Urinary system
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
111 Terms
Function of the Urinary System is to Maintain Homeostasis
-Storage and excretion of urine
-Filtration of blood
-Release hormones
-Regulation of erythrocyte production
»»»Erythropoietin (EPO) → stimulates RBC production
-Regulation of ions and acid/base levels
F-E-H-I-A = Filtration, Excretion, Hormones, Ions, Acid-base.
Kidney disease
kidney is unable to filter toxins
Chronic kidney disease ↓ EPO → ↓ RBCs → anemia → low oxygen → organ failure
Tissue of origin
intermediate mesoderm (IM)
Pronephros
4-5 tubules
First to appear
Vestigial, non-functional
Degenerates quickly
duct develops alongside
pronephrosIts degeneration triggers mesonephros to form
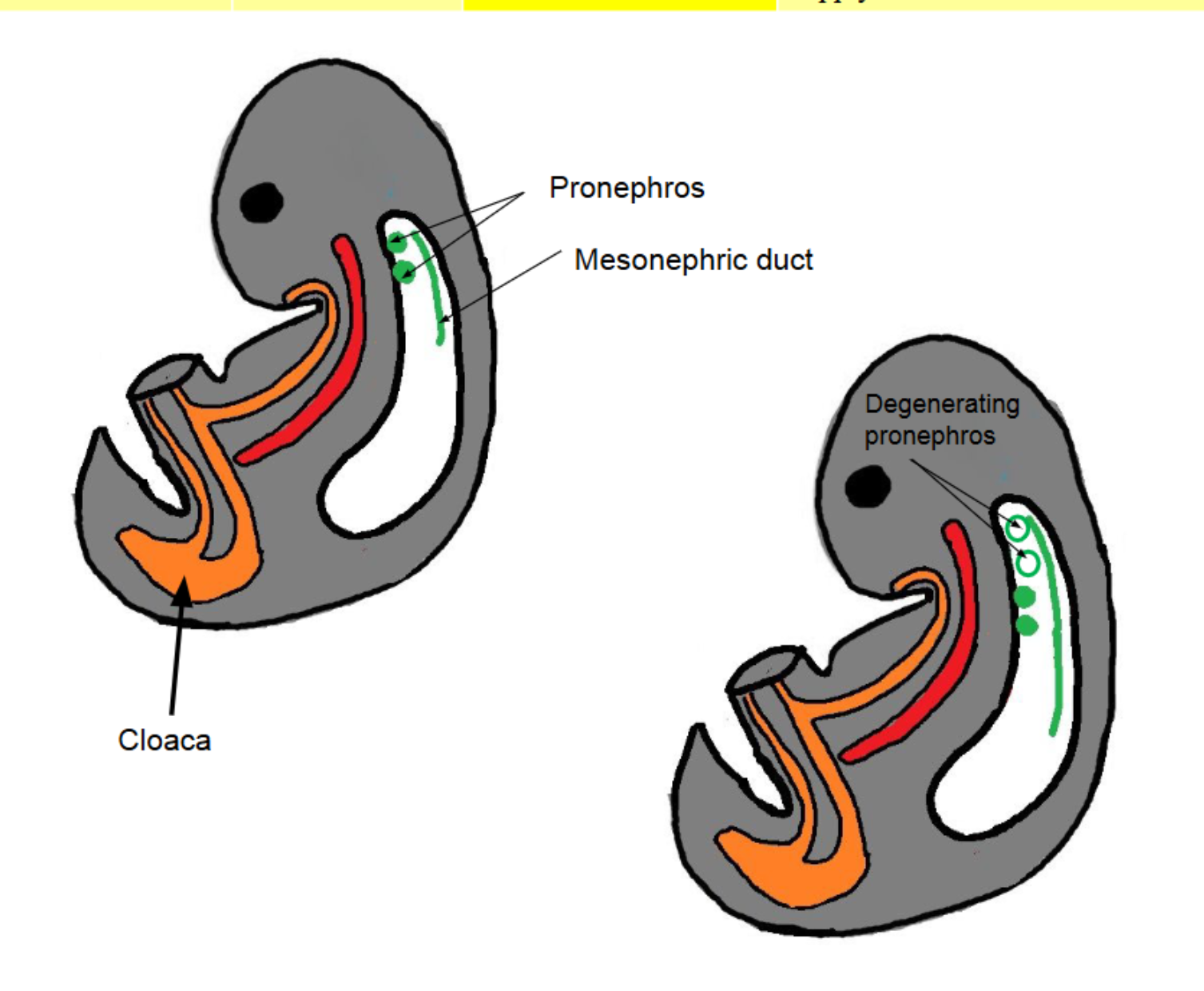
Mesonephros
Temporary functional kidney
Contains small nephrons that filter blood
Drains via mesonephric duct → cloaca
Eventually degenerates
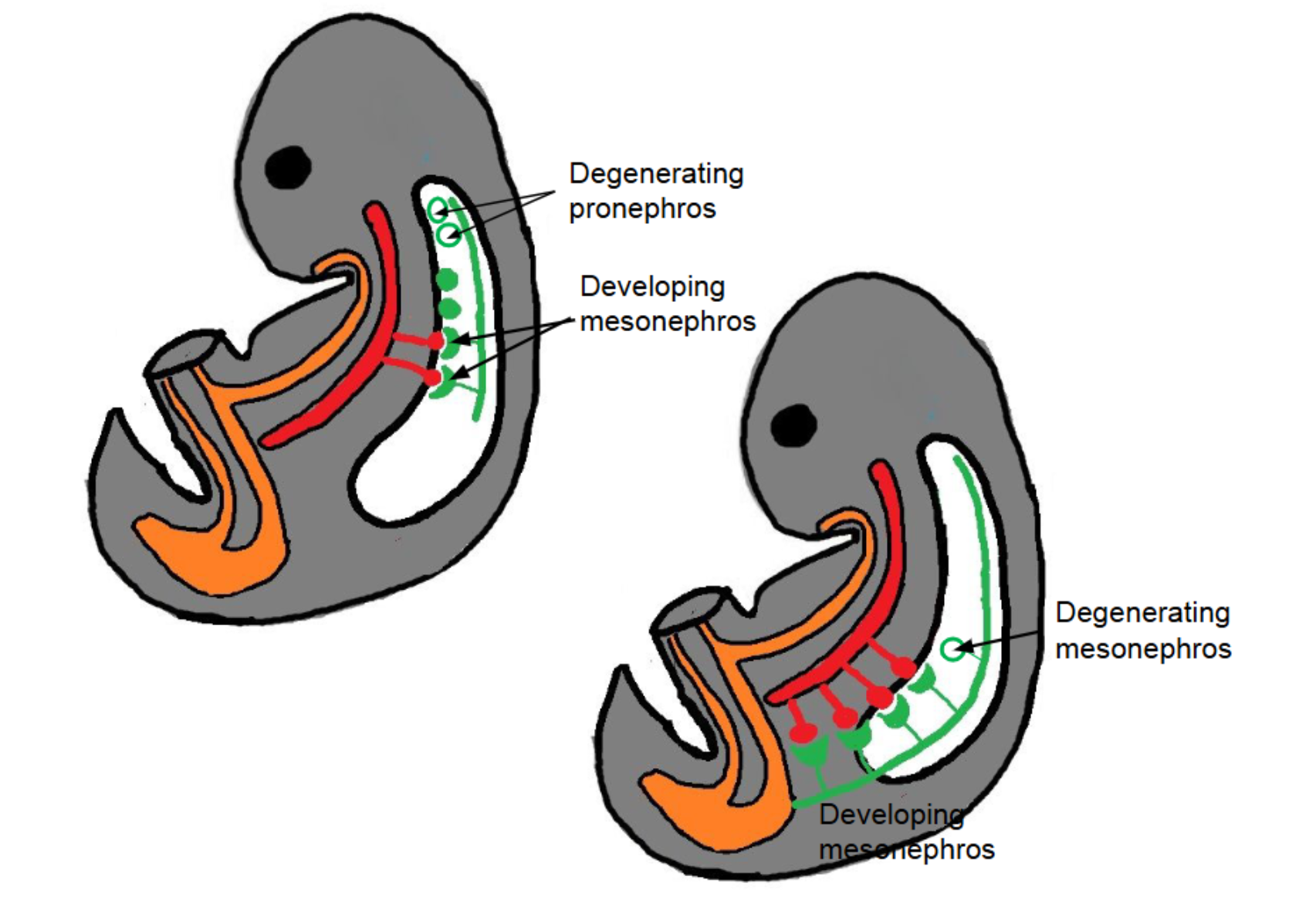
Metanephros
Adult kidney
Formed from:
Ureteric bud → urine collecting system
(ureter, renal pelvis, calyces, collecting ducts)bud=collecter
Metanephric blastema → urine-producing system
(nephrons
blasetema>builder>proudcing
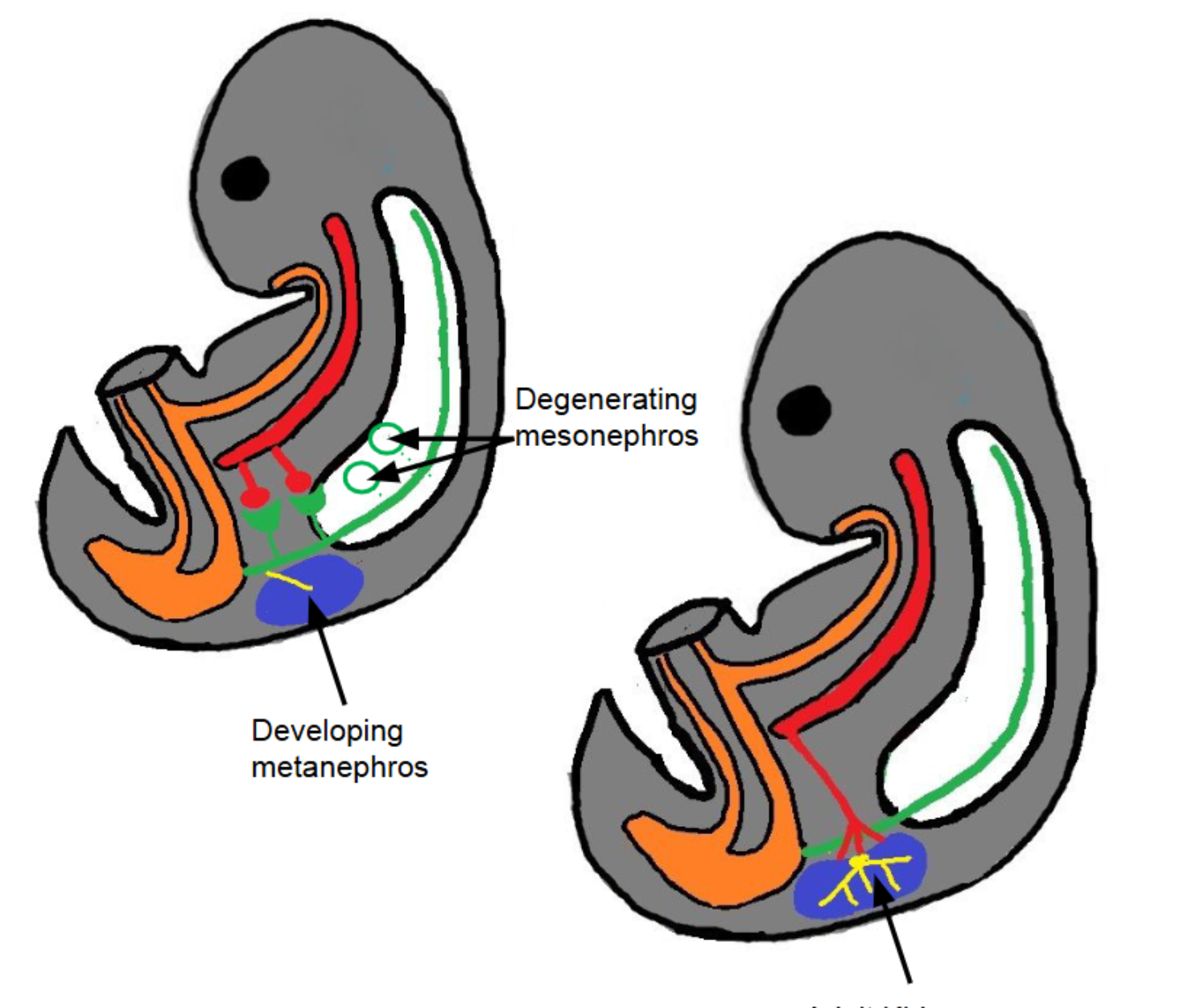
Ureteric buds will develop into the structure
that collect urine
Metanephric blastema will develop into
the structures
that produce urine
AT WEEK 7…
urorectal septum divides
the cloaca into the …
1.urogenital sinus (The urogenital sinus will develop into the
future urinary bladder and urether)
2. anorectal canal
Renal agenesis
>Rare congenital disease….
>a kidney does not form during development.
A baby normally forms two kidneys, but sometimes one or both fail to develop.
>Results from failure of metanephric
blastema to develop
Unilateral Renal Agenesis
👉 Unilateral = one side
If a person is born with one kidney missing, they usually have zero symptoms
>Because one kidney can fully take over the work of two.
The remaining kidney grows larger (compensatory hypertrophy) and handles filtration on its own
3. Bilateral Renal Agenesis
👉 Bilateral = both sides
(BOTH kidneys missing)
This is very serious because no kidneys develop at all.
Key problems it causes
Low amniotic fluid
Because fetal urine normally contributes to amniotic fluid. With no kidneys → no urine → low fluid.Underdeveloped lungs
Clubbed feet
Respiratory problems at birth
Because lungs never developed well due to low fluid.
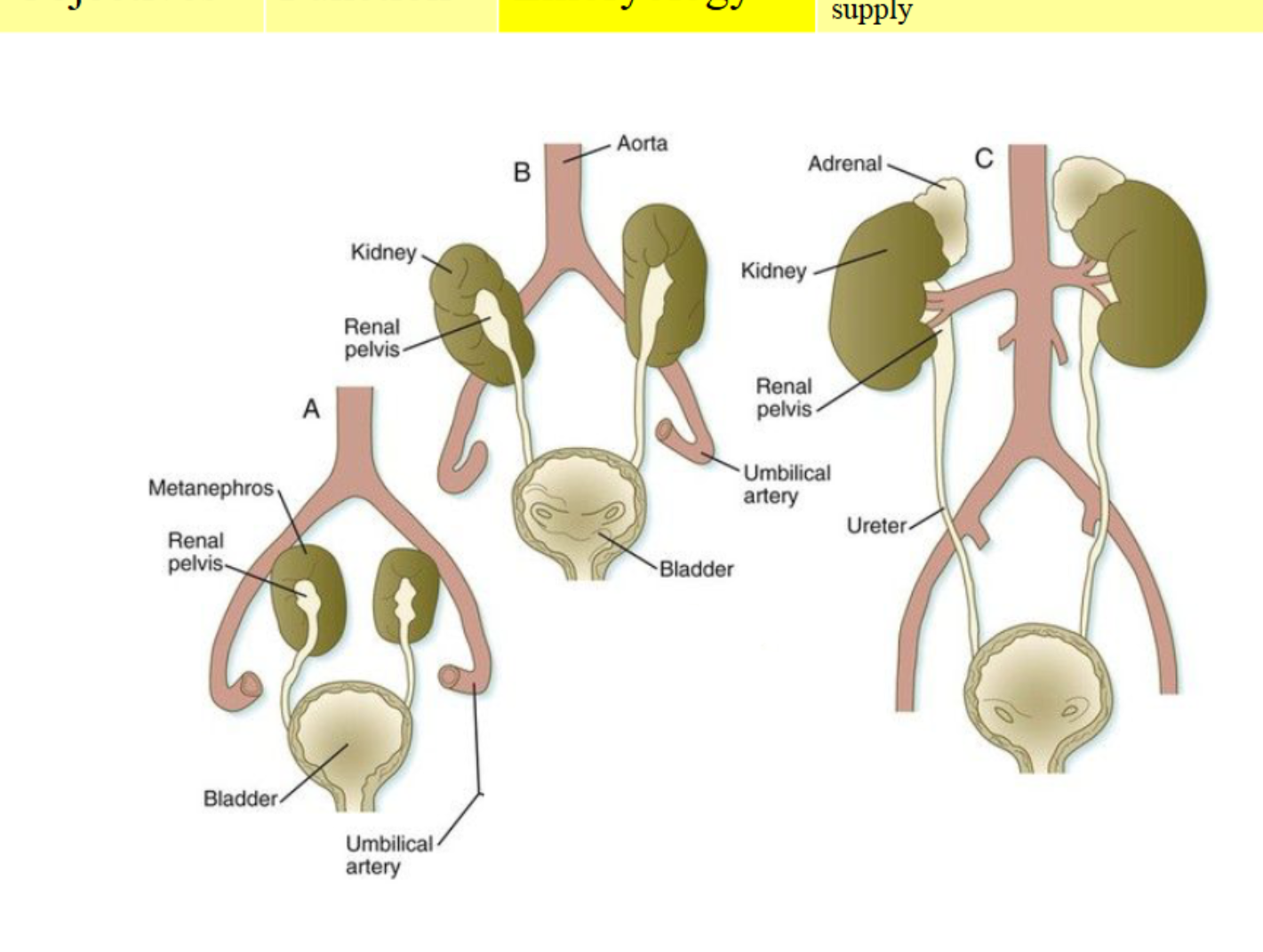
Weeks 6–9
Kidney migration
Kidneys ascend (superiorly)from pelvis → lumbar region
Receive temporary arteries during ascent
Final position at L1–L2 region with permanent renal arteries FROM ABDOMINAL AROTA
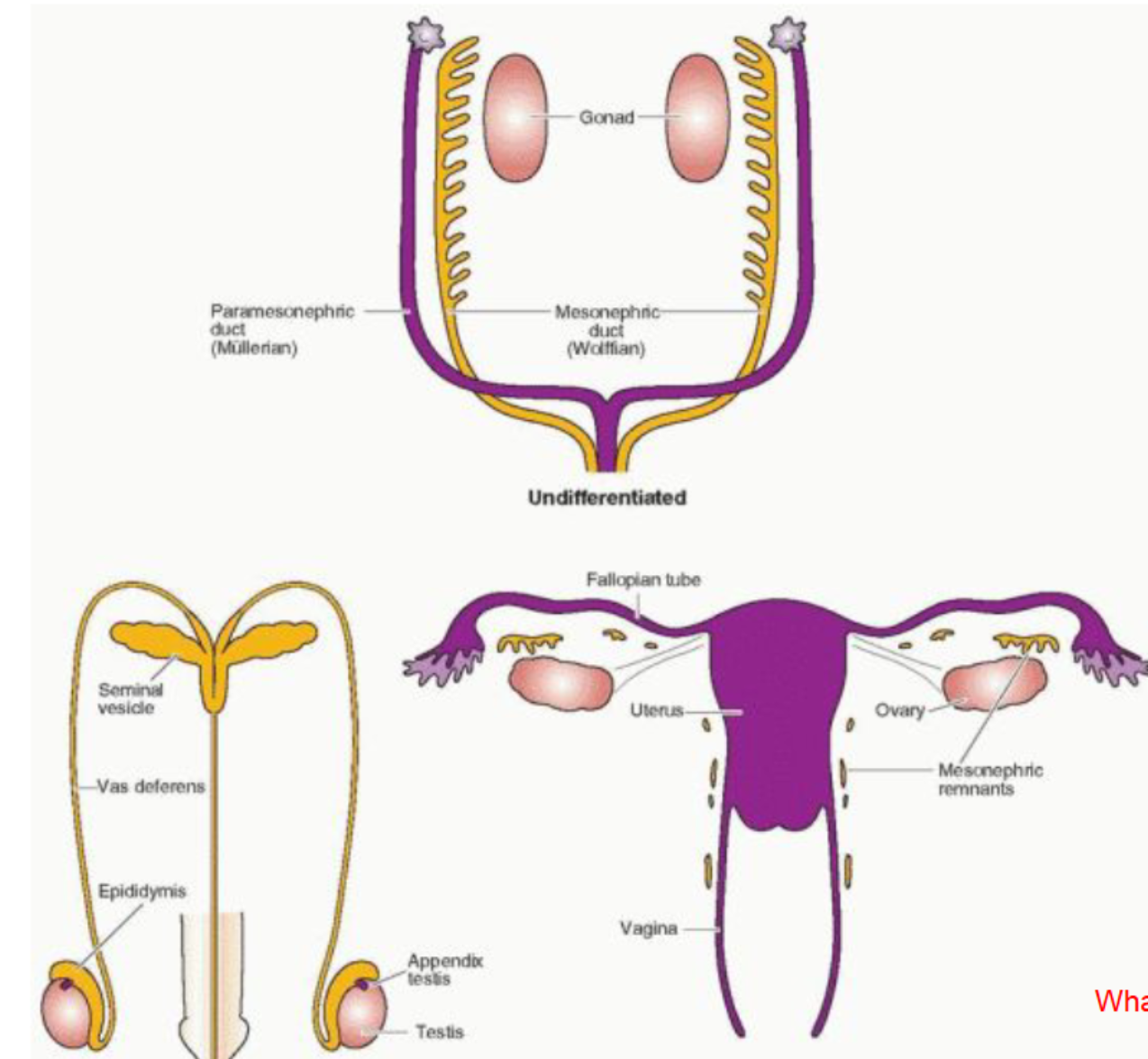
Indifferent duct system
Testosterone present → mesonephric duct kept (male structures)
No testosterone → paramesonephric duct kept (female structures)
Paired Kidneys →
filter blood & produce urine
convert filtrate to blood
Ureters, Urinary bladder,
Urethra:
(collectively referred to as the
urinary tract) transport the urine
out of the body)
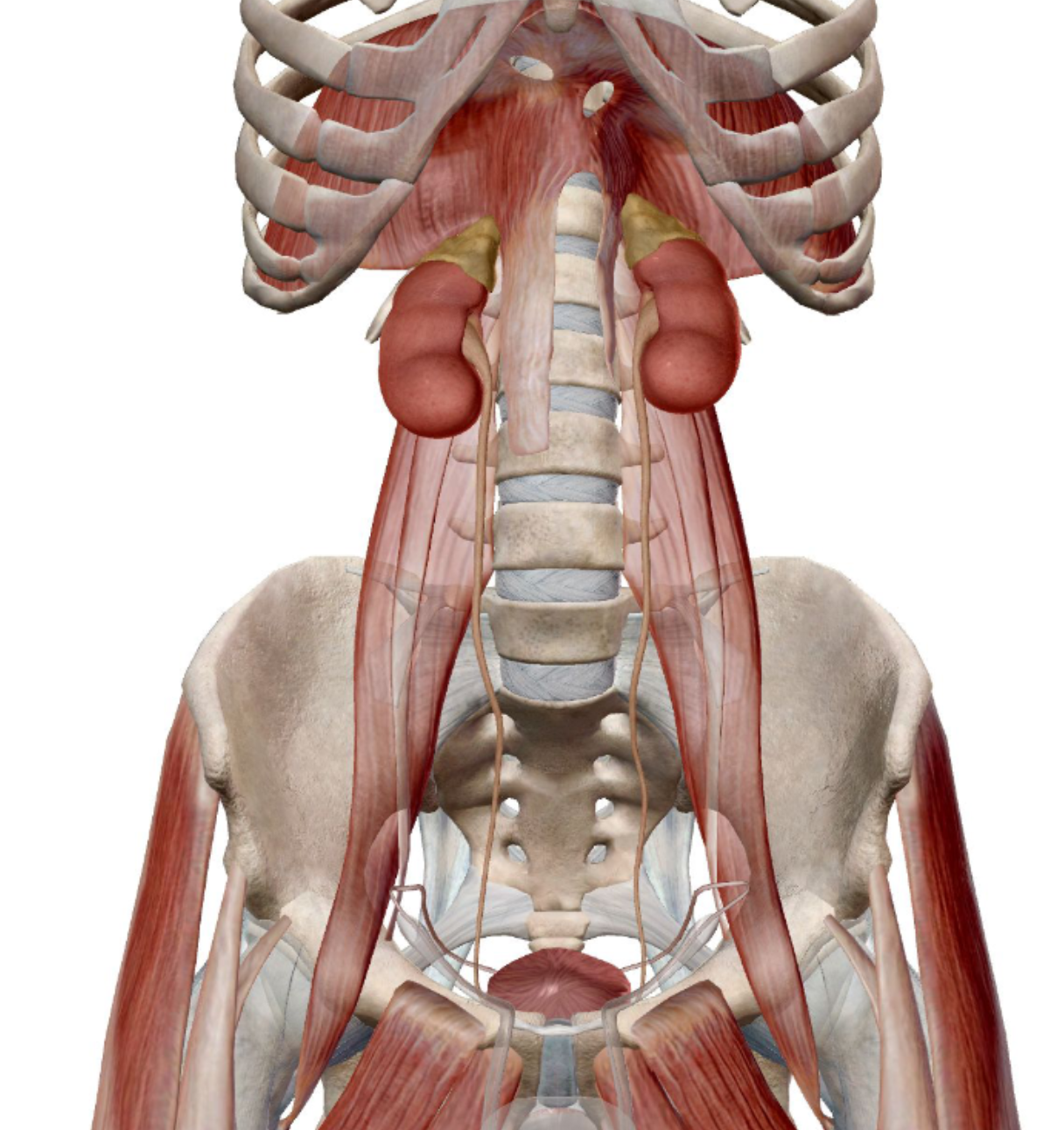
Kidney location & appearance
Retroperitonea l(located behind the peritoneum.)
Superior border at T12, inferior at L3
Right kidney lower/inferior (liver pushes it down)
Reddish-brown
Adrenal gland/Suprarenal sits on top of each kidney
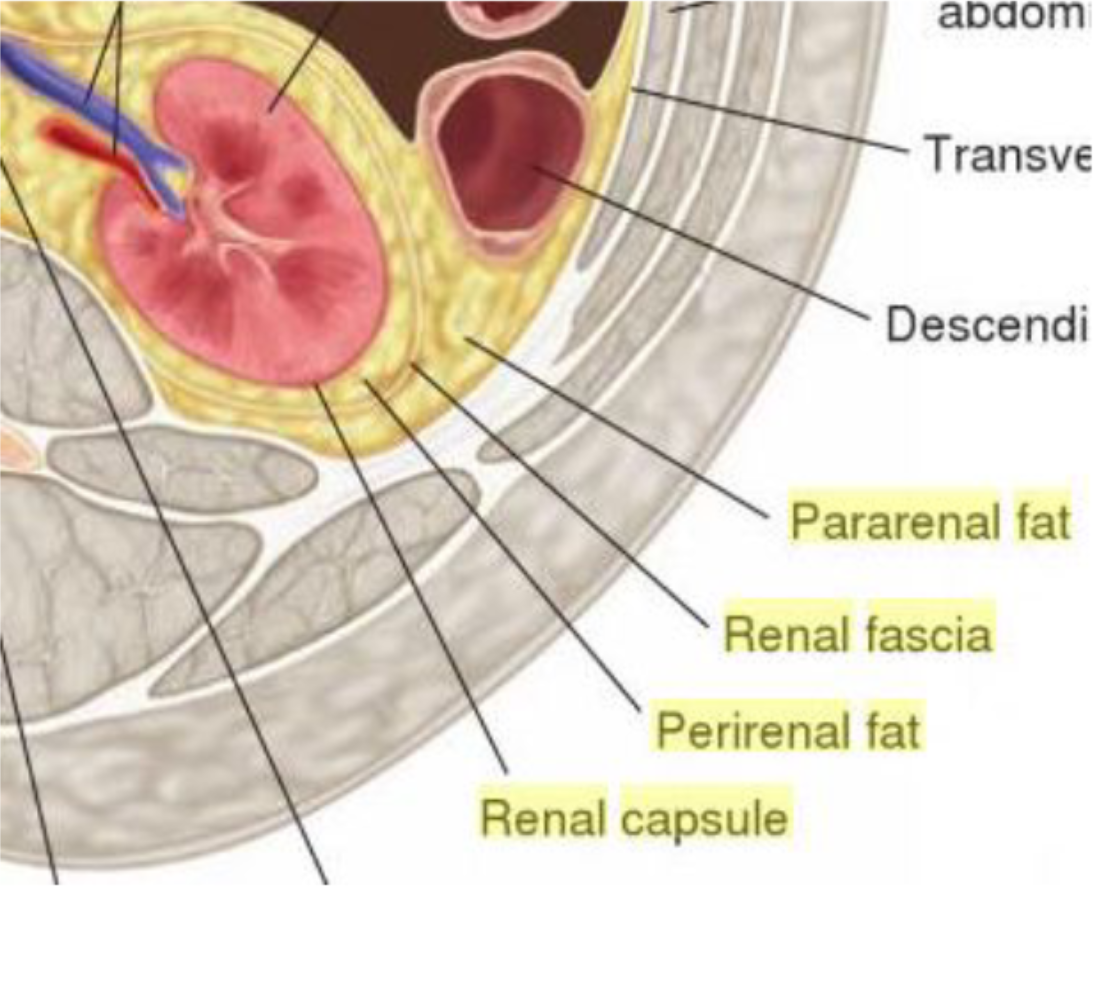
Kidney has 2 surrounding fat layers
Perirenal fat + pararenal fat
→ Cushion and protect kidney.
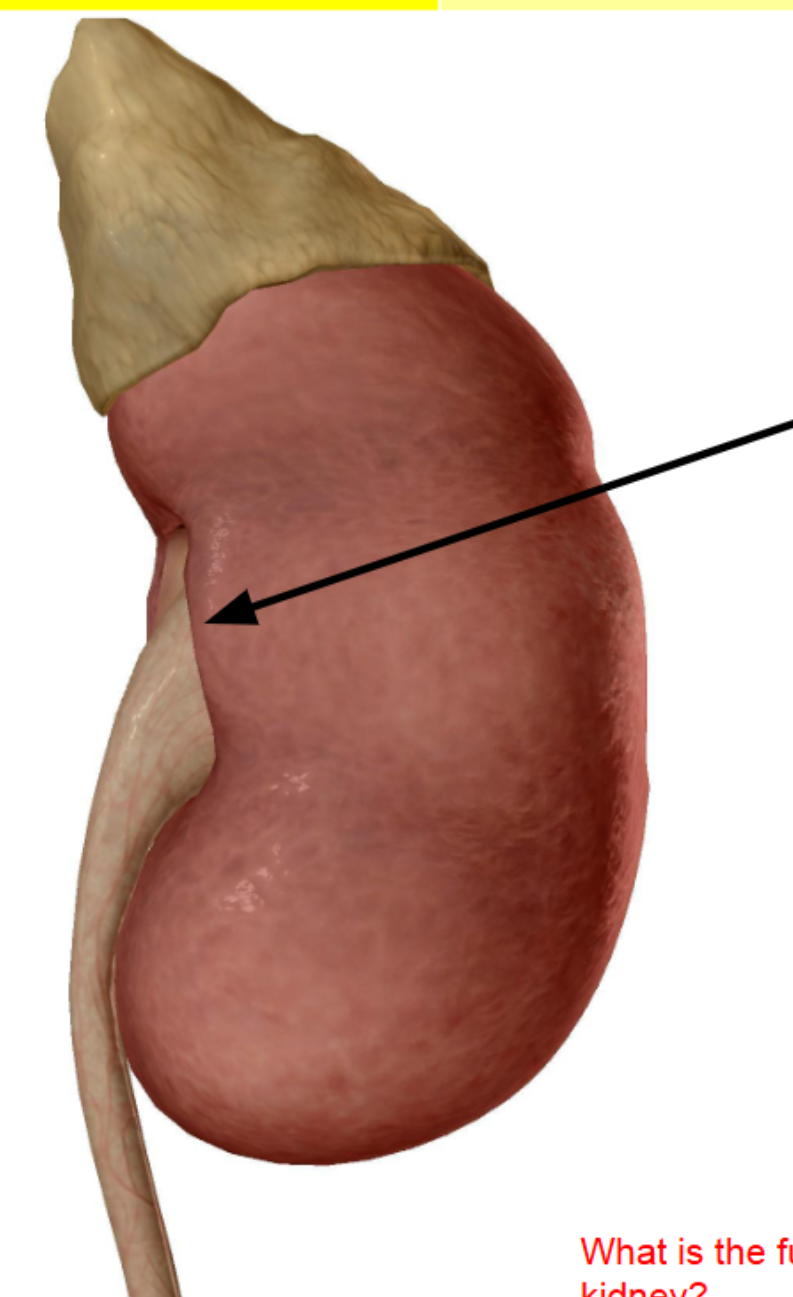
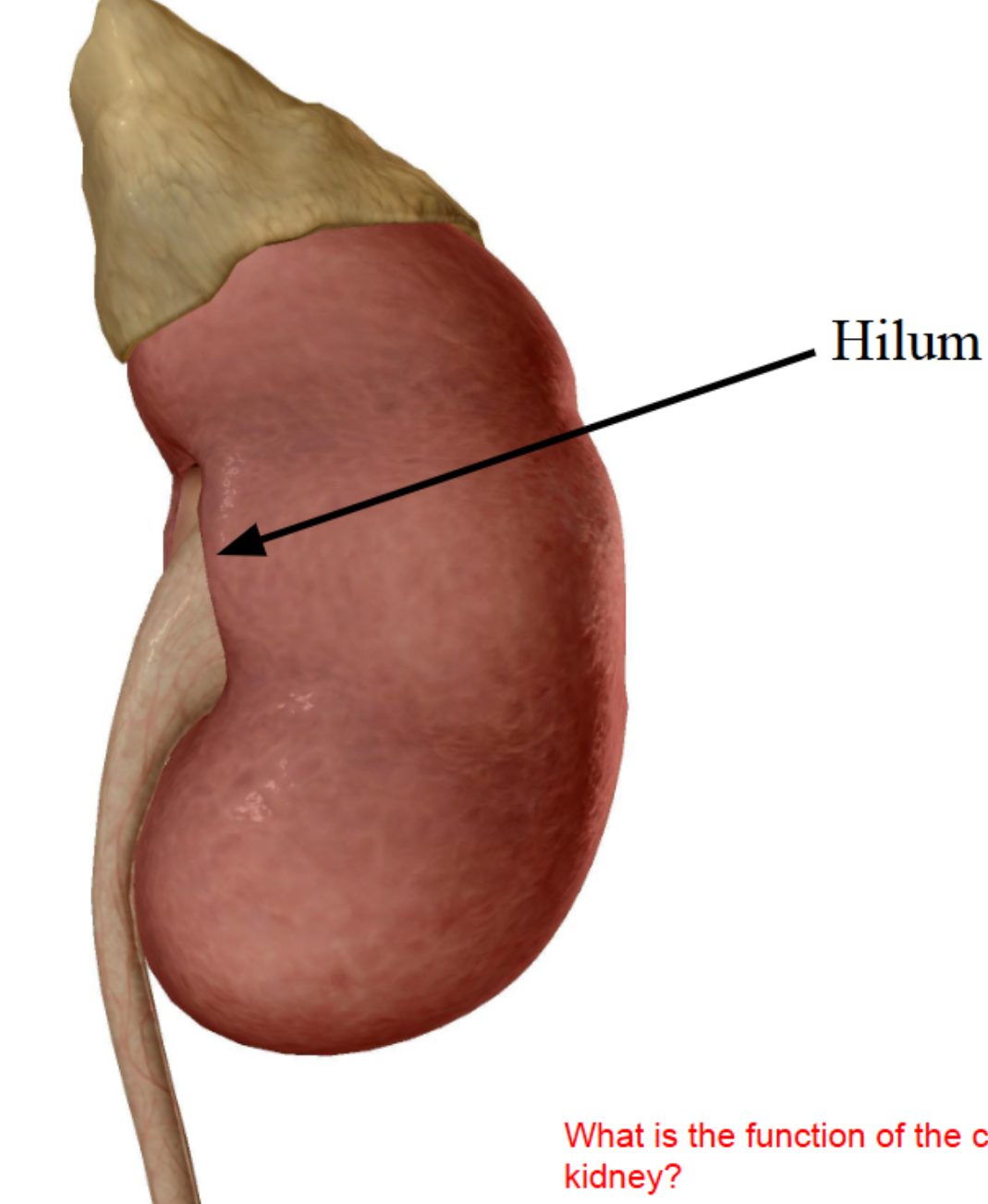
black arrow is
Concave medial border: hilum
Hilum = entry/exit for vessels + ureter
Renal capsule
Dense irregular CT:
Maintains shape
Protects from trauma
Prevents infection spread
The kidney is divided into…
1.the cortex (outer)
2.medulla (inner) and the
renal pelvis
Contains medullary pyramids
Renal columns (cortex tissue between pyramids)
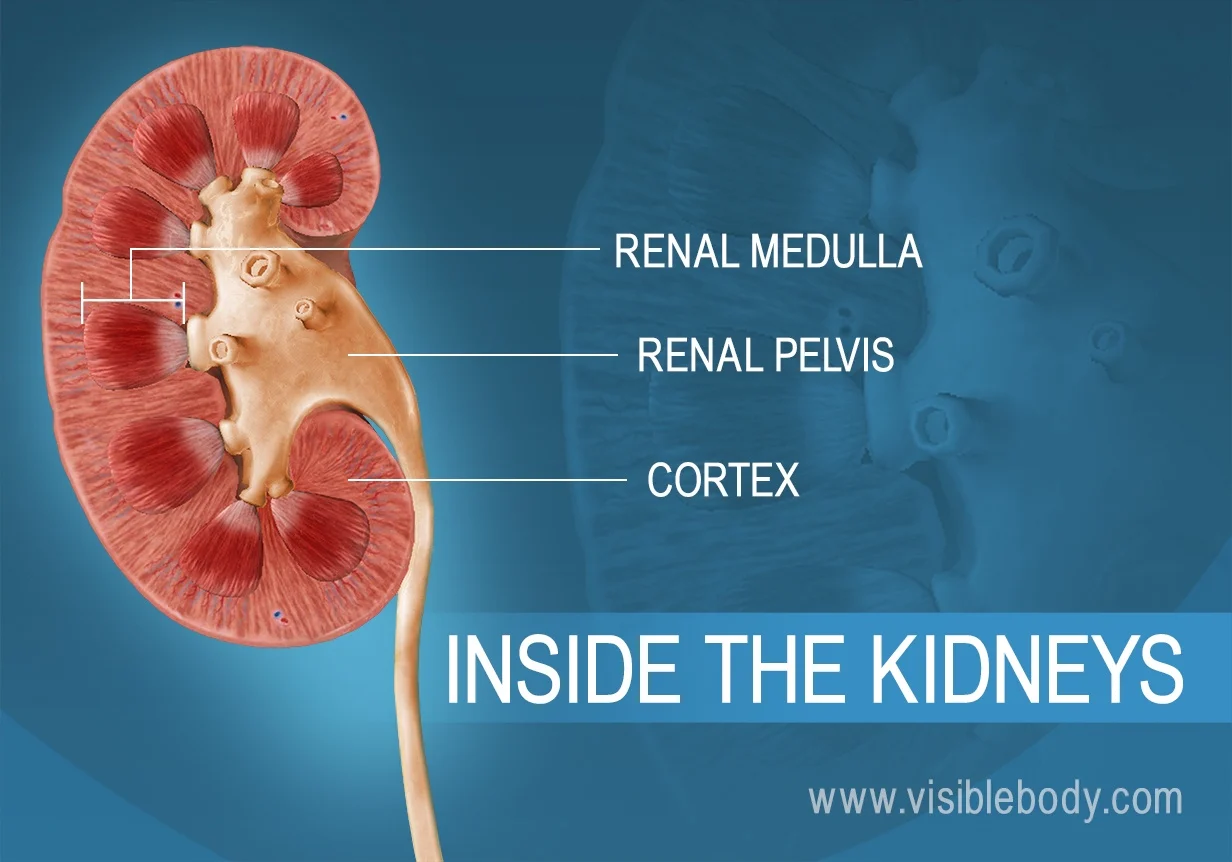
Where is urine produced?
renal (medullary pyramid) via the nephrons
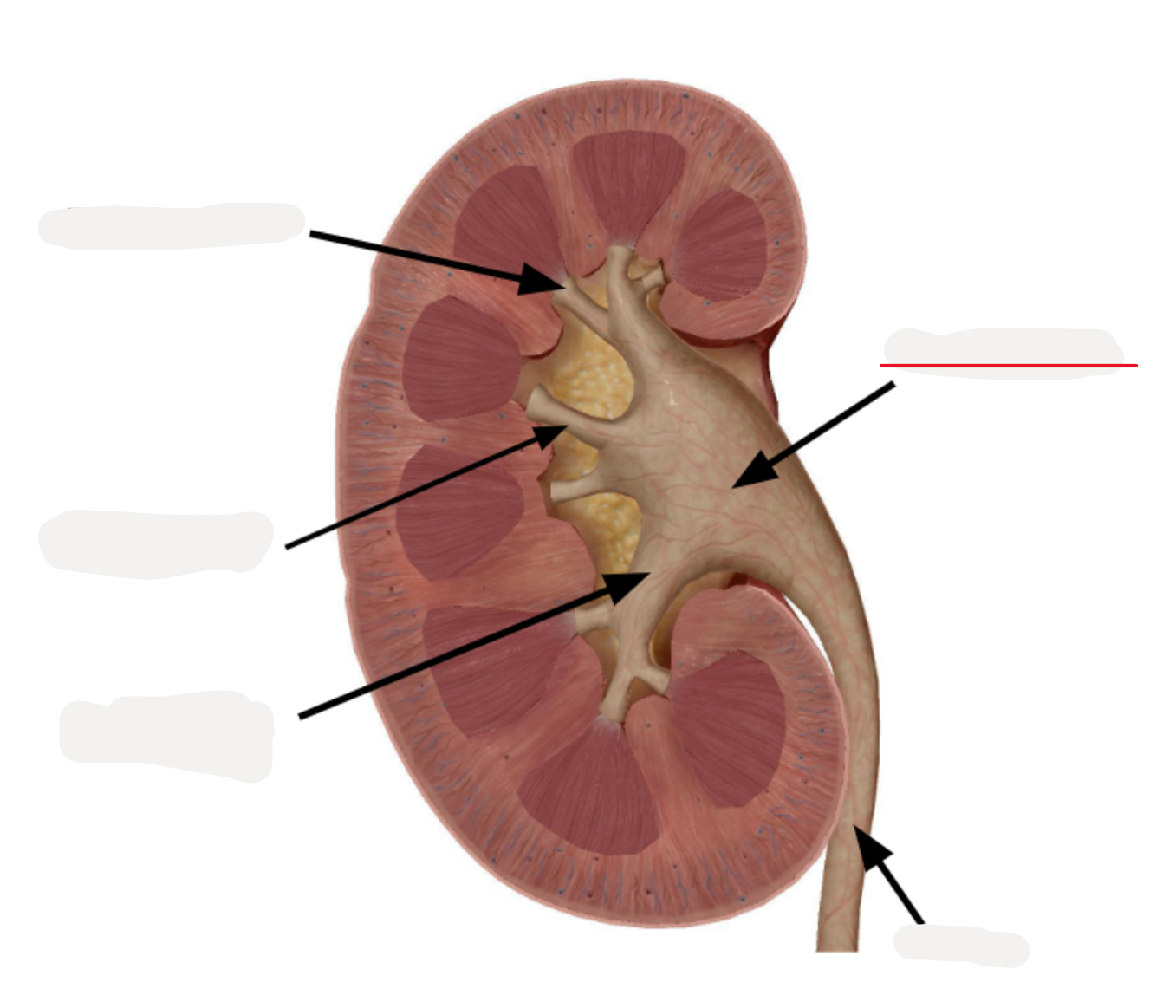
Renal pelvis
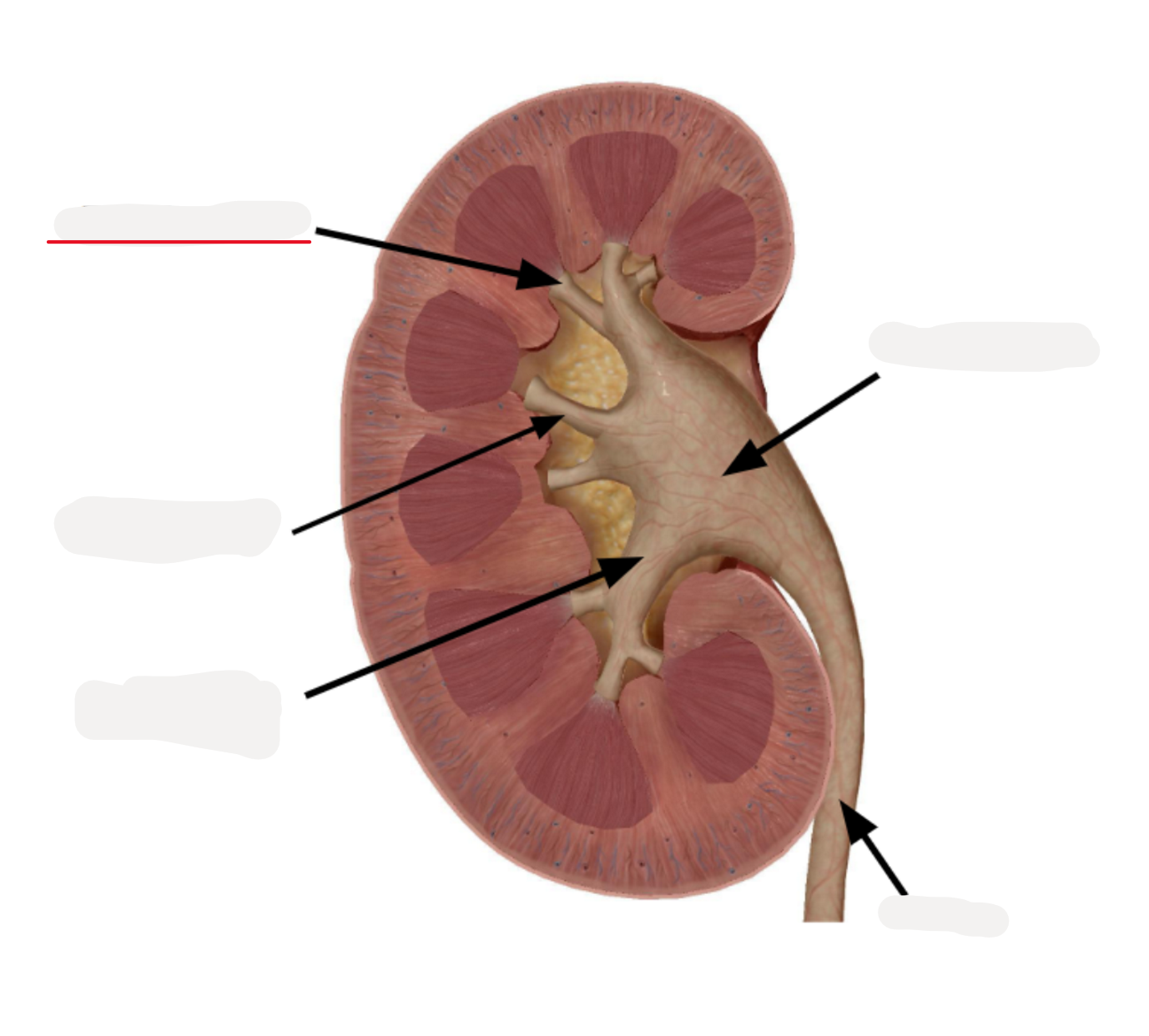
Renal papilla
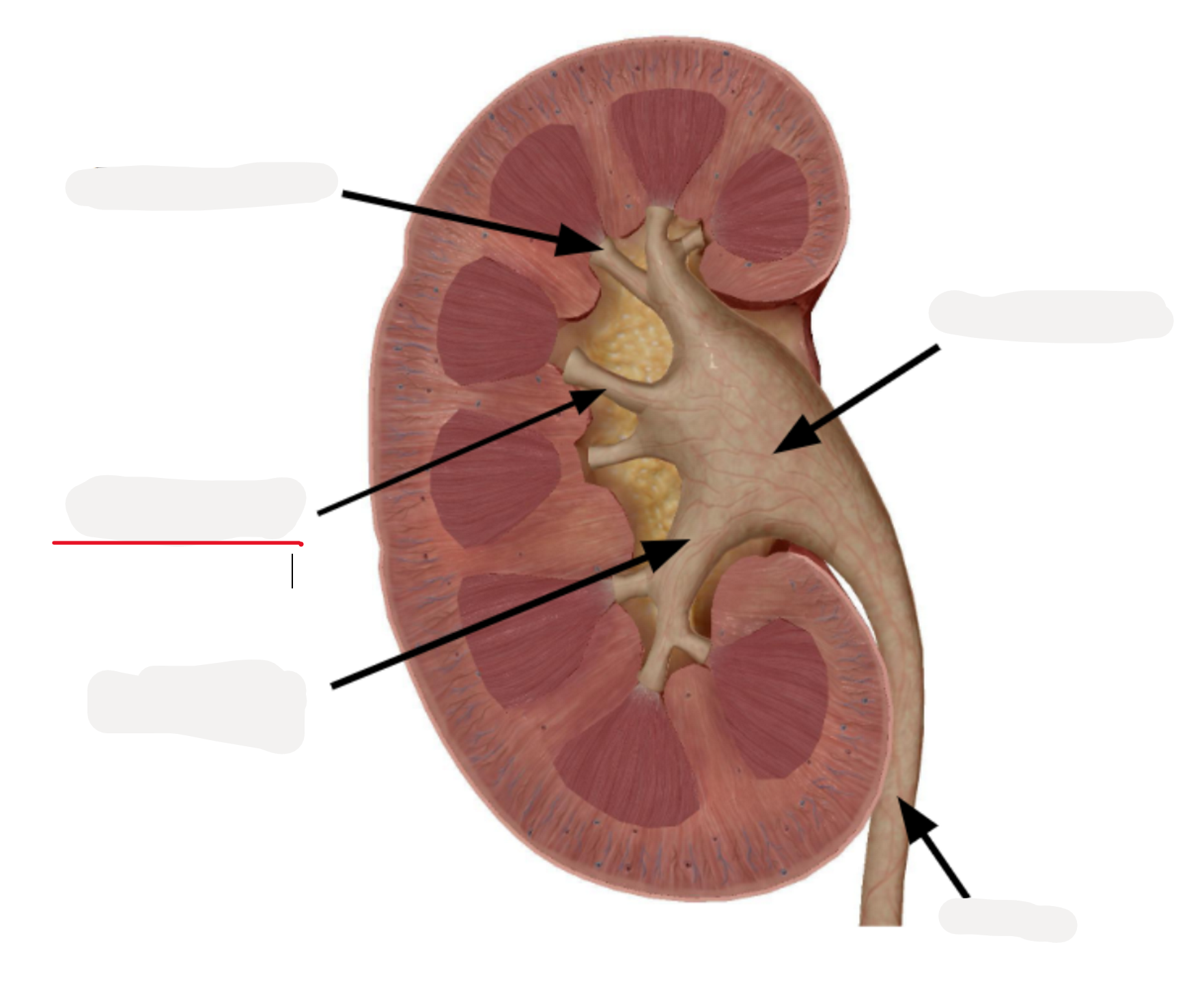
Minor calyx
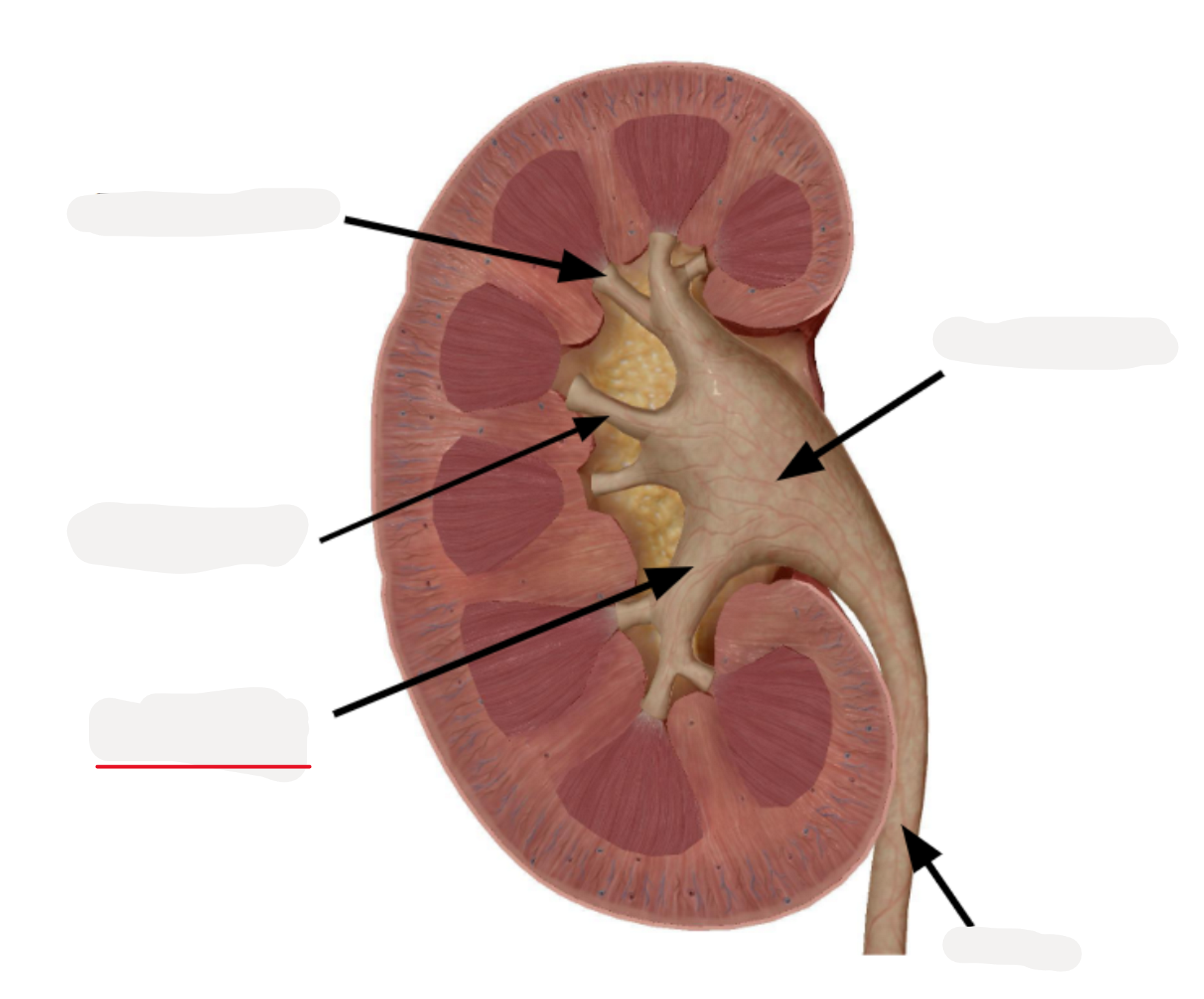
Major calyx
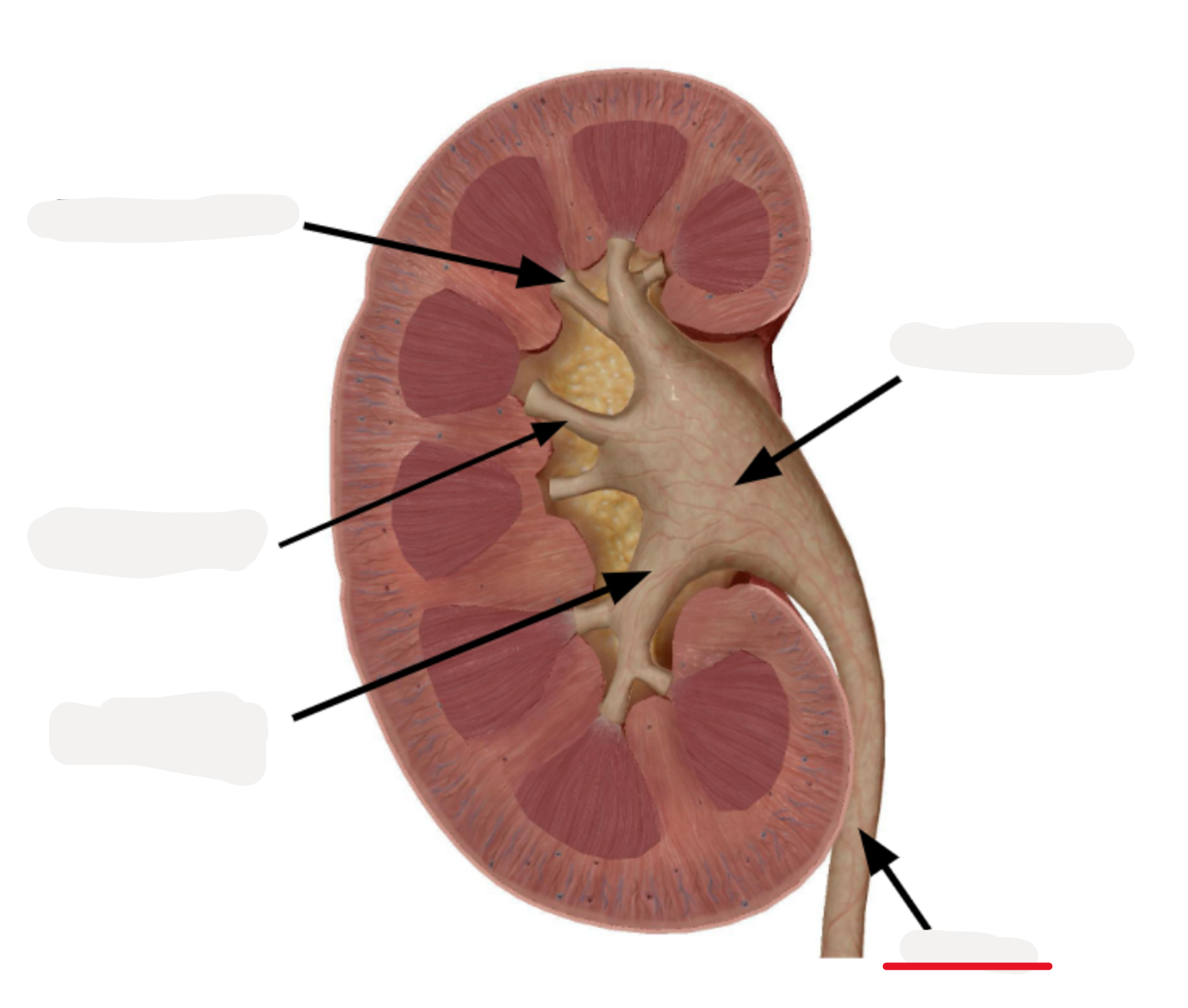
Ureter- urinary bladder
Urine collection system pathway
Renal papilla → Minor calyx → Major calyx → Renal pelvis → Ureter
"Pee Makes My Red Ureter" = Papilla → Minor → Major → Ureter.
KIDNEY MAIN FUNC IS
TO FILTER BLOOD
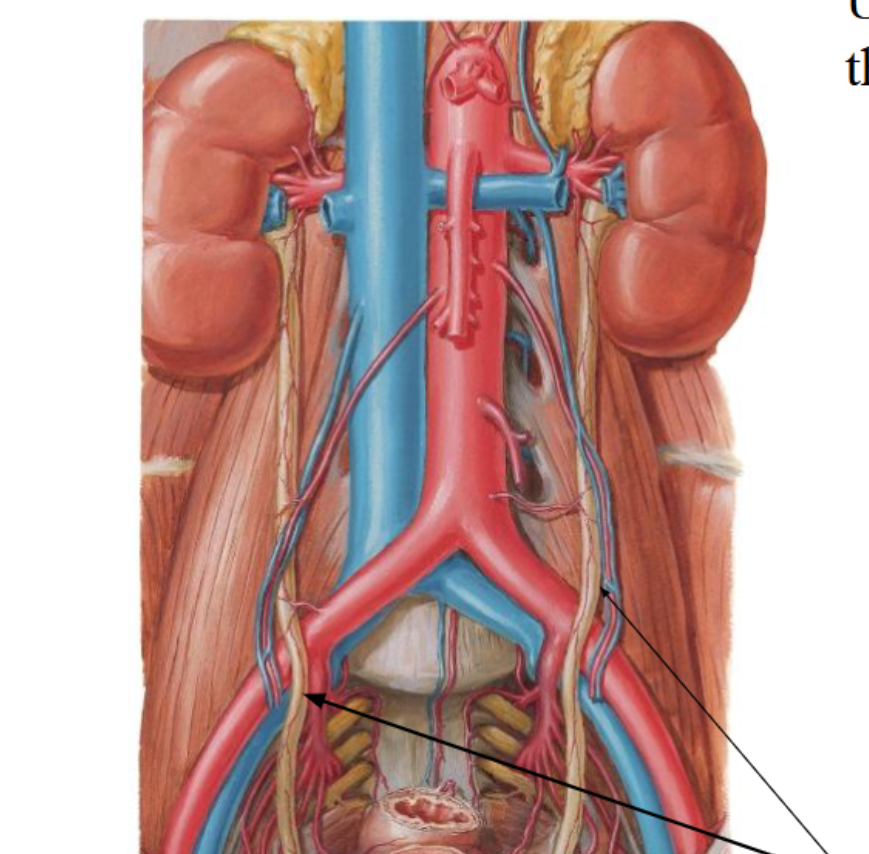
⭐ Arterial Blood Flow Into the Kidney
Blood reaches the kidneys through the renal arteries.
These branch directly off the abdominal aorta.
→ This provides a high-pressure, high-volume blood supply needed for filtration.
⭐ Venous Drainage From the Kidney
Renal veins return deoxygenated, filtered blood back to the inferior vena cava (IVC).
Important relationship:
Renal veins lie superior to renal arteries at the hilum
Asymmetry Between Left and Right Renal Veins
Because the IVC sits on the right side of the body:
Right renal vein
Very short
Drains directly into the nearby IVC
Left renal vein
Much longer because it must cross the midline to reach the IVC
The left renal vein collects blood from the left gonadal
veinPasses under the superior mesenteric artery (SMA)
→ This anatomical relationship explains Nutcracker syndrome
“Renal Vein is on Top!”
Renal vein sits superior to artery at the kidney hilum.
⭐ Left Gonadal Vein Drainage
The left gonadal vein (ovarian/testicular) drains into the left renal vein
The right gonadal vein drains directly into the IVC
Why this matters:
This is why varicoceles are more common on the left side—because drainage is more easily compressed.
“L→L→IVC”
Left gonadal → Left renal vein → IVC
Nutcracker syndrome
Left renal vein compressed between SMA + aorta → varicocele, blood pooling in gonads.
happens when the left renal vein gets squeezed between two arteries,(superior mesenteric artery and the abdominal aorta)
blocking blood flow and causing backed-up blood in the gonads.
>Causes varicocele and toxic pooling of blood in the gonad
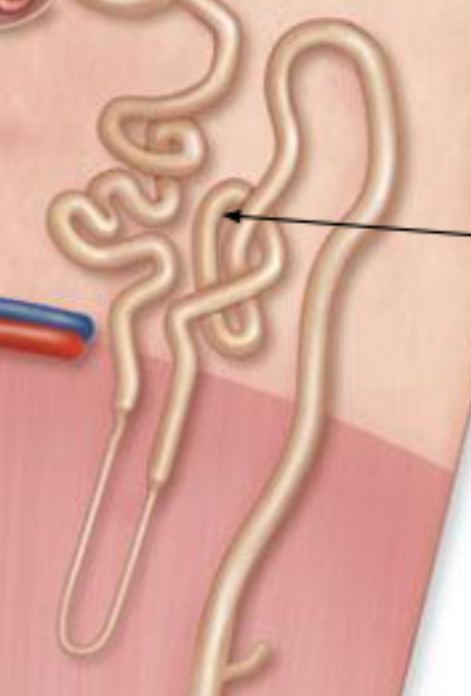
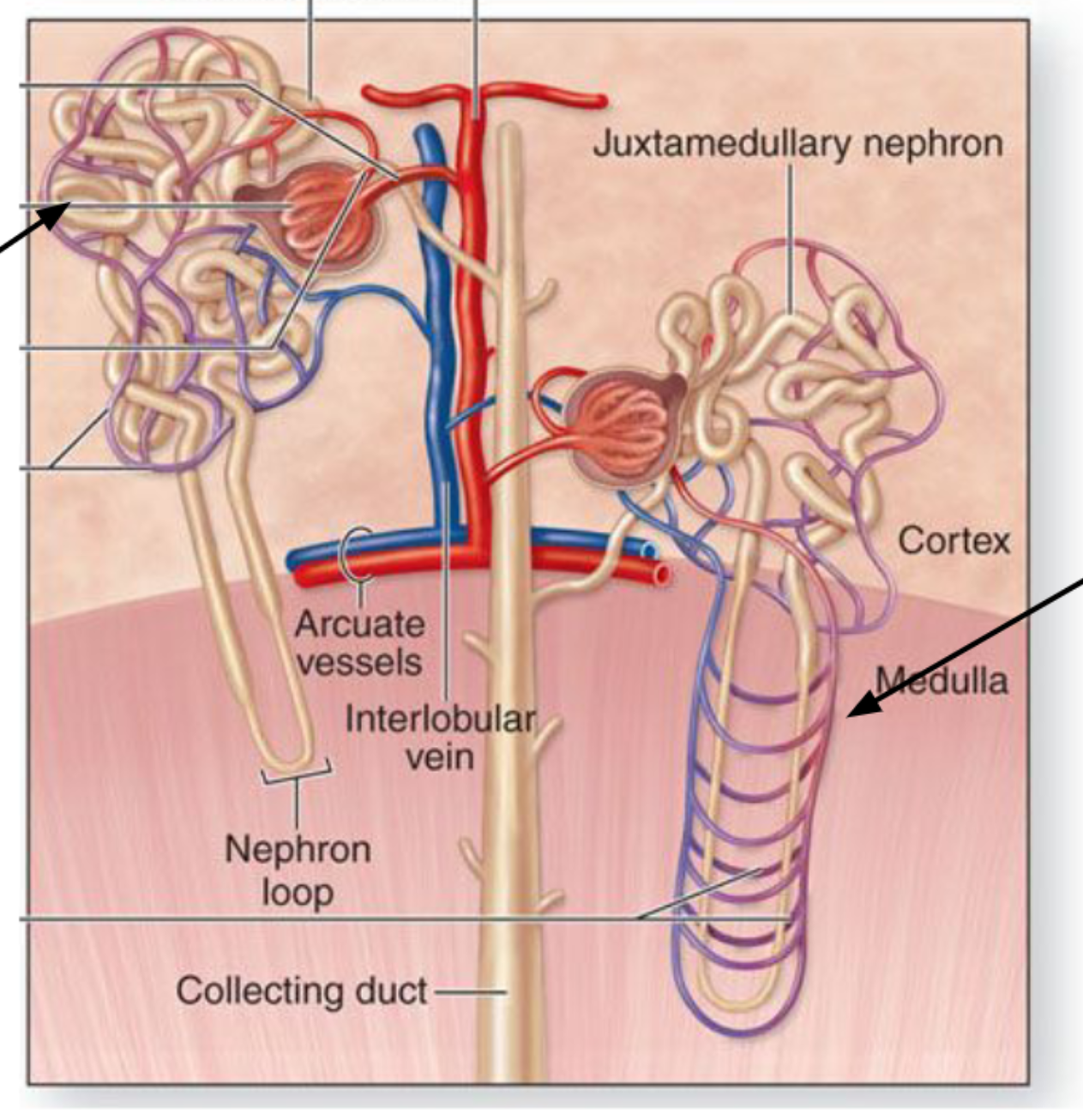
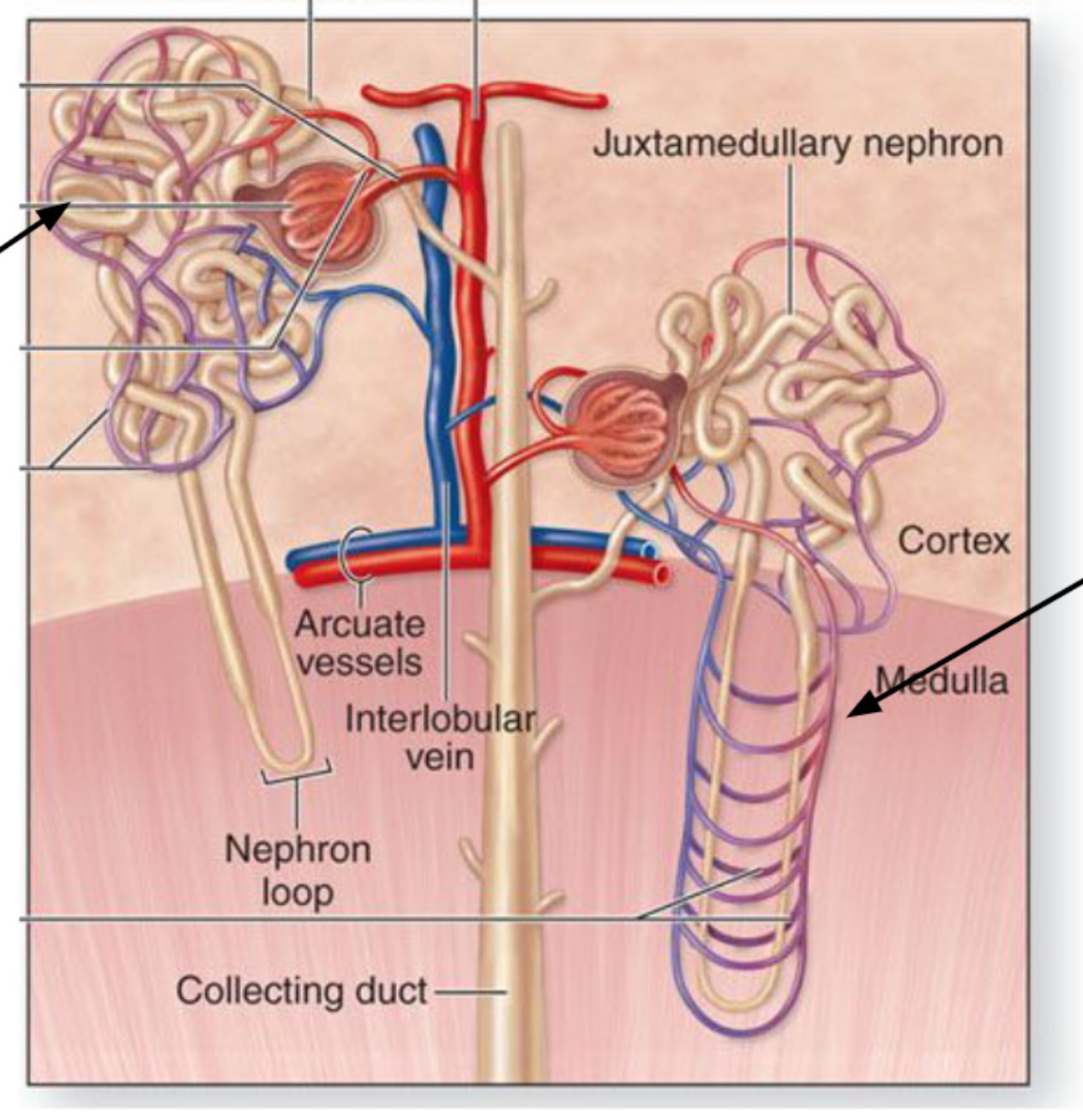
Arterial flow into kidney
Renal artery → Segmental → Interlobar (between pyramids) →
Arcuate (arch over pyramids) → Cortical radiate/interlobular →
Afferent arteriole → Glomerulus → Efferent arteriole
Really Smart Intelligent Anatomy Class Always Gets Easy
Interlobar = between pyramids
Arcuate = arches over pyramids
Cortical radiate = radiates into cortex
Arteries =
carry blood AWAY from heart (oxygen-rich)
veins =
carry blood TOWARD the heart (oxygen-poor)
V-A-U = “Veins Always Up”
At the kidney hilum → Vein on top, artery in middle, ureter on bottom.
Kidneys →
Ureters →
carry urine to bladder
Urinary bladder →
store urine
Urethra →
excrete urine
Q: What vessels bring blood into the glomerulus?
A: Afferent arterioles. - are the
smallest branches which
create capillary balls called
glomeruli
Q: What vessel drains blood away from the glomerulus?
A: Efferent arteriole.
Q: What are the 5 parts of the nephron?
A: Corpuscle, PCT, Loop of Henle, DCT, Collecting duct.
Q: What are the three processes of urine formation?
A: Filtration, reabsorption, secretion.
Q: Which layer of the glomerular capsule contains podocytes?
A: Visceral layer.
Q: Which nephron segment has tall microvilli?
A: PCT.
Q: What capillaries surround the loop of Henle?
A: Vasa recta.
Q: What hormones act on the collecting duct?
A: ADH and aldosterone.
Q: What type of epithelium lines the ureter and bladder?
A: Transitional epithelium.
Q: Why do ureters enter the bladder at an angle?
A: To form a one-way valve preventing urine reflux.
Q: What carries urine from kidney to bladder?
A: Ureters.
Q: List the path of urine from collecting duct to outside body.
A: Papilla → Minor calyx → Major calyx → Renal pelvis → Ureter → Bladder → Urethra → Out.
Q: What structure collects filtrate in the renal corpuscle?
A: Capsular space.
Q: What epithelium type allows the bladder to stretch?
A: Transitional epithelium.
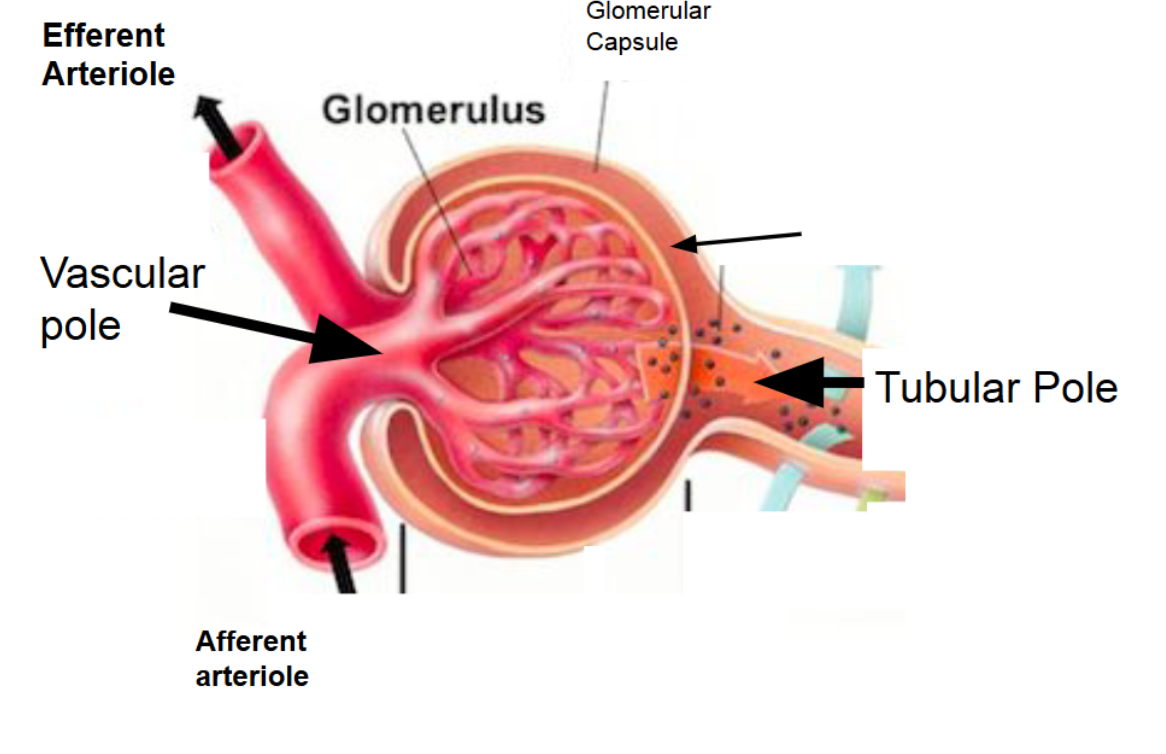
The glomerulus
ball” of capillaries for filtration.
a tangle of
capillaries that originate from
the afferent arteriole
Cortical arteries
branch from arcuate arteries and enter the cortex.
Blood Supply to the Glomerulus Key Points
Cortical arteries branch from arcuate arteries and enter the cortex.
They give rise to afferent arterioles → the vessels that bring blood into the glomerulus.
The glomerulus is a “ball” of capillaries for filtration.
Efferent arterioles carry blood out of the glomerulus.
Big idea:
Afferent = Arrive, Efferent = Exit
Nephron Func.
Modify filtrate → create final urine.
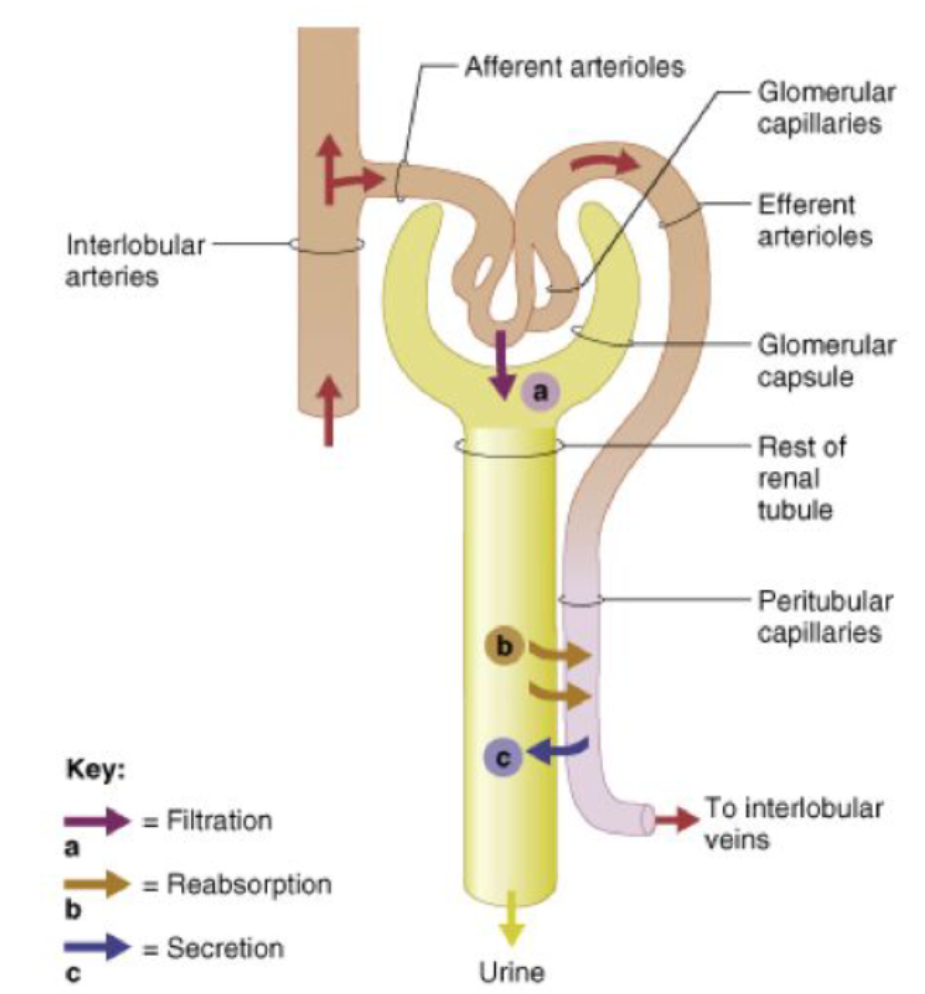
Processes of Urine Formation
Three key processes:
Filtration — blood → filtrate
Reabsorption — filtrate → blood
Secretion — blood → filtrate
Why?
Filtration alone is NOT selective → body must reabsorb what it needs and secrete what it doesn’t.
Filtration and Secretion
— blood → filtrate
Reabsorption
— filtrate → blood
Renal Corpuscle includes:
Glomerulus (capillary tangle)
Glomerular capsule (Bowman’s capsule)
Visceral layer: podocytes
Parietal layer: simple squamous epithelium
Capsular space: where filtrate collects
Glomerular capsule (Bowman’s capsule)
Visceral layer: podocytes
Parietal layer: simple squamous epithelium
Capsular space: where filtrate collects
Visceral layer
podocytes- forms a
leaky filtration membrane
Parietal layer:
simple squamous epithelium
Capsular space:
where filtrate collects
also separate visceral and parietal
Renal corpuscle
glomerulus + glomerular capsule
Renal Corpuscle poles are
vascular and tubular pole
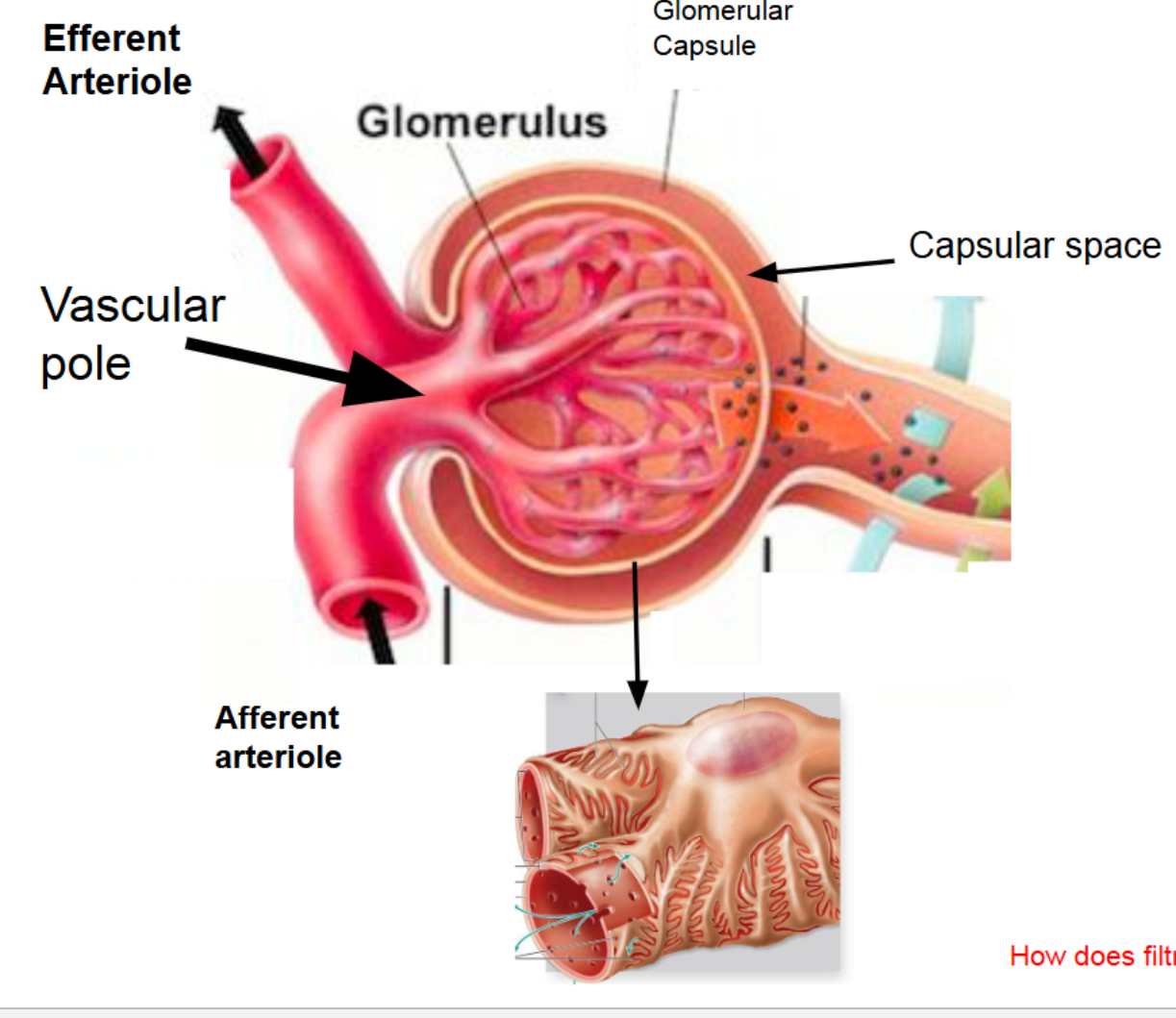
Filtration Process:
modified
1. Blood enters the glomerulus from the
afferent arteriole
2. High pressure forces blood against the
filtration membrane
3. Filtration membrane allows the
passage of smaller solutes into the
capsular space
NOTE: This method of filtration is not
selective
Filtrate must be
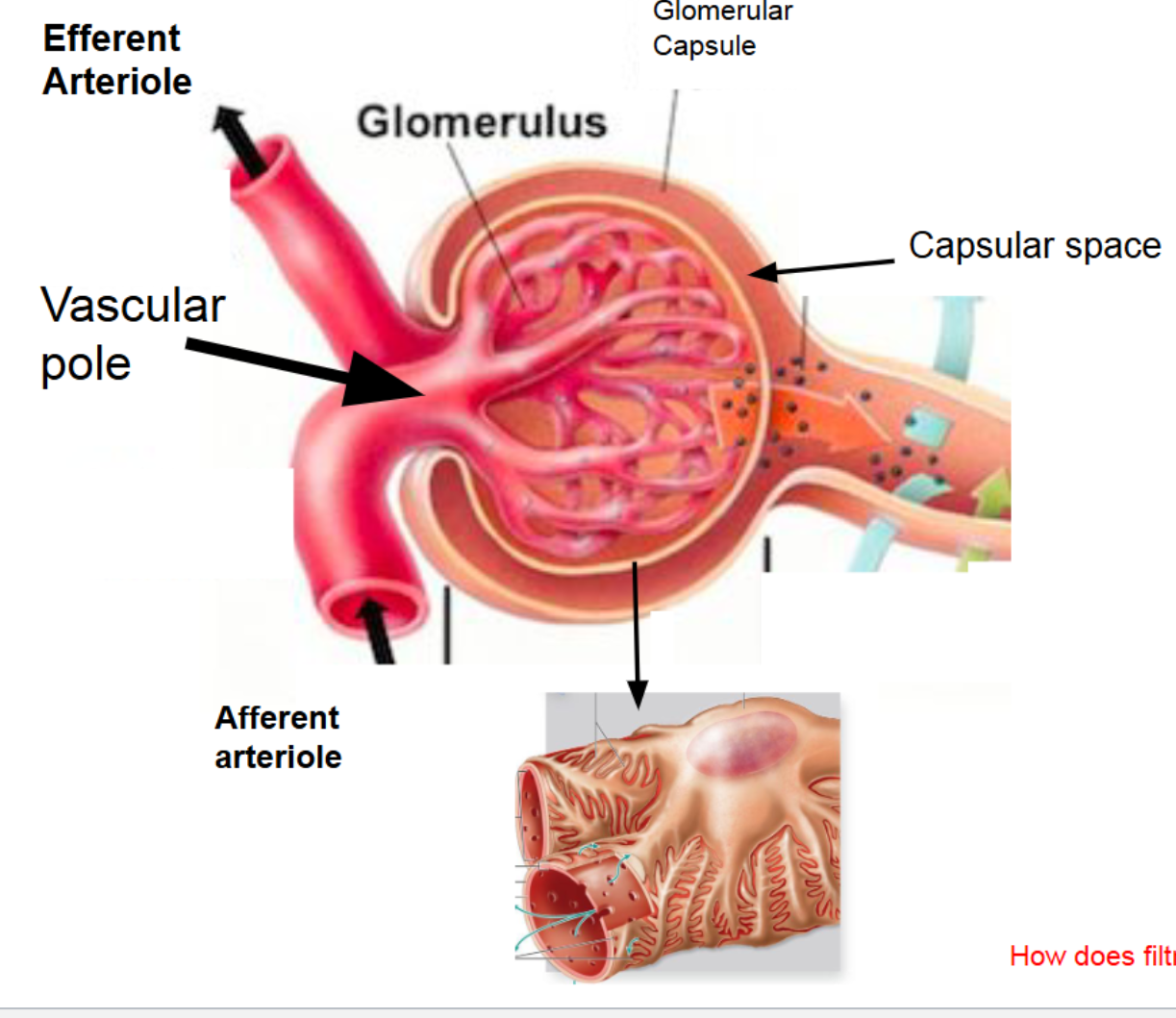
Filtration Process: step 1
Blood enters the glomerulus from the
afferent arteriole
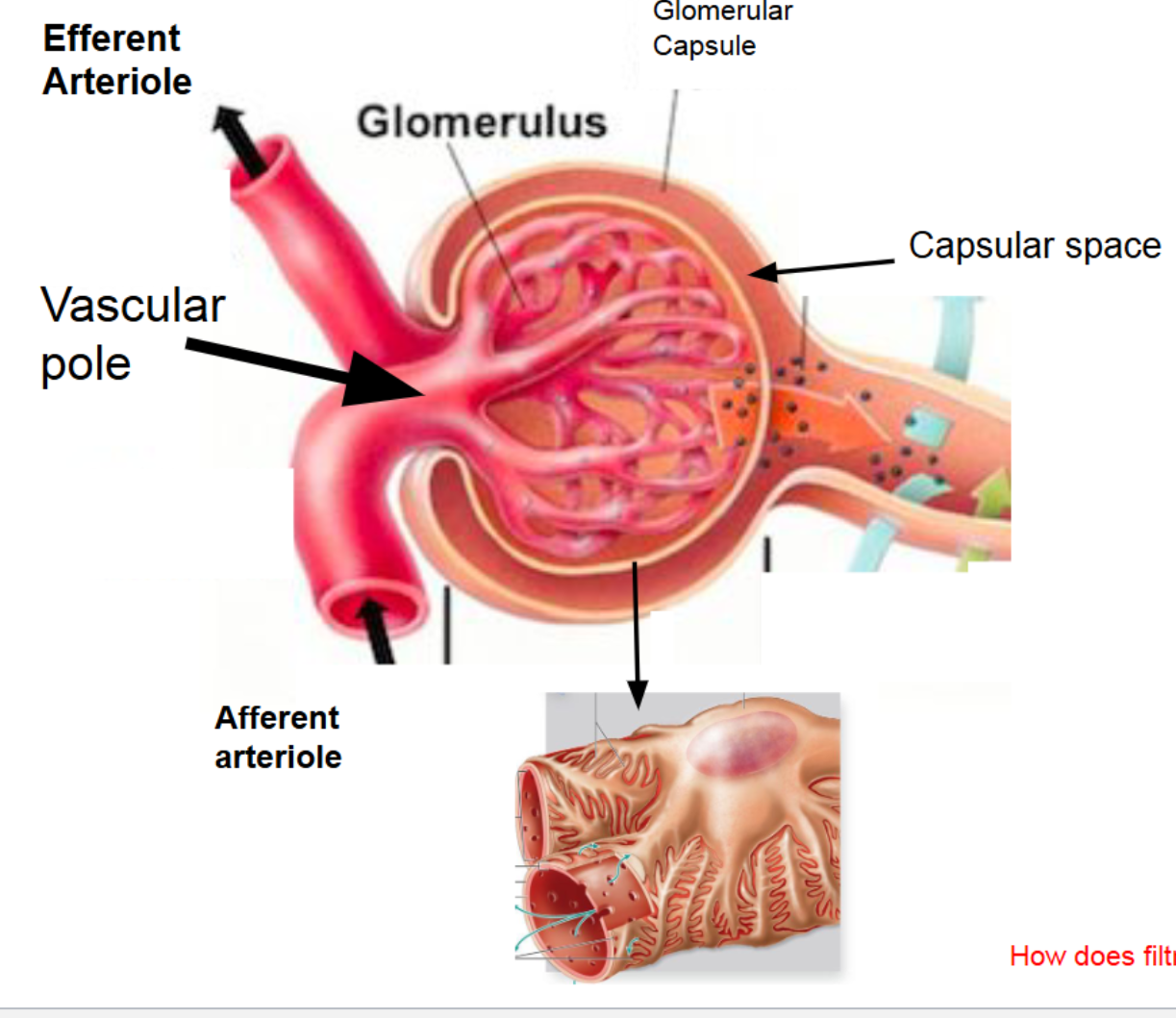
Filtration Process: step 2
High pressure forces blood against the
filtration membrane
Filtrate must be
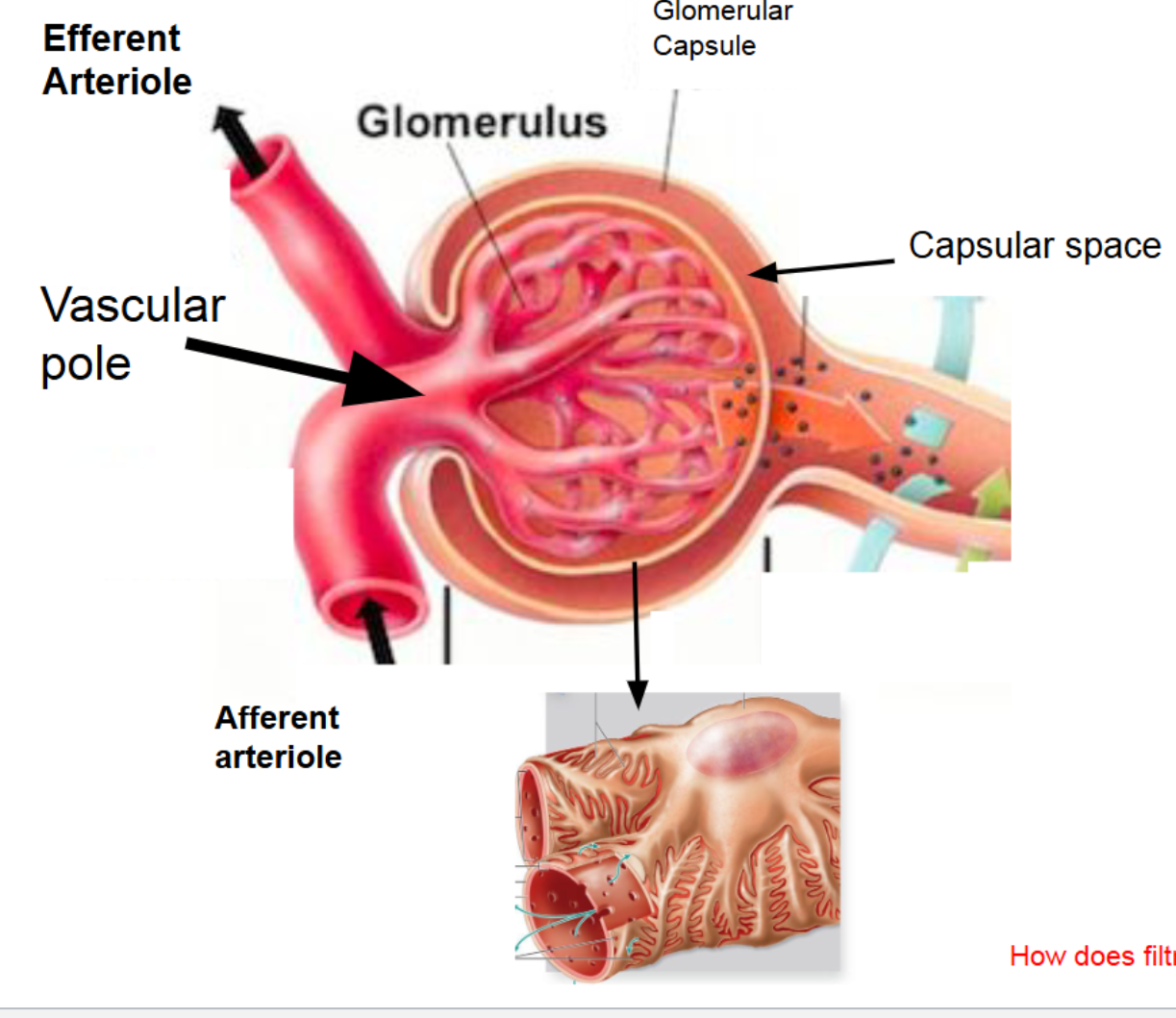
Filtration Process: step 3
Filtration membrane allows the
passage of smaller solutes into the
capsular space
PCT Function:
Major reabsorption site
Returns nutrients (glucose, amino acids), ions, water back to blood
Some secretion (H⁺, drugs)
PCT Histology:
Simple cuboidal epithelium
Tall microvilli → increases surface area
“Fuzzy” brush border appearance.
Nephron Loop Structure:
Descending limb → goes into medulla (water)
Ascending limb → goes back to cortex ( Salt)
Nephron Loop Func.
Creates concentration gradient
Reabsorbs water from descending limb
Reabsorbs salts in ascending limb
Important for concentrated urine production
DCT Function:
Fine-tunes filtrate
Secretion (K⁺, H⁺, drugs)
Reabsorption, especially under hormone control
DCT Histology:
Simple cuboidal epithelium
Sparse microvilli (clear lumen)
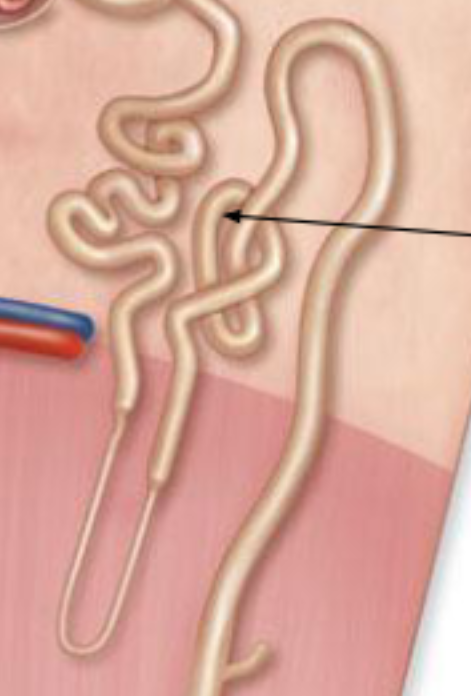
Types of Nephrons?
Cortical nephrons
Short loops
Majority of nephrons
Used during normal conditions
Juxtamedullary nephrons
Long loops deep into medulla
Important in concentrated urine production
Cortical nephrons
Short loops
Majority of nephrons
Used during normal conditions
Juxtamedullary nephrons
Long loops deep into medulla
Important for producing concentrated urine.
Capillary Beds
Two capillary networks:
1. Peritubular capillaries
Surround PCT + DCT
Involved in reabsorption + secretion
2. Vasa recta
Surround loop of Henle
Maintain concentration gradient
Prevent “washout” of medulla
1. Peritubular capillaries
Surround PCT + DCT
Involved in reabsorption + secretion
2. Vasa recta
Surround loop of Henle
Maintain concentration gradient
Prevent “washout” of medulla
Collecting ducts & tubules respond to:
ADH → water reabsorption
Aldosterone → sodium reabsorption
Function:
Determines final urine concentration.
Flow of Filtrate
Glomerulus
PCT
Loop of Henle
DCT
Collecting duct
→ Renal papilla
→ Minor calyx
→ Major calyx
→ Renal pelvis
→ Ureter
→ Bladder
→ Urethra
→ Outside bod
Ureters Function:
Carry urine from kidneys to bladder (carry
urine into pelvic cavity to
empty into urinary bladder)Enter bladder posterolaterally
Type:
Fibromuscular tubes
Layers of Ureter
Three tunics:
Mucosa (with transitional epithelium)
Muscularis (smooth muscle for peristalsis)
Adventitia (outer connective tissue)
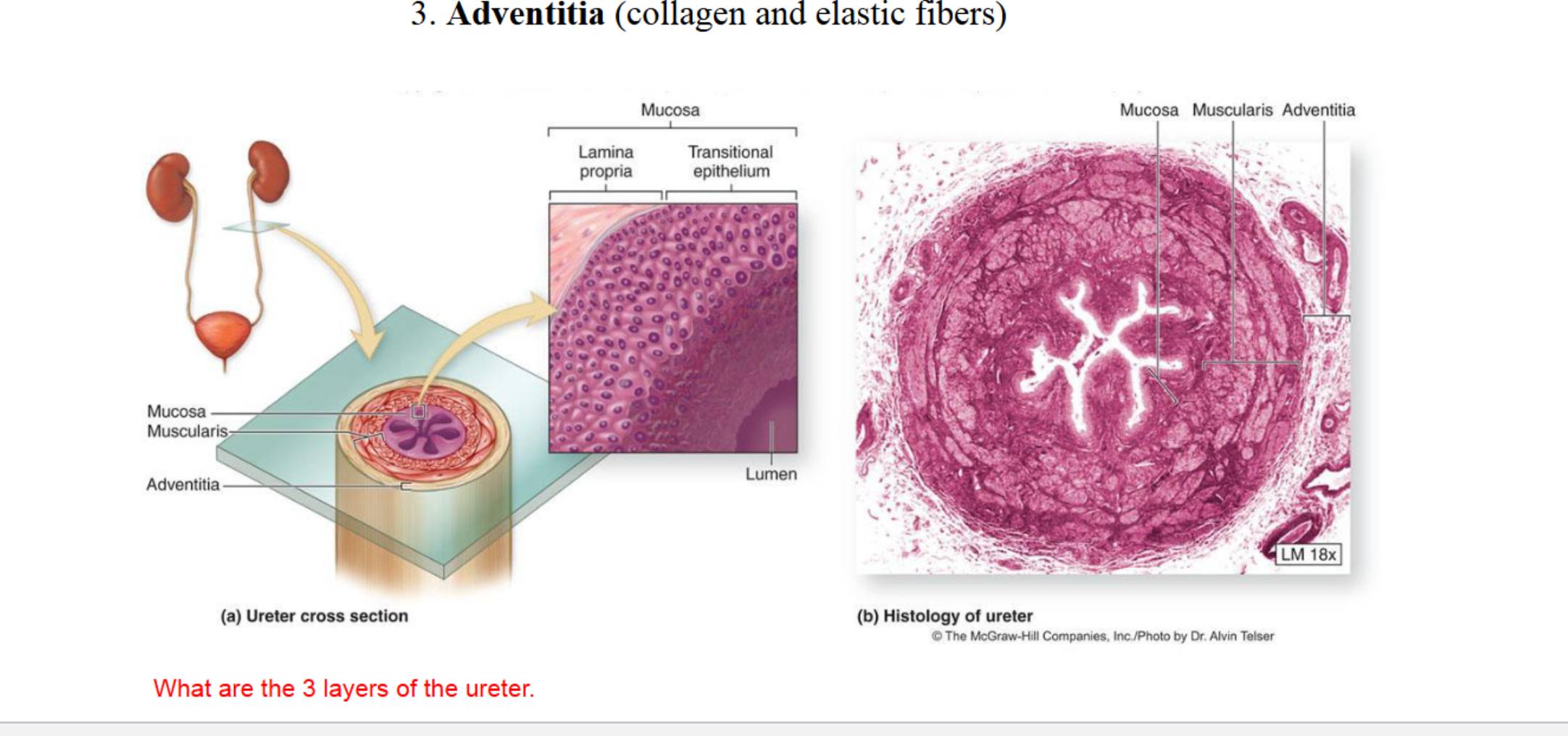
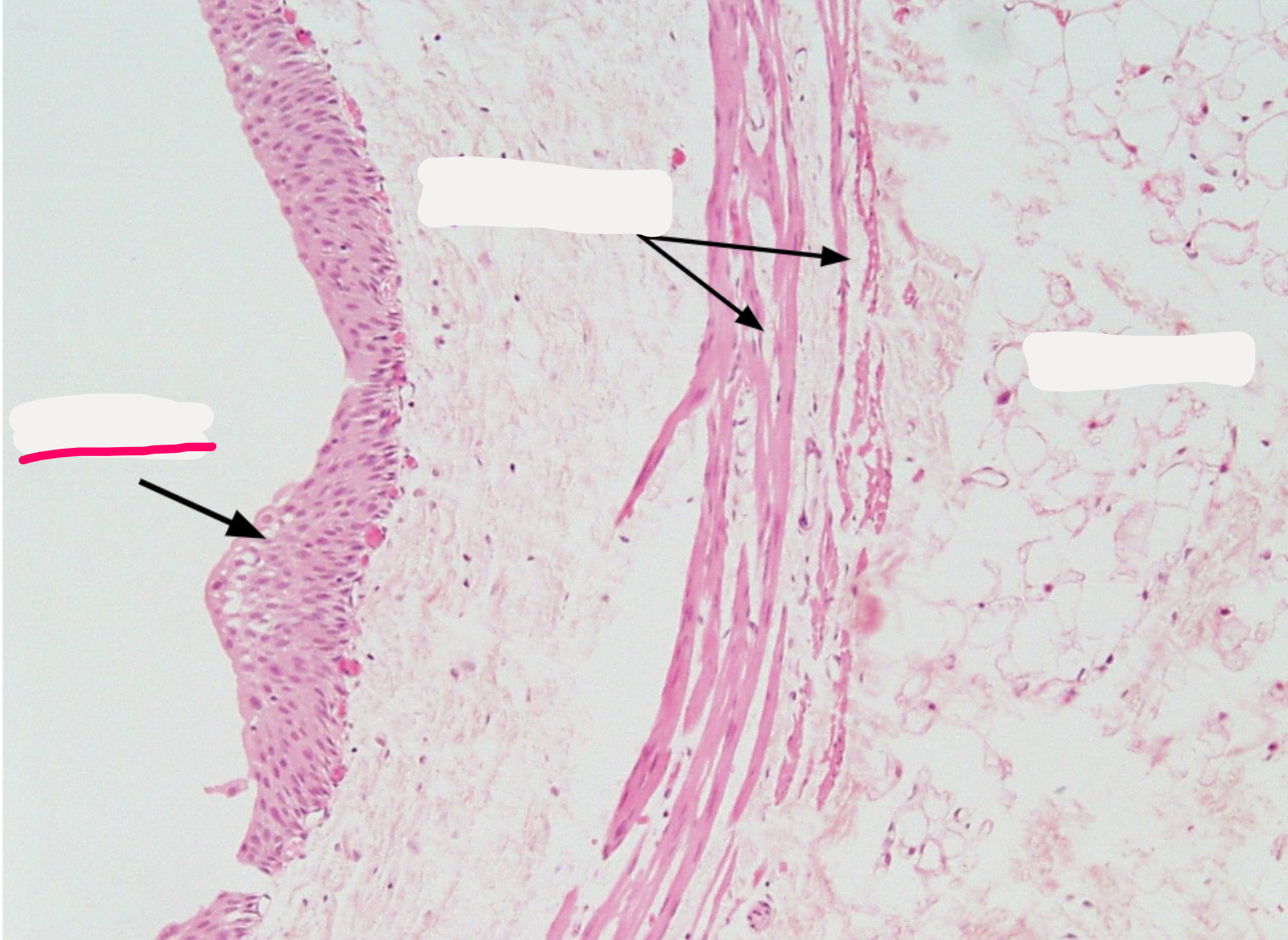
Mucosa
(with transitional epithelium)
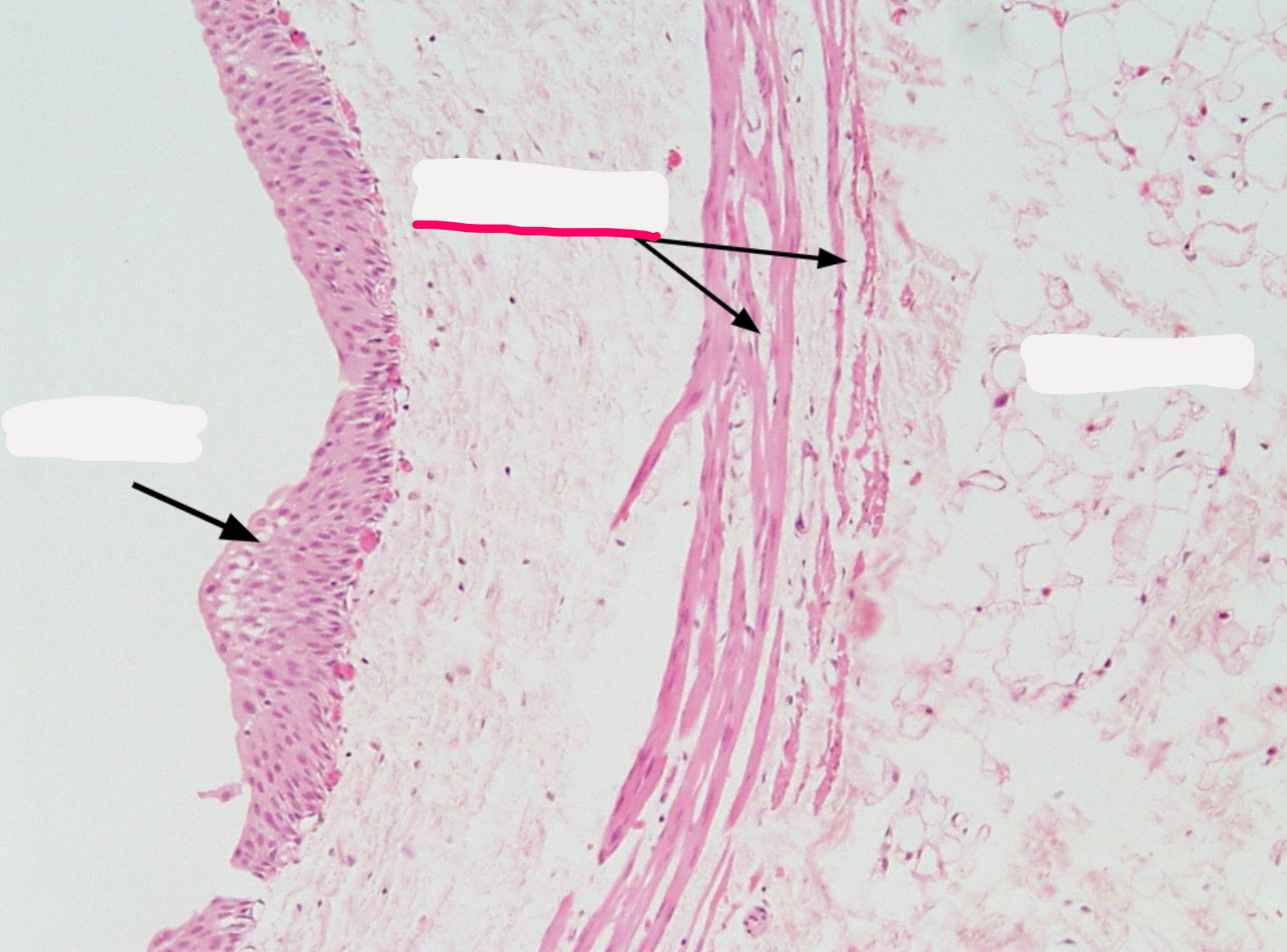
Muscularis
(smooth muscle for peristalsis)
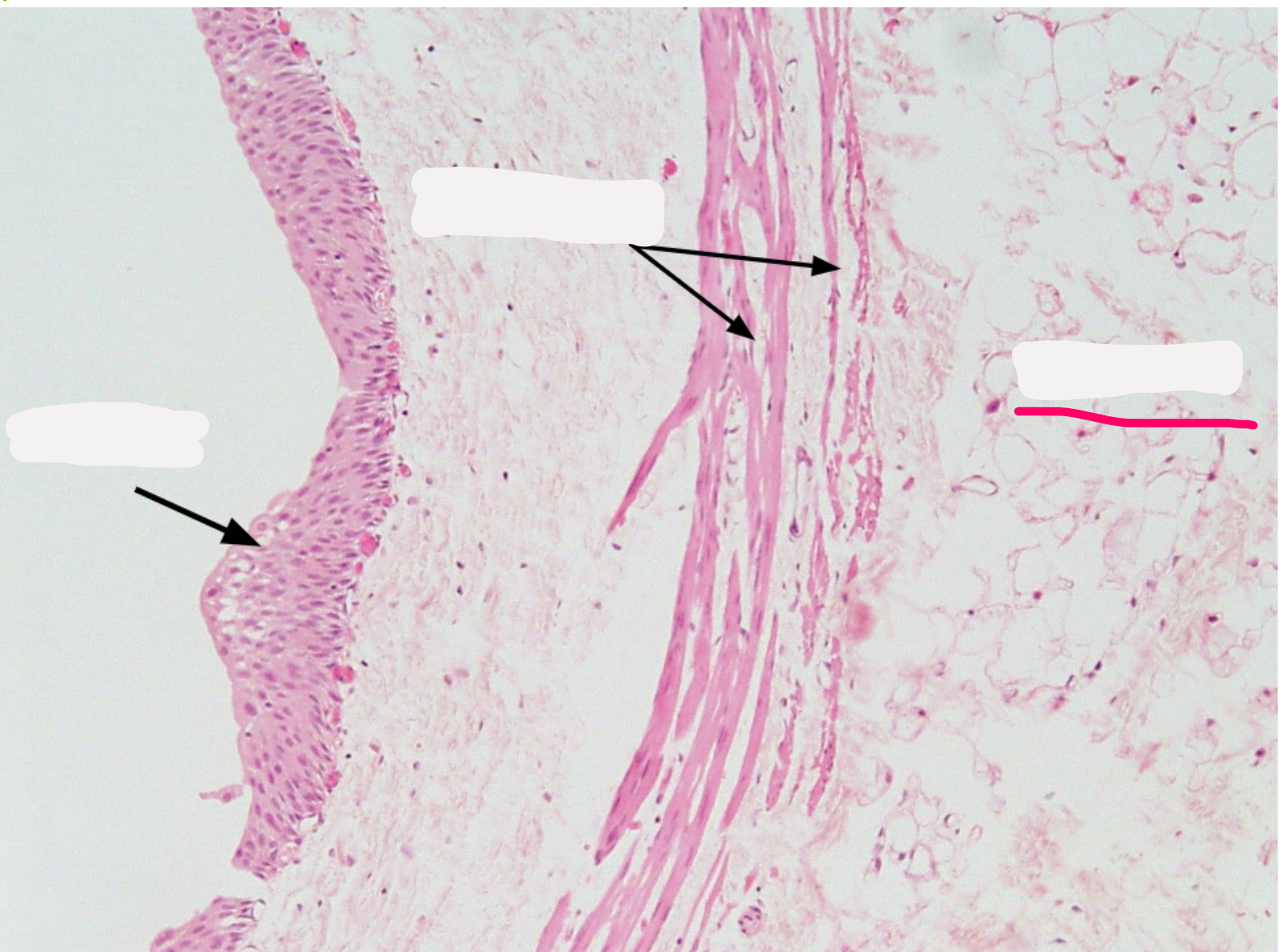
Adventitia
(outer connective tissue)
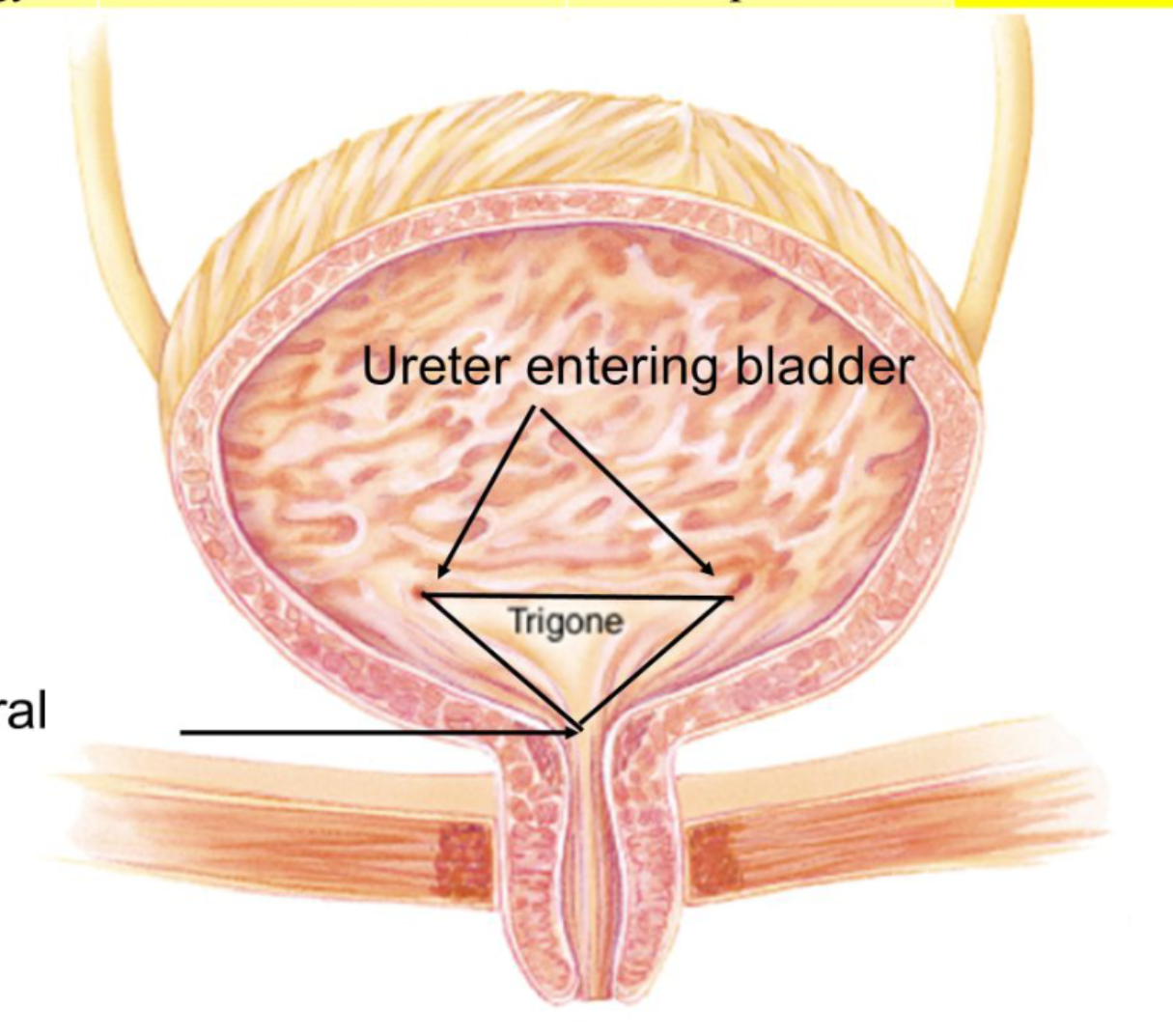
One-Way Valve at Bladder Entry
Ureter enters bladder obliquely
Creates a passive one-way flap
Prevents urine from traveling backward into ureters
(Prevents reflux → kidney damage)
Bladder Wall
Layers include:
Transitional epithelium (can stretch)
Thick smooth muscle (= detrusor muscle)
Adventitia
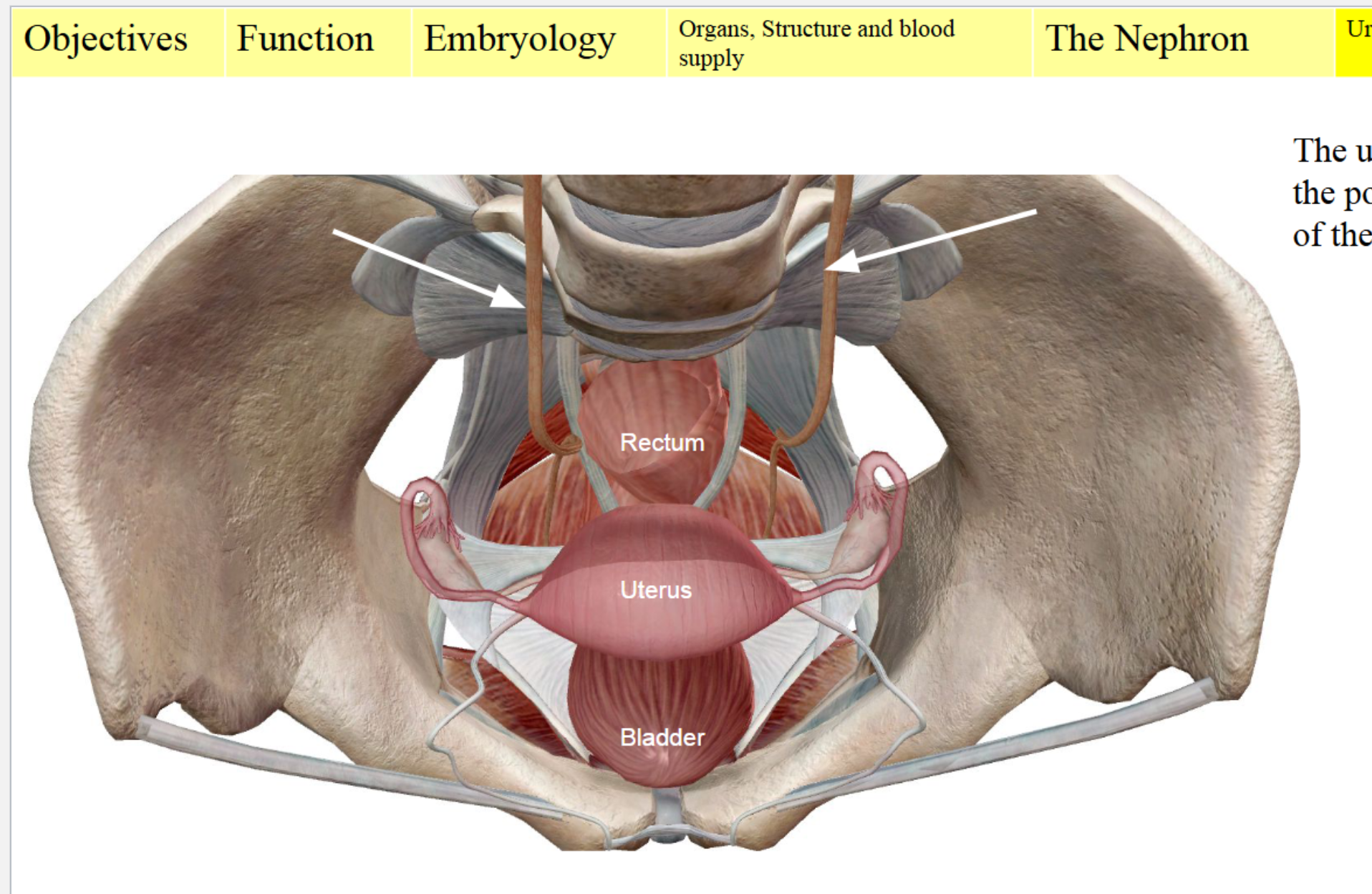
Anatomy of Bladder Position
Ureter enters posterior-lateral wall
Bladder sits anterior to uterus (female)
Urethra exits inferiorly
Each ureter approaches the bladder from behind (posterior side).
They enter the bladder at an angle on the upper side of the bladder wall.
Why this angle matters
This angled insertion forms a natural flap valve:
When the bladder fills with urine, the expanding wall compresses the ureter opening,
Preventing urine from flowing backwards into the ureter (vesicoureteral reflux).
If the angle is too shallow (common in infants), reflux happens → ↑ risk of kidney infections.
Trigone (MUST KNOW)
A smooth triangular area at the base of the bladder
Corners = 2 ureteric openings + urethral opening
Does NOT stretch like the rest of the bladder
Sensitive to stretch → signals “time to pee”
Detects bladder fullness
Common site of UTIs