Cancer Introduction
1/220
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
221 Terms
Concepts to Review
•The cell cycle - from Intro to Patho slides
•Euchromatin and heterochromatin Genetics
•Penetrance Slides
•Expressivity
•miRNA (microRNA)
•Point mutation, chromosomal mutation
•Autosomal dominant, autosomal recessive
Role of cytotoxic T cells - Inflammation slides
Cancer
•Cancer is the name given to a collection of related diseases. In all types of cancer, some of the body's cells begin to divide without stopping and spread into surrounding tissues." (Definition from cancer.gov)
-Uncontrolled cellular proliferation is the defining characteristic of cancer.
Carcinogen
Any substance that can cause cancer.
KNow this
Cancer is the second leading cause of death in US
What has the highest cancer incidence
Breast Cancer is the most newly-diagnosed cancer
What causes the highest mortality?
Lung Cancer is the #1 most deadly cancer
US Cancer Epidemiology
Cancer mortality is higher among males/AMAB than females/AFAB.
Highest Black Males
Lowest Asian/PAcidic Island Females
All ages can get cancer
What causes incidence?
•Incidence varies with age, race, geographic factors, genetic background
oGeographic variation due to different environmental exposures
o In poorer nations, cancer from infectious causes (such as cervical cancer) tends to predominate, rather than cancers typical of older age (See NY Times article in module)
o In general, cancer can be thought of as a disease associated with older age, although it can happen at any age.
o88% of people diagnosed with cancer (life time of accumulating murations) in the US are 50 years of age or older, and 57% are 65 or older.
Colon cancer in younger people... should we chnage guidelines (45?) for people?
Epidemiolgy and Cancer Risk Factors
Colon cancer (least to most) Japan, Japanaese families in the U.S., U.S
Stomach Cancer (h.pylori is more commo in asia) Japan, Japanese families in the US, US
What is cancer primarily caused by?
Cancer is primarily caused by changes to genes that control cell function, especially growth and division.
What are BRCA1 and BRCA2 mutations linked to?
BRCA1 and BRCA2 mutations are linked to an increased risk of breast and ovarian cancers.
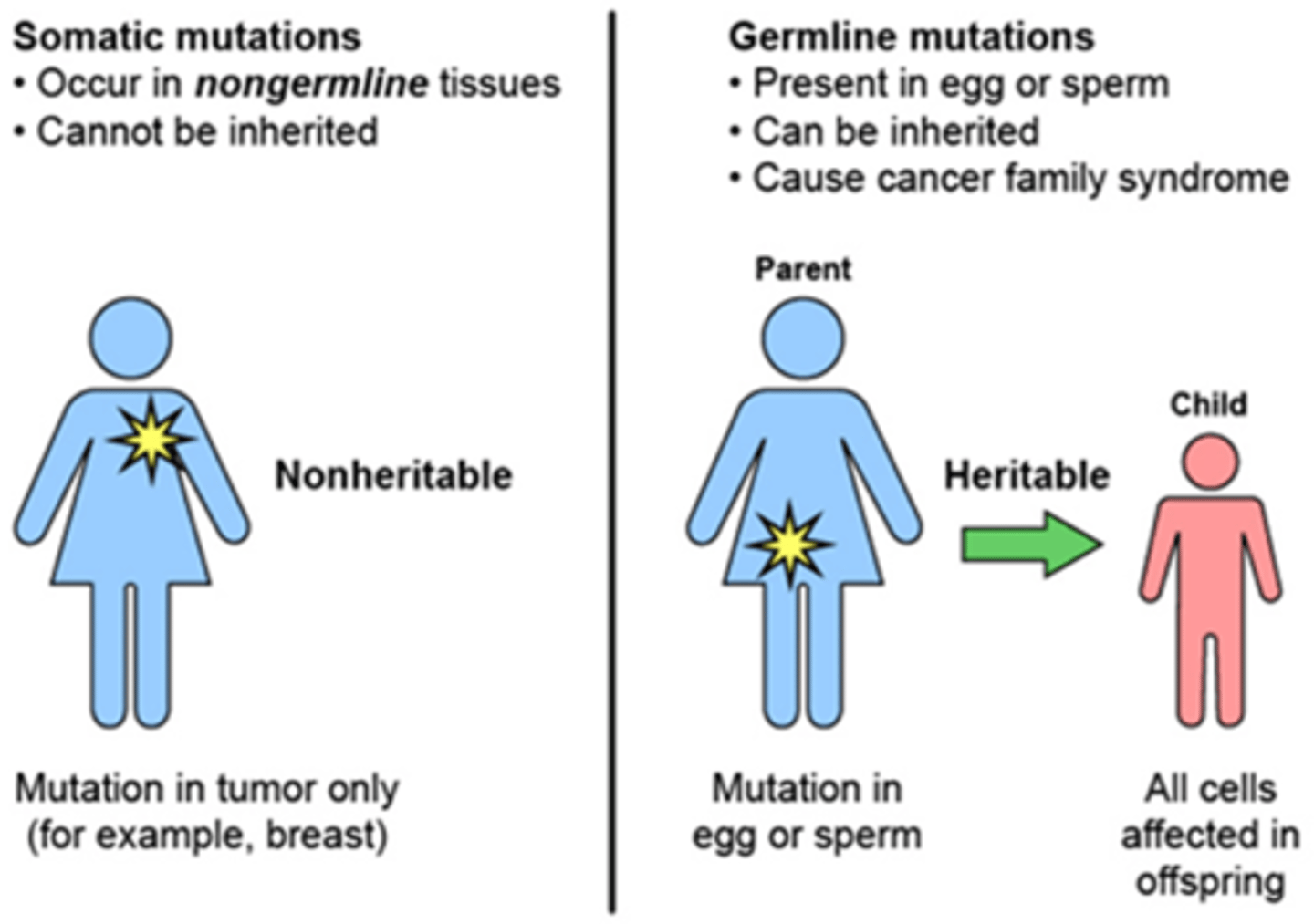
What is the difference between somatic and germline mutations?
Somatic mutations occur in non-reproductive cells, while germline mutations are inherited and present in reproductive cells.
Do all mutations cause cancer?
No, not all mutations cause cancer; some may only change the expression of the gene.
What environmental factors can contribute to cancer?
Environmental factors include sunlight, UV radiation, air pollutants, and occupational exposure to radiation or chemicals.
Which profession is mentioned as being at risk for bladder cancer?
Hairdressers are mentioned as being at risk for bladder cancer.
What types of microbes are known to increase cancer risk?
Bacteria like H. pylori and viruses such as Epstein-Barr, HPV, and Hepatitis B and C are known to increase cancer risk.
How does HPV affect cancer risk?
HPV affects/inactivates tumor suppressor proteins that are already made, increasing cancer risk.
What individual factors are associated with greater cancer risk?
Tobacco use, obesity, poor diet (excess red meat, few fruits and vegetables), inactivity, and heavy alcohol use.
Which group may be at higher risk for certain cancers according to the American Cancer Society?
LGBTQ+ people.
What are some medical treatments for cancer?
Chemotherapy, radiation, targeted treatments, and immunosuppressive drugs.
What risk is associated with cancer treatments?
They can damage healthy cells and lead to 'second cancers'.
What is a potential risk for survivors of childhood cancer?
They may be at risk for adult cancer due to the original treatment.
How has the risk of adult cancer for childhood cancer survivors changed over time?
It is becoming less of a risk as cancer therapy becomes more targeted.
What is an example of a late effect of childhood cancer treatment?
Childhood chest radiation can lead to later breast cancer.
What are potenitally modifiable causes of cancer?
Cigarette smokinf, excess body weight, Alcohol consumption, UV radiation exposure, poor diet, pathogenic infections, physical inactivity
What are the two types of carcinogens found in tobacco?
Initiator (causes genetic damage) and Promoter (promotes tumor growth)
How many known carcinogens are in tobacco smoke?
At least 60 known carcinogens
What percentage of cancer deaths in the US is cigarette smoking directly related to?
At least 1/3 of all cancer deaths annually
What is the most significant cause of lung cancer?
Cigarette smoking
What types of cancer are most commonly associated with tobacco use?
Lung cancer, larynx cancer, oral cavity cancer, and esophagus cancer
Which cancers are highly associated with tobacco use besides lung cancer?
Bladder, kidney, pancreatic, and cervical cancers
What is the effect of second-hand smoke on lung cancer risk?
It increases the risk for lung cancer
How many types of cancer is tobacco associated with?
18 types of cancer
KNow this
Obesity and PHysical INactivity increase risk of certain cancers
Alcohol increases the risk (5+)
What dietary factor is believed to increase the risk of prostate, endometrium, and colon cancer?
High-fat diet
What substance is associated with an increased risk of cancer when used heavily?
Heavy alcohol use
What dietary component is likely protective against cancer?
Fiber
What type of nutrients are considered likely protective against cancer?
Antioxidants
What food preparation methods are associated with stomach cancer?
Pickling, curing, and smoking food
What are certain food additives believed to be associated with?
Cancer
What is the definition of neoplasia?
Neoplasia is a tumor or neoplasm, meaning 'new growth' and is an abnormal mass of tissue.
What are the two types of neoplasia?
Neoplasia may be benign or malignant.
What is a malignant neoplasm commonly referred to as?
A malignant neoplasm is commonly referred to as cancer.
Benign vs Malignant Tumor (Degree of differenciation, Rate of Growth, Local Invasivesness, DIstant Spread/ Can metasizie
Benign: HIgh, Slow, not invasive usuallly encapsulated, no
Malignant: Poor, Rapud, Invasive, Metatasees COmmon
Differentiate
•Recall that stem cells can differentiate and become any kind of cell.
•Differentiation is a developmental process in which cells acquire the capacity for a more specialized function by change of phenotype.
•When cells differentiate, they mature and become specialized for a specific function.
•General rule: Once healthy cells are differentiated, they do not change into a different type of cell.
-Do not confuse this with metaplasia, where one cell type is replaced by another cell type.
•Cancer cells have poor differentiation, meaning that they do not mature and take on a specific function.
What is the malignant phenotype?
It arises due to loss of control of cell number (uncontrolled growth).
What causes the malignant phenotype?
It is due to increased proliferation of cells and reduced death of cells.
How do cells behave in the malignant phenotype?
Cells lose their differentiated features and contribute poorly to the function of their tissue.
What can happen to cells in the malignant phenotype regarding differentiation?
Cells may have multiple stem cell types and can dedifferentiate to act more like stem cells.
What is carcinoma?
Cancers that occur in epithelial tissues in the body, comprising 80% to 90% of all cancers.
What are some examples of carcinoma?
Breast, lung, colon, skin, prostate cancers, and adenocarcinoma.
What is sarcoma?
Cancers that occur in connective tissue like bones, cartilage, fat, blood vessels, and muscles.
What are some examples of sarcoma?
Osteosarcoma, Ewing sarcoma, rhabdomyosarcoma, and leiomyosarcoma.
What is myeloma?
Cancers that occur in plasma cells in the bone marrow, including multiple myeloma.
What are leukemias?
A group of cancers of the bone marrow that cause large numbers of abnormal blood cells to enter the bloodstream.
What are leukemias sometimes called?
Liquid cancers.
What are lymphomas?
Cancers that develop in the glands or nodes of the lymphatic system.
What are the two main types of lymphomas?
Hodgkin lymphoma and non-Hodgkin lymphoma.
What are mixed cancers?
Cancers that arise from more than one type of tissue.
What are multiple myeloma cells?
Multiple myeloma cells are abnormal plasma cells that build up in the bone marrow and form tumors in many bones of the body.
What is the function of a plasma cell?
A plasma cell is known as an 'antibody factory'.
What happens to plasma cells in multiple myeloma?
Numerous clones of a single plasma cell are typically generated.
What effect does an increase in multiple myeloma cells have on antibodies?
As the number of multiple myeloma cells increases, more antibodies are made.
What can result from the increased production of antibodies in multiple myeloma?
It can cause the blood to thicken and keep the bone marrow from making enough healthy blood cells.
How do multiple myeloma cells affect bones?
Multiple myeloma cells damage and weaken the bone.
Grading and Staging Cancers
higher numbers in grading mean the cancer cells are more abnormal and higher numbers in staging mean the tumor is larger and has spread farther
Genetic Mechanisms of Cancer
•Cancer cause - mutations
•Mutations acquired (somatic) or inherited (germline)
What percentage of all cancers are sporadic?
95%
What are sporadic mutations?
Mutations that are acquired/somatic and not inherited.
What are the three patterns of hereditary cancer inheritance?
Autosomal Dominant, Autosomal Recessive, Familial Cancers of Uncertain Inheritance.
What is the characteristic of Autosomal Dominant Cancer Syndromes?
A single copy of an inherited mutant gene increases cancer risk.
What is usually required for cancer to manifest in Autosomal Dominant Cancer Syndromes?
An acquired mutation in the other copy of the gene.
What is meant by incomplete penetrance in Autosomal Dominant cancers?
Not all individuals with the mutant gene will develop cancer.
What is the inheritance pattern of Autosomal Recessive cancers?
Two copies of the mutated gene are inherited.
What do parents of children with Autosomal Recessive cancers typically carry?
One copy of the mutated gene, but do not usually show signs of cancer.
What are the characteristics of Familial Cancers of Uncertain Inheritance?
Early age of onset, predisposition to cancer, higher incidence of tumors in relatives.
What types of genes are most commonly involved in inherited cancers?
Tumor suppressor genes or DNA repair genes.
Are oncogenes usually involved in inherited forms of cancer?
No, most occur as somatic mutations.
Genes That Drive Cancer
•Two general classes of genes: proto-oncogenes and tumor suppressor genes
•Proto-oncogenes - once converted to oncogenes -- act like "gas pedals" to accelerate cell growth and division
•Tumor suppressor genes act like "brakes" to inhibit cell growth and division.
-An important sub-type of tumor suppressor gene is a DNA repair gene. (Some sources consider it a completely separate category and for purposes of this lecture, we will think of it as a separate category.)
Oncogense "the gas"
1 mutation sufficient for accelerated cell growth
Tumor Suppressor Genes: the "brakes
2nd mutation or loss (leads to cancer)
DNA Repair Genes: the Mechanics
Correct Errors so fewere mutations; more mutations more we would like these to fix the problems
Proto-Oncogenes
•Are normal cellular genes that are essential for growth/proliferation
•Transformed into oncogenes by mutations that are activating (gain-of-function);
•One copy of an activated proto-oncogene is sufficient to start the process of accelerated/uncontrolled cellular growth.
•Proto-oncogenes may code for:
-Growth factors
-Growth factor receptors
-Cytoplasmic signaling molecules
-Nuclear transcription factors
-Proteins involved in cell-cell or cell-matrix interactions
Proto-Oncogenes Are Important for Normal Cellular Proliferation, But Can Cause Out-of-Control ProliferationWhen Mutated
How can oncogenes be introduced to host cells?
Oncogenes can be introduced to host cells by retroviruses.
What is one way a proto-oncogene can become an oncogene?
A proto-oncogene can mutate to an oncogene through a point mutation.
What happens when a normal proto-oncogene becomes overactive?
A normal proto-oncogene can become overactive through translocation or mutation of its regulatory sequence.
What is gene amplification in the context of proto-oncogenes?
Gene amplification refers to having extra copies of a normal proto-oncogene in the genome.
What are the three related proto-oncogenes in the RAS gene family?
KRAS, HRAS, NRAS
What percentage of cancers involve a mutation in one of the RAS genes?
More than 30%
What percentage of pancreatic cancers involve a mutation in RAS genes?
95%
What is the normal function of RAS proteins?
To signal a cell to divide and proliferate
What activates RAS proteins to their 'on' state?
Extracellular signals
What molecule do RAS proteins bind to when activated?
GTP (guanosine triphosphate)
How do RAS proteins turn 'off'?
By hydrolyzing GTP to GDP (guanosine diphosphate)
What happens to cancer-causing forms of RAS proteins?
They have a disabled 'off' switch and cannot hydrolyze GTP to GDP
What state do cancer-causing RAS proteins remain in?
Stuck in the 'on' state, bound to GTP
What do continuously signaling RAS proteins lead to?
Cancer
What is the role of Tumor Suppressor (ts) Genes in cancer?
They contribute to cancer when inactive.
What happens to both copies of tumor suppressor genes when cancer develops?
Both copies are inactivated, leading to loss of function.
What is the 'Two Hit Hypothesis'?
It states that if a defective copy of a tumor suppressor gene is inherited, there is a much higher risk for later cancer development.