Type II Diabetes
1/8
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
9 Terms
What is Type II Diabetes Mellitus?
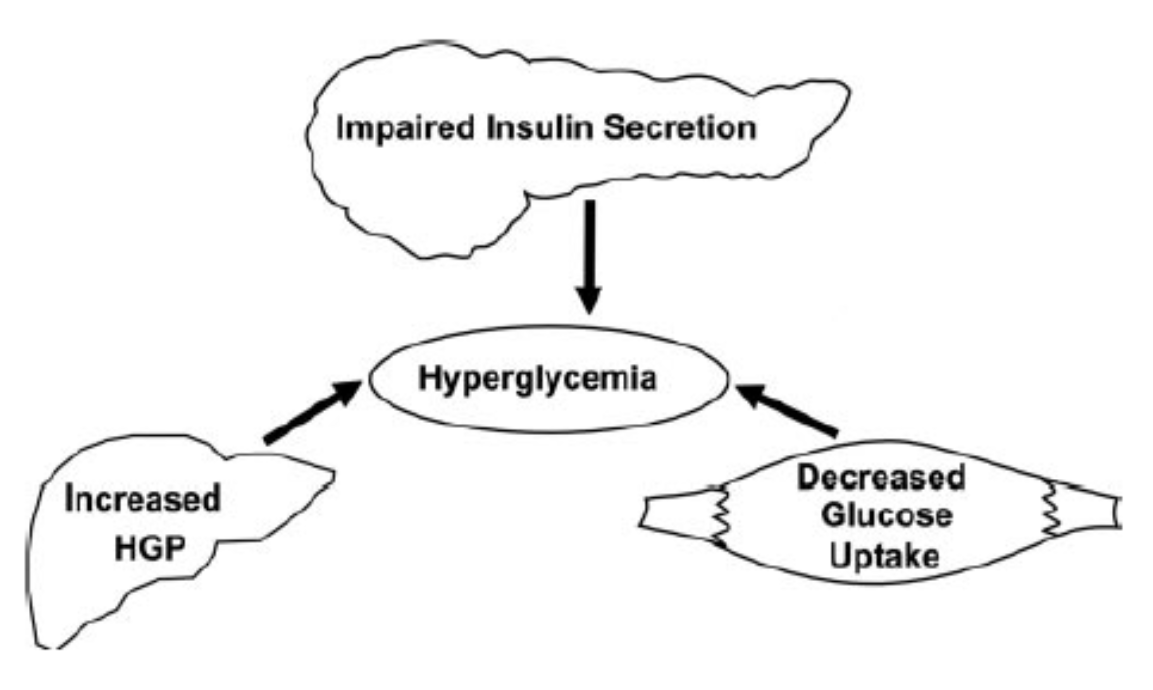
Type II Diabetes Mellitus is a disease of chronic hyperglycemia caused by insulin resistance and dysfunction of beta-cells
1) Insulin Resistance
→ patient will require more insulin than necessary in order to have a response
→ leads to increased gluconeogenesis at the liver as well as decreased glucose uptake at the muscle
2) Beta-Cell Dysfunction
→ there is inadequate insulin secretion even though the patient has hyperglycemia and insulin resistance
What are the physiological changes in a type II diabetes patient over time?
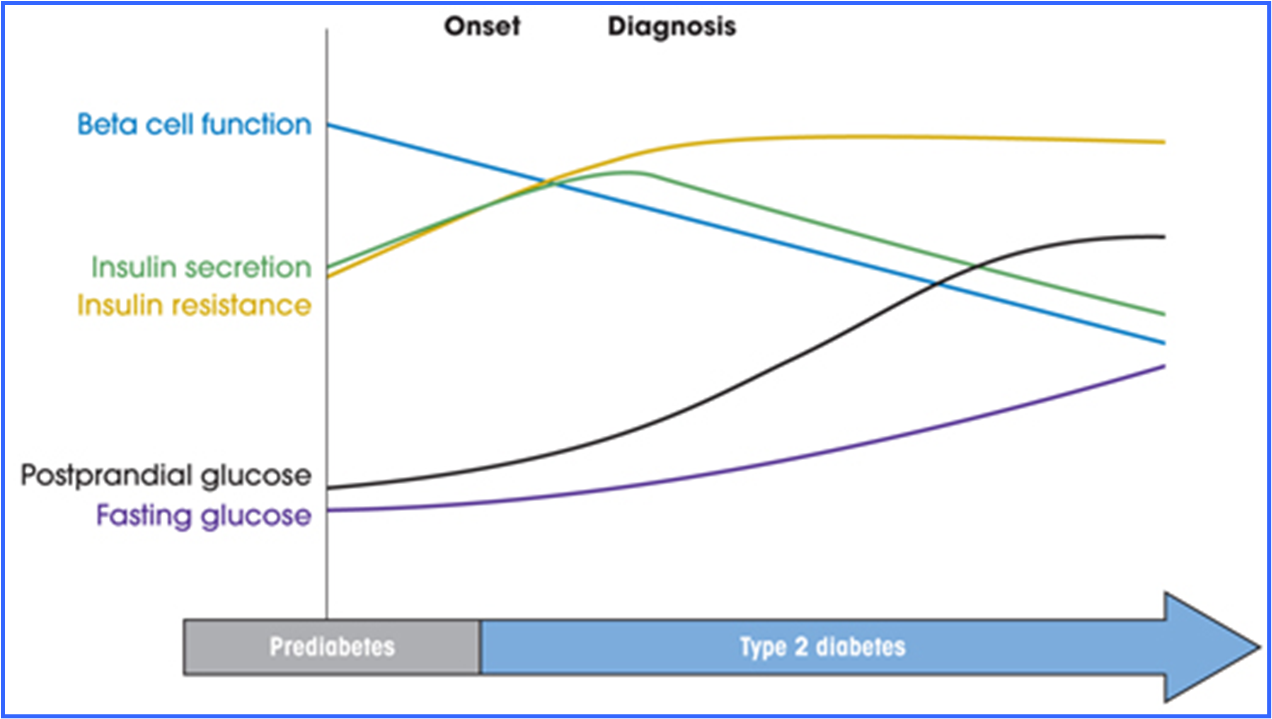
1) Patients will start out as prediabetic
→ will have insulin secretion that matches rising insulin resistance
→ beta cell function will slowly drop
Once beta cell function drops past insulin resistance, patient becomes type II diabetic
→ will have hyperglycemia as well as decreased insulin secretion
What lab values qualifies a patient as having diabetes?
HbA1c is used most commonly and is a measure of blood sugar over the past 3 months
To qualify as diabetic
→ 2 hour postprandial - above 200
→ fasting glucose above 126
→ hemoglobin A1C of 6.5%
To qualify as prediabetic
→ hemoglobin A1C of 5.7% to 6.4%
→ fasting glucose above 100
→ two hour postprandial between 140-199
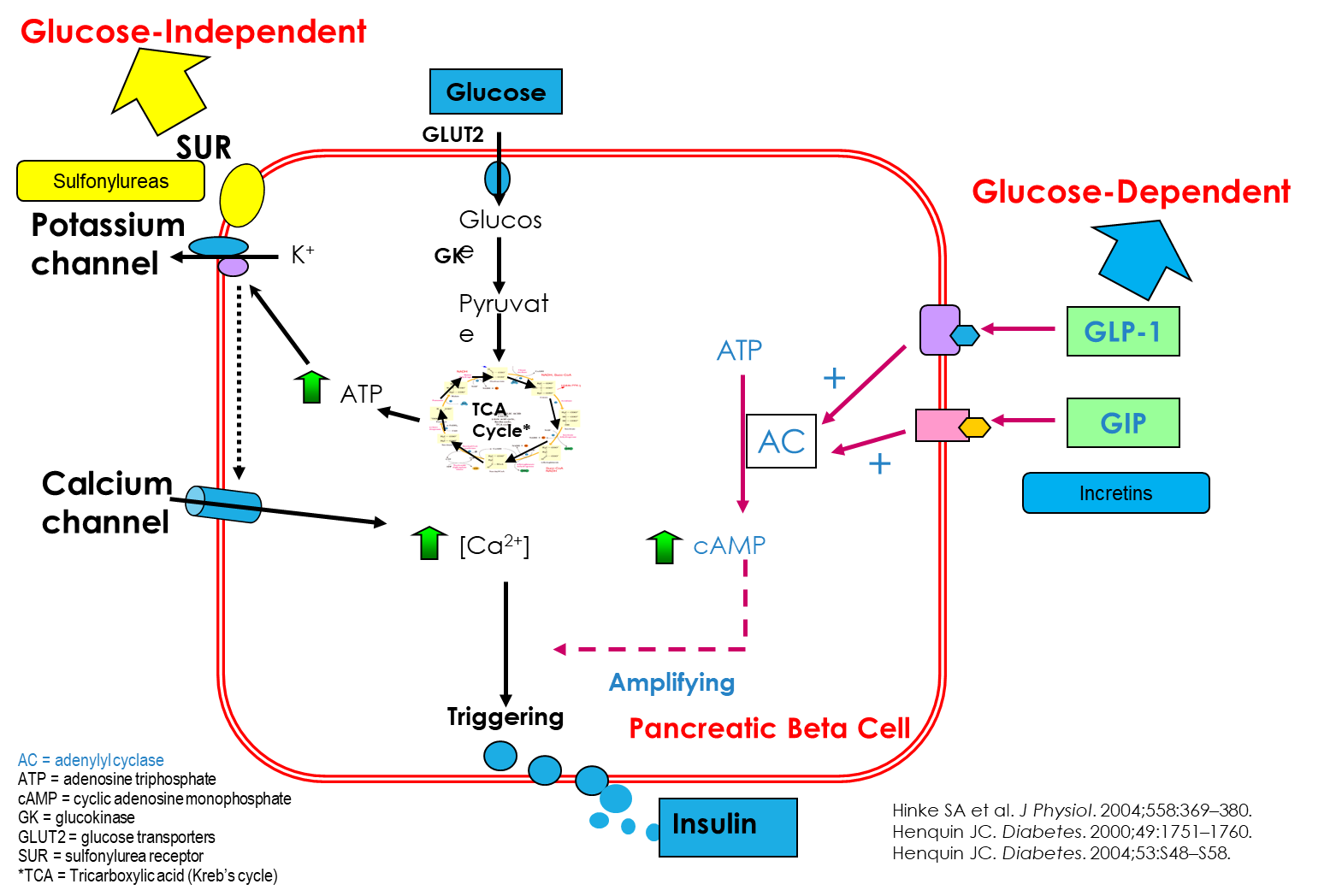
What are Sulfonylureas?
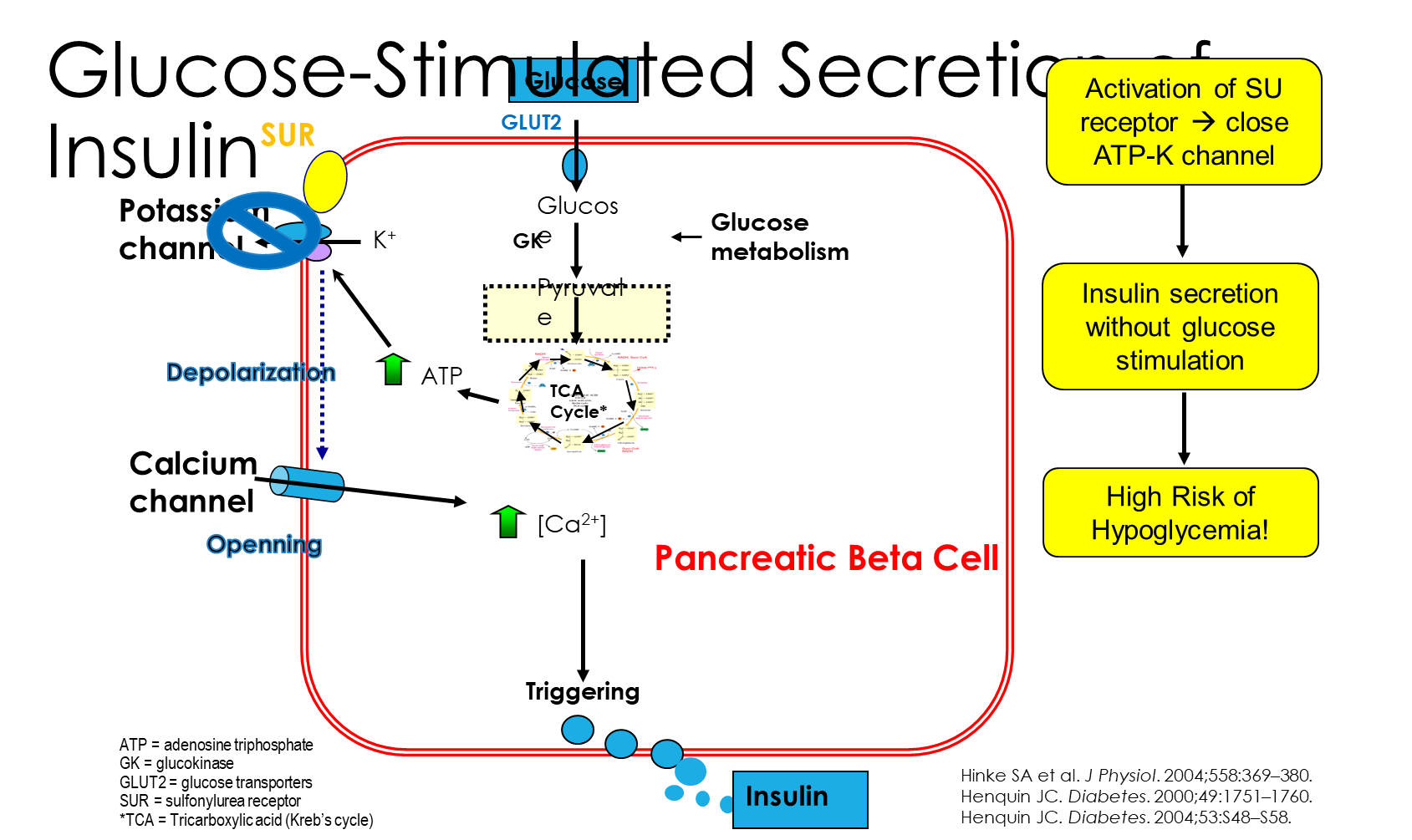
Sulfonylureas or Insulin Secretagogues
1) These drugs will increase the secretion of insulin irrespective of blood glucose and are used to decrease HbA1c
→ Sulfonylureas will blocking the potassium channel by binding to the sulfonylurea receptor on pancreatic beta cells, leading to an increased release of insulin
2) has a high risk of hypoglycemia and patients on these drugs can gain weight
What are Carbohydrate Absorption Inhibitors?
Alpha Glucosidase Inhibitors include Acarbose and Miglitol
1) Alpha-Glucosidase Inhibitors are inhibitors of carbohydrate absorption by blocking absorption of carbohydrates in the intestines
→ because these drugs keep complex carbs in the intestines, it can lead to overgrowth of bacteria in the gut leading to bloating and gas
What are Insulin Sensitizers?
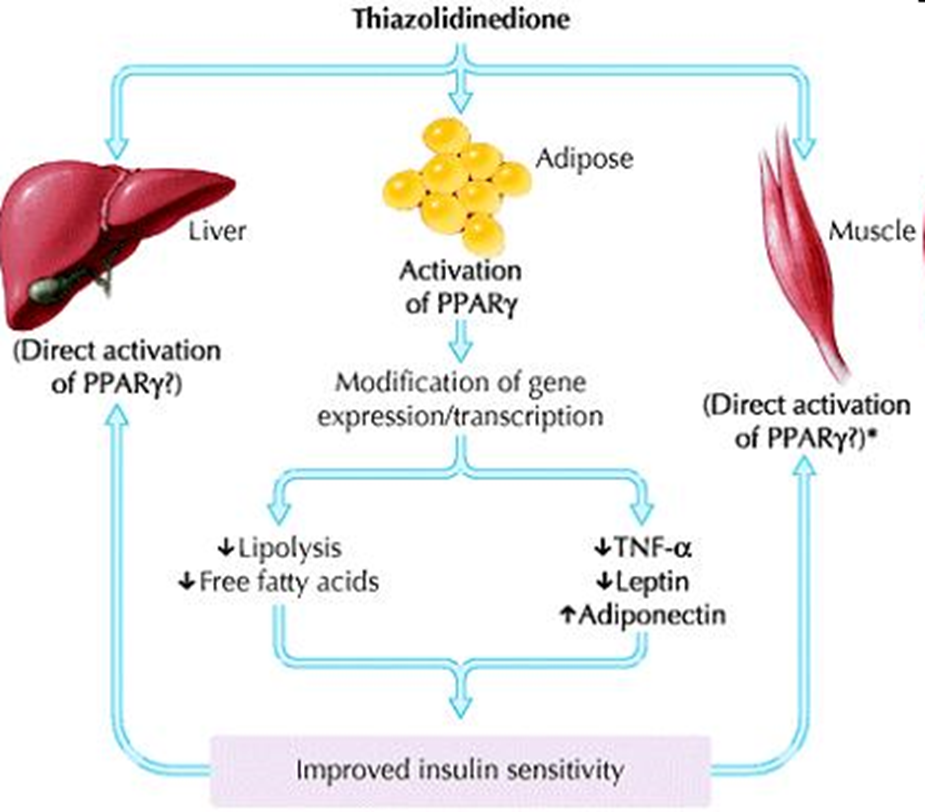
Insulin Sensitizers are subdivided into biguanides and thiazolidinediones
1) Biguanides include drugs like Metformin
→ decrease hepatic glucose production and decrease intestinal glucose absorptions
→ increases peripheral glucose uptake and utilization
→ these drugs can sometimes cause GI symptoms
2) Thiazolidinediones like Troglitazone and Pioglitazone
→ function at the PPAR-gamma ligands and lead to an increase in peripheral glucose uptake and decrease in hepatic glucose production
→ can cause weight gain and osteoporosis
What are GLP1 Receptor Agonists and DDP-IV Inhibitors
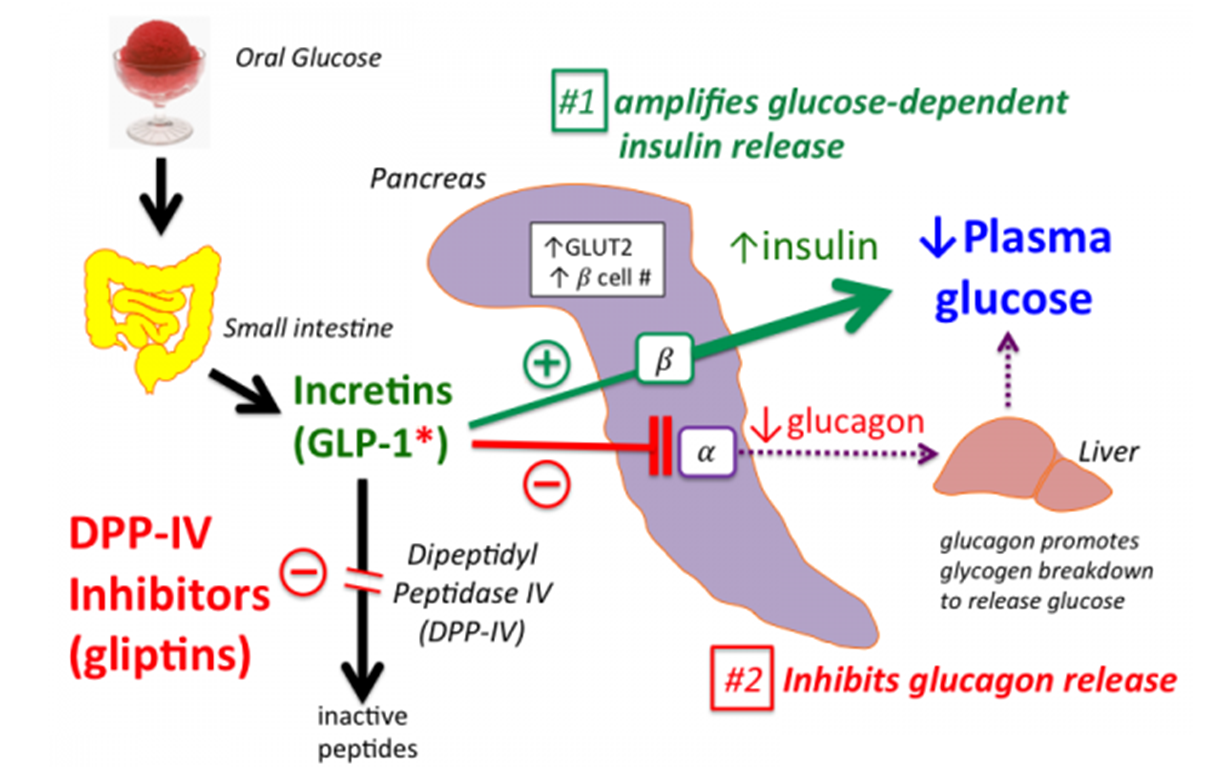
GLP1 Receptor Agonists or Incretins will alter our food intake
→ includes Liraglutide, Dulaglutide, and Semaglutide
1) Increases the level of GLP1 expression following a meal
→ GLP1 agonists will also stimulate insulin response in a glucose dependent manner
→ GLP1 agonists will also inhibit glucagon secretion from alpha cells in a glucose dependent manner
→ also decreases gastric emptying allowing for us to stay full for longer
2) There are also DPP-IV inhibitors that block the breakdown of GLP-1
3) GLP-1 agonists are protective against chronic kidney disease and cardiovascular disease
What are Inhibitors of Renal Glucose Reabsorption?
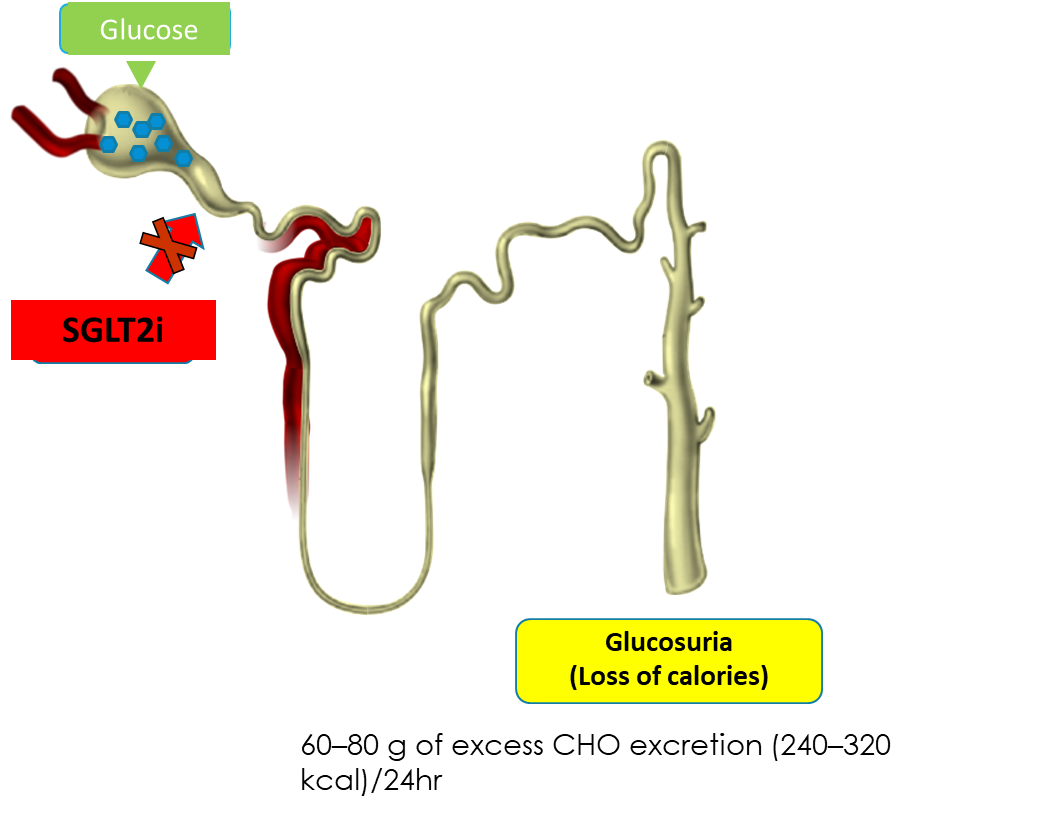
SGLT2 Inhibitors block the SGLT2 on the proximal renal tubules, preventing glucose reabsorption at the kidneys
→ Canagliflozin
→ Dapagliflozin
→ Empagliflozin
→ Ertugliflozin
1) These drugs will lower our A1C and decrease glomerular hyperfiltration
→ this makes these drugs protective against heart failure, cardiovascular disease, and chronic kidney disease
When is insulin used to treat type II diabetes
when oral medications by themselves are insufficient