eating disorders -> treatment + prevention
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
39 Terms
what did Linienfeld et al. (2013) identify as concerns surrounding the treatment of eating disorders
out of 600 therapies identified in total, many were described as, but few had substantial evidence supporting them
found therapies e.g. dolphin-assisted therapy (???), which were not published in peer-reviewed journals
what are empirically-grounded interventions + what is the process of how they’re made (Salkovski, 2002)
refers to the process of formulating a theory of what causes a particular health condition, then performing experimental studies to test the theory (e.g. specific cognitions/schemas)
results of validity of these theories are therefore used to develop particular therapies to treat said causes
therapies are tested in clinical practice via case studies + outcome research through RCTs + efficacy trials → implemented in practice + informs clinical guidelines, which can be used to inform patients of appropriate treatment
what 4 problematic facts did Lilienfeld’s review find surrounding clinicians in practice
only 38% of clinicians reported using the strongest therapy, and some of those who did removed the key elements of it (if scared to deliver particular aspect of treatment, treatment isn’t properly conducted)
only 6% reported using evidence-based treatment manuals
more (majority) delivered eclectic or integrative therapies → not supported by evidence-based theory
many were untrained in the therapy they were using
what 5 factors in aetiology + maintenance have different therapies focused on
biology/genes
family interaction, e.g. communication style
sociocultural influences
trauma/negative life experiences
bullying
what 5 maintenance factors do effective ED treatments often feature
safety behaviours
cognitive + emotional patterns
social maintenance
family accommodation of symptoms
nutrition
what are benefits of implementing prevention of eating disorders
implementation of strategies in late childhood/early adolescence inoculates the individual against the development of eating disorder psychopathology
has massive potential benefits for limited investment, e.g. integration into school curriculum
what are two potential targets of prevention strategies
a lowering of eating + other concerns in the present
a lower level of future development of eating disorders
what prevention strategy did Carter et al. (1997) + Baronowski et al. (2001) evaluate + what were the findingsq
attempted to implement psychoeducation about dieting + eating disorders in schoolchildren ages 11-14
found pathology (significant eating problems) got worse in both cases → short term for one + long term for another
what 4 prevention approaches did Le et al. (2017) identify as effective in their meta-analysis
based on 58 studies (some with weak evidence, limiting conclusions):
media literacy approaches reduced shape + weight concerns for everyone in the young population
cognitive dissonance approaches reduce problematic eating behaviours + attitudes in high-risk groups
CBT interventions reduce risk of dieting
weight management interventions reduced some risk factors
what is the only intervention approach that has been evidenced to reduce number of people developing eating disorders
dissonance-based approaches
what does the national institute for health + clinical excellence (NIHCE) recommend as interventions for obesity
rather than specific psychological interventions, recommends ones on a wider scale including schools, local governments, families + policies e.g. taxation
this encourages lifestyle changes that reduce/prevent obesity
what is the prevalence of obesity in the UK
since 1993, proportion of obese population has risen from 14.9 → 28%
almost ¾ of people aged 45-74 are overweight or obese
this number is significant due to other health issues that accompany obesity e.g. hypertension → increased risk of stroke/heart attack
why is NIHCE (2017) a good guideline to use for treatments
does best-practice systematic reviews + guideline panels that target multiple avenues e.g. representatives of patients, clinicians, academics etc. to implement interventions
collects evidence from different avenues to find most effective interventions
these guidelines tend to informs other recommendations internationally due to robust research process
drives commissioning advice for the NHS
what are 2 factors to take into account when recommending treatments
adults vs children/adolescents
underweight vs non-underweight patients
what are 3 effective treatments for anorexia nervosa in adults + what do these have a similar level of effectiveness as
40 sessions of individual CBT for eating disorders (CBT-ED) → longer scheme than most other mental health conditions, highlighting the amount needed for positive change
20-30 sessions of Maudsley anorexia nervosa treatment for adults (MANTRA)
20-30 sessions of specialist supportive clinical management (SSCM) → uses case-management approach to increase food intake + reduce problematic behaviour
these have similar level of effectiveness to behavioural therapy
what are 2 effective treatments for anorexia nervosa in children/adolescents
AN-focused family therapy = most effective
CBT-ED or adolescent-focused psychotherapy
what 4 features/stages of AN-focused family therapy make it an effective intervention
families are often in difficult interpersonal situations, so resetting the family dynamic reduces stress + can reduce need to resort to safety behaviours. features:
non-blaming
preventing accommodating patterns occurring → starts by taking control of the child’s eating
eventually gives control back to the child
finishes with relapse prevention to ensure change is maintained
what is the most effective treatment for adults or adolescents with binge eating disorder
16-20 sessions of group or individual CBT-ED
what are the most effective treatments for adults or adolescents with bulimia nervosa
children/adolescents → family therapy for BN
adults → 16-20 sessions of individual CBT-ED, but can try guided self-help CBT-ED first
what is the most effective treatment for adults or adolescents with OSFED
recommendation is the use the therapy recommended for the most similar full syndrome, e.g. use CBT-ED for atypical AN
what recommendations are made for treating ARFID + why are conclusions limited
disorder not addressed by NIHCE (2017) due to its recency → doesn’t have enough evidential basis to draw strong conclusions as research on mental health disorders = slow developing
Thomas et al. (2021) performed small open trial for CBT-avoidant/restrictive with positive results, but no control group/randomised design means evidence is limited
what 4 pieces of recent research on EDs has corrected myths in the field
briefer therapies can be as effective for non-underweight eating disorders (Waller et al., 2018) → found 10-session CBT-ED delivered by non-specialist therapists performed at comparable level to versions twice as long
early symptom reduction enhances therapeutic alliance + treatment outcomes, but requires specific attention for younger patients + those receiving non-behaviourally oriented treatments (Graves et al., 2017)
most robust predictor of efficacy was greater symptom change during early stages of treatments (Vall + Wade, 2015) → early change = critical
no evidence that severity or duration of ED reduces effectiveness of treatment (Raykos et al., 2018)
what is the common element of what works in ED treatments
start with food as key element of treatment → issues mostly rooted in disordered food consumption, so changing diet/exposure to foods establishes a more positive relationship with it
this has physical, cognitive, emotional + social benefits
this is potentially the only necessary step in underweight ED cases, whether non-underweight cases experience extra value in psychological element of therapy
what is the need for case/risk management + what is a main example
monitors + manages risks in severe cases of EDs → as ED has the highest mortality rate of any mental health condition, intensive treatments e.g. in-patient care may be necessary
use varies across cultures → rare in UK, but common in Germany
this can be good for management + weight restoration in high-risk cases, e.g. establishing meal plans/slowly increasing dietary intake
may also improve cognitive function, which may have been lost if body weight = low enough
what are limitations of in-patient care for EDs + what is its best use
there is almost no evidence of it establishing recovery + there is a risk of creating patient dependence on the treatment
very expensive to run
therefore is best used in stage 1 of anorexia nervosa treatment (if severe enough), prior to outpatient evidence-based therapies
what two kinds of medication have recommended to treat EDs + what are limitations
medications can be useful short-term, but do not have lasting positive effects (e.g. on cognitive patterns) once they cease, as well as having side-effects
SSRIs at high doses for BN → enhances functional serotonin + reduces binges for some people taking it in short-term
novel antipsychotics for AN → may reduce anxiety but increase weight gain due to metabolic slowing (not useful obviously)
what is an example of therapy that was recommended for EDs in the past
NIHCE previously recommended dialectical BT → developed for those with complex emotional needs/personality disorders to reduce suicidality + in order to manage emotions
had good evidence due to reducing impulsive behaviours, but resulted in little change in core pathology → since overtaken by stronger evidence (e.g. of family therapy/CBT-ED)
what 3 other psychological therapies have some (weaker) evidence
interpersonal therapy (IPT) focuses on relational dynamics in friends + family to improve eating behaviours → works for BN, but requires greater number of sessions + generally less effective than CBT
focused psychodynamic approaches (FIT) focuses on psyche conflict based on Freud’s theories → effective for AN in Germany, but results not replicated
integrative cognitive-affective therapy → less effective than CBT
what are 4 examples of psychological therapies with little evidence of efficacy
mentalisation-based therapy enhances ability to attribute internal states to oneself + how you respond to them (based on psychoanalytic approaches) → mainly used for personality disorders/complex emotional needs, but less effective than CBT for EDs + takes longer to be effective (18 months)
acceptance + commitment therapy (ACT) → originally used for physical health problems; evidence has only resulted from poorly-designed studies
mindfulness-based approaches
family therapies not food/eating focused
what did Hansen et al. (2002) find the mean effectiveness of evidence-based therapies for psychological disorders was generally
50% recovery
25% improvement
20% unchanged
5% deterioration
this has been reproduced in clinical settings if therapy is delivered correctly
did Fairburn (2009; 2013) find the same recovery rate for eating disorders
50% recovery rate can still be achieved in non-underweight cases, but it is lower (30%) for underweight cases
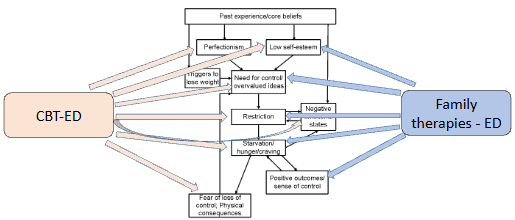
where do ED therapies have their impact
based on formulation of EDs used, different therapies will target different areas
e.g. both CBT-ED + family therapies will target factors e.g. low self-esteem + restriction
CBT-ED also targets perfectionism + fear of loss of control, while FTs target the sense of control resulting from starvation
how is homeostasis related to ED therapy
large goal of ED therapy is to restore homeostasis to reestablish healthy eating patterns by addressing diet, cognition + emotions
encourages person to overcome reasons for not eating healthily + supports person to eat in response to biological need, rather than toxic environment or psychological concerns
what 4 positive effects does addressing eating + nutrition have
reduces psychological symptoms e.g. anxiety, depression + impulse/compulsivity by increasing serotonin levels
reduces co-occurring issues with substances due to mood stability + reducing negative effects from decreased starvation
enhances cognitive flexibility + social skills
normalises + stabilises weight
these all work to increase quality of life generally
what have outcomes been for psychological therapies treating obesity (Cooper et al., 2010)
they can support weight loss in the short term, but regardless of therapy type are poor at maintaining lower weight
devised a new CBT for obesity + find in 3 conditions offered, weight gain actually increased after treatment → suggests long-term weight management is necessary
why does Brownell (2010) propose treating obesity is so difficult
suggests poor treatment + maintenance outcomes can be attributed to strong biological + environmental forces that oppose weightloss/foster regain → our evolutionary biology in combination with the toxic environment makes obesity difficult to achieve
though even 5-10% weight loss can have major health benefits
what are 4 possible interventions of support for obesity
political changes e.g. substantial sugar tax → has positive impacts on encouraging healthy eating, but has risk of fat shaming
lifestyle coaching e.g. exercise programmes for overweight patients
longer styles of therapy → relatively limited benefits
continuing care models → found to be most likely to work
what is another style of effective obesity intervention + why does it still require psychological support
long-term maintenance of weight loss through bariatric surgery → reduces amount of food that can fill the stomach, meaning one feels full sooner
psychological interventions = still necessary with this for adapting to lifestyle changes + developing preparation/maintenance strategies
what 3 symptom-based therapies does Waller (2016) suggest to address elements of ED pathology
these are not expected to produce remission/recovery:
nutritional work → restores nutritional balance to improve cognition
cognitive remediation therapy → addressive cognitive inflexibility associated with AN
support or carers