 2-37 g/day)
ceruloplasmin levels
n Increased values
– Rheumatoid arthritis (gives blood a greenish cast)
– Biliary cirrhosis
– Pregnancy
– Oral contraception
– Some infections
– Cancer
n Decreased Values:
– Wilson’s Disease
– Menke’s Steely Hair Syndrome
menkes syndrome vs wilson’s disease