A&P of Speech (SLHS 3400) -- Exam 2
1/143
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
144 Terms
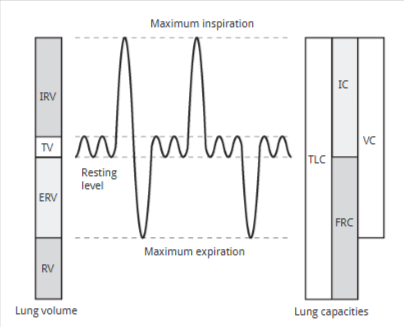
Volume (L)
how much air that an individual inhales or exhales
Tidal volume (TV)
the volume of air that we move in and out of our lungs during resting breathing or during speech activities; ~0.5 L, but will be more for yelling/singing
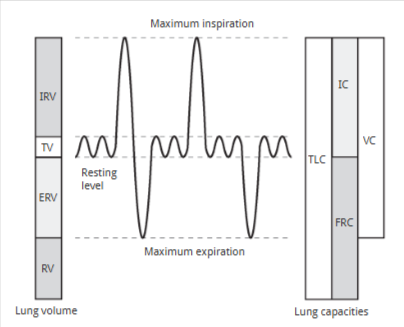
Inspiratory reserve volume (IRV)
the maximum volume of air that we can voluntarily inhale above tidal volume
~ 3 L
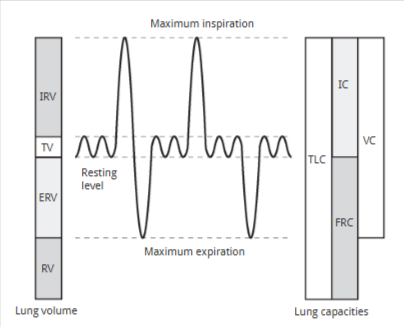
Expiratory reserve volume (ERV)
the amount of air that we can voluntarily expel from our lungs
~ 1.1 L
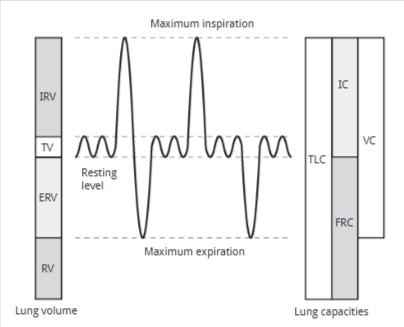
Residual volume (RV)
the volume of air that is always present in our lung tissue (unusable, does not leave until we die)
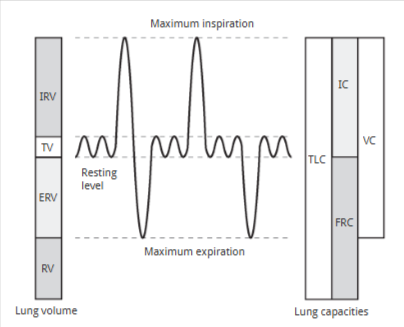
Vital capacity (VC)
Tidal Volume (TV) + Inspiratory Reserve Volume (IRV) + Expiratory Reserve Volume (ERV)
~ 4.5 L of air
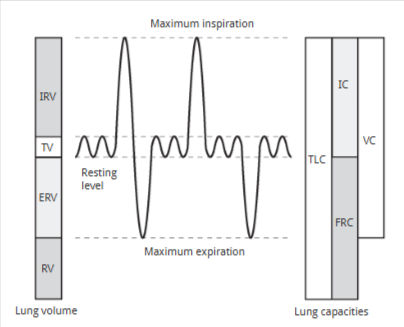
Inspiratory capacity (IC)
Tidal Volume (TV) + Inspiratory Reserve Volume (IRV)
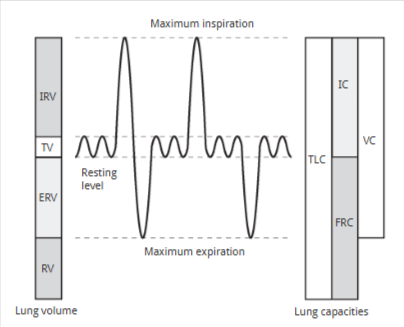
functional reserve capacity (FRC)
Residual Volume (RV) + Expiratory Reserve Volume (ERV)
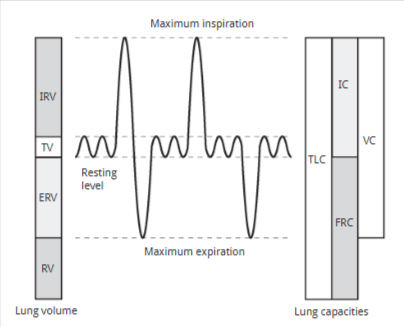
total lung capacity (TLC)
sum of everything
~ 6 L of air
Pulmonary ventilation (VE)
measure of the rate at which we move air in and out of the lung
calculated in minutes
= Tidal volume (TV) × Breathing frequency
Ex) Average: 0.5 L × 12 breaths per min = 6 L per minute
During Rest Breathing, we inhale and exhale approx. ______ liter(s) of air
½
Pressure
used to indicate how the combo of muscle forces and air volumes can be used to produce speech at a target loudness level or for production of a cough that is sufficient to clear the airway
Equation for Pressure
Force/Area
Pressure exerted by a gas results from…
the collision of air molecules with the walls of the lungs
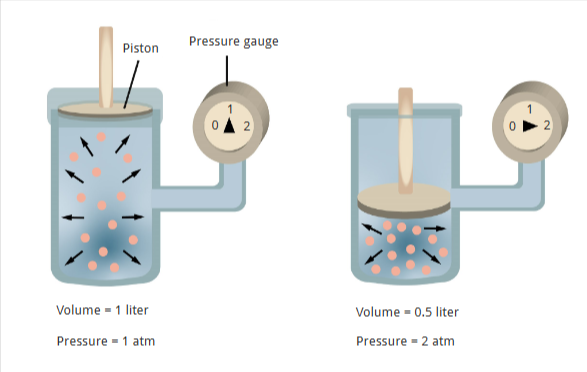
The greater the number of collisions…
the higher the pressure
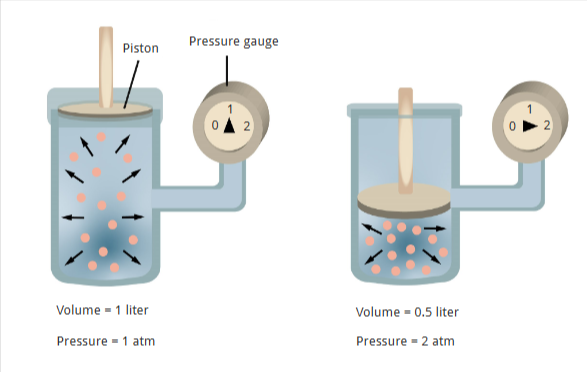
The fewer the number of collisions…
the lower the pressure
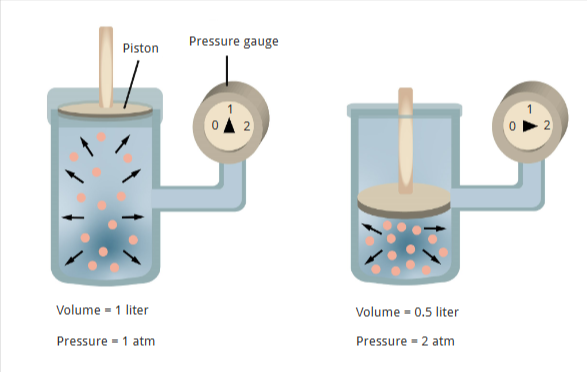
Boyle’s Law
decrease volume of a gas → pressure increases
increase volume → pressure decreases
Pressure = 1/Volume
Atm
average air pressure at sea level on earth
pulmonary ventilation (breathing) depends on …
periodic pressure changes in the lung
Air flows from an area of ________ to _______
higher pressure to lower pressure
During inspiration, pressure in the lungs becomes _____ than the pressure in the atmosphere
lower
(We are expanding our lungs, increasing the size of the container.)
During expiration pressure in the lungs is ______ than the pressure in the atmosphere.
higher
(Our lungs deflate, decreasing the size of the container.)
High temp = ____ pressure
low
Cold temp = ____ pressure
high
Inspiration begins when…
the diaphragm contracts and enlarges the thoracic cage (makes bigger space, lowering pressure)
air moves from high pressure in atmosphere to low pressure in the lungs
During expiration…
The diaphragm relaxes and the elastic tissues in the lung recoils
As the lungs recoil, the air is compressed and the alveolar pressure rises above the atmospheric pressure
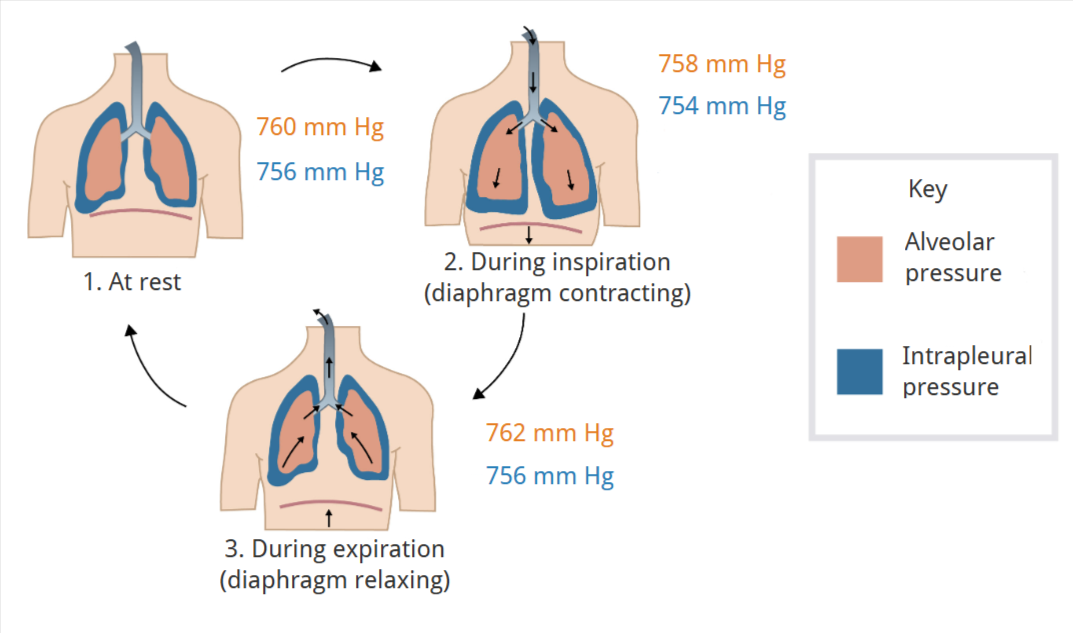
Alveolar Pressure vs Intrapleural pressure (Picture)
Alveolar pressure = lung pressure = intrapulmonary pressure
Intrapleural pressure is DIFFERENT
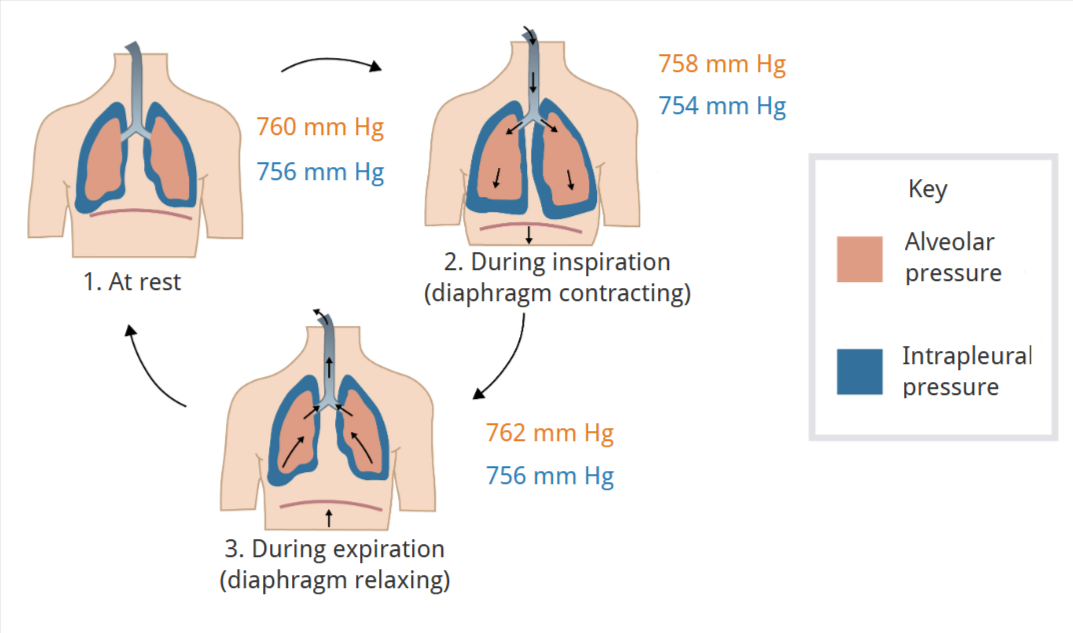
What is our resting state atmosphere (lung) pressure?
760 mm HG
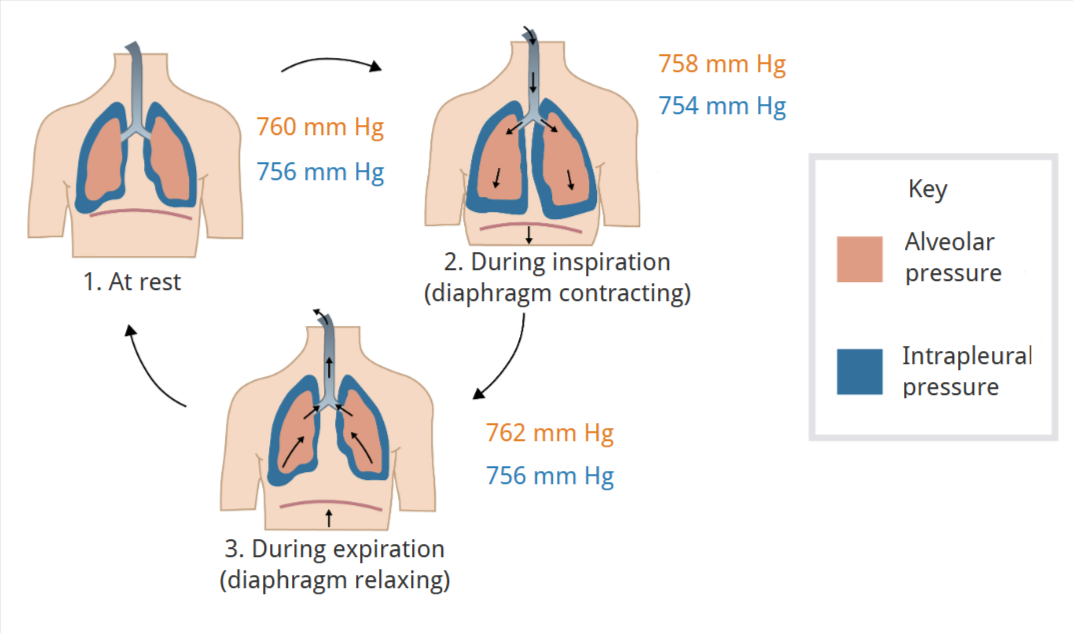
During inspiration, the resting state atmosphere pressure (760mm) becomes ______.
lower
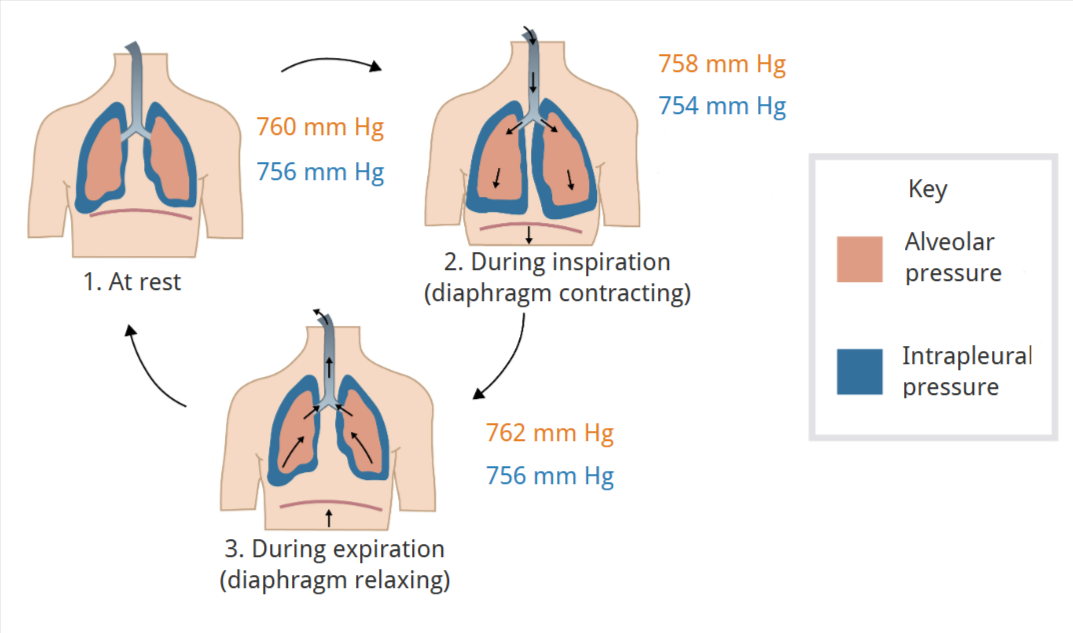
During expiration, the resting state atmosphere pressure (760mm) becomes ______.
higher
Lung Compliance
a measure of the ease with which the lungs can be inflated
Lung Compliance Equation
Change in lung volume / Change in pressure
(Compliance = dV / dP)
As lung compliance increases, the elastic recoil of the lungs _______.
decreases
if compliance gets too high, what is necessary to produce adequate pressures for speech?
forced exhalation
As lung compliance decreases…
elastic recoil of lungs increases
vital capacity of lings reduces
If compliance gets too low, what happens?
frequent breath pauses occur during speech
Emphysema
Lungs expand easily, but may not recoil well → increases compliance
Asbestosis
Thickening or stiffening of lung tissue → decreases the compliance of the lung
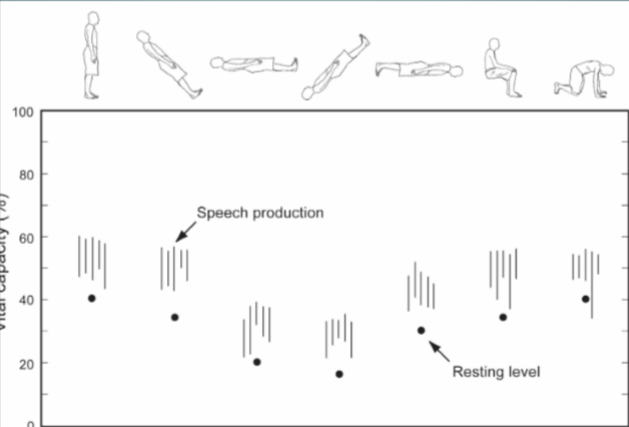
Lying down, you use muscle differently due to gravity because….
you’re relying less on the abdominal wall
Speech Breathing
the specific pattern of respiration that occurs when a person speaks; we modify our expiration and use the respiratory system as "air source” or “air supply”
involves both muscular and non-muscular forces
Speech requires…
requires fairly constant pressure and flow in the upper airway
Output Variables of Speech Breathing (what impacts speech breathing):
Lung Volume
Pressure
Flow of Pressure
Shape of Chest Wall
Lung Volume
Tidal volume for normal breathing ~0.5 L (10- 20%
VC)
Speech : about 60-35 % VC
Pressure
Tidal breathing: alveolar pressures ~1cm H2O
Speech breathing: alveolar pressures ~8-10cm H2O
Flow of Pressure
air flow: areas of higher pressure → areas of lower pressure
Airflow is measured: the rate at which volume change occurs (volume/time)
Airflow during speech: ~100-300 mL/sec
Shape of Chest Wall
shape of the chest wall varies based on shapes of the rib cage, abdominal wall, and diaphragm. The movement of these components impact our speech breathing.
rib cage contact area with the lungs vs. abdomen and diaphragm
rib cage contact: 75%
abdomen and diaphragm contact: 25%
(Less volume of air is moved with the abdomen than with the rib cage)
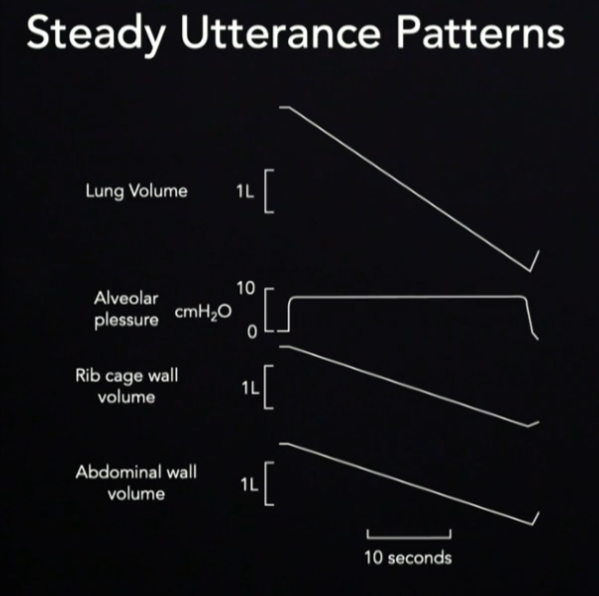
Steady Utterance Patterns
Lung Volume: decreases as we speak/exhale
Alveolar Pressure: remains steady as we speak/exhale and drops when we stop
Rib Cage/Abdominal wall volume: decrease as we speak/exhale
Inspirations are ____, expirations are ______.
faster
slower/longer
Alveolar pressure is _____ during inspiration, and ______ during expiration.
negative
positive
the volume inspired for conversational loudness is _____ than than inspired for loud speaking.
lower
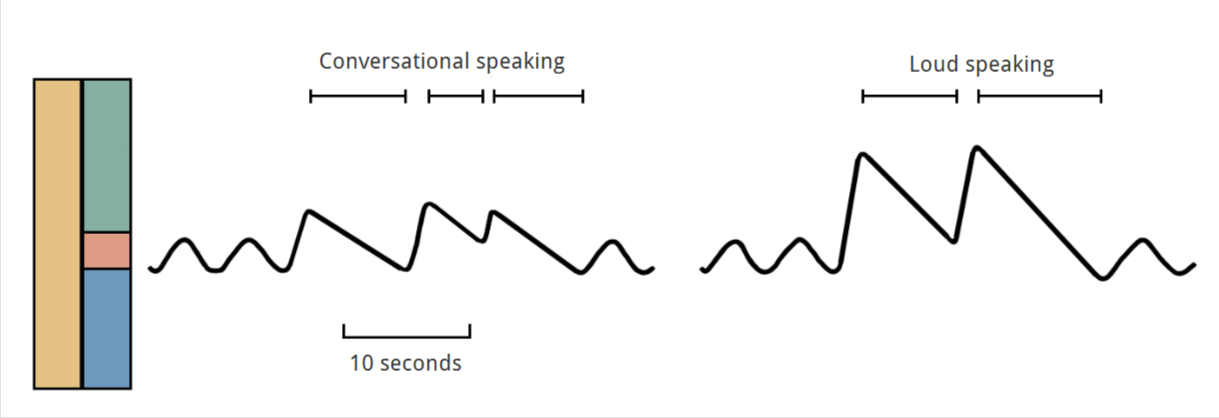
Loud Speaking:
less inspiratory muscle effort required, shorter vital capacity range
greater expiratory muscle effort required, greater vital capacity range
Soft Speaking:
greater inspiratory muscle effort required, greater vital capacity range
less expiratory muscle effort required, less vital capacity range
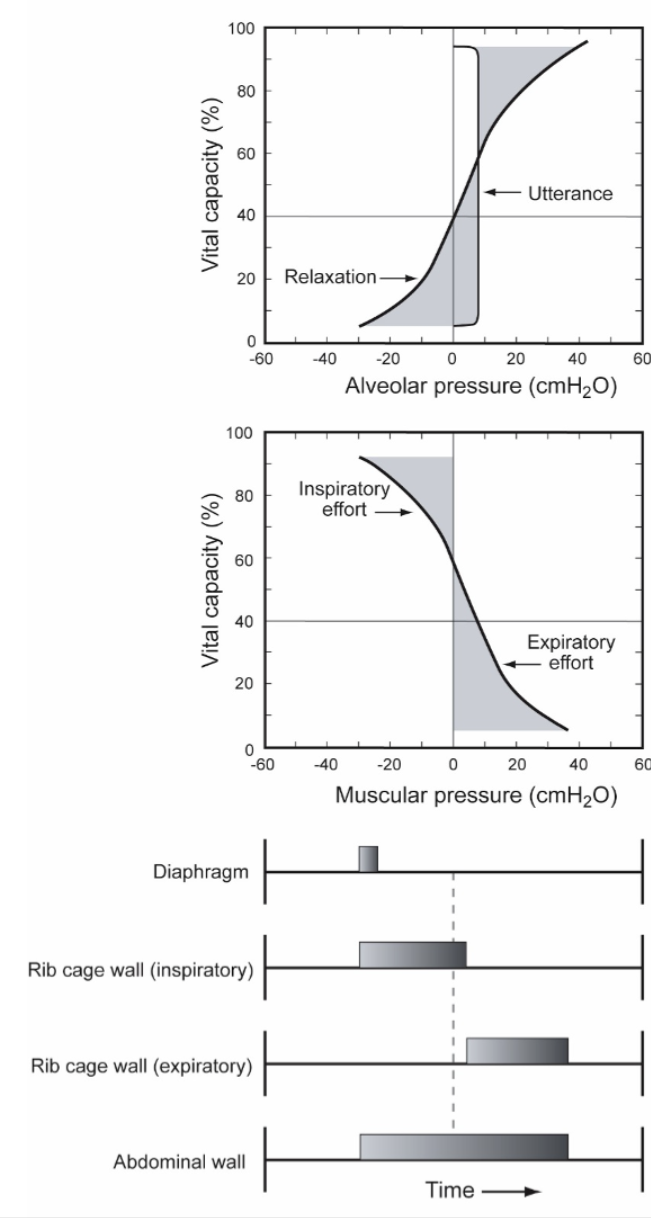
At high lung volume (80-60%VC), speech breathing involves...
passive expiratory pressures and some active inspiratory musculature
recoil pressures are considerable → must use inspiratory muscles to check or "brake" the expiratory recoil
In mid- (60-35%VC) and low- lung volumes (<35%VC), speech breathing involves…
active expiratory pressures.
mid lung volumes: passive recoil is increased with active muscle
low lung volume: we need expiratory muscles to overcome inspiratory recoil
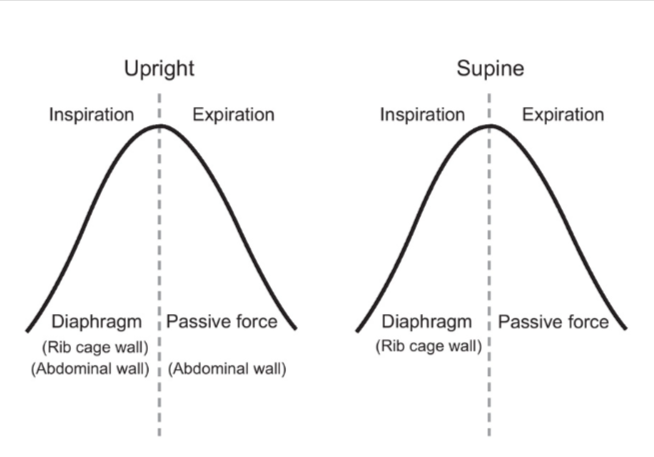
Upright body position
Steady utterance
Relaxation pressure
Alveolar pressure
Muscular pressure
Chest wall patterns
first, inspiratory muscles “brake” the natural recoil of the lungs.
then, expiratory muscles and abdominals take over to keep air pressure steady for the sound
Supine body position
Steady utterance
Relaxation pressure
Alveolar pressure
Muscular pressure
Chest wall patterns
The diaphragm does most of the work at first, while rib and abdominal muscles only join in toward the end to help keep pressure steady.
Heavy Exercise impacts on Chest/Abdominal Wall
requires higher ventilation rates to carry oxygen to working muscles → requires maximal changes to both the rib cage wall and abdominal wall diameter
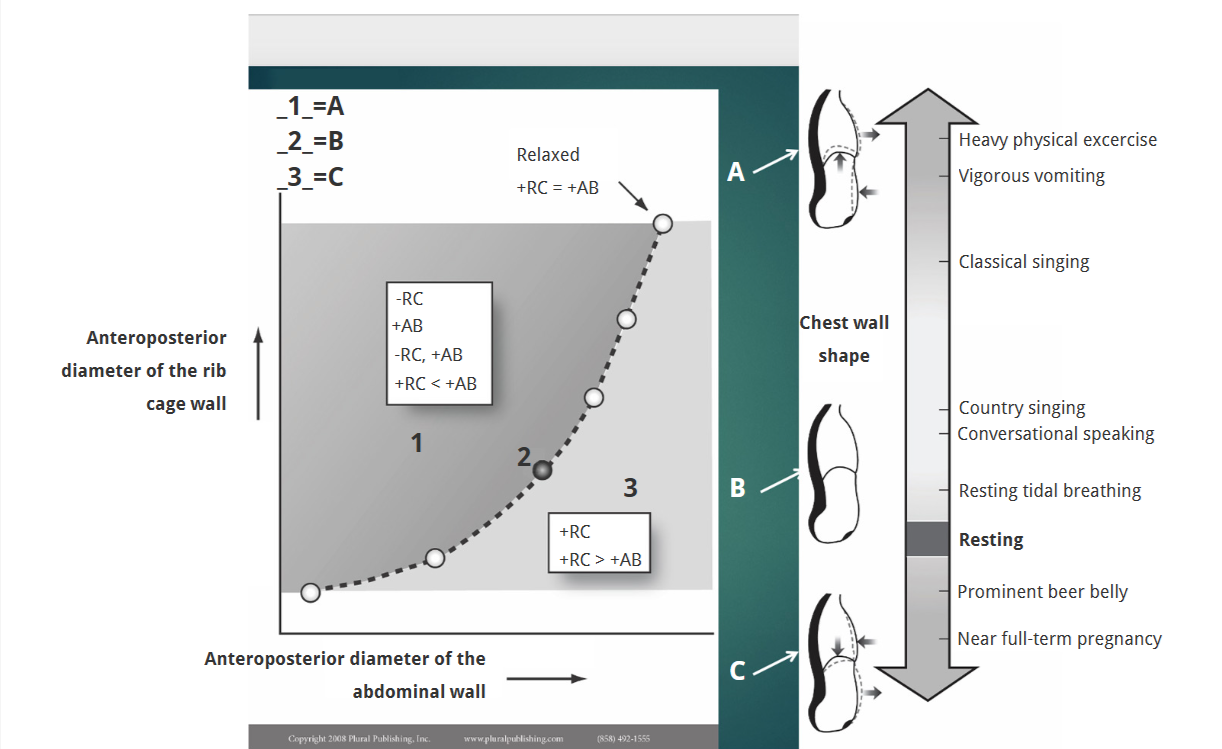
Conversational Speech impacts on Chest/Abdominal Wall
Conversational speech requires relatively equal contributions of chest and abdominal wall displacement.
Endomorph
high relative fatness; abdominal wall has a greater inward position and motion than the other types, likely due to the need for increased tuning of the diaphragm for speech.
Mesomorph
high muscular development; the position of the diaphragm varies between the locations of the endomorph and ectomorph
Ectomorph
high relative linearity and maintains the ideal diaphragm position for speech
By age ___, speech breathing patterns become more like those of an adult.
10
By the time adults enter their ______, breath groups start at larger lung volumes
70s - 80s
males in this age group become more "leaky," while females tend to "blow off" air more frequently.
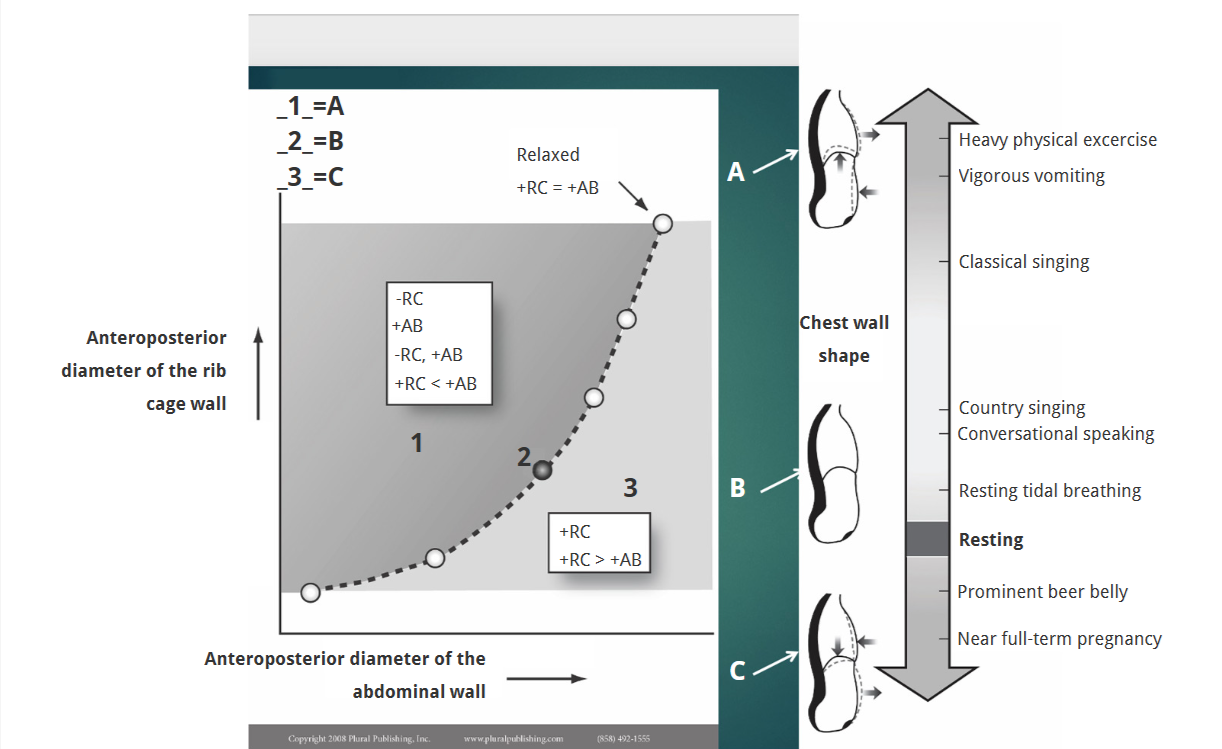
respiratory muscles
are skeletal muscles
contract as a result of the action of motor neurons
under automatic and voluntary control
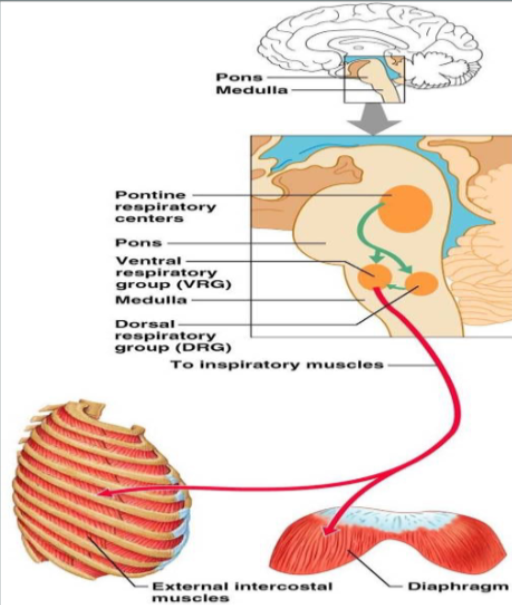
Automatic respiratory muscle control depends on…
groups of neurons in the brainstem
Voluntary respiratory muscle control depends on…
cortical control
Voluntary control of respiration
Descending pathways from the cerebral cortex let us modify breathing to Speak, Sing, Swim/dive, Play wind instruments
rhythmic breathing; “pacemaker-like” activity that turns the inspiratory neurons on and off
Expiratory neurons are silent at rest, but are activated when breathing activity must be increased
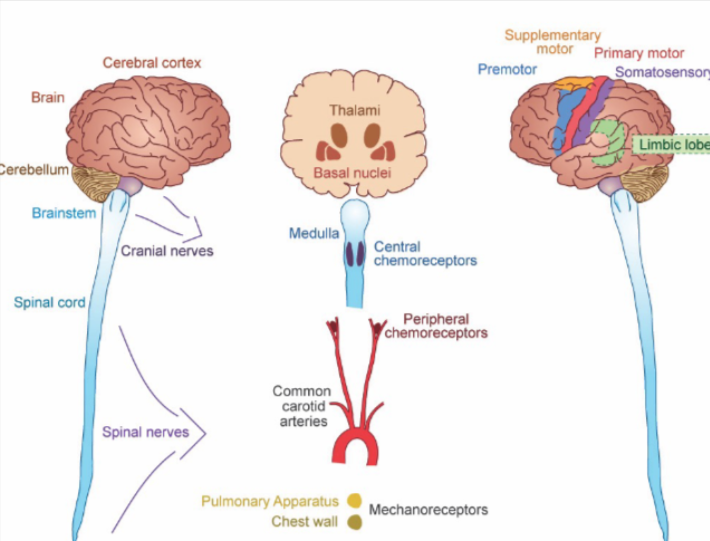
Automatic Control
Dorsal respiratory group (DRG)
Ventral respiratory group (VRG)
→ “pre-motor” neurons - they synapse on and excite motoneurons to respiratory muscles
Dorsal respiratory group (DRG)
contains inspiratory neurons
→ “pre-motor” neurons - they synapse on and excite motoneurons to respiratory muscles
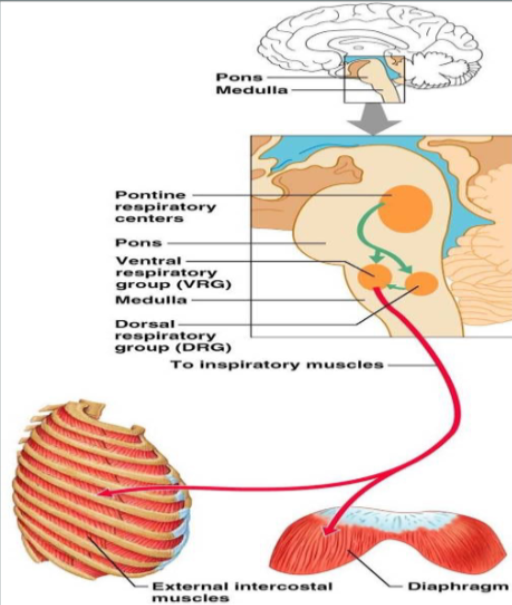
Ventral respiratory group (VRG)
contains expiratory neurons
→ “pre-motor” neurons - they synapse on and excite motoneurons to respiratory muscles
Tools to Measure Breathing
Pressure
Volume
Airflow
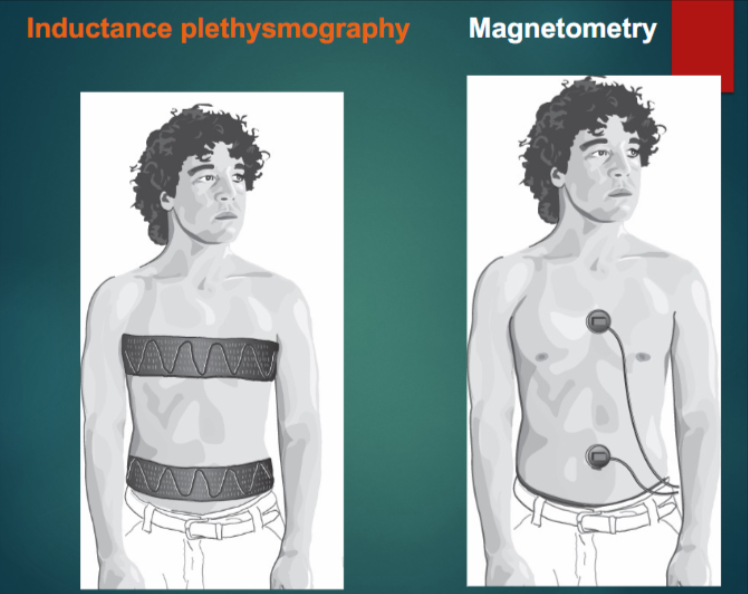
Chest Wall Kinematics
Pressure
(measured in cm H2O)
U- tube water manometer (measures pressure w/ water column height)
Pressure transducer (measures pressure w/ pneumotachograph/face mask device)
Volume
(measured in cc, ml or L)
Wet spirometer (measures volume w/ clip on nose and inhalation and exhalation)
Airflow
(measured in ml/sec or LPS)
Pneumotachograph (measures airflow by using a pressure transducer that detects and quantifies the speed at which the volume of air passes through it)
Chest Wall Kinematics
(Rib cage and abdominal volume changes associated with breathing or speaking)
respiratory induced plethysmography (respitrace) (around torso patient wears a miniature oscillator that connects to coils of wire)
magnetometer
specialized receptors
inform the neurons about the body’s needs for ventilation
Chemoreceptors
Sense O2 , acidity, alkalinity, CO2 in bloodstream (carotid and aortic bodies)
Sense CO2 in Cerebral Spinal Fluid (CSF) via brainstem receptors
Mechanoreceptors
stretch receptors
Progressive Neuromuscular Disorders
affect the nerves that control voluntary muscles and the nerves that communicate sensory information back to the brain; cause progressive deterioration
Ex) ALS
Spinal Muscular Atrophy
disease that damages and kills motor neurons, affecting the movement in your arms, legs, face, chest, throat, and tongue
muscles start to weaken and waste away; can affect speaking, walking, swallowing, and breathing.
Q: What is the formula for pulmonary ventilation (VE)?
VE = Tidal volume x Breathing frequency
Q: During expiration, what happens to alveolar pressure?
It becomes higher than atmospheric pressure
Q: The term "passive force" of the respiratory system means:
The force is developed by recoil of elastic structures which have been deformed from their
rest positions
Q: Dyspnea means:
breathing discomfort or perception of shortness of breath
Q: Chemoreceptors detect changes in:
Oxygen, acidity, alkalinity, and carbon dioxide in the bloodstream
Q: The ectomorph body type is characterized by:
High relative linearity and ideal diaphragm position for speech
Q: What percentage of lung surface area does the rib cage contact?
75%
Q: Vital capacity (VC) is the sum of which three volumes?
TV + IRV + ERV
Q: Which body type is characterized by high relative fatness?
Endomorph
Q: What does conversational speech typically require in terms of chest and abdominal wall displacement?
Relatively equal contribution of chest and abdominal walls
Q: Females have ________ vital capacity than men.
smaller
Q: At low lung volumes (lower than 35% VC), what is primarily required for speech breathing?
Expiratory muscle force
Q: In extended steady utterances (sustained vowels) of normal loudness (with an alveolar pressure target of 5-10 cmH20), why is inspiratory muscular effort required at very high lung volumes?
The passive expiratory forces (recoil pressure) are too strong, inspiratory muscles are used to "check" this excess pressure and maintain a steady airflow
Q: What kind of pressure is responsible for generating alveolar pressure during tidal breathing?
Relaxation pressure (elastic recoil)
Q: Which device measures pressure by the difference in height of water columns?
U-tube water manometer
Q: Respiratory capacity is measured using which of the following?
Spirometer
Q: What is lung compliance defined as?
Change in volume per unit change in pressure
Q: In a supine position, what muscle primarily contributes to inspiration?
Diaphragm
Q: Chest wall movements are measured by:
Respiratory-induced plethysmography or magnetometer