fluid and electrolyte imbalances - lecture 15 FIRST LECTURE FOR EXAM 3
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
the achieve homeostasis, the body must maintain ...
strict control of water and electrolyte distribution
- concentration of sodium is higher in extracellular fluid and super low in intracellular fluid
-concentration of potassium is lower in extracellular fluid and super high in intracellular fluid
levels of electrolytes can become too low or too high when the ...
amount of water in your body changes
water
provides the aqueous medium for biochemical reactions, serves as a vehicle for the transport of solutes
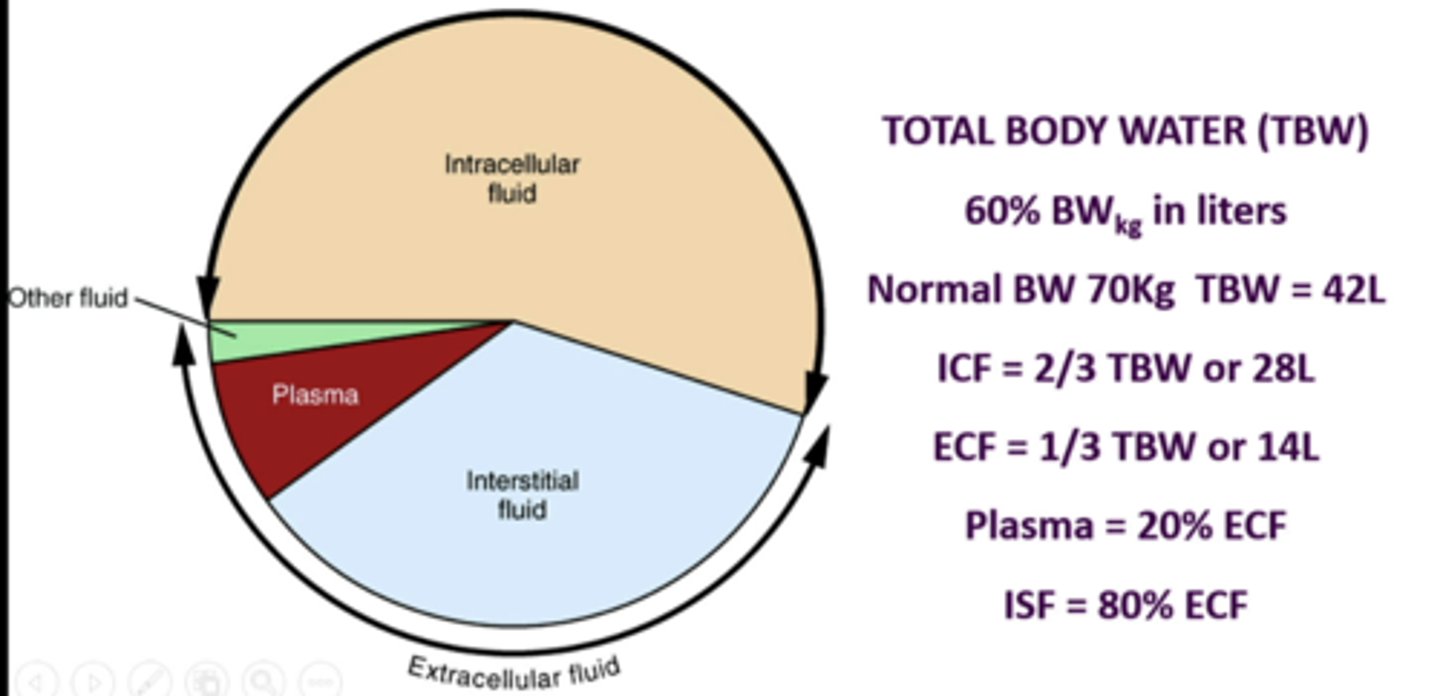
intracellular fluid
volume of fluid within cells
extracellular fluid
all non-intracellular fluid (interstitial space, intravascular compartment, lymph, transcellular)
total body water
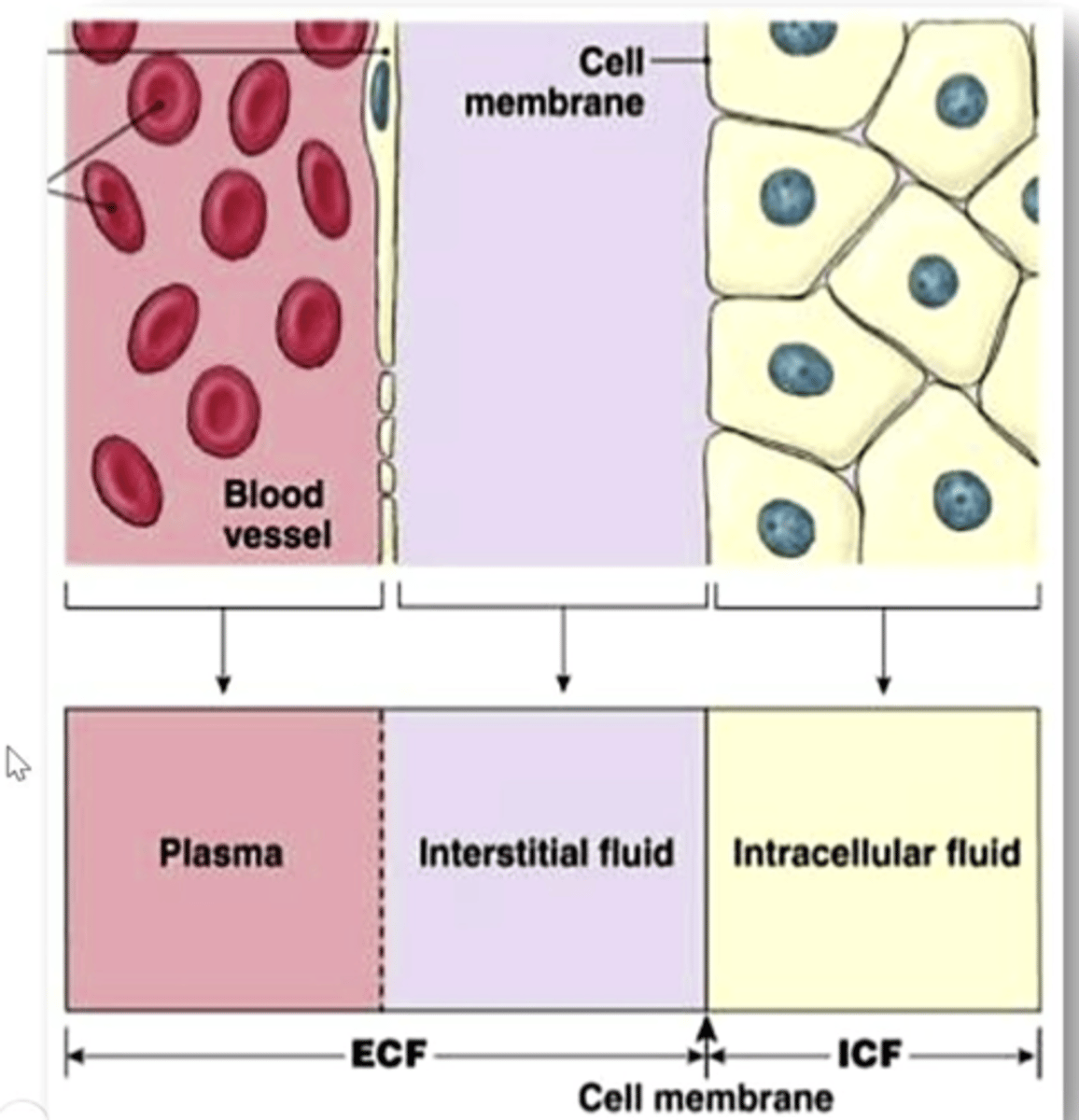
describe this image
on the left is a capillary and on the right are epithelial cells. the purple represents the interstitial fluid. the intracellular fluid is in yellow and the plasma is in the pink. what separates the plasma from the interstitial fluid are the endothelial cells. what separates the interstitial fluid from the intracellular fluid is the plasma cell membrane
an athlete ran a marathon even though she felt ill. after the race, she collapsed. she was pale with low blood pressure and sunken eyes. one knee and ankle were badly swollen; her abdomen was distended with fluid. the doctor diagnosed appendicitis and dehydration
questions:
what has happened to her:
1. blood osmolarity?
2. cell size?
3. volume of vascular compartment?
1. blood osmolarity - INCREASES bc water amount has decreased
2. cell size - SHRUNK bc extracellular fluid increases so water moves from intra to extra to maintain equilibrium
3. volume of vascular compartment - DECREASED bc she has been sweating and has low blood pressure
amount of sodium in body is a prime determinant of ...
ECF volume
sodium
usually enters the body via the GI tract. intake typically exceeds amount needed (recommended <2300 mg/day)
most excess sodium is excreted via the ...
kidneys
dietary salt overload
adds NaCl and increases total [solute] of ECF
dietary water overload
decreases total [solute] of ECF
____ ________ indicates water balance - NOT Na+ balance
Na+ plasma
___ ____ controls ECF/ICF water distribution
Na+ ECF
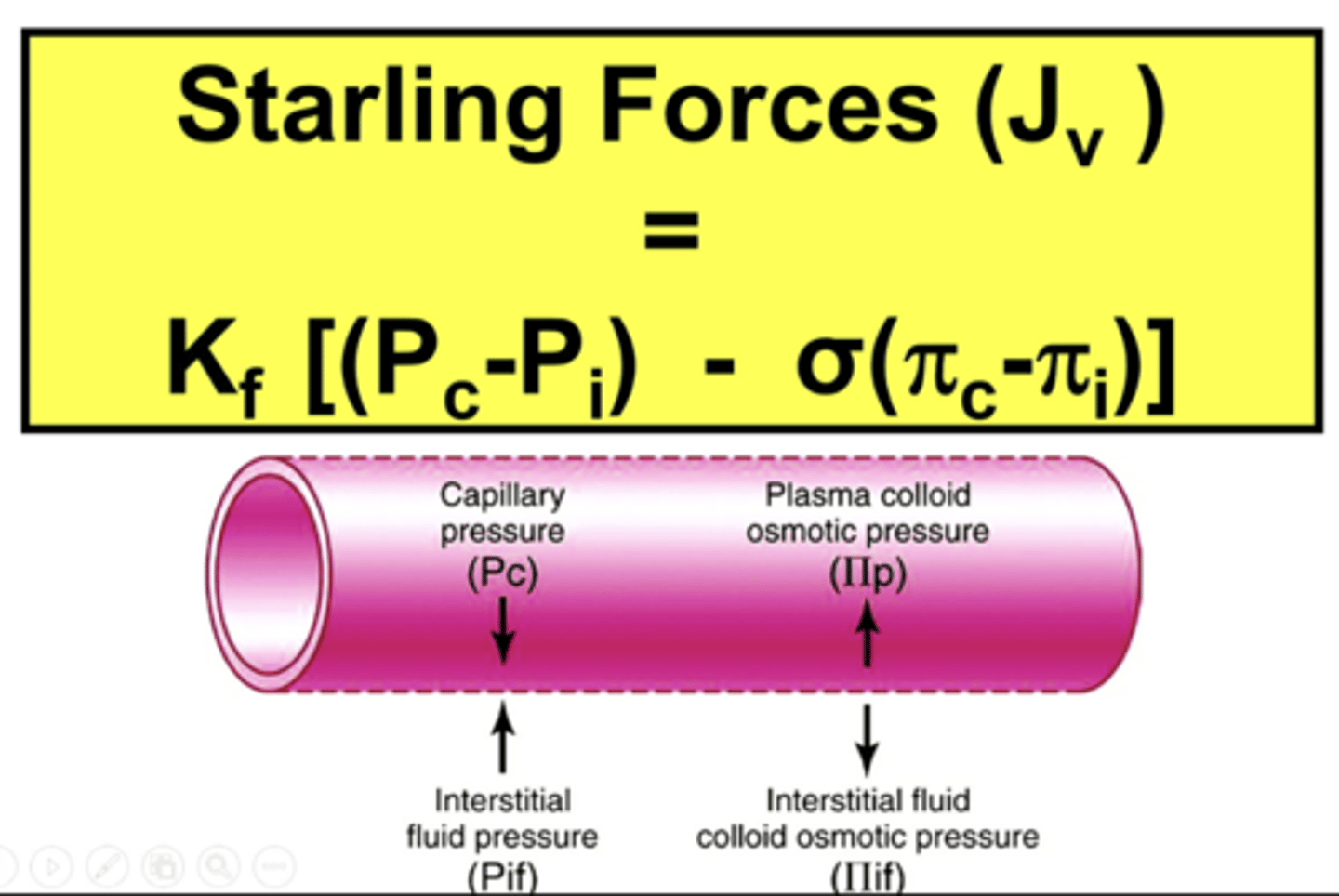
describe this image - starlings forces
capillary hydrostatic pressure is abbreviated Pc and the interstitial fluid hydrostatic pressure is abbreviated Pif
plasma colloid osmotic pressure is abbreviated πp and the interstitial fluid colloid osmotic pressure is abbreviated πif
notice the direction of arrows for these 4 pressures:
1. the capillary hydrostatic pressure (Pc) pushes fluid out of the capillaries and into the interstitial fluid space
2. the interstitial fluid osmotic pressure (πif) pulls fluid out of the capillary and into the interstitial fluid space
- so these favor fluid filtration out of the capillaries and into the interstitial space
in contrast
1. the interstitial fluid hydrostatic pressure (Pi) opposes fluid leaving the capillary
2. the plasma colloid osmotic pressure (πp) opposes fluid leaving capillary
- so these favor fluid absorption from interstitial fluid space into the capillary
what forces work to keep plasma in the capillary?
a. capillary colloid osmotic pressure (COP) and tissue COP
b. capillary hydrostatic pressure and tissue COP
c. capillary hydrostatic pressure and tissue hydrostatic pressure
d. capillary COP and tissue hydrostatic pressure
colloid osmotic pressure = oncotic pressure due to large protiens
d. capillary COP and tissue hydrostatic pressure
rationale: hydrostatic pressure can be thought of as PUSHING PRESSURE and colloid osmotic pressure can be thought of as PULLING PRESSURE. COP in the capillary that pulled/kept fluid in and hydrostatic pressure pushing fluid out of the tissue results in forces favoring fluid in the capillary
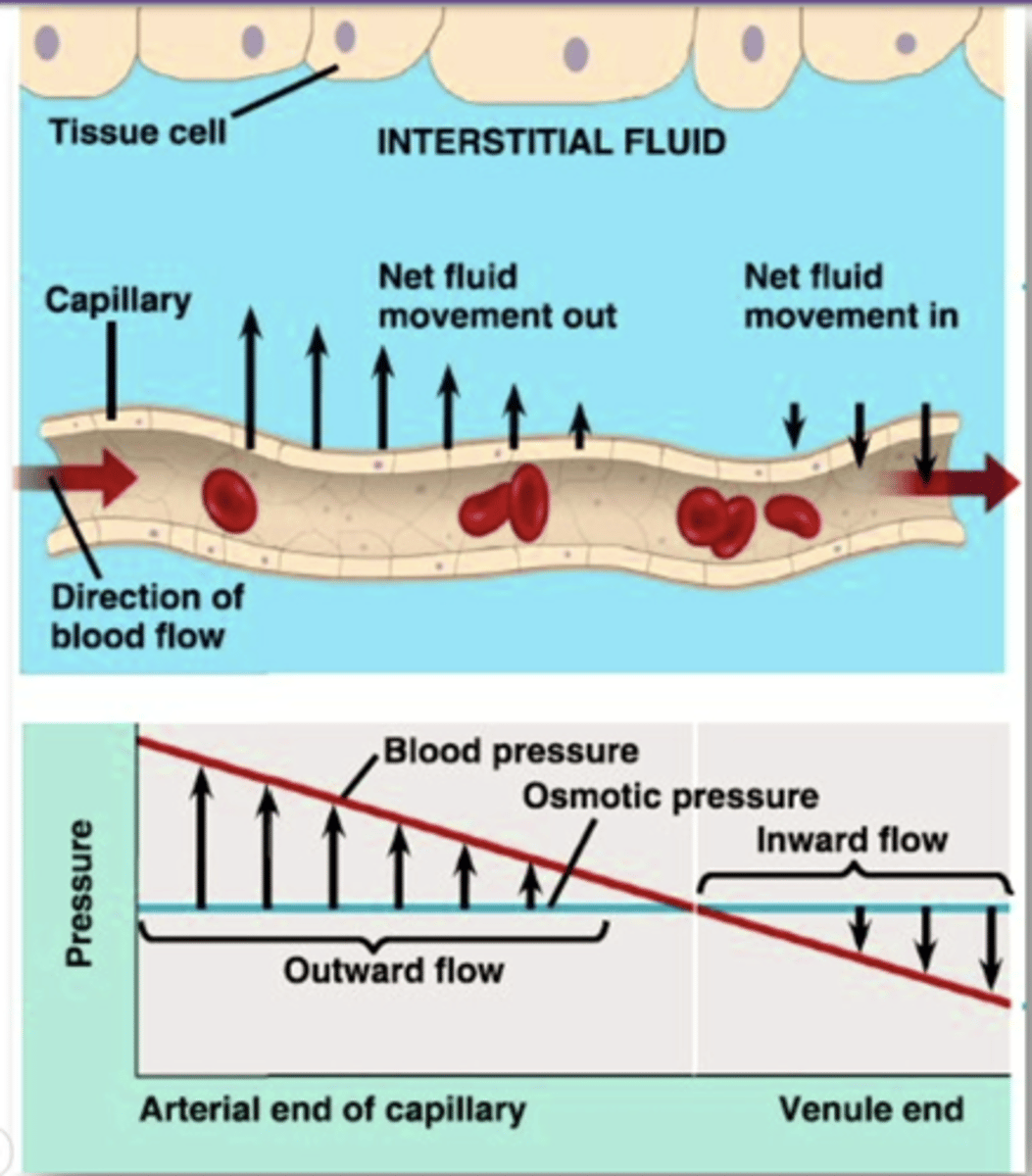
describe this image
at the arterial end of capillary, blood pressure is greater than colloid osmotic pressure and fluid flows out of the capillary into the interstitial fluid
at the end of the capillary, blood pressure is less than colloid osmotic pressure and fluid flows from the interstitial fluid into the capillary
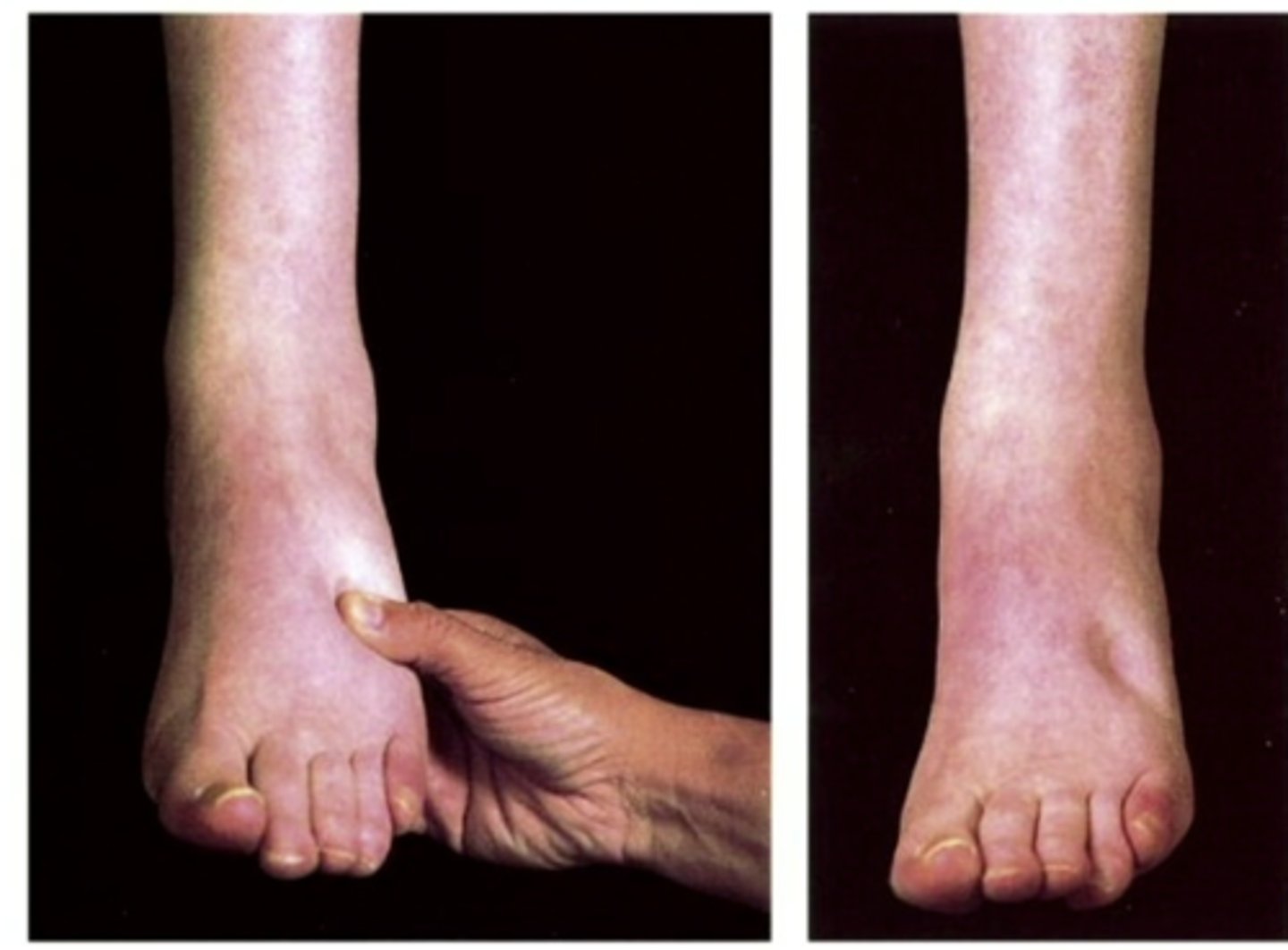
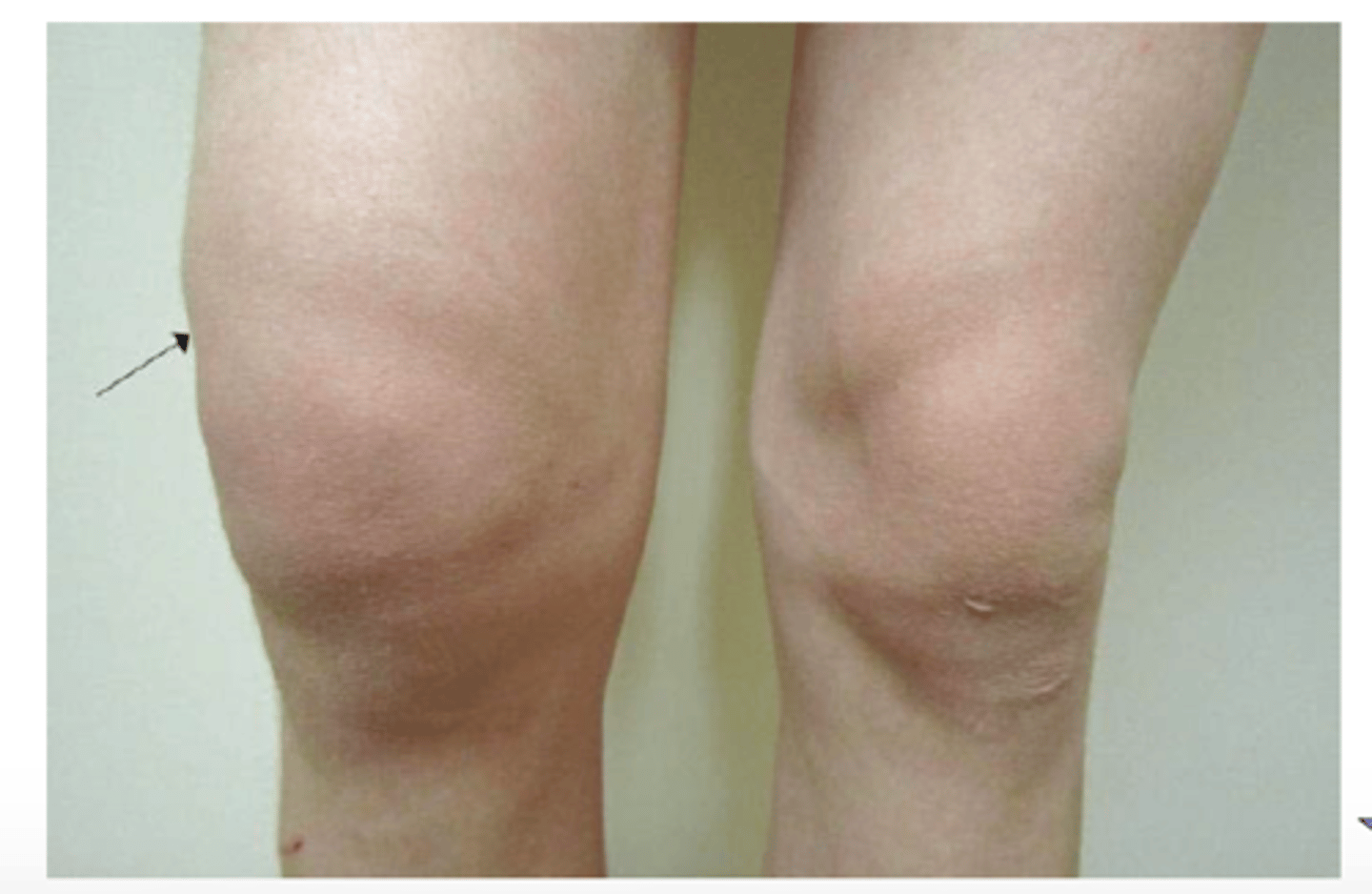
edema
palpable swelling produced by an increase in interstitial fluid volume
does not become evident until the interstitial volume has been increased by 2.5-3.0 L
can be localized, systemic, or dependent
generally accounts for 10-30% of body weight, wounds heal more slowly, risks of pressure sores and infections increase, may interfere with movement, can be life threatening
localized edema to site of trauma - injury
includes cerebral edema, pleural effusion, pericardial effusion, ascites
systemic edema - everywhere
associated with diseases such as renal failure

dependent edema
where fluid pools in gravity-dependent areas-may be a sign of systemic. also known as pitting edema

localized, systemic, dependent edema
associated with weight gain, puffiness, swelling, tight-fitting shoes, and clothing

what causes edema?
1. increased capillary permeability
2. decreased plasma oncotic pressure
3. increased plasma hydrostatic pressure
4. obstruction to lymph flow (lymphedema)
increased capillary permeability - edema
when capillary pores become enlarged or the integrity of the capillary wall is damaged capillary permeability is increased
plasma proteins and other osmotically active particles leak into the interstitial spaces, increasing the tissue colloidal osmotic pressure and contributing to the accumulation of interstitial fluid
potential causes:
1. burn injury
2. capillary congestion
3. allergic inflammation reactions
4. immune response
5. malignancy

decreased capillary oncotic pressure - edema
may be caused by decreased plasma protein synthesis (liver disease), glomerular diseases, drainage from large, open wounds
tends to produce generalized edema rather than dependent edema. swelling in face, legs, and feet
potential causes:
1. increased loss of plasma proteins
2. protein losing kidney diseases
3. extensive burns
4. decreased production of plasma proteins
5. liver disease
6. starvation, malnutrition
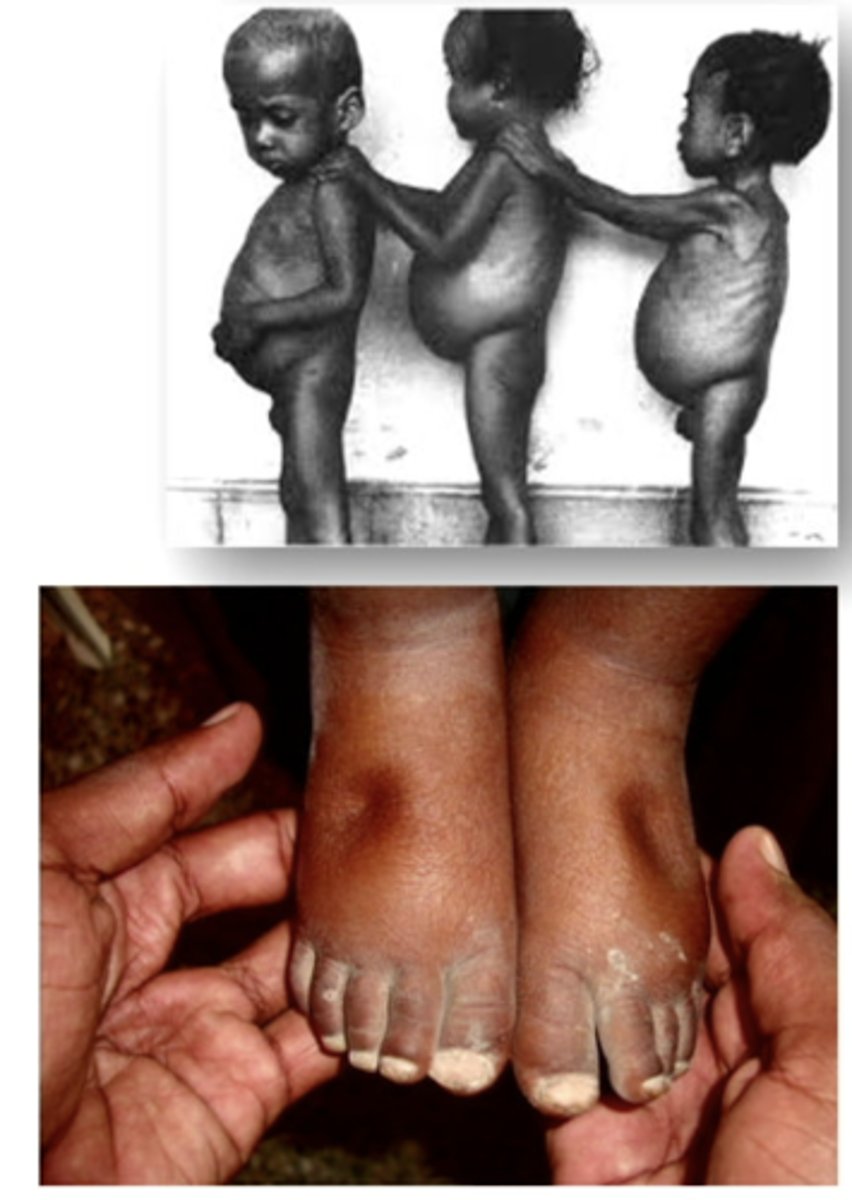
increased capillary hydrostatic pressure - edema
localized edema - allergic or inflammatory conditions resulting from the release of histamine or other inflammatory mediators
generalized edema - result of increased vascular volume, caused by venous obstruction, excessive salt intake or water retention due to congestive heart failure/renal failure
potential causes:
increased vascular volume
1. heart failure
2. kidney disease
3. premenstrual sodium retention
4. pregnancy
venous obstruction:
5. liver disease with portal vein obstruction
6. acute pulmonary edema
7. venous thrombosis

obstruction of lymphatic flow - edema
edema due to impaired lymph flow is commonly referred to as lymphedema
may be caused by infection, surgical excision, or tumors

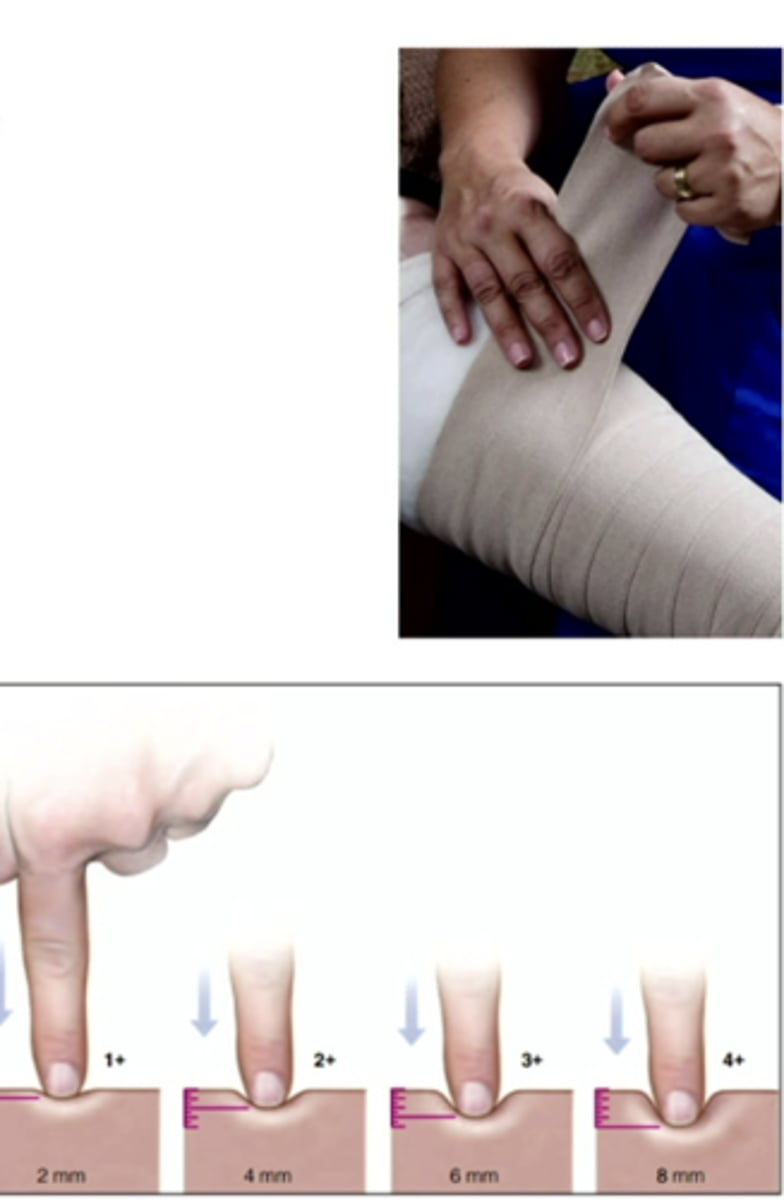
how should we assess and treat edema
1. daily weight, visual assessment, measurement of affected region, assess for pitting
2. diuretic therapy
3. administer albumin (like giving a plasma protein)
4. elastic support stockings and sleeves
5. elevation of affected area
6. moderate to severe lymphedema can be treated with light pressure massage
T or F? increased levels of antidiuretic hormone decrease urine output
TRUE
rationale: ADH prevents diuresis by causing more water to be reabsorbed in the kidney tubules. if more water is reabsorbed, there is less water left to eliminate as waste, decreasing urine output
controlling blood osmolarity
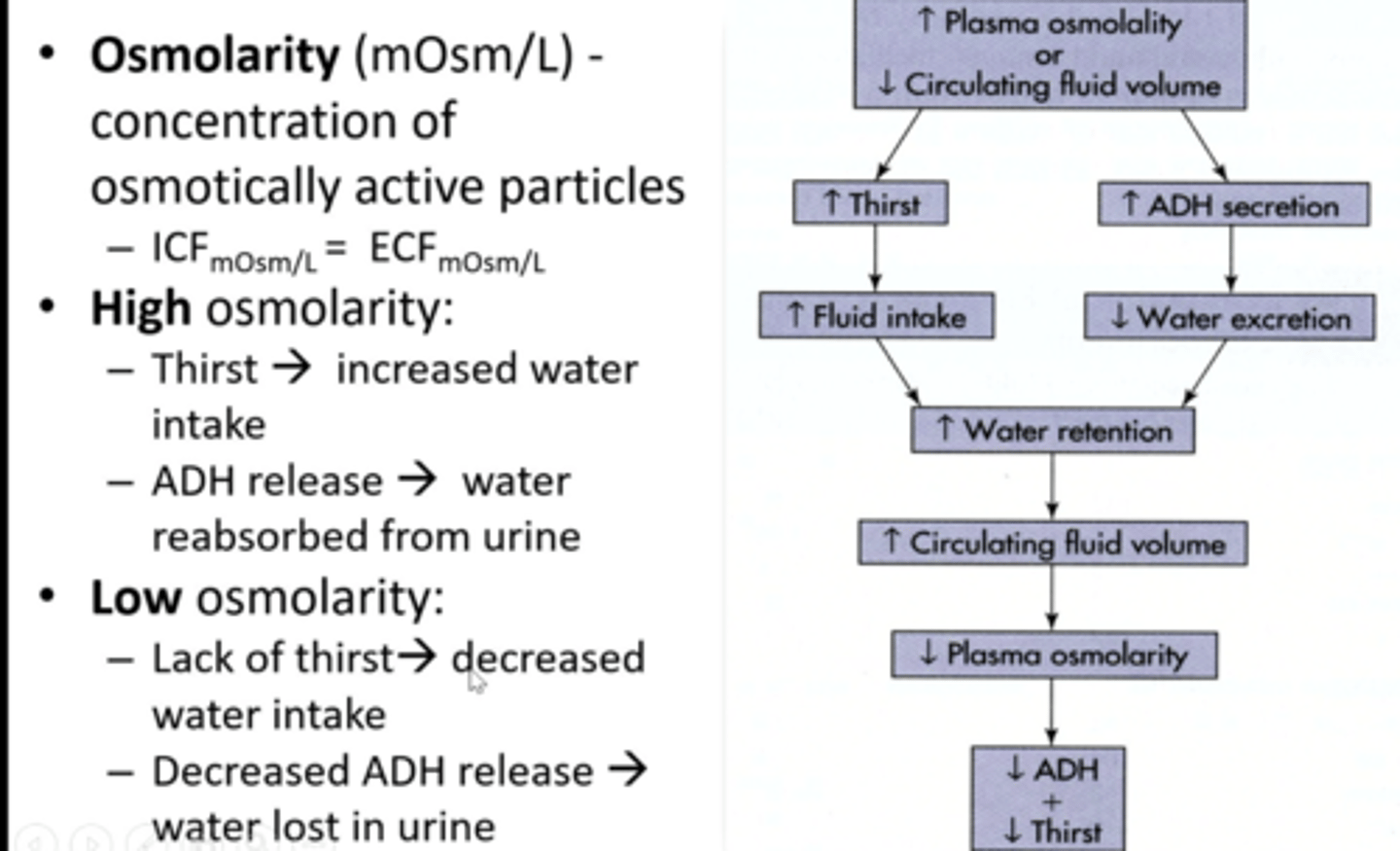
polydipsia - excess thirst
excessive
symptomatic thirst due to water loss
inappropriate/false thirst - adequate hydration, congestive heart failure, chronic kidney disease
compulsive thirst - psychiatric disorders like schizophrenia
hypodipsia - decrease thirst
decreased ability to sense thirst
associated with lesions of the hypothalamus
thirst is decreased in elderly, despite higher serum sodium, and osmolarity levels
-common in elderly


thirst is regulated by the _______________ in the hypothalamus
osmoreceptors
diabetes insipidus (DI)
kidneys pass an abnormally large volume of urine that is insipid (dilute and odorless)
due to deficiency of or decreased response to ADH, unable to concentrate urine during periods of water restriction = polyuria
1. neurogenic - brain
2. nephrogenic - kidneys
3. dipsogenic - thirst
4. gestational - pregnancy
neurogenic diabetes insipidus
lack of ADH production in hypothalamus
symptoms: polyuria, nocturia, polydipsia
causes: idiopathic (50%), hypoxic encephalopathy, head trauma, neoplasia, infections
treatments: ADH analogs (desmopressin, no pressure activity - intranasally, oral tablet, parenteral), low solute diet, diuretic
nephrogenic diabetes insipidus
kidneys do not respond to ADH, impairment of urine concentrating ability
symptoms: polyuria, nocturia, polydipsia
causes: genetic loss of ADH receptor, hypercalcemia, hypokalemia, lithium toxicity
treatments: low-salt, low-normal protein diet, diuretics, nonsteroidal anti-inflammatory drugs (NSAIDS)

dipsogenic diabetes insipidus
defect of or damage to thirst mechanism (hypothalamus)
- ingest excess fluid - suppresses ADH = polyuria
treatments: ADH V2 R analogs, drugs to stimulate ADH secretion

gestational diabetes insipidus
excess placental production of vasopressinase = increased breakdown of ADH
causes: diseases of pregnancy including pre-eclampsia
treatments: ADH V2 R analogs, drugs to stimulate ADH secretion

syndrome of inappropriate ADH (SIADH)
body retains water instead of excreting in urine due to elevated ADH
failure of negative feedback; leads to dilutional hyponatremia
common > 200,000 US cases/year
causes:
S - surgery
I - intracranial: infection, head injury
A - alveolar
D - drugs: opiates, anti epileptics and psychotics
H - hormonal - hypothyroid, low cortisone level
treatments: fluid restriction, diuretics, drugs to inhibit V2 receptor actions of ADH (vaptans)
normal sodium
135 to 145 mEq/L
hypernatremia
sodium > 145 mEq/L
hyponatremia
sodium <135 mEq/L
plasma sodium
regulates extracellular fluid volume and osmolarity
why would retaining sodium cause high blood pressure
the water will follow sodium which will increase extracellular fluid volume, increase interstitial fluid volume, increase plasma volume, increase blood volume, increase blood pressure

its a very hot day and you fall down the stairs on the way to see the doctor about your hepatitis and renal disease
question:
explain why you have edema in your sprained ankle and foot
localized edema from the fall (inflammation, leaky capillaries)
could also have problems from hepatitis (decreased albumin = decrease plasma oncotic pressure) and renal disease (proteinuria - loss of protein in urine = decrease oncotic pressure)
all cause an increase in filtration of fluid from capillaries