lab final written exam - immunohematology lab (cls 545)
1/57
Earn XP
Description and Tags
only includes the written final objectives and some other miscellaneous info; would recommend studying the other sets ive made for practicals 1 & 2
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
how would you QC antisera for antigen typing?
pos control = 1 drop antisera + 1 drop of panel cell HETEROZYGOUS for antigen
aka (C+c+)
neg control = 1 drop antisera + 1 drop of panel cell NEGATIVE for antigen
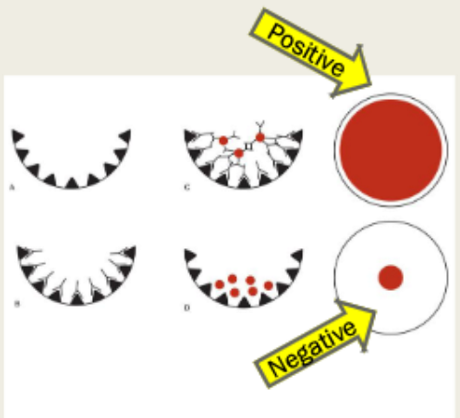
describe the principle of solid phase technology
relies on the formation of antigen-antibody complexes to assess the presence of antibodies in a patient's plasma/serum
patient plasma added to a microwell containing a target antigen for a specific antibody
microwell incubated at 37C
pH buffered isotonic saline is used to wash any unbound serum antibodies
indicator cells (RBCs coated with anti-IgG) added to detect antibodies bound to the microwell from pts plasma/serum & wells centrifuged
**if the antibody is attached to the target antigen during incubation, the indicator cells will form a smooth monolayer of RBCs
**if no antibody is attached to the target antigen, the indicator cells form a tight pellet/button of cells as there is no complex for the indicator cells to attach, and they settle at the bottom of the microwell
explain why intact RBC’s in urine are not indicative of a hemolytic transfusion reaction.
in a HTR, the transfused red blood cells are destroyed, or hemolyzed, by antibodies or other factors ; the damaged RBCs release hemoglobin into the bloodstream, which can lead to hemoglobinuria (hemoglobin in the urine) rather than intact RBCs
explain the purpose of the last wash in an elution. what do we do with the last wash sample that's collected and why?
the last wash is used as a negative control to ensure that all non-specifically bound or unwanted substances have been removed as intended
ABY screen is performed on the last wash—must be negative to validate elution procedure
provide circumstances where an elution might be performed (3)
identify antibodies coating cells of patients with a pos DAT
in conjunction with adsorption when patient has multiple antibodies
to confirm the presence of weakly expressed antigens
massive transfusion protocol (MTP)
Designed to deliver blood in a prompt and standardized fashion
Current massive transfusion guidelines recommend a 1:1:1 ratio of RBCs, plasma, and platelets
Common practice: 6 units RBC, 6 plasma, 1 single donor platelet
MTP aims to avoid the negative effects of excessive crystalloid administration and minimize coagulopathy by administering blood products in a balanced ratio
what types of patients need massive transfusion protocols?
GI bleeds
Aortic aneurysms
OB patients
Trauma patients
GSW
MVC
problems with massive transfusion protocols
Rapid infusion of cold blood can result in hypothermia
Increased risk of cardiac arrhythmias
Hypotension
Decreased cardiac output
Decreased coagulation factor activity
Platelet dysfunction
Reduced citrate metabolism
Can be prevented by pre-warming resuscitation fluids, blood warmers, warm air blankets for patient
why is citrate toxicity a potential risk in massive transfusion protocols?
Citrate anticoagulant used in blood products
Liver may not be able to metabolize as fast as products are transfused
Causes hypocalcemia, hypomagnesemia
Symptoms of hypocalcemia easy to overlook in unstable patients receiving multiple transfusions
Hypotension
Narrow pulse pressures
Tetany
Parestesias
Treat with IV replacement to prevent complicatons (arrhythmia, death)
daratumumab (general)
Monoclonal antibody therapy used to treat multiple myeloma
Anti-CD38, CD38 is present on all human cells but increased on myeloma cells
Goal is to destroy myeloma cells
Issues
"acts" like an antibody and agglutinates CD38 positive cells in-vitro
causes pan-agglutination with everything
dithiothreitol (DTT) treatment of rbcs
Mechanism of DTT
Reducing agent, breaks disulfide bonds
Destroys CD38 antigen (cell surface marker)
Also destroys Kell and other less significant cell antigens
RBC treatment procedure
Select a "custom panel" of cells to treat, ensuring everything can be ruled out
Series of washing steps
Cells good for 5 days post-treatment
transfusion considerations for patients on daratumumab
Reporting results
"Dara present, no other alloantibodies detected"
"DTT-treated cells used for resolution, Kell negative units required for transfusion"
Pathology Review
Will approve incompatible units only if DTT-treated panel results in complete allo-antibody rule outs
blood group genotyping (general)
involves identifying specific genetic markers that determine blood group antigens, offering a precise match for transfusions
significance: allows for broader range of antigens to be matched compared to traditional serology, reducing risks of adverse transfusion reactions
provides highly compatible blood products
challenges: cost, complexity, limited technology
paternal phenotyping and genotyping
done if mother has anti-D and the father is D-positive
A complete Rh phenotype can help determine the father's chance of being homo/heterozygous for D antigen
DNA genotyping method is more sensitive and precise
Helpful in determining further testing of the mother AND in counseling the mother about potential plans for HDFN prevention/treatment
fetal DNA testing
done if the mother has anti-D and father is likely heterozygous for the D antigen
can determine whether the fetus has the gene for the D antigen
During the 2nd trimester, maternal plasma can be tested for fetal DNA to determine genotype
Genes coding for c, e, C, E, K, Fya, Fyb, Jka, Jkb, M, and others
postpartum testing when mother is Rh(-) and fetus Rh(+)
Maternal sample is further evaluated to detect a feto-maternal hemorrhage (FMH)
FMH screen will detect hemorrhages in excess of 30 mL of whole blood
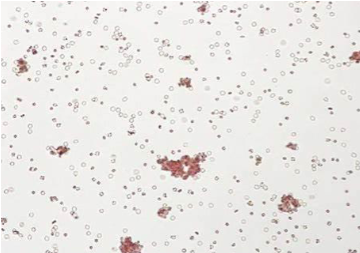
what does it mean when the FMH screen is positive?
indicates that hemorrhage is more than 30mL of whole blood
approx quantification is then performed using Kleihauer-Betke test
Flow cytometry and enzyme-linked antiglobulin testing can also be used for quantification; however, less common
why do we need to quantify a positive FMH screen?
to determine the amount of RhIg needed to prevent the mother from forming an immune response due to the hemorrhage
serologic testing of newborn infant
ABO and Rh typing
Direct Antiglobulin Test
Most important serologic test for diagnosing HDFN
Positive indicates IgG antibody is coating the infant's RBCs
Note: positive result can be found without clinical evidence of hemolysis (mother received RhIG)
Elution--reflex testing
Ordered when the cause of HDFN (or the positive DAT) is unknown
what test is performed to determine how many vials of rhogam should be administered to an Rh(-) mother delivering an Rh(+) baby?
Kleihauer-Betke test
note: regardless of the results of the fetal screen, an Rh-negative mother delivering an Rh pos infant will receive 1 dose of Rh immune globulin as long as she has not developed anti-D
also: the fetalscreen test does NOT indicate how much rhogam should be give
it only determines the presence or absence of fetomaternal hemorrhage
transfusion reaction (general)
Any adverse event that occurs during or after the transfusion of any blood component including fever, pain, anxiety, SOB etc.
Statistically, the greatest risk of morbidity and mortality from transfusion is from noninfectious complications such as TRALI, TACO and HTRs
most common type of transfusion reaction is febrile, nonhemolytic reactions
cytokines in the product or antibody to donor WBCs causes the reaction
what to do when transfusion reactions happen and the patient is symptomatic?
STOP THE TRANSFUSION!
Alert the blood bank and the ordering provider & then request:
The patient’s symptoms
Documentation of the patient’s vitals before and after transfusion
The component itself, even if the bag is empty
Copy of the unit tag
Pink top EDTA tube
Urine for urinalysis
Depending on the symptoms, we may request additional testing and/or contact the pathologist on-call.
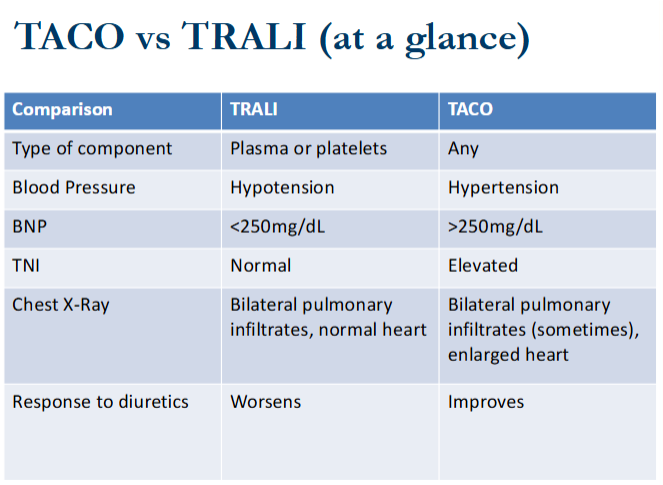
transfusion associated circulatory overload (TACO) vs transfusion related acute lung injury TRALI
TACO = blood is transfused too quick
TRALI = WBC antibodies in donor/WBC activating agents in tranfusion components
BNP: high in TACO; low in TRALI
Bilateral infiltrates on chest film in TRALI
TACO only one responds to diuretic treatment
BP increases in TACO; decreases in TRALI
“Dce” in Fisher-Race correlates to what in Wiener notation?
R0
“DCe” & “DcE” in Fisher-Race correlates to what in Wiener notation?
DCe = R1
DcE = R2
“DCE” & “dCE” in Fisher-Race correlates to what in Wiener notation?
DCE = Rz
dCE = ry
“dce” in Fisher-Race correlates to what in Wiener notation?
dce = r
“dCe” & “dcE” in Fisher-Race correlates to what in Wiener notation?
dCe = r’
dcE = r’’
interpretation of reactions in solid phase
positive: single, smooth monolayer present in the microwell
negative: tight button at the bottom of the well
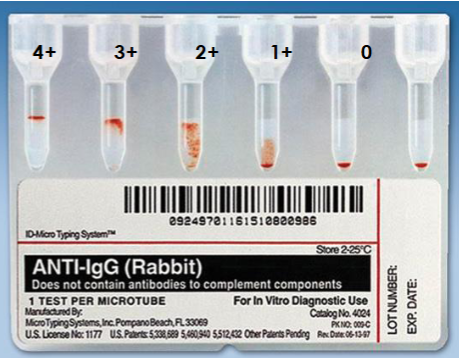
interpretation of reactions in gel testing
4+ = cells remain suspended at top of gel
3+ = most cells suspended at top of gel
2+ = cells dispersed throughout the gel; few agglutinates may be observed in bottom of gel
1+ = cells dispersed in lower portion of gel; unagglutinated cells form pellet in the bottom
negative (0) = complete sedimentation of all red cells at the bottom
mf = band of red cells at top of gel accompanied by a pellet of cells at the bottom
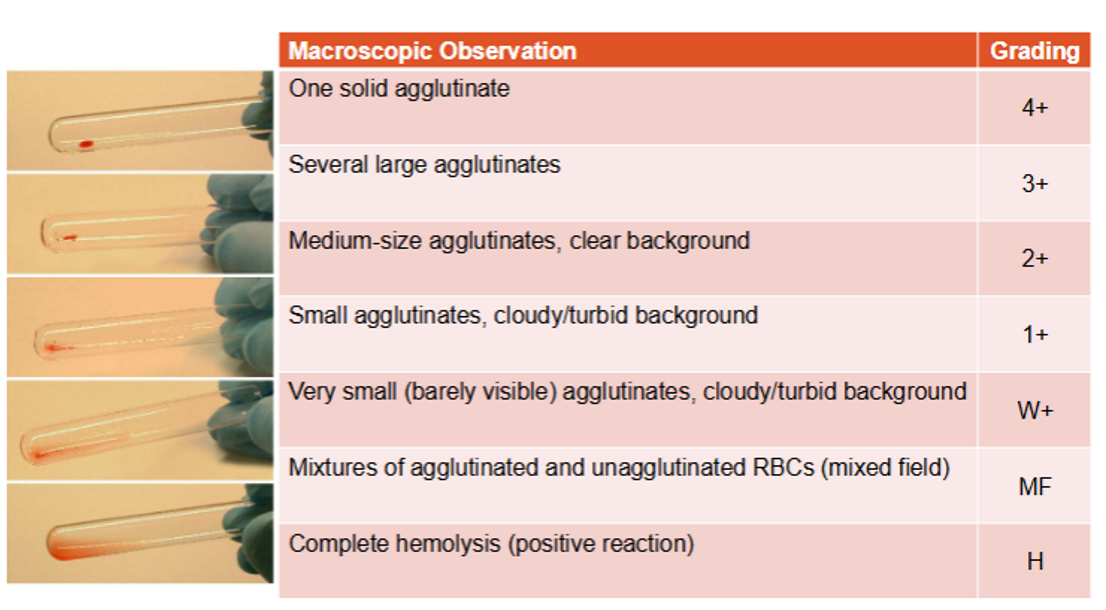
interpretation of reactions in tube testing
negative (0): cells fail to show visible agglutination after button dislodges
1+: hazy red background with many small agglutinates available
2+: clear bkg w medium sized agglutinates
3: clear bkg w fewer than 5 larger clumps
4+: one large clump or one large and one smaller clump w clear bkg (no free cells)
why do mixed fields occur and how to report them?
presence of two distinct populations of RBCs are present due to recent transfusion or BMT
can also indicate chimerism/mosaicism
report: “No Type Determined (NTD), Give O RBCs”
donor recon for A, B, or AB pos units requires what reaction tubes?
anti-A + anti-B
donor recon for A, B, or AB NEG units requires what reaction tubes?
anti-A, anti-B, anti-D
donor recon for O pos units requires what reaction tubes?
anti-A,B
donor recon for O NEG units requires what reaction tubes?
anti-A,B + anti-D
when is it appropriate to perform weak D testing?
weak D testing done in the following patients:
BMT patients who are Rh neg @ IS
check for mixed fields !
cord bloods or newborns <4 mo
pregnant mothers w/o a history
when is it appropriate to perform DAT testing?
on cord bloods (IgG & saline only!)
on patients with suspected HTRs
investigate antibody or complement mediated hemolytic anemia (HDFN, HTR, AIHA, DIHA)
when is it appropriate to perform an elution procedure?
elutions are performed when DAT testing is positive—will ID the antibody coating the cells of a DAT pos pt
can confirm the presence of weakly expresed antigens on RBCs
combined w adsorption to remove specific antibodies from sample with multiple antibodies
when is it appropriate to perform a saline replacement?
done to resolve discrepancies in the back type
done in mutiple myeloma patients
differentiating between true agglutination and rouleaux
why is weak D testing almost always invalid when the DAT is positive for IgG?
if the DAT is positive, it indicates that the cells were already coated with an ABY that wasn’t the anti-D that was added to detect the D antigen
invalidates all IAT testing procedures bc IAT involves the addition of anti-IgG in vitro, so if the cells you are testing are already covered with IgG, then you can’t be sure that the anti-IgG you add in the tube is actually binding and agglutinating the antigen/ABY of interest
explain the theory behind weak D testing
utilizes the IAT technique/principle:
addition of antibody will attach onto an antibody/antigen of interest in optimal conditions if present (IN VIVO sensitization)
addition of monospecific AHG (anti-IgG) will agglutinate the antibody added in the previous step if it managed to bind to its specific target
monospecific AHG will crosslink antibody coated cells to form visible agglutination
explain the theory behind DAT testing
demonstrates IN VIVO attachment (sensitization) of rbcs by antibody/complement using a modified indrect antiglobulin procedure
if IgG or complement is bound to a pt’s RBCs, the AHG (anti-IgG) will crosslink the sensitized cells to create a visible agglutination reaction
explain the theory behind elutions/elution procedure
removes antibody from RBC by exposure to low pH
cells to be eluted first thoroughly washed in special wash solution to remove all unbound antibodies
cells suspended in a low pH glycine solution to dissociate bound antibody and then centrifuged
supernatant (eluate) containing dissociated antibodies removed and neutralized with buffering solution to a appropriate pH
eluate tested against selected cell suspensions such as Panel Cells, Screening Cells or A 1 , A 2 , & B cells using modified IAT technique
explain the theory behind saline replacements
patients’ samples with abnormal serum protein concentrations, reversed albumin-to-globulin ratio, or plasma expanders can aggregate reagent red blood cells and can mimic agglutination
saline replacement frees cells in the case of true rouleaux formation
true agglutination: RBCs remain clumped after addition of saline → positive
rouleaux: RBC aggregates disperse into free cells with the addition of saline → negative
differentiate between major vs minor crossmatch
minor: tests recipients RBCs against donor plasma
used with whole blood
not done in transfusion services but common in war
major: tests recipient plasma against donor RBCs
uses IAT; most common
differentiate between a full vs abbreviated crossmatch
full XM: through AHG, done when:
ABY screen is pos
evidence of clinically significant antibodies
abbreviated XM is pos at IS
goal: detect unexpected patient antibodies
ISXM done when:
ABY screen negative
no evidence of clinically significant antibodies
goal: detect ABO incompatibilities
antigen frequencies of ABO types in Caucasians
O = 45%
A = 40%
B = 11%
AB = 4%
antigen frequencies of ABO types in African Americans
O = 49%
A = 27%
B = 19%
AB = 4%
Rh antigen frequencies in Caucasians
D = 85%; no D = 15%
C = 70%
E = 30%
c = 80%
e = 98%
Rh antigen frequencies in African Americans
D = 92%
C = 27%
E = 22%
c = 96%
e = 98%
kell antigen frequencies
K= 9%
k = 99.8%
duffy antigen frequencies
Fya = 66%
Fyb = 80%
antigen frequency of M & N
M= 79%
N = 70%
antigen frequency of S & s
S = 55%
s = 90%
kidd antigen frequencies
Jka = 76%
Jkb = 74%
how to find the compatibility frequency of anti-__?
take the antigen frequency of the antigen and subtract it from 100
ex: compatibility frequency of anti-C = 30%
100-70% = 30%
how to find the frequency of specific antigen pos/neg cells?
multiply the frequencies of the antigen expression and convert to a percentage
ex: frequency of a K neg and C pos cell?
K neg = 91% of the time = 0.91
C pos = 70% of the time = 0.7
0.91 × 0.7 = 0.637 = 64%