Labor Variations
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
Cervical Ripening
A process that prepares the cervix for labor induction
Laboe induction
A procedure that stimulates contractions to start labor
augmentation
stimulates uterine contractions after labor has already started
Induction of Labor (IOL)
artificial initiation of labor before spontaneous onset.
When is induction of labor useful?
when benefit of delivery outweighs benefit of a continued pregnancy
Nursing role of induction of labor
Ensure well-documented discussion of risks, benefits and alternatives (r/b/a)
○ Include rationale for induction, method of induction and risks
Maternal indications
○ Premature rupture of membranes (PROM)
○ Hypertensive disorders of pregnancy
○ Gestational Diabetes
○ Post-term pregnancy
○ Elective
○ Many more
Fetal indications
● Post-term pregnancy
● Maternal diabetes (pre-gestational or insulin dependent)
● Fetal growth restriction (FGR)
● Macrosomia
● Oligohydramnios
● Many more
IOL Contraindications
● Complete placenta previa- placenta covering the cerix, risk of bleeding
● Non Cephalic presentation
● Previous classical cesarean (usually)
● Prior uterine rupture
● Active genital herpes
what can we do if we can’t induce labor?
c section
Starting an Induction: Vaginal Exam
● Palpation of cervix
● Presentation
● Position
● Membranes
● Pelvic assessment
● Fetopelvic relationship
What number on the bishop score requires a cervical ripening
6 or less
Bishop score minimum and maximum
0-15
dilation
the gradual opening of the cervix measured in centimeters from 0-10 cm
Mechanical ripening methods
cervical ripening balloons work by applying direct pressure to the internal cervical os, stimulating endogenous prostaglandin release and promoting mechanical cervical dilation
foley balloon
cook balloon
Foley Balloon:
A single balloon filled with saline that gently stretches the cervix to help it open. It’s affordable and commonly used.
Cook Balloon
Has two balloons—one inside and one outside the cervix—for more even pressure. It may be easier to place and can be more effective in some cases
pharmacologic methods if cervical ripening
•Prostaglandins:
•help soften and open the cervix by triggering inflammatory responses. They increase cytokines like interleukin-8, which attract white blood cells and promote collagen breakdown and tissue remodeling
cervidil (dinoprostone)
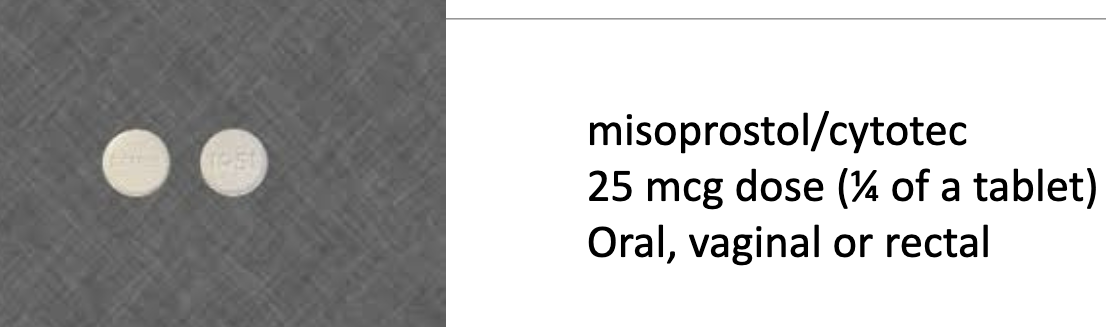
misoprotol (cytotec)
contraindiacation c section
Contraindications of pharmacologic method
previous c section/uterine surgery
risk tachsystole (uterine hyperstimulation)
Cervidil (Dinoprostone)
vaginal insert that releases prostaglandins slowly to soften and dilate the cervix.
•Considered gentler and more controllable, with fewer risks of uterine overstimulation

Misoprostol (Cytotec)
Used off-label for labor induction. It’s a tablet (oral or vaginal) that acts faster and is more potent, but carries a higher risk of uterine hyperstimulation
Adverse Effects of Prostaglandins
tachysystole can occur with overstimulation
Nursing interventions Adverse Effects of Prostaglandins
position change—sideline
Monitor breathing, HR, BP
discontinue cervidil (if applicable)
turn off pitocin (if running)
fluid bolus- rehydrates the body and muscle. dilutes the medication
K.H is a 28 year old G1P0 who presents to L&D for induction of labor due to pre-eclampsia without severe features at 37w0d. Her cervix is assessed by the nurse and found to be 1cm/50%/-3, posterior, firm.
○ What is her bishop score?
○ Does she need cervical ripening?
2
yes less than 6
Z.B is a 33 year old G2P1001 at 41w2d who presents for IOL due to post-term pregnancy. Her cervix is assessed to be 3cm/70%/0, mid, soft.
○ What is her bishop score?
○ Does she need cervical ripening?
9
no
Which of the following patients is NOT a candidate for cervical ripening with
prostaglandins?
A. G1P000, gestational diabetic this pregnancy
B. G2P1001, first baby born via cesarean section
C. G2P1001, first baby born vaginally
G2P1001, first baby born via cesarean section
Methods of augmentation
○ Pitocin (most common)
○ Artificial rupture of membranes (AROM)
Pitocin route
IV
Pitocin
is a synthetic version of oxytocin (natural labor inducer produced by the body), used for labor induction.
○ It works by binding to oxytocin receptors in the uterine muscle, triggering rhythmic contractions that help dilate the cervix
effect of pitocin
causes uterine contractions
dangers of pitocin
○ Tachysystole
○ Uterine rupture
○ Uterine atony and PPH
○ Fetal distress
IV Oxytocin (Pitocin) Infusion
Hung as a secondary line
○ Should be inserted into the primary (maintenance) IV line as close as possible to the venipuncture site (proximal port) to limit the amount of drug infused after stopping it
○ Start at a low dose, and increase every ~30 minutes until uterine contractions are regular (check facility protocol)
Nursing considerations when giving pitocin
○ Monitor patient’s BP and HR q30 minutes (or per site protocol)
○ Must do continuous monitoring of fetal HR and contractions
Pitocin use and non-reassuring fetal heart tones
● Reduce or Stop Pitocin infusion
● Increase rate of primary IV line (typically LR)
● Move patient to side-lying position
● Continue to assess fetal heart rate and contractions
● Administer Terbutaline (tocolytic) if ordered (stops contractions)
Artificial rupture of membranes (AROM) via Amniotomy risk
○ Cord prolapse
■ If fetal head not well engaged cord can slip when fluid is relased leading to cord compression and reducted fetal oxygenation
○ Chorioamnionitis (infection)
■ Protective barrier now gone, particularly with frequent vaginal exams
○ Fetal Distress
Artificial rupture of membranes (AROM) via Amniotomy reasons to use
Labor induction/Augmentation
■ Other: Internal fetal monitoring needed
Artificial rupture of membranes (AROM) via Amniotomy procedure
Amnihook perforated amniotic sac
Nursing role with amniotomy (AROM)
○ Fetal Heart Rate:
■ Obtain baseline fetal heart rate tracing (20-30 min) before procedure
■ Monitor fetal heart rate for at least 1 full minute after procedure; report abnormal finding to provider immediately (I advise more time)
○ Provide supplies: towels, amnihook, sterile glove, sterile lubricant
○ Chart color, quantity, and odor of fluid
○ Assess for signs of infection
■ Take patient’s temperature on interval determined by unit
● Report temp > 100.4 F
■ Monitor for fetal tachycardia (sustained rate >160 bpm)
types of vaginal delivery
vacuum
forceps
indication for vaginal delivery
• Prolonged second stage of labor
• Maternal exhaustion or medical conditions limiting pushing
• Signs of fetal distress requiring expedited deliver
mechanism forceps delivery
Metal instruments are placed around the baby’s head to guide it out during contractions
benefits forceps delivery
Offers strong traction and control, especially useful for rotating the baby’s head
risk of forceps delivery
Higher chance of maternal perineal tears and fetal facial injuries (e.g., bruising, nerve palsy
vacuum delivery mechanism
A suction cup is placed on the baby’s head to assist with pulling during
contractions
vacuum delivery benefits
Easier to learn and less invasive for the mother
vacuum delivery risk
Increased risk of fetal scalp injuries like cephalohematoma, intracranial fetal
hemorrhage, and jaundice, also higher risk of maternal perineal tears
Operative vaginal- RN considerations mother
● Patient’s bladder should be empty (typically by straight cath)
● Assess FHR
● After birth, observe for trauma of patient or baby
● Cold application to perineum/ vagina for the first 12 hours may reduce pain and limit bruising and edema
Operative vaginal- RN considerations newborn
○ Assess for skin breaks; if present, keep them clean
○ Assess for facial asymmetry that may suggest nerve injury (typically temporary)
○ Assess for neurologic abnormalities such as seizures which suggest intracranial hemorrhage, hypoglycemia, or sepsis
○ Scalp edema after vacuum extraction is common; facial bruising after forceps is common
■ Both will resolve without treatment
TOLAC
trial of labor after cesarean
VBAC
-vaginal birth after cesarean
TOLAC trial of labor after cesarean
○ Small, but significant risk of uterine rupture (1/100)
○ Advised in setting with access to emergency services: OR, anesthesia
○ Prostaglandin cervical ripening methods contraindicated
○ Pitocin can be used
○ Electronic fetal monitoring needed
TOLAC benefits
● Lower Maternal Risk:
○ Successful TOLAC (resulting in VBAC) is associated with less bleeding,
fewer infections, and shorter recovery time compared to repeat cesarean delivery.
● Fewer Future Complications:
○ VBAC reduces the risk of placenta previa, placenta accreta, and surgical complications in future pregnancies.
● Avoids Major Surgery:
○ TOLAC offers a chance to avoid another cesarean, which is a major abdominal surgery with its own risks.
● Supports Birth Preferences:
○ It allows birthing individual who prefer vaginal birth the opportunity to achieve that goal.
● Reduces Cesarean Rates:
○ On a population level, successful TOLAC helps lower overall cesarean
delivery rates, which benefits maternal health systems.
Episiotomy
A small surgical cut made in the perineum during vaginal delivery to widen the opening
Episiotomy risk
pain, infection, and longer healing time
Episiotomy benefit
prevent severe tearing or speed up delivery in emergencies.
External Cephalic Version (ECV)
A procedure done around 37 weeks to manually turn a breech baby to a head-down position
External Cephalic Version (ECV) benefits
Can reduce the need for cesarean delivery and increase chances of vaginal birth
External Cephalic Version (ECV) risk
low but may include fetal distress or emergency C-section in rare cases
C section indications that occur 50% of the time
labor dystocia
abnormal/indeterminate fetal heart rate tracing
c section indications
○ Labor dystocia
○ abnormal/indeterminate fetal heart rate tracing
○ Fetal malpresentation
○ Multiple gestation
○ Suspected macrosomia
○ Active genital herpes
○ Various placental abnormalities (complete previa, vasa previa)
○ Cord prolapse
○ Elective/Repeat cesarean
○ More
c section risk
○ Major hemorrhage
○ Uterine rupture
○ Anesthetic complications
○ Shock
○ Cardiac arrest
○ Infection
○ Wound disruption
○ Injury to newborn
C/S: pre-op nursing interventions
● Assess time of last oral intake
● Allergies
● Current medications (including last dose)
● Informed consent must be signed
● Obtain lab work: CBC, blood type and screen
● Pre-op teaching
● Start IV and bolus
● Clip abdominal hair
● Administer prep-op antibiotic (Ancef typical)
● Administer ordered medication to control gastric secretions
○ Commonly Bicitra or pepcid
● Insert catheter
● Assist patient onto the table; place wedge under hip
● Apply grounding pad for electrocautery
● Do sterile prep of abdomen