L12 - Coronary Artery Disease and Cardiac Failure
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
48 Terms
_______________ is the most common cause of coronary heart disease
Atherosclerosis
_________ build-up increases the risk of clot formation (coronary artery disease)
Plaque
A PT that has artery stenosis (narrowing) < 60% occuluded results in ____________
Normal coronary blood flow at rest and during exertion
A PT that has artery stenosis (narrowing) of around 70% occluded results in _________________
-normal at rest
-coronary flow reserve is reduced, causing ischemia during exertion,
A PT that has artery stenosis (narrowing) of > 90% occluded results in ____________
ischemia at rest and even worse with exertion
Acute Coronary Syndrome I — spectrum of acute ischemic heart disease ranging from _____________ to ______________
unstable ischemia to acute myocardial infarction (MI)
Acute Coronary Syndrome I is classified based on _____________ on the EKG
ST segment elevation
Acute Coronary Syndrome categories:
_____________ — (no ST elevation)
_____________ — (present ST elevation)
Unstable Angina (UA) and Non-ST Elevation Myocardian Infarction (NSTEMI) — no ST elevation
ST Elevation Myocardian Infarction (STEMI) — present ST elevation
What are the implications of unstable angina being caused by the disruption of atherosclerotic plaque with partial thrombosis?
Acute Myocardial Infarction is imminent (aka Preinfarction)
Characteristics of unstable angina
no serum biomarkers are present
pain
occurs at rest, lasting less than 20 minutes
severe and of new onset, not within 1 month
Characteristics of NSTEMI
type of heart attack, minor artery of the heart is blocked or a major artery of the heart is partially blocked
less serious than a “classic” heart attack
serum biomarkers may be present
Characteristics of STEMI
“heart attack”, is a serious event, one of the heart’s major arteries is blocked
characterized by ischemic death necrosis of myocardial tissue
area of infarction is determined by the affected coronary artery and its distribution of blood flow
elevated ST segment
What are the symptoms associated with STEMI?
severe, crushing pain
constricting chest pain
pain that is not relieved with nitroglycerine
What are the symptoms of STEMI in women?
pain in arms, back, neck, jaw
stomach pain
fatigue
SOB
nausea
lightheadedness
sweating
Acute myocardial infacrtion (AMI) leads to _____________
necrosis (cell death)
What are the serum biomarkers of acute coronary syndrome?
___________ — not cardiac specific (1 through 4-8 hrs)
___________ — highly specific for myocardial tissue
___________ — myocardial tissue specific
Myoglobin — not cardiac specific (1 through 4-8 hrs)
Creatine Kinase MB (CK-MB) — highly specific for myocardial tissue
Troponins — myocardial tissue specific
Identify the following type of chronic ischemic heart disease:
fixed coronary obstruction creates blood flow and metabolic demand mismatch
initial manifestation of ischemic heart disease
not present in all patients due to coronary collateral growth
angina due to exercise, emotional stress; relieved by rest or nitroglycerin
Chronic Stable Angina
Identify the following type of chronic ischemic heart disease:
more common in women
absence of angina
impaired blood flow due to atherosclerosis or vasospasm
observed in people with diabetes due to neuropathies (commonly in elderly)
Silent myocardial ischemia
Identify the following type of chronic ischemic heart disease:
ischemia/angina caused by coronary artery spasm
mechanisms not understood
occurs during rest and at night
associated with migrains and Raynaud’s syndrome
Variant (Vasospastic) Angina
What are the triggers for ischemia?
exercise
assuming upright posture
smoking
cold exposure
mental stress
What are the physiological responses to ischemia?
• ↑ sympathetic activity
• ↑ blood pressure & HR
• ↑ force of cardiac contractility
What is the diurnal variation associated with ischemia?
more cases occur within first hour of waking
What method of revascularization is appropriate to use:
less severe → mild symptoms, mild CAD
normal left ventricle function
Medication
What method of revascularization is appropriate to use:
mild
1-2 vessels are diseased (narrowed)
not fully occluded
ballon angioplasty/STENT
Percutaneous Coronary Intervention
What method of revascularization is appropriate to use:
severe
2-3 vessels are diseased (blocked)
Coronary Artery Bypass Graft (CABG)
________________ — imbalance/failure of the heart to supply blood to meet the metabolic needs of the body
Heart Failure
NYHA Functional Classification of Heart Failure (symptom-based)
Class I — ____________________
Class II — ____________________
Class III — ____________________
Class IV — ____________________
Class I — no physical limitations
Class II — slight limitation of physical activity
Class III — marked limitation of physical activity
Class IV — symptoms at rest
ACC/AHA Heart Failure Stages (disease progression):
Stage A — ________________
Stage B — ________________
Stage C — ________________
Stage D — ________________
ACC/AHA Heart Failure Stages (disease progression):
Stage A — PT at risk for heart failure; no structural disease
Stage B — structural disease; no heart failure symptoms
Stage C — structural disease; heart failure symptoms
Stage D — end-stage disease
_____________ is the most common cause of heart failure
coronary heart disease
Cardiac Output = ______________ x _____________
Heart Rate x Stroke Volume
What influences stroke volume?
preload
contractility
afterload
What are the determinants of cardiac function that can lead to heart failure?
decreased preload (Less blood returning to the heart → less blood to pump out)
decreased contractility (Less force → less blood ejected)
increased afterload (The heart has to push harder → pumps less blood)
decreased cardiac output (caused by the above 3)
What factors reduce/impair preload?
decreased myocardial compliance (cardiomyopathy/hypertrophy)
valvular disorders (mitral valve stenosis)
pericardial disease (compression of heart within pericardial sac)
What factors can reduce/impair contractility?
necrosis of heart muscle following an acute MI
What factors can increase/impair afterload?
hypertension
valvular disorders (aortic valve stenosis)
What are the compensatory mechanisms during heart failure?
increased sympathetic nervous system activity
increased heart rate and cardiac contraction → increased CO
activation of the Renin-Angiotensin-Aldosterone System (RAAS)
increased sodium and water reabsorption in kidneys → increased preload → increased CO
increased catecholamine release
increased heart rate and cardiac contraction → increased CO
_____________ Ejection Fraction (HFREF) — the inability of the ventricle to eject an adequate cardiac output (EF of < 40%)
Reduced
________ Ejection Fraction (HFPEF) — the heart pumps normally but is too stiff to fill properly and eject blood (EF > 50%)
Preserved
Heart failure is classified by _____________ and ________________
ejection fraction
left-sided or right-sided failure
What are the characteristics of diastolic heart failure (HFPEF)?
may be due to sustained hypertension
increased wall thickness leads to a reduced ability to fill
reduced stroke volume, reduced preload
compliance is decreased
Define diastolic dysfunction
resistance to filling of one or both ventricles leading to symtpoms of congestion
What are the characterstics of systolic heart failure (HFREF)?
results from conditions that impair contractile performance (ischemic heart disease)
enlarged ventricles (dilated heart, unable to pump same amount of blood out, increased preload)
Define systolic dysfunction
impaired ability to eject blood at a rate to meet metabolic needs of the tissue
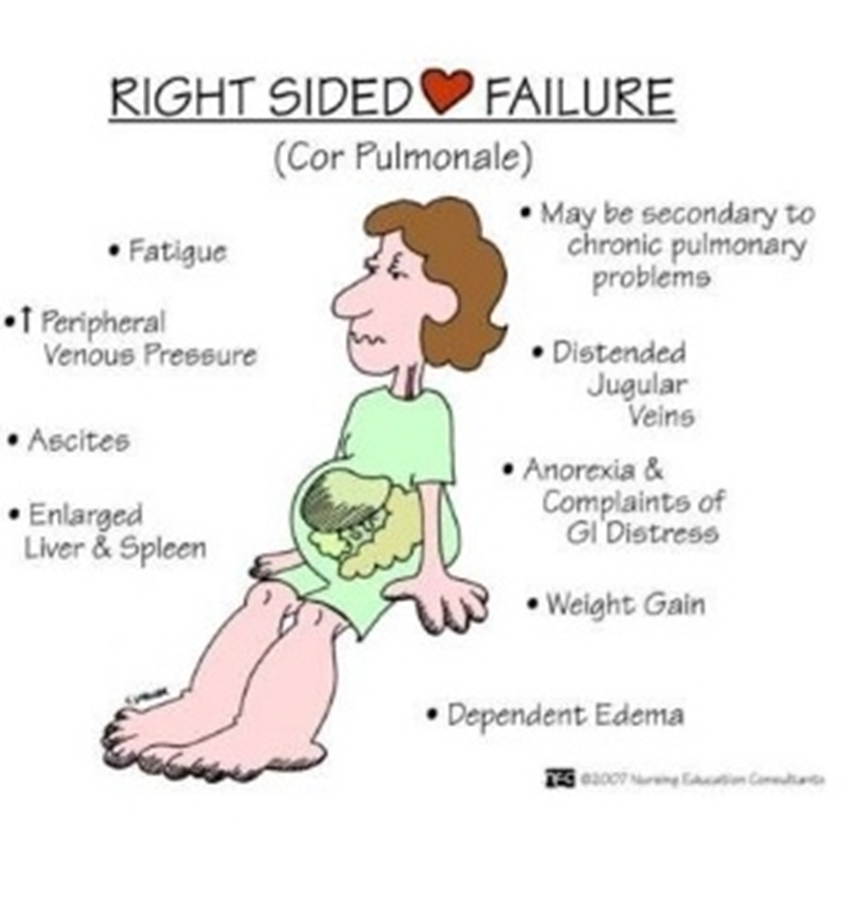
What is the most common cause of right ventricular heart failure (dysfunction)?
left ventricular heart failure (dysfunction), which results in pulmonary hypertension due to left artery congestion
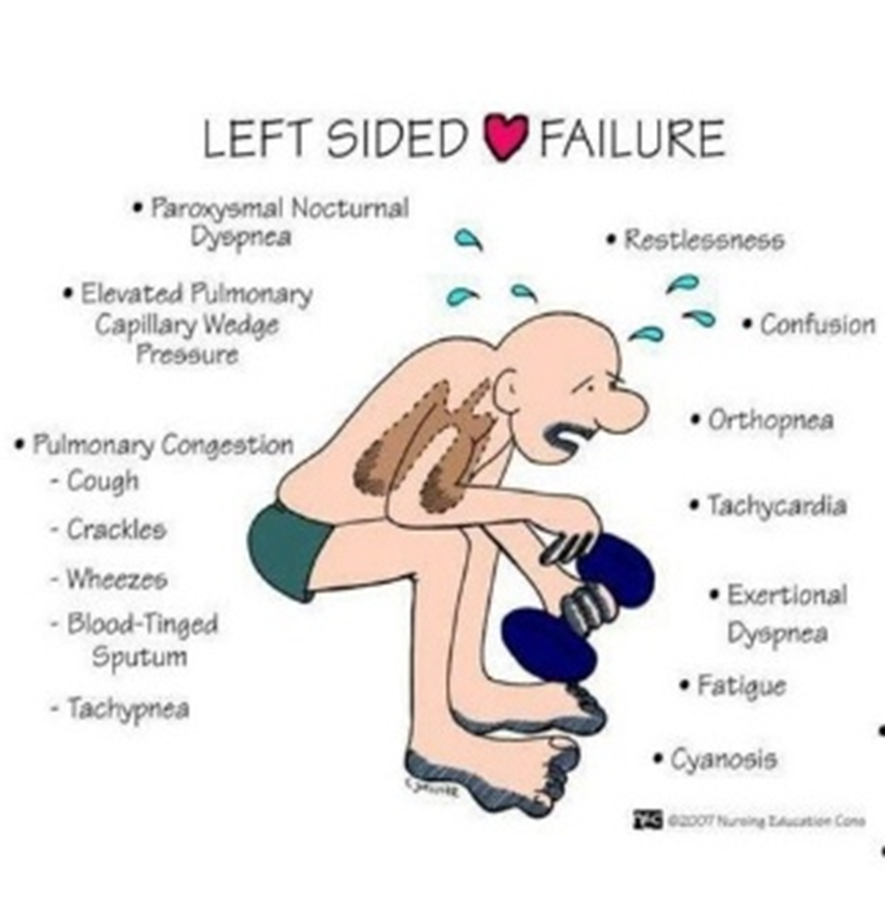
What are the causes of left ventricular heart failure (dysfunction)?
hypertension
myocardial infarction
valve defects (aortic/mitral)
What does right heart failure result in?
congestion of peripheral tissues
liver congestion
GI tract congestion
What does left heart failure result in?
decreased cardiac output
pulmonary congestion
imparie gas exchange
pulmonary edema
What are the signs of heart failure?
fatigue
activity limitation
congestion
edema or ankle swelling
shortness of breath