Responding to GIT symptoms
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
Responding to symptoms general framework
✓ INTRODUCTION : scene setting
✓ ASSESS : take a medical history
✓ EVALUATE: Diagnosis and explanation to the patient (Explains possible cause(s) or triggers)
✓ ACTION: Clinical Decisions and Solutions – formulating an appropriate evidence-based decision (using resources and guidelines) to treat or refer
✓ MONITOR and RISK management: safety-netting, adherence, side effects, precautions, self-care, signposting, appropriate referral to other Health care Professionals etc
✓ CLOSING contacts and questions
✓ CONSULTATION BEHAVIOURS
What resources are available in the responding to symptoms
• RTS Lectures
• Class Pre-work
• Product information
• PIL
• Counter- Intelligence book
• BNF
• Stockleys interactions
• NICE/CKS guidelines
• Frameworks
Describe how you as a Pharmacist should safety net?
-Inform patients about the time course of symptom resolution
-Recommend a treatment plan, including any self-care advice
-Share any diagnostic uncertainty or possible complications
-Inform patients about what exactly to look out for
-Recommend how and where to seek further help - prescriber might be themselves or someone else
-Seek acceptance and confirmation of understanding/commitment
-Summarise the advice
-(Document the advice given)
Patient education
• Top 100 drugs : gastrointestinal, skin, endocrine, cancer, infections, genitourinary
• Using different resources to communicate the following (SPC)
• Using the SPC (or PIL) to provide information
• Side effects / MHRA warnings – more complex/high risk medicines eg carbimazole, insulin administration, biologics
• Managing different patient groups eg language differences, disability, sight impairment, tricky questions from the patient
• Managing Repeat medicines • Checking Adherence
• BRAN Benefits – risks – alternatives – do nothing
• Contextualising risk (1 in 10 etc) and managing risk • Use of Validated tools to explain risks v benefits eg statin charts
• Complex regimens eg COC
• Missed doses and implications eg COC
• Safety netting and monitoring (As themselves as a prescriber or another presecriber)
What does BRAN stand for and what is it beneficial for?
Benefits - Risks - Alternatives - Nothing
• Shared decision-making using BRAN
• Encourage patients get the best from conversations with healthcare professionals by asking four questions • Collaboration based on clinical evidence, patient’s informed preferences and values.
• More than 1 way to treat a problem including ‘no treatment’
• Helps to weigh up risks vs benefits to determine best choice for patient
Questions to consider:
• What are the benefits of the treatment? :
-What can I expect to gain from the treatmen?
-What is the chance of the treatment being successful?
• What are the risks of the treatment?:
• What is the chance the treatment won’t work?
• What are the possible side effects?
• What are the possible complications?
• How might the treatment affect my quality of life?
• What are the alternatives?
• What are the other treatment options?
• What are benefits and risks of the other treatment options?
• Which treatment options should be used first?
• What if I do nothing?
• How will my condition change if I don’t have treatment?
• Will my condition be more difficult to treat later?
Monitoring points you must mention
• Be specific
• what needs to be monitored and why
• Who will do this?
• When? How often?
• Patient questions and concerns
• Use SPC, CKS, NICE, PIL to answer
• State the likelihood (risks) of side effects and provide context
• Use Validated tools to support decision making
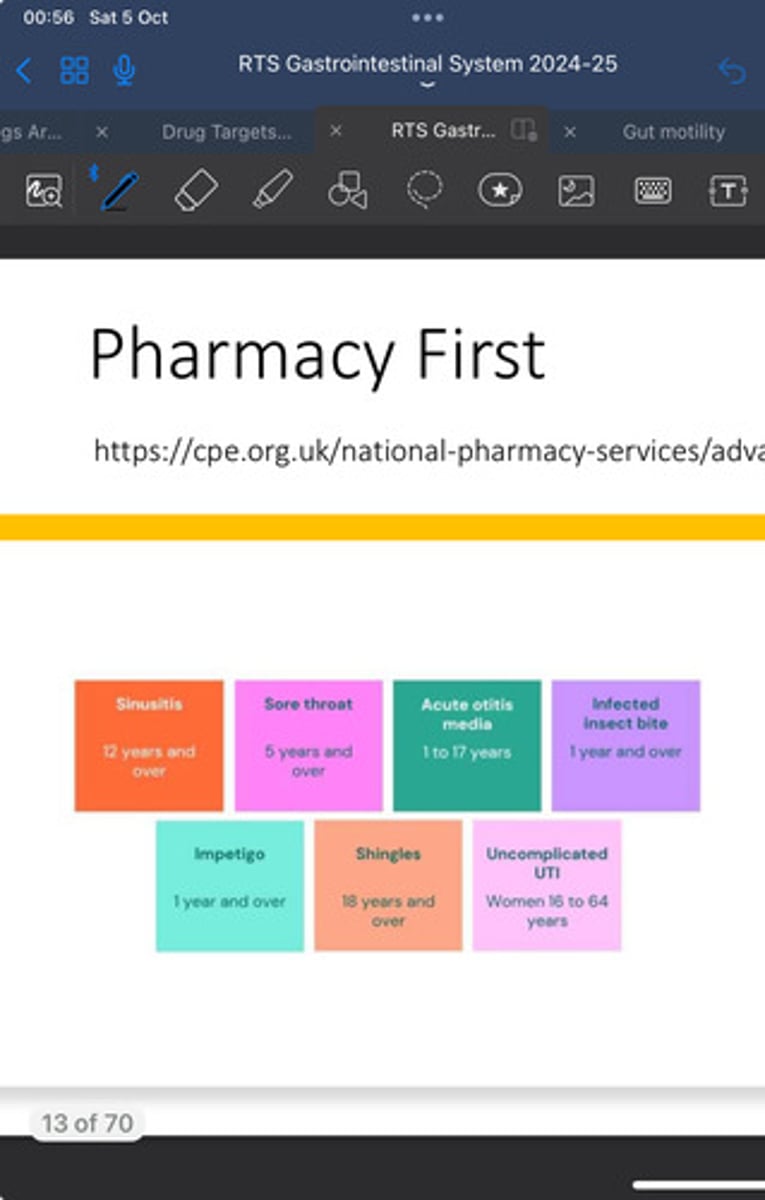
What is the Pharmacy First Service?
-a healthcare initiative in the UK, where people can go directly to their local pharmacy for advice and treatment for minor illnesses without needing to see a GP first. The service covers conditions named in the image - Sinusitis, Sore Throat, Acute otitis media, infected insect bite, Impetigo, Shingles and uncomplicated UTI.
-In the clinical pathway consultations with a pharmacist, people with symptoms suggestive of the seven conditions will be provided with advice and will be supplied, where clinically necessary, with a prescription-only treatment or an over-the-counter medicine
How can we improve sustainability in pharmacy?
Here are some ways to improve sustainability in pharmacy:
- *Reduce pharmaceutical waste*: Implement programs for the safe disposal of unused or expired medications to prevent environmental contamination.
- *Encourage green pharmacy practices*: Promote the use of eco-friendly and biodegradable packaging, reducing plastic use and carbon footprints.
- *Optimize energy use*: Improve energy efficiency in pharmacies by using energy-saving lighting, equipment, and appliances.
- *Promote digital prescriptions*: Shift towards electronic prescriptions and records to reduce paper waste.
- *Support sustainable supply chains*: Source medications from suppliers that prioritize environmentally friendly production processes and reduce transportation emissions.
- *Educate patients*: Encourage patients to return unused medicines and educate them on the environmental impact of improper drug disposal.
- *Adopt sustainable procurement policies*: Choose suppliers with environmentally responsible practices and products that meet sustainability criteria.
- *Sustainable compounding and production*: Reduce the use of hazardous chemicals in drug production and focus on sustainable compounding practices.
GI History taking method?
SOCRATES
• Site (location, site of any pain?)
• Onset (how and when did it appear? gradual or sudden?)
• Character (describe symptom, come and go or constant?, describe any pain is it sharp, dull, throbbing?)
• Radiation (Pain felt elsewhere?)
• Associated symptoms Are there any other symptoms that seem associated with the pain? • Eg vomiting associated with bowel obstruction, bleeding in bowels – what colour?, fever?
• Timing How has the pain/symptoms changed over time? Have you had similar symptoms like this in the past?
• Exacerbating and relieving factors (what makes symptoms better or worse? Eg GORD worse lying flat but better with antacid)
• Severity (on a scale of 0-10, how would you rate your symptoms, pain etc?)
Best source to find Red Flag symptoms for a disease
CKS will list the red flag symptoms
What is constipation, and speak about its prevalence ?
• Infrequent bowel movement with a sensation of pain and incomplete evacuation, often accompanied by straining and the passage of small, hard stools
Note: NICE – defines normal bowel habits as passing stools between three times a day and three times a week
Prevalence:
• Increases with age • Women> men • Pregnancy (upto 38%)
What are the causes of constipation?
Poor fibre intake, diet, water, sedentary lifestyle , pregnancy, medications eg codeine, antacids containing aluminium, iron supplements, diuretics, long term laxative usage, IBS, cancer
State some red flag symptoms of Constipation
New or worsening symptoms , weight loss/fatigue, Blood in stools (red/black etc) Age > 40 yrs with major change in bowel habit → Colorectal cancer?
Treatment of Constipation
• Consider efficacy vs speed of treatment
• Formulations – fibre drink, liquid, tablets, suppositories
• Advise on lifestyle measures, such as increasing dietary fibre, fluid intake, and activity levels
• offer treatment with oral laxatives using a stepped approach.
• Dose titration to produce soft formed stools at least 3 times/week without strain
BOSS:
1st line: Bulk forming laxative eg isphagula husk, bran . Increases mass of stool. Work within 24-36 hours – plenty of water. Avoid at bedtime - as you are lying down so we don't want faeces getting lodged in the stomach area. First line.
NOTE: When a patient has Opioid induced constipation, we do not use Bulk Forming Laxatives as it can cause Faecal impaction - Faeces gets blocked in the gut and doesn't travel down (use osmotic / stimulant laxative)
2nd line: • Osmotic Laxative eg macrogol or lactulose. Retains fluid in bowel. Onset – upto 2-3 days but gentler action. Can be used in children / pregnancy/ breast-feeding . Side effects : flatulence /cramps (20% patients but reassure – will settle
3rd line: -Stimulant laxative eg bisacodyl, senna , sodium picosulfate, docusate sodium • Stimulate nerve endings in bowel to promote movement of faeces. Fast onset (8-12 hours) .Adults should take at night. Can cause abdominal cramps. Short term use only. Not for children /pregnancy
4th line: • Stool softener eg glycerine suppositories and docusate sodium. Lubricates
• If patient asks for Liquid paraffin – discourage use
• POM : Prucalopride – if symptoms persist, short term trial ,prescribing criteria
What should be considered in patients with constipation?
• Pregnancy
• Older patients
• Laxative use in children • Opioid induced constipation (avoid bulk forming, use osmotic / stimulant laxative)
• Faecal impaction
• Laxative abuse
List Lifestyle advice for constipation
• Diet – plenty of fruit and vegetables.
• Aim for 30g fibre/day (adults)
• Increased fluid consumption (water)
• Regular exercise
• Avoid holding back the urge to pass a motion
What are the risk factors to Bowel cancer (lower GI) - (Colorectal cancer - Colon / Rectum)
Risk Factors:
• age – almost 9 in 10 people with bowel cancer are aged 50 or over
• family history
• Underlying medical condition eg IBD (UC/Crohn’s disease)
• Modifiable Risk Factors • diet - Red or processed meats and low in fibre
• weight – more common in overweight or obese people
• exercise – inactivity increases risk
• alcohol
• smoking
What are the red flag symptoms for Bowel (Colorectal) cancer?
• Bleeding from the back passage without a reason - patients can become anaemic where patients Iron or Haemoglobin levels have dropped, Patient may also look drained and pale
• A persistent change to normal bowel habits, such as diarrhoea, constipation or passing stools more frequently than usual
• Abdominal pain
• Unexplained weight loss / loss of appetite
• Bloating, swelling, pain or an unexplained lump in the tummy
• Tiredness or looking pale/anaemia :
• Age 40 years and over with unexplained weight loss and abdominal pain; or
• Age 50 years and over with unexplained rectal bleeding; or
• Age 60 years and over with changes in their bowel habit;
• Repeat purchases of haemorrhoid medicine or loperamide without diagnosis.
• Any symptom that persists could indicate cancer, e.g. bowel changes that have lasted more than 3 weeks
How do we screen for bowel cancer?
-The Faecal Immunochemical test (FIT) - a type of faecal occult blood test used to detect traces of human blood in stool samples
-Occurs when you turn 60 years old
What is Diarrhoea and what is happening in the body when it is occuring?
• Frequent bowel movements of a watery consistency with a sensation of urgency.
• Often accompanied by abdominal pain and cramps
• Vomiting and headache can be present
• Occurs when lining of large intestine becomes inflamed preventing sufficient fluid absorption from food in the intestine
What are the causes of Acute Diarrhoea?
• Comes on suddenly
• Range 5-10 days upto 4 weeks
• Viral infection eg norovirus / rotavirus
• Bacterial infection eg Salmonella,E.coli or Parasite
• Infected water “traveller’s diarrhoea”
• Stress or anxiety
• Alcohol / coffee
• Medications eg antibiotics and antacids containing magnesium
What are the causes of Chronic Diarrhoea, Lasts> 4 weeks?
• Bacterial or viral
• Overuse of laxatives
• Poor diet
• Long term conditions:
• IBD - Irritable Bowel Disease (Ulcerative colitis, Crohn’s disease)
• IBS - Irritable Bowel Syndrome,
• Malabsorption Syndromes (lactose intolerance, coeliac disease)
• Bowel Cancer
• Faecal Impaction
List the consequences of Long term Diarrhoea
• Dehydration - Pinch test of skin, look pale, confusion, poor articulation, don't use the toilet to urinate a lot
• Mild:
• Less than 5% of body fluid is lost, and a patient may have the following symptoms:
• Headache , nausea, postural hypotension (low blood pressure upon standing, often seen as light headedness or dizziness), tiredness
• Moderate
• Between 5-10% of body is fluid lost
• dry mouth, lethargy or tiredness, muscle cramps, oliguria (decreased urine output), sunken eyes.
• Severe:
• More than 10% of body fluid is lost
• reduced skin turgor – the pinch test, where pinched skin takes longer than two seconds to return to its normal position
• Shock, confusion, oliguria or anuria (failure to produce urine).
Note: Infants – rapidly dehydrate
In RTS what questions should be considered when you suspect Diarrhoea?
• Age /Duration/Symptoms/Causes
• Important to ask about medicines - new, changes
• Altered bowel habit
What are the Red Flag symptoms - REFER?
• Drowsiness or confusion
• Passing little urine
• If symptoms not improved after taking anti-diarhoeals (within 48 hours)
• If symptoms in children under 12 years and elderly
• Diarrhoea usually lasts 5-7 days, and in most children stops within 2 weeks.
• Vomiting usually lasts 1-2 days, and in most children stops within 3 days.
• Sunken fontanelle in babies/ young children
• Dehydration ,lethargy ,dry mouth ,loose skin, sunken eyes
• Fever & patient has been abroad recently
• Bloody, black , mucus stool
• Severe abdominal pain or rectal pain
How do we treat Diarrhoea ?
• Drinking fluids
• Oral rehydration therapy eg dioralyte
• Replaces lost electrolytes, reduces dehydration
• Reconstitute with fresh water
• Suitable for babies and children
• Antidiarrhoeals eg Loperamide hydrochloride 2mg
• Loperamide binds to the opiate receptor in the gut wall
• Reduces propulsive peristalsis (Loperamide slows down the movement of the intestines), increases intestinal transit time and enhances resorption of water and electrolytes. Loperamide increases the tone of the anal sphincter, which helps reduce faecal incontinence and urgency
-Fast onset of action
• Not suitable for < 12 years old
• Forms – capsules, melts, liquicaps etc
Avoid: Kaolin / morphine, bismuth subsalicyclate
What is the drug Enterosgel used for and MOA?
• Enterosgel is a clinically proven treatment for IBS with diarrhoea (IBS-D) and acute diarrhoea
• All-in-One Symptomatic Treatment of: • Diarrhoea • Urgency • Bloating • Abdominal pain
MOA:
Targets the cause of the gastrointestinal symptoms by binding to bacterial toxins and other harmful substances and expelling them from the body via the stool'
Note: ENTEROSGEL® is expelled from the body with the stool, this way eliminating the adsorbed toxins and harmful substances,which can be beneficial for treatment of indicated conditions of acute diarrhoea and chronic IBS diarrhoea
Safe for Children 1+
What is sign posting in pharmacy?
the process of directing patients to other health and care providers for advice, treatment, or support that the pharmacy cannot provide
What selfcare advice will we give Diarrhoea patients ?
• To prevent further infection:
• Good food hygiene , Wash hands, Clean and disinfect toilet
• Advise that children should not attend school or other childcare/social settings until at least 48 hours after the last episode of diarrhoea or vomiting.
• Drink water regularly, rest
• BRAD diet : Bananas ,rice ,apples ,dry toast. No need to avoid solid food.
• Avoid dairy, spicy foods, high in fibre, fat or alcohol
• Probiotics - microbiomes, Lactobacilli
-Babies Should continue with breast or bottle milk
-Vaccinations - Rotavirus
What is irritable bowel syndrome (IBS) and what are the symptoms?
• Chronic non-inflammatory bowel condition (note: IBD is inflammatory whereas IBS is non-inflammatory)
Symptoms:
• Recurrent abdominal pain / cramps
• Changes in bowel habit
• Alternating constipation / diarrhoea
• Abdominal discomfort or distention
• Passage of mucus in stools , bloating
• Flatulence, faecal urgency
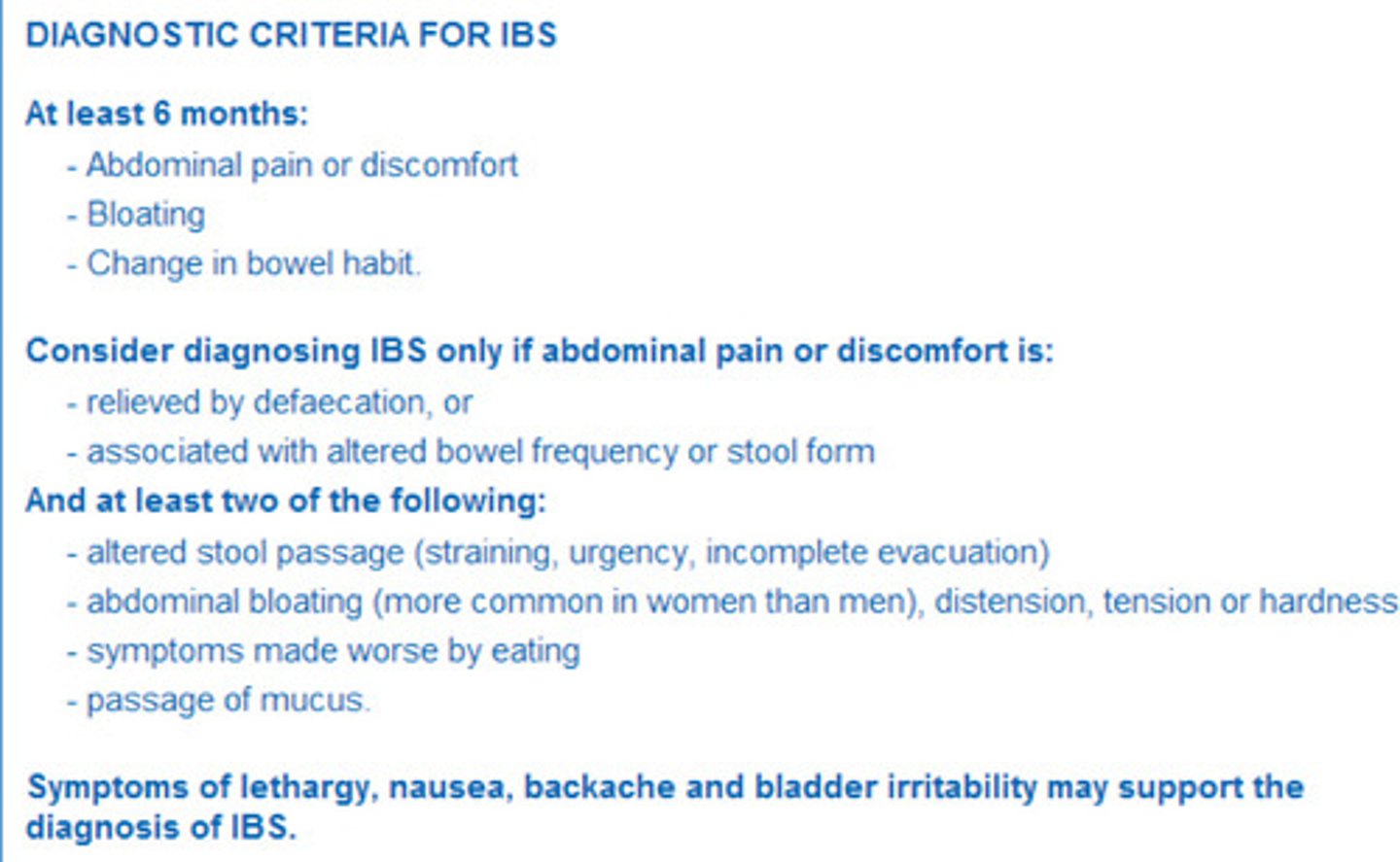
What are the Diagnostic Criteria for IBS
-good for patients to keep a trigger diary to understand why they are getting IBS
What is a Colonoscopy?
a medical procedure that allows a doctor to examine the inside of the colon, rectum, and anus to check for abnormalities or disease
When you suspect IBS when would you refer?
• Anyone who presents with symptoms and have not had IBS confirmed by GP
• Danger Symptoms
• Rectal bleeding with change in bowel habit →? GI cancer
• PMS, endometriosis, , diarrhoea due to infection, IBD or medication
• GI condtions eg gallstones, GORD, pancreatitis
How do we treat IBS
Treated dependent on the cause - sometimes patients need multiple treatments.
• Dependant on presenting symptoms:
❖ Bulk forming laxative eg isphagula for constipation
❖ Anti-diarrhoeals eg loperamide
❖ Antispasmodics (when patients have bloating/ spasms in their gut) eg mebeverine, alverine citrate ,hyoscine butylbromide (Buscopan) – abdominal pain
❖ Peppermint oil – direct relaxant on smooth intestinal muscle.
❖ Antiflatulents eg Simeticone – symptomatic relief of flatulence, wind pain, bloating
❖ Enterosgel
Also :
• Psychological interventions via referral CBT, Hypnotherapy
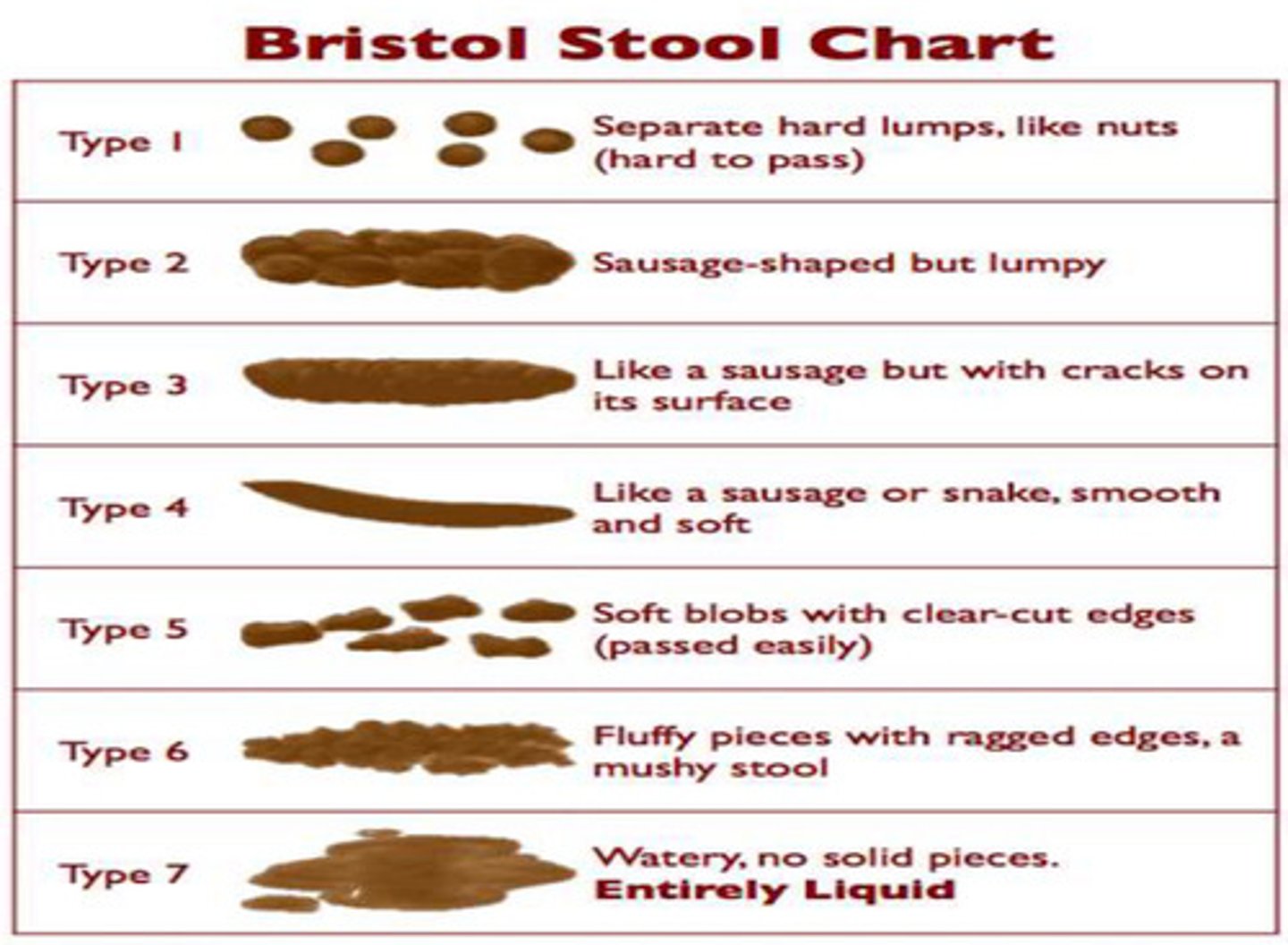
What is the Bristol Stool Chart?
a chart that characterizes different types of stool based on size shape and consistency
-Normal is Type 3 and Type 4!
What selfcare advice, referrals and signposting would be given for IBS
• Exercise
• small regular meals
• fibre? , adequate fluid intake , low fat , cut out processed foods. Probiotics?
• Symptom diary – monitor triggers eg foods, stress, hormonal
• Quit smoking
Referral: Dietician - Low FODMAP Diet:
-An elimination Diet
-Should only be attempted with a nutritionist
-Eliminates Oligosaccharides and Disaccharides from the patients body for a period of time to let the gut rest and slowly reintroduced.
Signposting:
-You can also refer your patient to IBS networks to get more information and support
Define Nausea - this is not a condition but a symptom
queasy feeling a person gets before being sick or throwing up
Define Vomiting - this is not a condition but a symptom
body's way of getting rid of stomach contents it feels may be causing harm
What are some common causes of nausea and vomiting
Internal Causes:
-Headaches
-Infection eg Norovirus, Gastroenteritis (a transient disorder due to enteric infection, usually caused by viruses, characterized by sudden onset of diarrhoea, with or without vomiting)
-Brain tumour
-Heart attack
-Severe Pain
-Abdominal Sources
-Pregnancy
-cancer
External Causes:
-Motion Sickness
-Alcohol Poisoning
-Food Poisoning
-Medicines
-stress
-allergy
-overeating
-bulimia (an eating disorder characterized by regular, often secretive bouts of overeating followed by self-induced vomiting or purging, strict dieting, or extreme exercise, associated with persistent and excessive concern with body weight)
What advice should you offer a pregnant woman with nausea and vomiting?
Offer advice on sources of information and support, such as:
-The NHS leaflet
-Pregnancy sickness support
-The Royal College of Obstetricians and Gynaecologists
-The UK Teratology Information Service
-Reassure that mild-to-moderate symptoms are common in pregnancy and usually resolve by 16–20 weeks of gestation.
Advise on the following self-care measures for mild-to-moderate symptoms:
-Rest as needed, and try to avoid sensory stimuli that may trigger symptoms, such as odours, heat, and noise.
-Try eating plain biscuits or crackers in the morning.
-Try eating bland, small, frequent protein-rich meals which are low in carbohydrate and fat.
-Cold meals may be more easily tolerated if nausea is smell-related.
-Drinking little and often, rather than large amounts.
-Ginger
-Acupressure
-Advise avoiding medications that may contribute to symptoms
-Advise on the management of associated gastro-oesophageal reflux disease, oesophagitis, or gastritis symptoms
-Advise on the need for urgent medical review if the woman develops clinical features suggesting a complication or alternative cause for symptoms
-Advise that for any subsequent pregnancy, early use of lifestyle measures and antiemetic drug treatment before or immediately at the start of symptoms may be helpful.
When should we refer when a patient has Nausea and Vomiting ?
Pregnancy - if nausea and vomiting persists
Other causes:
Dehydration (following ORT), head injury ,Infection, food poisoning eg E.coli
Advise parents/carers on the need for follow up and to seek urgent medical advice if a child has:
-Any features requiring hospital admission or assessment.
-Any new features requiring stool culture testing, such as blood, mucus, and/or pus in the stool (suggesting possible dysentery)
-Symptoms that do not resolve within the expected timeframe — arrange stool culture testing and consider whether an alternative diagnosis is possible. (• Diarrhoea usually lasts 5–7 days, and in most children stops within 2 weeks.
• Vomiting usually lasts 1–2 days, and in most children stops within 3 days)
URGENT REFERRAL:
• Blood in the vomit (bright red or looks like 'coffee grounds’) - GI bleed? Ulcer?
• Severe headache or stiff neck – Meningitis?
• Sepsis
• Lethargy, confusion or decreased alertness – severe dehydration?
• Severe abdominal pain – Appendicitis?
• Temperature above 40C (104F) , rapid breathing or pulse
How do we treat Nausea and Vomiting?
List some Selfcare advice
Signposting?
TREATMENT: Antiemetics (usually actually antihistamines - They are not all interchangeable!!)
• Prochlorperazine, buclizine (migraine)
• Promethazine ,cinnarizine , hyoscine (travel sickness)
• Bismuth subsalicylate (nausea due to dyspepsia)
• Acupressure bands (travel sickness, morning sickness in pregnancy)
• Oral Rehydration Therapy
Self-care:
• Small, frequent sips of water
• Small meals if possible
• Food handling and storage
• Ginger tea/biscuits/acupressure bands (devices that apply gentle, constant pressure to specific points on the body to stimulate acupoints, to relieve the feelings of nausea)
• Hand hygiene
Signposting:
-NHS leaflets/website
What are the worms involved in threadworms ?
Enterobius vermicularis
What is the Threadworm cycle?
1.Eggs: Threadworm eggs are too small to see without a microscope, but they can cause an itch around the anus. This is because the mucus that surrounds the eggs irritates the skin.
2. Hatch: If the eggs are swallowed, they hatch into larvae in the gut.
3. Threadworms mature: The larvae take 1–2 months to mature into threadworms.
4. Adult worms lay eggs: Before the adult threadworms die, they lay more eggs around the anus. This usually happens at night.
5. Eggs are spread: The eggs can get on fingers and under fingernails, and can be swallowed again. This can cause the cycle to continue.
Reinfection: Children can reinfect themselves if they touch their bottom and then put their fingers in their mouth
How do we treat threadworms and when would we refer?
• Anthelmintics eg mebendazole 100mg tabs/suspension
• Advice to prevent recurrance
• Treat whole family, hygiene measures
• cut fingernails
• second dose after 2 weeks if infection not cleared.
• not < 2 years old
Refer: Patients with secondary complications
What are haemorrhoids (piles)?
Swellings that contain enlarged blood vessels found inside or around rectum and anus
Note: Patients with constipation have an increased likelihood of getting piles due to the straining
Symptoms of haemorrhoids (piles)
• Anal Itch
• Bleeding after passing a stool (bright red blood)
• Lump hanging down from anus
• Soreness, redness and swelling around anus
• Incomplete defaecation sensation
Who is at risk of haemorrhoids (piles)
Obese, persistent constipation, regular lifting heavy objects, prolonged sitting ,pregnant,> 45 years old, family history
How do we treat haemorrhoids (piles) and when do we refer, Selfcare ? and Signposting?
Depends whether the Piles are internal or external.
External: Creams (to reduce the capillaries and the piles will go away)
Internal: Suppositories (can sometimes contain hydrocortisone to reduce inflammation)
OR combination of both
Treatment:
• Self-limiting
• Topical formulations – ointment, suppositories
• External and internal use formulations
• Anaesthetics eg lidocaine
• Allantoin
• Zinc Oxide
• Hydrocortisone
• Bismuth
• Treatment in Pregnancy
REFER:
• Persistent rectal bleeding / unresolved piles
• Prolapse (occurs when the muscles and connective tissues of the pelvis weaken and can no longer support the pelvic organs)
• Severe pain/fever
Selfcare:
• Increase fibre in diet
• Plenty of water
• Avoid medication which causes constipation
• Exercise / lose weight
Signposting: NHS website/leaflets
What is "Dyspepsia (indigestion)"?
Term used to describe a range of symptoms including:
• Pain/discomfort in upper abdomen (stomach, oesophagus or duodenum)
• Regurgitation food or acid reflux
• Nausea and vomiting related to eating
• Sour or acid taste (like bile)
• Fullness, bloating, wind • Heartburn
Note:
• Symptoms come and go eg after spicy meal
What are the triggers of Dyspepsia?
Smoking, heavy or spicy meals, eating near bedtime, alcohol, medications eg NSAIDs, being overweight , pregnancy, tight clothing around waist
Conditions linked to cause Dyspepsia ?
• Non ulcer or functional dyspepsia (NUD) (most common cause of dyspepsia, endoscopy detection)
• Gastro-oesophageal reflux disease (GORD) - acid reflux
-Peptic ulcer disease (gastric or duodenal) (PUD)
• Hiatus hernia
• Duodenitis and gastritis • Infection with Helicobacter pylori
• Medication: NSAIDs, digoxin ,steroids ,iron, calcium antagonists,nitrates ,theophyllines, bisphosphonates
• Pregnancy
When to refer when we suspect dyspepsia?
• GI bleeding (bright red or "coffee grounds" in vomit), dysphagia, unintentional loss of weight ,persistent vomiting, black "tar" stools
• Cardiac pain (often mistaken for dyspepsia) pain radiating down arm, not relived by antacids, related to eating ,exercise
• Patients > 55 years urgent investigation with unexplained, unresponsive to treatment (? gastric /oesophageal cancer)
• Recurring indigestion
• Also Refer / consider:
• Medications ADR: NSAIDS, iron, bisphosphonates , corticosteroids
• IBS (change in bowel habit, bloating)
• Motility disorders
• Biliary Colic
How do we treat Dyspepsia?
• Simple & combination antacids:
-Containing aluminium & magnesium salts, calcium carbonate or sodium bicarbonate
• neutralise acid, fast symptomatic relief, short acting.
• Take after meals or at bedtime .
• Avoid taking with other medications.
• Combinations salts (magnesium & aluminium) less likely to cause GI upset (Mg – diarrhoea ; Al – constipation when used alone)
• Alginates (e,g, Gaviscon) - “rafts” or foam barrier to minimise acid reflux - Can be used in pregnancy
• Take with or after food
• Bismuth subsalicylate – coat the stomach lining to prevent irritation and minimise nausea
For Patients that need something more :
• H2 Antagonists (can take a couple of days to work)
• inhibit stomach acid production.
• Up to 12 hours relief. Short term use (6 days)
• Only > 16 years old
• Not for use in pregnancy / breast feeding/ liver or renal impairment
-Proton Pump Inhibitors (PPI) – eg omeprazole, pantoprazole & esomeprazole
• supress acid within 1-2 hours and build to affect after 2-4 days.
• Short term use – up to 14 days OTC
• Only > 18years old.
• Not for use in pregnancy (omeprazole) / breast feeding/ liver or renal impairment
What is Gastro-oesophageal reflux disease (GORD)?
Unpleasant burning feeling felt behind breastbone (heartburn) often accompanied by a sour or bitter taste in the throat caused by reflux of GI contents into the oesophagus.
What complications can occur due to oesophagitis?
• Oesophageal stricture
• Barrett's oesophagus
• Oesophageal cancer
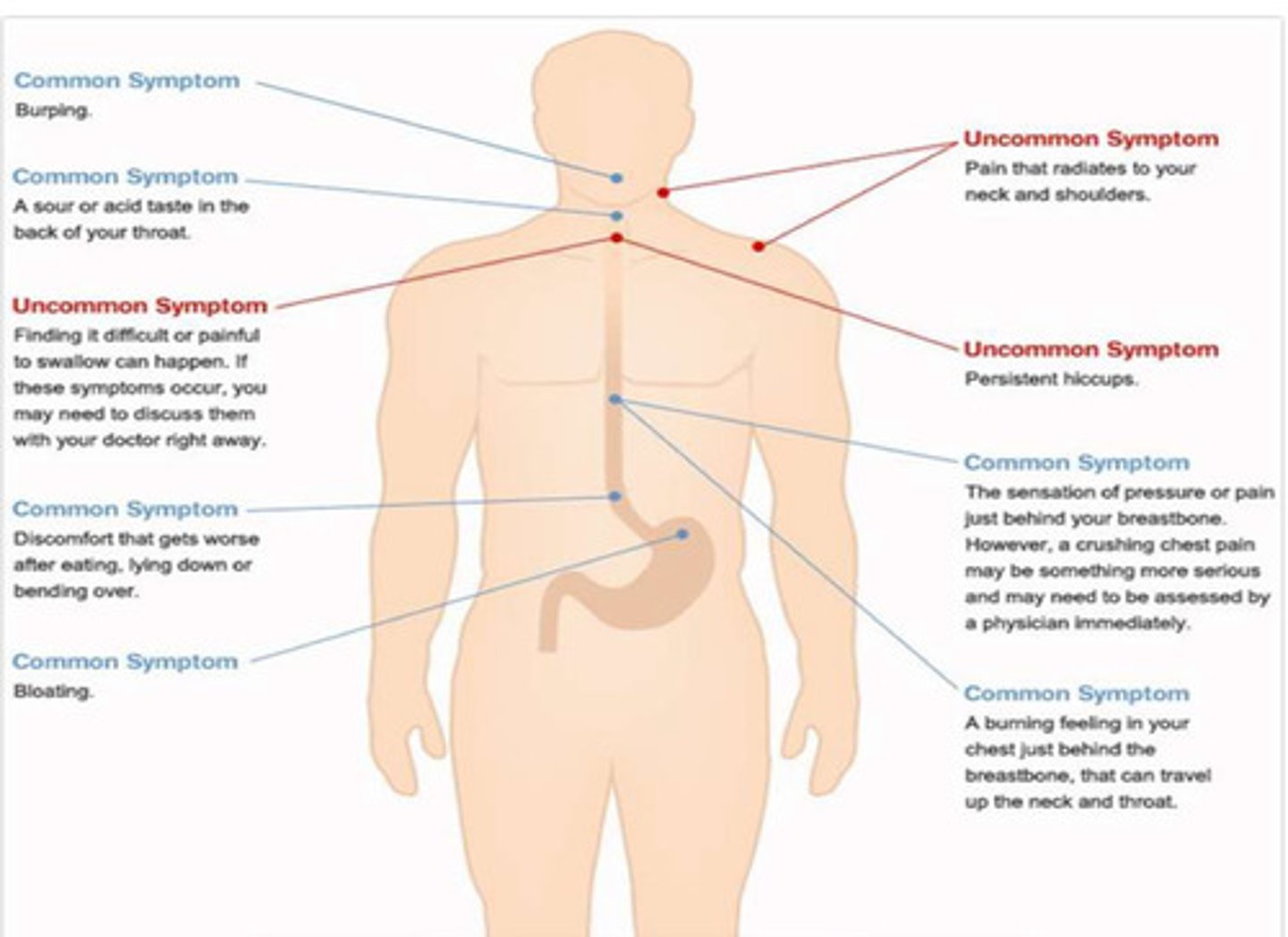
Symptoms of GORD
Uncommon symptoms are RED FLAG SYMPTOMS
How do we treat GORD in infants
-Gaviscon infants
Frequent in < 6 weeks old
• Spontaneous resolution often at 12-18 months
• Half of babies < 3months bring up food at least once / day.
• Refer to GP / Health visitor if any feeding difficulties/failure to thrive
What is non-ulcer dyspepsia? (NUD)
-When the diagnosis made by the endoscopy shows normal results
-No particular reason for it
-Can be treated with H2 antagonists or PPI
• Reassurance and lifestyle changes
What is Peptic Ulcer Disease
Gastric or duodenal ulcers (peptic ulcer disease) describe a breach in the epithelium of the gastric or duodenal mucosa, which is confirmed on endoscopy
-Can occur with patients that use NSAIDs long term with no PPI