Ch 3: Gallbladder
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
Where is the gallbladder located and how is it classified anatomically (intraperitoneal vs retroperitoneal)?
Posterior to the right lobe of the liver within the gallbladder fossa; it is an intraperitoneal organ.
What is the most reliable sonographic landmark for locating the gallbladder fossa?
The main lobar fissure.
What is the function and basic shape of the gallbladder?
A pear-shaped sac that stores and concentrates bile produced by the liver.
What are the three layers of the gallbladder wall from inner to outer?
Mucosal layer (with folds and rugae), fibromuscular layer, and serosal layer.
What are the anatomic parts of the gallbladder and how does it connect to the biliary tree?
The gallbladder has a neck, body, and fundus; the neck connects to the cystic duct, which joins the common hepatic duct to form the common bile duct.
Where do gallstones most commonly collect and why?
In the fundus, because it is the most dependent portion of the gallbladder.
What supplies blood to the gallbladder?
The cystic artery, typically a branch of the right hepatic artery.
What hormone causes gallbladder contraction and when is it released?
Cholecystokinin (CCK), released by duodenal enteroendocrine cells when chyme leaves the stomach and enters the duodenum.
What is the most common gallbladder shape variant and key named variants that may be tested?
Phrygian cap is the most common variant (fold at gallbladder fundus); other named variants include bilobed (dumbbell/figure-eight shape), Hartmann pouch (outpouching of the neck), and junction fold (fold at the gallbladder neck).
What gallbladder anomaly can lead to torsion, and what is the key sonographic sign?
A floating gallbladder can twist its blood supply, causing gallbladder torsion; the key sonographic sign is the whirlpool sign (spiral appearance of the cystic artery on color Doppler).
What positional and developmental anomalies of the gallbladder are important for boards?
Interposition (gallbladder located between liver and abdominal wall instead of posterior to the right lobe), duplication (two gallbladders present), floating gallbladder (suspended by a mesentery, risk for torsion), septate gallbladder (internal septations dividing the lumen), agenesis or hypoplasia, left-sided gallbladder (located to the left of the falciform ligament), midline or right lower quadrant gallbladder (abnormal position), and intrahepatic gallbladder (completely surrounded by hepatic parenchyma).

Normal variant of GB
Phrygian cap
Normal variant of GB
Septate GB
Normal variant of GB

Bilobed GB (dumbbell sign)
Two normal variants of GB
Hartmann pouch and phrygian cap

Normal variant of GB which may mimick a cystic liver lesion
Intrahepatic GB, which is one type of ectopic GB.
Other forms of ectopic GB include left-located (to the left of the falciform lig), RLQ, retroperitoneal
What are the normal size parameters of the gallbladder, and when should obstruction be suspected?
Normal length is 8–10 cm and diameter should be ≤4–5 cm; a transverse measurement >4 cm should raise concern for biliary obstruction.
What is the normal gallbladder wall thickness and why is it important?
The wall should measure ≤3 mm; focal or diffuse thickening suggests pathology.
Which laboratory values are most useful in suspected gallbladder or bile duct disease?
Alkaline phosphatase (ALP) and bilirubin are the most helpful; others include GGT and WBC count (signal cholecystitis).
What are important causes and considerations in gallbladder non-visualization?
Most commonly prior cholecystectomy; recent cholecystectomy may show residual fluid in the gallbladder fossa.

Thickend GB wall (>3 mm)
What is cholelithiasis and what are gallstones typically composed of?
Cholelithiasis refers to biliary stones within the gallbladder; gallstones are typically composed of cholesterol, calcium bilirubinate, and calcium carbonate.
Which patients are at highest risk for developing cholelithiasis?
Cholelithiasis is more common in patients who are fat, female, fertile, flatulent, fair, and forty (the six F’s).
What are the typical clinical presentations of cholelithiasis?
Often asymptomatic; when symptomatic, biliary colic, abdominal pain after fatty meals, epigastric pain, nausea and vomiting, and pain radiating to the right shoulder.
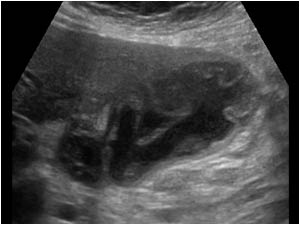
What are the classic sonographic features of cholelithiasis?
A mobile echogenic structure within the gallbladder lumen that produces posterior acoustic shadowing; may or may not demonstrate twinkle artifact.
What is the wall-echo-shadow (WES) sign and when does it occur?
It occurs when the gallbladder is completely filled with cholelithiasis; only the gallbladder wall and posterior shadowing are visualized.
How can the twinkle artifact assist in identifying cholelithiasis?
Twinkle artifact occurs posterior to a strong granular or irregular surface and can help detect small stones in the gallbladder neck or differentiate an adhered stone from a gallbladder polyp.
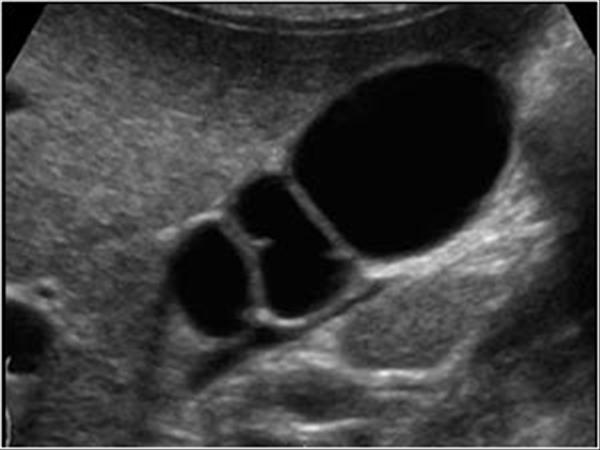
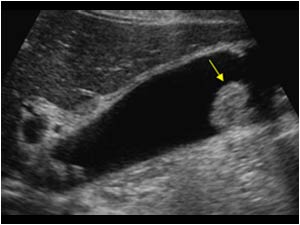
Cholelithiasis
Wall-echo-shadow sign (WES). GB is packed with gallstones
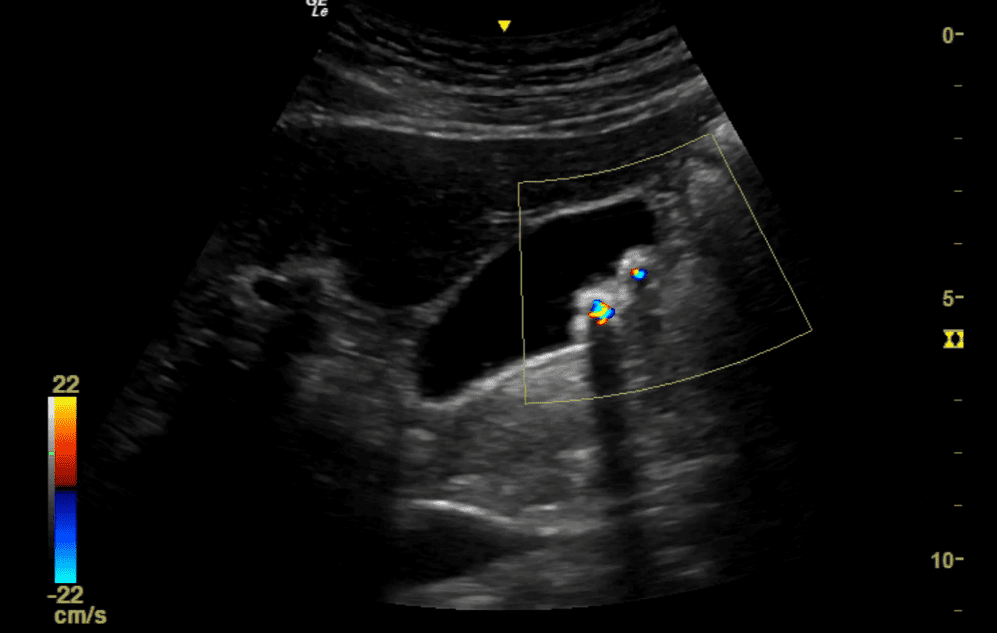
Polyps or cholelithiasis?
Cholelithiasis (shadowing and twinkle artifact)
What is gallbladder sludge and what is its most common underlying mechanism?
Gallbladder sludge is echogenic bile material within the gallbladder and is most commonly associated with biliary stasis.
What conditions are associated with gallbladder sludge and how do patients typically present?
Coexisting cholelithiasis, gallbladder carcinoma, jaundice, liver disease, sepsis, prolonged fasting. Sludge is usually asymptomatic.
What are the classic sonographic features of gallbladder sludge and what should be evaluated when it is present?
Low-level, non-shadowing, dependent echoes within the gallbladder lumen; the gallbladder should be carefully evaluated for small stones and signs of cholecystitis.
What is tumefactive sludge and how is it differentiated from a true gallbladder mass?
Tumefactive sludge is thick sludge that mimics an intraluminal mass; mobility/layering with patient repositioning and absence of vascularity on color Doppler favor sludge over a solid mass.
What are sludge balls and hepatization of the gallbladder?
Sludge balls are mobile collections of tumefactive sludge without acoustic shadowing; hepatization occurs when the gallbladder is completely filled with tumefactive sludge and appears isoechoic to liver parenchyma.

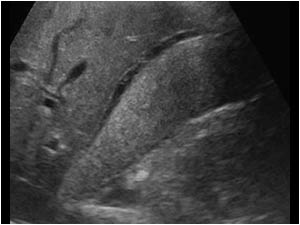
Gallbladder sludge

Sludge and stones
Gallbladder pathology that is mobile; no vascularity on color Doppler
Favors sludge ball
No shadowing= unlikely gallstone, no vascularity and mobility= unlikely polyp
Hepatized GB (gallbladder is completely filled with tumefactive sludge and appears isoechoic to liver parenchyma)
What is a gallbladder polyp and what type is most common?
A gallbladder polyp is a projection of tissue from the gallbladder wall into the lumen; cholesterol polyps are the most common type.
What are the typical size, composition, and behavior of cholesterol polyps?
They are usually <10 mm, composed of cholesterol and triglycerides within the gallbladder wall, and are benign and often incidental.
What are the classic sonographic features that differentiate gallbladder polyps from cholelithiasis?
Polyps appear as hyperechoic, non-shadowing, non-mobile projections attached to the gallbladder wall; they do not move with patient repositioning (ball-on-the-wall sign).
When should a gallbladder polyp raise concern for malignancy?
A large polyp or one that demonstrates rapid growth is suspicious for gallbladder carcinoma.
What is hyperplastic cholecystosis and which conditions does it include?
Hyperplastic cholecystosis is a group of proliferative and degenerative gallbladder disorders that includes cholesterolosis and adenomyomatosis.
What is cholesterolosis and how is it related to gallbladder polyps?
Cholesterolosis is a disturbance of cholesterol metabolism causing cholesterol accumulation in the gallbladder wall; it is often associated with cholesterol polyps and may produce a focal or diffuse polyploid appearance.
What is adenomyomatosis and what is its classic sonographic feature?
Adenomyomatosis is hyperplasia of the gallbladder epithelium with muscular thickening and formation of Rokitansky–Aschoff sinuses; cholesterol crystals within these sinuses commonly produce comet-tail artifact.
What is the clinical significance of adenomyomatosis?
It is typically asymptomatic, and is most often clinically insignificant.
This pathology is stable on a 6 month follow-up ultrasound. What is the most likely diagnosis and why?
Polyps. Their small size, echogenicity, multiplicity, and stability at follow-up sonography indicate hyperplastic (cholesterol) polyps.
Adenomyomatosis
What is acute cholecystitis and its most common cause?
Acute cholecystitis is sudden gallbladder inflammation most commonly caused by a gallstone lodged in the cystic duct or gallbladder neck.
What clinical and laboratory findings are associated with acute cholecystitis?
RUQ or epigastric pain, fever, leukocytosis, positive sonographic Murphy sign; labs may show elevated ALP and ALT, with elevated bilirubin if bile duct obstruction and posthepatic jaundice are present.
What are the classic sonographic findings of acute cholecystitis?
Gallstones, gallbladder wall thickening (often striated from edema), pericholecystic fluid, and sludge.
What sonographic findings suggest progression to gangrenous cholecystitis?
Focal wall necrosis, wall bulging, sloughed membranes, ulcerative craters, and an irregular gallbladder contour.
How does gallbladder perforation appear and why is it critical?
A focal wall defect or rupture with an irregular gallbladder shape; it carries high morbidity and mortality due to peritonitis and may lack a positive Murphy sign.
What is emphysematous cholecystitis and its key sonographic signs?
A severe form of acute cholecystitis caused by gas-forming infection, most common in diabetics; gas produces dirty shadowing, reverberation or ring-down artifact, and the champagne sign (gas bubbles along the nondependent/anterior wall).
How does chronic cholecystitis develop and how does it present?
Results from repeated cystic duct obstruction and recurrent acute cholecystitis; patients often have fatty food intolerance and a non-tender gallbladder, with thickened walls and possible WES sign.
What is acalculous cholecystitis and who is most at risk?
Acute cholecystitis without gallstones; more common in children, recently hospitalized patients, and immunocompromised individuals.

Acute cholecystitis with wall thickening, stones, and pericholecystic fluid
Gangrenous cholecystitis (sloughed membranes, wall irregularity)

Emphysematous cholecystitis with sludge

Acute acalculous cholecystitis
What are the normal gallbladder size limits and which measurement is most indicative of enlargement?
Normal size is ≤4–5 cm in transverse width and 8–10 cm in length; the transverse measurement is most indicative of gallbladder enlargement, and >4 cm should prompt evaluation for biliary obstruction.
What is a hydropic gallbladder (mucocele), what causes it, and how do patients present?
A hydropic gallbladder is gallbladder enlargement caused by obstruction of the cystic duct or biliary tree; patients may be asymptomatic or have epigastric pain, nausea, vomiting, and a palpable gallbladder.
What is Courvoisier gallbladder and what is its clinical significance?
A palpable, enlarged gallbladder caused by a pancreatic head mass; it is classically associated with painless jaundice and suggests malignant biliary obstruction.
What pediatric condition is associated with gallbladder hydrops and what is its underlying pathology?
Kawasaki disease, a vasculitis affecting lymph nodes, skin, and mucous membranes, commonly associated with gallbladder hydrops in older infants and children.
What is a porcelain gallbladder and how is it identified sonographically?
Porcelain gallbladder results from calcification of the gallbladder wall and appears as an echogenic curvilinear structure with posterior acoustic shadowing in the gallbladder fossa; it is typically clinically silent.
How is porcelain gallbladder differentiated from WES sign or emphysematous cholecystitis?
Identification of a calcified posterior gallbladder wall favors porcelain gallbladder; WES sign obscures the posterior wall, and emphysematous cholecystitis shows gas artifacts; CT or radiography is often used for confirmation.
What are the risk factors, clinical features, and sonographic appearances of gallbladder carcinoma?
Gallbladder carcinoma is rare but the most common biliary tract cancer; it is strongly associated with cholelithiasis and chronic cholecystitis. Patients may be asymptomatic or present with RUQ pain, jaundice, nausea, vomiting, weight loss, or hepatomegaly. Sonographically, it may appear as a non-mobile hypoechoic intraluminal mass, diffuse wall thickening, or an irregular polypoid mass filling the gallbladder fossa with liver invasion.
At what size should a gallbladder mass be suspected malignant and how is it differentiated from tumefactive sludge?
Malignancy is suspected when a polyp or mass measures >1 cm; color Doppler demonstrates vascularity within the non-mobile carcinoma, unlike tumefactive sludge which has no vascularity and is mobile.

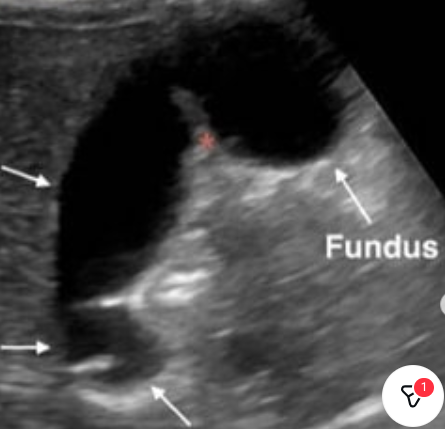
What pathology of the gallbladder is seen, and which underlying condition is this pathology often associated with in children?
Hydropic GB, Kawasaki disease

The palpable gallbladder seen here corresponds with _____ sign.
Courvoisier’s
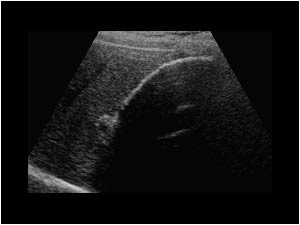
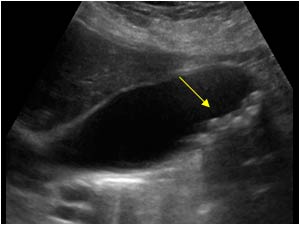
Porcelain GB (we see an echogenic posterior wall, which favors porcelain GB over WES sign)

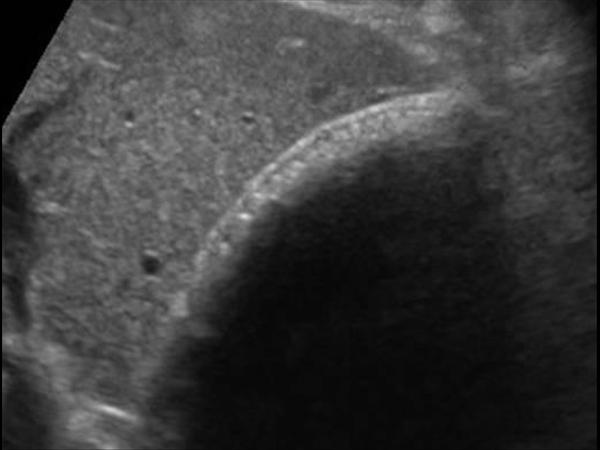
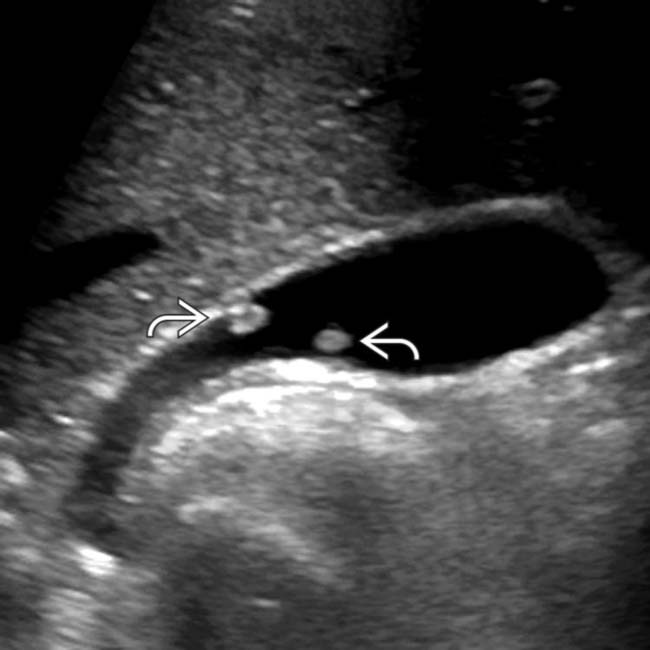
Demonstrates vascularity and is non-mobile
GB carcinoma