UTI & STI
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
Classification of UTI:s
Lower or upper UTI
Asymptomatic or Symptomatic
Sporadic or Recurrent (at least 3 a year):
Nosocomial (hospital acquierd) or Non-nosocomial
Cystitis/urethritis or pyelonephritis (often complicated)
In recurrent UTI a primary antibiotic treatment disturbs the enteric microflora which promotes UTI pathogens and increased resistance.
UTI categorization
Asymptomatic bacteriuria (ABU)
Acute cystitis
Acute pyelonephritis (febrile UTI)
Complicated (structural/functional abnormalities)
UTI symptoms
Cystitis (burning UTI): Pelvic pressure, frequent painful urination, and blood in urine.
Urethritis (can be STI): burning with urination and discharge
Acute pyelonephritis: upper back and flank pain, high fever, nausea, and vomiting
Asymtomatic bacteriuria (ABU): ABU is most common in the elderly; symptoms include cloudy urine, bad-smelling urine, nausea, and sudden fatigue (but no burning sensation). ABU isn’t treated with antibiotics. ABU is especially common in those with catheters.
UTI causing backteria
Group 1: E. coli, S. saprophyticus
Group 2: Enterococci, S. aureus, coliforms, Pseudomonas. aeruginosa
Group 3: Coagulase negative staph, Group B street, environmental gram neg rods
UTI sample taking
Try to avoid start - and end-stream urine as they tend to be contaminated, go for midstream as that is more likely to not be contaminated by bacteria on the skin and mucosa.
What are the characteristics of Neisseria gonorrhoeae
Gram neg diplococcus
Strictly aerobic
Needs blood to grow
Oxidase positive
Master of antigen variation
Pili is a virulence factor, adhesion to host cells inhibits phagocytosis
Outer membrane protein 1 - porin
OMP II - adhesion to other cells LPS → toxic effect
Neisseria gonorrhoeae clinical manifestations
Transmission frequency = 20%
Short incubation time: 2 - 6 days
Abundant with pus in local infections
Chronic inflammation and fibrosis
Sensitive for heating and drying
Targets: Urethra, cervix, rectum, eye, throat, blood
Male symptoms: yellow discharge with pus and painful urination (more so infected abroad)
Female symptoms: vaginal discharge, bleeding, and edema (more so infected in Sweden)
Neisseria gonorrhea diagnostics
Method: direct microscopy, PCR, Culture, Serology, Culture
Most sensitive and specific: Direct microscopy, PCR, Culture
Cultures need to be complemented with oxidase test, PCR, biochemical fermentation, or agglutination for confirmative tests.
Give examples of gonorrhea antibiotic treatments and resistance in sweden
Most countries have a high prevalence of resistance or decreased sensitivity against multiple NG antibiotics like:Tetracycline, Penicillin, Erythromycin, ampicillin.
This is not the case for ceftriaxone (first-line treatment), cefixime (second-line treatment), cefotaxime, and spectinomycin. Other second-line treatments: azithromycin and ciprofloxacin.
In Sweden. Ciprofloxacin is the highest along with traditional NG antibiotics (e.g penicillin G, ampicillin, etc); resistance has also been recorded in Ceftriaxone, Spectinomycin, and Cefixime (although still unusual). Resistance against Azithromycin is increasing in Sweden.
Gonorrhoea resistance mekanisms
Enzymatic breakdown or modification of antibiotics
Modification of antibiotic target molecules
Decreased influx of antibiotics into cells
Increased efflux of antibiotics from the cell
Neisseria gonorrhea naturally competent cells → uptake of foreign DNA → recombination, transformation, and conjugation.
Resistance develops via selection or acquiring chromosomal mutations or resistance plasmids.
Mycoplasma spp structure and infections
Mycoplasma spp are small bacteria having only a sterol-containing membrane (no cell wall), no amino acid biosynthesis, and are facultative anaerobes except for M. pneumoniae, a strict aerobe.
Infections and species:
M. genitalium: Urethritis in both genders and Cervicitis in women. Complications are salpingitis, reactive arthritis, conjunctivitis, and possibly associated with ectopic pregnancy and infertility.
M. hominis: Genital microflora in 15% of adults, Postpartum fever, genital infections in women, CNS infections in neonates (rare), and pyelonephritis.
U. urealyticum: Genital microflora in 45-75% of adults, possible/suspected cause of urethritis and cause of kidney stones.
How are Mycoplasma spp diagnosed and treated?
Diagnosis: PCR, serology, culturing (difficult and slow growth)
Treatment:
Azithromycin → increasing resistance in Sweden & Europe
Tetracycline → limited treatment success
Moxifloxacin → highly effective but increasing resistance
Syphilis causing Treponema pallidum: structure
Treponema pallidum is a long spiral-formed rod with a long generation time that is very difficult to culture. They can’t survive outside the body, very sensitive to dryness, heat, and disinfection. Entry into host via wounds or affected skin/mucosa and can result in congenital infection.
Syphilis clinical manifestations
Incubation time: 3 weeks
Primary stage: small wounds, swollen lymph nodes, local T.pallidum growth, and spontaneous clearance.
Secondary stage (contagious stage): Mucocutaneous lesions, lymphadenopathy, flu-like symptoms, muscle pain, headache, and fever.
Latent stage (3-30 years): T.pallidum is latent in the liver or spleen and can be reactivated (from a symptomless manifestation) in about 40% of cases.
Tertiary stage: Continued spread and invasion resulting in cardiovascular or cerebral syphilis. Congenital syphilis results in 200K stillborns/year, premature births, and fetal deaths. Screening is efficient where it’s available.
Syphilis diagnosis and treatment
Serology: Unspecific testing as antibodies cross-react with non-T.pallidum antigens and is used to track treatment success.
PCR: T.pallidum can be detected from small genital wounds in early-stage infection but also in the CSF and amniotic fluid.
Specific confirmation tests: Enzyme immunoassay (EIA) to look at IgM and blood screening, as well as Treponema passive particle agglutination (TPPA).
Treatment: Intramuscular penicillin - no resistance
Chlamydia Trachomatis strucutre and growth cycle
Chlamydia Trachomatis is an obligate intracellular bacteria, it has an cell wall with a peptidoglycan analog and major outer membrane proteins that are essential antigens that stabilize the cell wall.
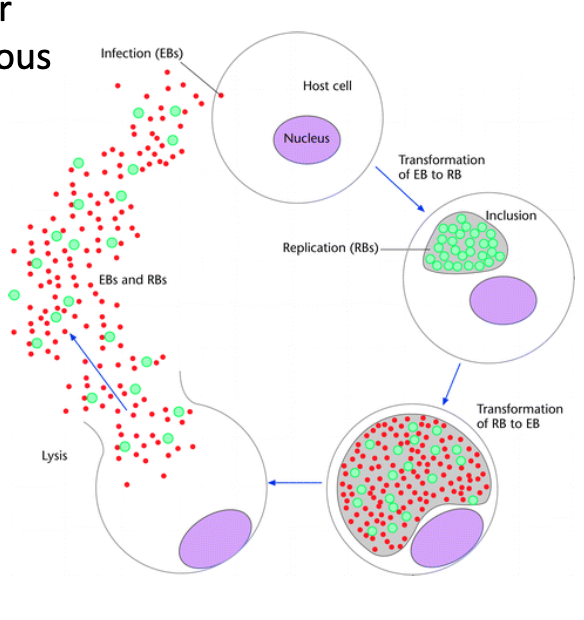
Growth cycle: Biphasic life cycle
Elementary body (metabolicly inactive, extracellular, infectious and robust) enters host cell.
EBs form inclusions where they replicate and form reticular bodies (metabolically active, intracellular, non-infectious and sensitive)
RBs transform into new EBs
Cell lysis releases EBs and remaining RBs
Chlamydia trachomatis pathogenesis
Infection of epithelial cells
Neutrophils and mononuclear leucocytes accumulate
Release cytokines
Inflammation
Tubal scars, ectopic pregnancy, infertility
54-84% of cases self-heal within one year
7.6% lead to ectopic pregnancy (5% of all ectopic pregnancies are caused by chlamydia)
10.8% lead to infertility: tubal-factor infertility (30% of all tubal-factor infertility is caused by chlamydia)
7.3 result in salpingitis (which develops into one of the three above)
Chlamydia trachomatis infections
Some chalmydia infections:
Cervicitis (cervix)
Urethritis
Pelvis inflammatory disease
Epididimytis (men)
Proctitis
Pneumonia (newborns)
Trachoma or eye disease
reactive arthritis
Endocarditis
Lymfogranuloma venereum (LGV) vs Genital chlamydia
LGV is caused by chlamydia trachomatis genotype L1-L3, is usually symptomatic, affects connective tissue and lymphatics as well, and causes severe inflammation. 30-70% of LGV patients are HIV positive.
Genital chlamydia is caused by chlamydia trachomatis genotype D-K, is usually asymptomatic, affects mucosal tissue, and causes mild inflammation
relevance if genetic differences in chlamydia trachomatis infection
Chlamydia trachomatis sampling, detection, and treatment
Sample:
Urine for men (non-invasive), can be sent via mail
Vaginal swab (non-invasive), can be sent via mail
Urethral -, cervix - and rectum swabs (invasive sampling)
Detection method: DNA extraction for PCR analysis
Treatment
Doxycycline: 100mg x2 for 7 days (for LGV 3 weeks instead of 7 days)
Azithromycin: 1g in one shot
Usually, there is no need for a control test after treatment
How is transmission rate determined
Transmission rate = mean duration of infection x transmission probability of contact x number of contacts.
Mean duration of infection is determined via lab diagnostics, treatment and contact tracing
transmission probability of contact = use condoms!!!
number of contacts = determined by individual choice