3) Monocular Subjective Refraction
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
What is the purpose of monocular subjective refraction?
→ determine pt’s refractive status using the pt’s input
subjective test
not fully subjective b/c the clinician’s subjectivity is taken into account too (DR judges the PT’s responses)
What is the goal of monocular subjective refraction?
→ improve pt’s vision to best corrected
this may not always be 20/20
if you can’t get your pt to 20/20, 2er cause of ↓VA MUST be explained!
List circumstances that make achieving 20/20 best-corrected vision more difficult.
Retinal disease
Media opacity
Amblyopia (refractive / strabismic)
Neurological issues
What is the key principle underlying successful refraction?
→ Establishing effective communication during the process
Pt needs clear understanding of what is expected of them
Examiner needs clear understanding of pt’s responses
What is the examiner’s role in determining the final rx during refraction?
→ Merge objective (retinoscopy) with subjective (pt’s visual complaints, daily visual demands, habitual rx, VA measurements) findings to create final rx
Objective + Subjective = Final RX
Give examples of patients who may not be good candidates for manifest refraction (“What’s better 1 or 2”?)
Non-verbal pt
Intellectual disabilities
Very young children
Malingering pt
may fabricate or exaggerate symptoms (e..g, want glasses)
seen in young children esp girls
STEP 1)
What does refractive analysis begin with? What are things you can do as a clinician during this stage?
Patient History!
Identifies pt’s perceived visual difficulty
VA ≠ patient satisfaction
20/25 may feel poor vision, BUT a 20/40 may feel comfortable
As a clinician:
Listen carefully to pt concerns
Educate patient on expected visual changes over time
young myopes - vision worsens, then stabilizes at ~25 yrs old
hyperopes - will need readers in a few years
What are typical behaviours shown by myopes?

Blurred distance vision (esp in dim illuminations)
Holding objects closer/moving closer to see
Needing to squint to see
What are typical behaviours shown by hyperopes?

Adults = trouble reading
Large hyperopes or older adults = blurred distance vision (bc lens can’t pull image front onto the macula)
Young adults = intermittent blur when fatigued or in poor lighting (bc lens can still pull image front onto the macula, but pt experience eyestrain)
headaches with near work (worsens as day progresses)
possible diplopia at near
Children/teens = no visual complaints, but may avoid near work
Note: These symptoms vary greatly by age & magnitude of error
What signs do both myopes of hyperopes exhibit when they require more power?
Myopes = push glasses back towards face
Hyperopes = push glasses down to nose
What are typical behaviours shown by astigmats?

Vision complaints at distance AND near
May be worse at one or the other
Head tilting with oblique axis
Squinting
Ghosting or doubling of images
ghosting = shadow appears behind obj
↓ astigmats usually have good vision
may experience tired eyes when doing detail oriented work
↑ astigmats = ↓ acuity (even if they dont have myopia or hyperopia)
STEP 2)
After patient history, what does a clinician assess?
VA – both distance & near using pt’s best corrected acuity
↓ vision at distance OR near = RE is likely the culprit (✅)
↓ vision at distance AND near = RE is possibly the culprit (⚠)
Rule of thumb for Estimation of RE: Myopia (simple vs compound)
Simple myope: each line of decreased acuity = -0.25D
Compound myope: each line of decreased acuity = -0.25D SE
SE = sph power + ½ cyl power
Rule of thumb for Estimation of RE: Hyperopia
Hard to estimate based on VA
Young patients - with active accommodation may have good distance VA with large RE (20/20 distance vision with +3.00D hyperope)
Presbyopes - ↓ distance & near vision
can estimate +0.25-0.50D increased power per line of decreased vision
so presbyope’s new rx can be estimated like myopes (but their change is not linear like myopes)
Rule of thumb for Estimation of RE: Astigmatism
→ Estimation includes amount & orientation of astigmatism
↓ impact on VA = ↓ astig amounts
↑ impact on VA: oblique > ATR > WTR (WTR has least impact on VA) (orientation)
STEP 3)
After VA, what does a clinician assess?
Lensometry!
pt’s current rx
whether or not pt is wearing their glasses correctly
Define Lens effectivity.
Change in vergence of light occurring at different points along the path
What does Effective lens power depend on?
location in front of the eye
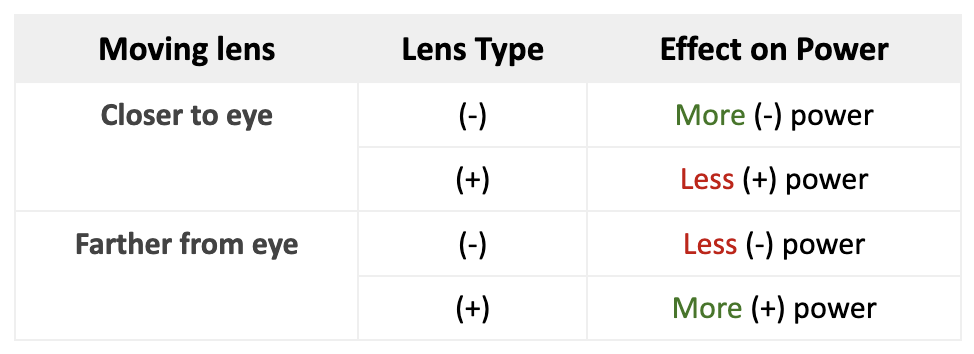
What happens to lens power when a lens is moved closer or farther from the eye?
💡 Connects to the “behaviour” myopes and hyperopes show when they need more power
STEP 4)
Once you have results of history, acuity & lensometry, what should you be able to do?
→ generate a “hypothesis” of what you expect pt’s RE to be
check if VA matches the pt’s symptoms
identify what type of RE explains the complaint
decide what Rx change should improve vision if VA is reduced
evaluate the reliability of patient responses
prevents the pt from controlling the exam
Scenario #1: What is the diagnosis under each VA?
Patient Complaint: I feel like I can’t see well when I drive home at night
Visual acuity #1: 20/30 distance, 20/20 near
Visual acuity #2: 20/30 distance, 20/30 near
Based on:
Patient’s complain = Myopia, hyperopia, astigmatism
Visual acuity #1 = Myopia (since pt can see 20/20 at near)
Visual acuity #2 = Hyperopia or astigmatism
Scenario #2: What is the diagnosis under each VA?
Patient Complaint: My eyes feel tired after working on the computer all day
Visual acuity #1: 20/20 distance, 20/30 near
Visual acuity #2: 20/30 distance, 20/25 near
Based on:
Patient’s complain = Hyperopia, astigmatism (myopes can’t sense computer strain, unless its uncorrected)
Visual acuity #1 = Hyperopia (b/c distance is 20/20)
Visual acuity #2 = Astigmatism
What is Just Noticeable Difference (JND) (aka “which is clearer 1 or 2?”)?
→ amount of optical change required for a difference in clarity or blur to be noticed
How to estimate JND?
Divide Snellen acuity denominator by 100 = JND
For a pt to show a difference of ___D JND a cross cylinder lens with + / - (JND/2) is needed
→ e.g., 20/200 = 2.00 JND (cross cylinder lens with +/- 1.00D is needed to show a patient a difference of 2.00D)
“To show a patient a 2.00-diopter difference, you need a cross-cylinder lens that flips between +1.00 and −1.00.”
What minimum VA is required to perform refraction with a phoropter?
20/50 - if the pt does NOT meet this, refraction should be performed using a trial frame instead
What is the typical JCC lens power built into a phoropter?
0.25 D or 0.50 D
List the 4 main steps of Refractive Determination.
Gross Sph Power Determination
Cyl Axis Refinement
Cyl Power Refinement
Cyl Power Search – only done if no cyl was found during retinoscopy
Sphere Power Refinement
Why do patients often report that more minus power looks clearer, and what problem can this cause?
→ More (-) power makes the image darker and smaller, which can seem clearer
this stimulates accommodation
can lead to near vision difficulty or headaches
What is the goal of refraction when determining final lens power?
→ achieve best visual acuity with the most (+) / least (-) power
BVA may not be 20/20
What is the JCC and how is it used in cylinder axis refinement?
→ has 2 equal-power cyl with opposite signs to refine cyl axis & power
cyl are oriented 90° apart
Red dots = MINUS cylinder
White dots = PLUS cylinder
SE of the JCC = 0
During “Cyl axis refinement” why do we use 5° and 1°, not 15° and 5° for people who had a retinoscopy cyl of -2.00>?
High astigmatism powers can sense/are sensitive to small axis changes
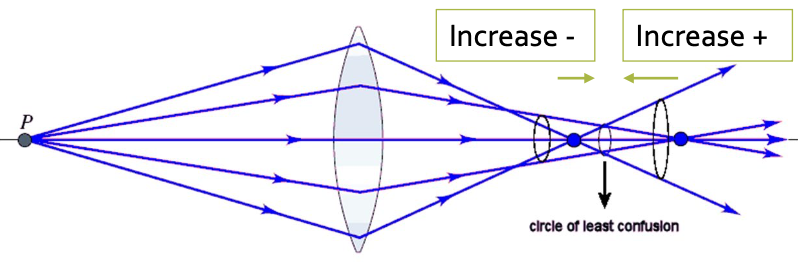
What is the goal of the “Cylinder Power Refinement” step?
→ Maintaining SE (sph equivalent) to move CLC closer to the retina on either side
If just change cyl power, you move the CLC off the retina & the focal point of the astig power onto the retina
During the “Cylinder Power Search” what does it mean if the patient said yes to any of axis with the Red dot?
It means you missed finding cylinder on retinoscopy
During the “Cylinder Power Search” what does it mean if the patient said yes to ALL the axis with the White dot?
No cylinder found → pt is a true sph
What do you do if you had a large increase in cyl power during “Cylinder power refinement” (~0.75D or more)?
→ Go back and recheck cyl AXIS at higher power
pt should be more discriminating due to more appropriate correction – need to make sure it is the correct axis
If you start with a high cyl power & it decreases – don’t need to recheck axis (b/c we want a low cyl)