4. Adaptation and Death
1/159
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
160 Terms
When an insult to homeostasis occurs, what are the two paths the body can take? What can they pathways each lead to?
1) Degeneration (reversible) -> Recovery or necrosis (irreversible)
2) Adaptation (reversible; But can switch to degeneration) -> Recovery or neoplasia (irreversible)
Adaptation usually occurs with more ___________ insults to homeostasis while degeneration usually occurs with more ___________ insults to homeostasis.
- Chronic
- Acute
Lack of __________ is an especially common insult to a cell.
- Oxygen
Define hypoxia, anoxia, and ischemia.
- Hypoxia = Partial reduction in oxygen supply (-oxia = oxygen)
- Anoxia = Complete loss of oxygen supply
- Ischemia.= Partial or complete loss of blood supply (-emia = blood)
What are some examples of things which can cause a reduction in oxygen supply to the tissues?
- Inflammation, trauma, etc. -> Damaged tissue unable to use oxygen
- Pressure (mass effect, fluid buildup, etc.)
- Disruptions in blood flow (ischemia), but also reduced erythrocytes (hemorrhage, reduced production, etc.), lung disease (unable to take up oxygen)
- Increased fluid in tissue -> Increased distance from cells to blood supply
- Demand > supply (ex. muscle cramps while running)
Regardless of the initiating cause/insult to the cell, the result is a cascade of stereotypical cellular responses. What are these responses? What is this generally referred to as?
1) Reduced oxygen
2) Reduced ATP production
3) Failure of Na/K ATP pump
4) Loss of fluid homeostasis
5) Accumulation of intracellular water
- This loss of fluid balance and accumulation of intracellular water is called hydropic degeneration
What is the hallmark of reversible cell injury?
- Hydropic degeneration (A loss of fluid balance and accumulation of intracellular water)
Hydropic degeneration is also called what?
- "Acute cell swelling" or just "degeneration"
What is "the mother of all degeneration"?
- (Hydropic) Degeneration
Cellular degeneration is "low key ___________" according to Dr. Ihms.
- Drowning
What is the definition of degeneration? How can the cell return to normal, if it can?
- Reversible deterioration of a cell as a result of sublethal injury
- Cell can return to normal if source of injury is removed in time
Describe what happens to organelles, cell membranes, and the nucleus during cellular degeneration.
- Damage to organelles
- Cell membranes are intact
- Nucleus is intact
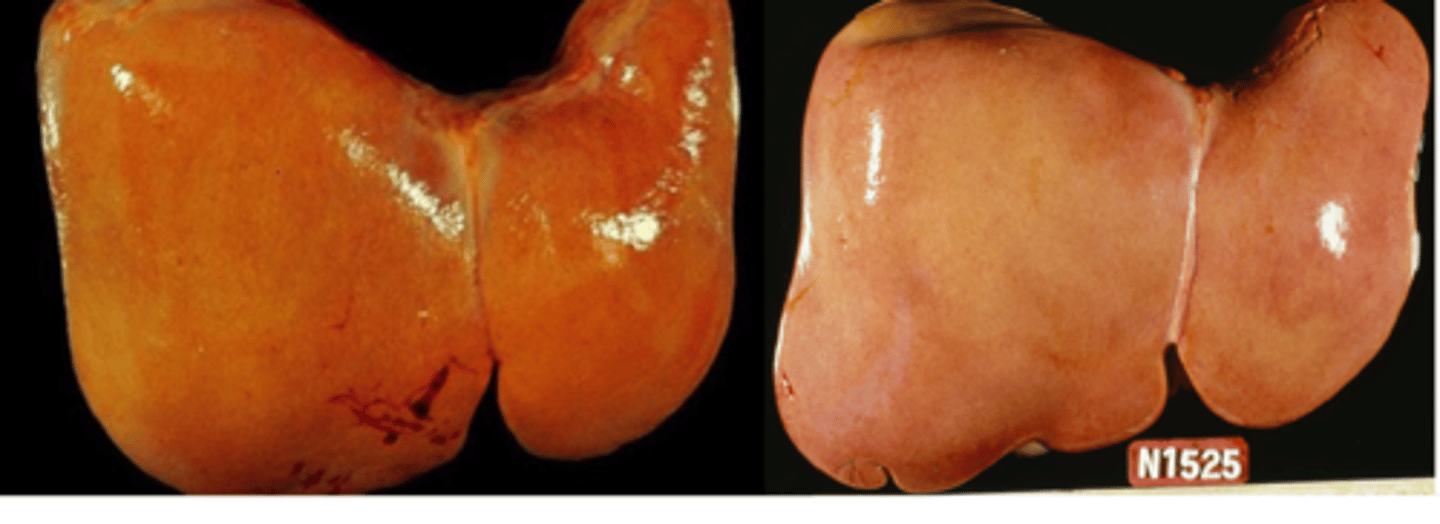
Describe tissues which are undergoing degeneration.
- Enlarged, swollen
- Wet, heavy
- Paler than normal
- Softer than normal
Define fatty degeneration.
- Intracellular accumulation of lipids within non-adipose cells (aka lipidosis) as cells are unable to process lipid (either due to excess delivery or organ dysfunction)
Describe fatty degeneration microscopically.
- Normally, lipid droplets in cells are not microscopically visible. Accumulation of lipids leads to coaslesce into larger (visible) droplets in cells. Droplets have sharp borders (lipid and water interface)
Where does fatty degeneration tend to occur?
- Tissues with high lipid metabolism = Liver > kidney > skeletal muscle
Grossly, how does fatty degeneration appear?
- Tissue is paler, softer, yellow, and greasy
What is a classic example of fatty degeneration in cats? Describe its pathogenesis.
- Hepatic lipidosis in cats
- 1) Obese cats become anorexic (any cause)
- 2) Delivery of lipid to the liver increases to prevent starvation
- 3) Delivery exceeds ability of the hepatocytes to process the lipid
- 4) Lipid accumulation in hepatocytes
- 5) Fatty degeneration of hepatocytes
Once a cat develops hepatic lipidosis, what two things can happen?
- Cat starts eating -> Lipid delivery to liver decreases -> Hepatocytes can process lipid and recover
- If cats do not start eating -> Eventual death of hepatocytes
What are the three primary effects of degeneration on body systems?
1) Loss of luxury functions
2) Switch from aerobic to anaerobic metabolism
3) Leakage of cellular contents
What does a loss of luxury functions during degeneration involve?
- Anything not immediately related to cell survival (hormone secretion, enzyme production, cilia, microvillia, etc.) is lost
A switch from aerobic to anaerobic metabolism can lead to what?
- Production of toxic metabolites (lactic acid) -> Additional damage
What does membrane injury result in?
- Calcium influx and intracellular release/activation of lysosomal enzymes
What are hallmarks of irreversible injury to a cell?
- Loss of control of calcium homeostasis (mineralization of mitochondria = beginning of the end)
- Loss of cell and organelles membrane integrity -> Rupture
- Intracellular enzyme release/activation -> Self-digestion
What is the end result of hydropic degeneration if the cell cannot recover?
- (Oncotic) necrosis
Is necrosis sometimes physiologic?
- No; always pathologic
Is necrosis a controlled, organized form of death or a messy, uncontrolled death.
- Messy, uncontrolled death
With membrane breakdown during (oncotic) necrosis, there is release of cell contents such as what?
- Damage associated molecular patterns (DAMPs): ATP, host DNA, Actin
- Alarmins
- Digestive enzymes
- Intracellular pathogens
Necrosis is pro- or anti-inflammatory?
- Pro-inflammatory
What is pyknosis?
- Shrunken, condensed, dark, homogenous clumped chromatin
What is karyorhexis?
- Rupture of nuclear membrane, release of nuclear fragments
What is karyolysis?
- Pale nucleus, dissolution of chromatin
Differentiate between degeneration and necrosis microscopically.
- Degeneration: Cells are clearly unhappy, but nuclei are intact
- Necrosis: Shrunken/absent nuclei, cells falling off basement membrane
The gross appearance of necrosis is highly __________________.
- Variable
What is the color of tissues associated with necrosis?
- Necrosis does not have a color; Takes on the color of what is happening around it (RBCs, WBCs, fluid, etc.)
Describe the texture of necrotic tissues.
- Soft (Friable)
Describe the demarcation of necrotic tissues.
- Necrotic tissues may be sharply demarcated from surrounding healthy tissue +/- surrounded by a red rim of acute inflammation
Necrosis on surfaces (i.e. skin, mucous membranes) can lead to what?
- Mucosal ulceration, sloughing
Why can necrotic tissues appear white, chalky, and hard?
- Dystrophic mineralization
What is erosion?
- Loss of surface epithelium above the basement membrane
What is ulceration?
- Loss of surface epithelium and basement
What may be observed with chronic ulcertion?
- Central depression (something lost) and raised borders (something added); The cells around the ulcer proliferate in an attempt to fill the gap
Does necrosis happen to dead tissues?
- No; Necrosis only happens in live tissue; autolysis occurs in dead tissue
Which is reversible, degeneration or necrosis?
- Degeneration
Describe the appearance of degeneration vs. necrosis.
- Degeneration: Swollen, pale, soft, wet, heavy
- Necrosis; Variable color, often soft; cell may be swollen (addition of fluid) or shrunken (removal of cells
Describe the nuclei, cell membranes, and other organelles of tissues undergoing degeneration vs. necrosis.
- Degeneration: Nuclei are intact; cell membrane and organelles are intact
- Necrosis: Nuclear changes (lysis, rhexis, pyknosis, absence); Rupture of cell and organelle membranes
Describe the calcification that occurs with degeneration vs. necrosis.
- Degeneration: No calcification
- Necrosis: Calcification of cell and organelles
What are the five types of necrosis?
1) Coagulative
2) Liquefactive
3) Caseous
4) Fat
5) "Gangrene"
Explain how coagulative necrosis occurs.
- Rapid death of cell (often ischemic and too fast for inflammatory signs to occur) -> Coagulation of cell protein (like cooking an egg), resulting in death of cells with visible "ghosts" of cell outlines
Is tissue architecture maintained during coagulative necrosis?
- Yes; Tissue holds together
Describe the appearance of coagulative necrosis.
- Often sharply demarcated; Often pale compared to adjacent tissue
What is the default form of necrosis in the brain?
- Liquefactive necrosis
How does liquefactive necrosis occur?
- Death of cells followed by enzymatic digestion -> Dead cells release proteases, DNAses, lysosomal enzymes, reactive oxygen species (ROS)
Is tissue architecture maintained during liquefactive necrosis?
- Loss of tissue architecture - Tissue is liquefied
During liquefactive necrosis, nucleated cells are replaced. by what?
- "Vast pink wasteland", sometimes surrounded by a blue rim of infiltrating inflammatory cells (necrosis is pro-inflammatory)
Describe tissues undergoing liquefactive necrosis.
- Tissue is very soft, color is variable (Hemorrhage -> Red/black; WBC -> White/pale)
What type of necrosis is typical in any tissue during bacterial infections?
- Liquefactive necrosis (think of the consistency of pus)
Coagulative necrosis often occurs very ______________ with ______________ inflammation. Liquefactive necrosis is often associated with _________________ and with _____________ inflammation.
- Rapidly; Minimal
- Bacteria; More
Caseous means "___________-like".
- Cheese
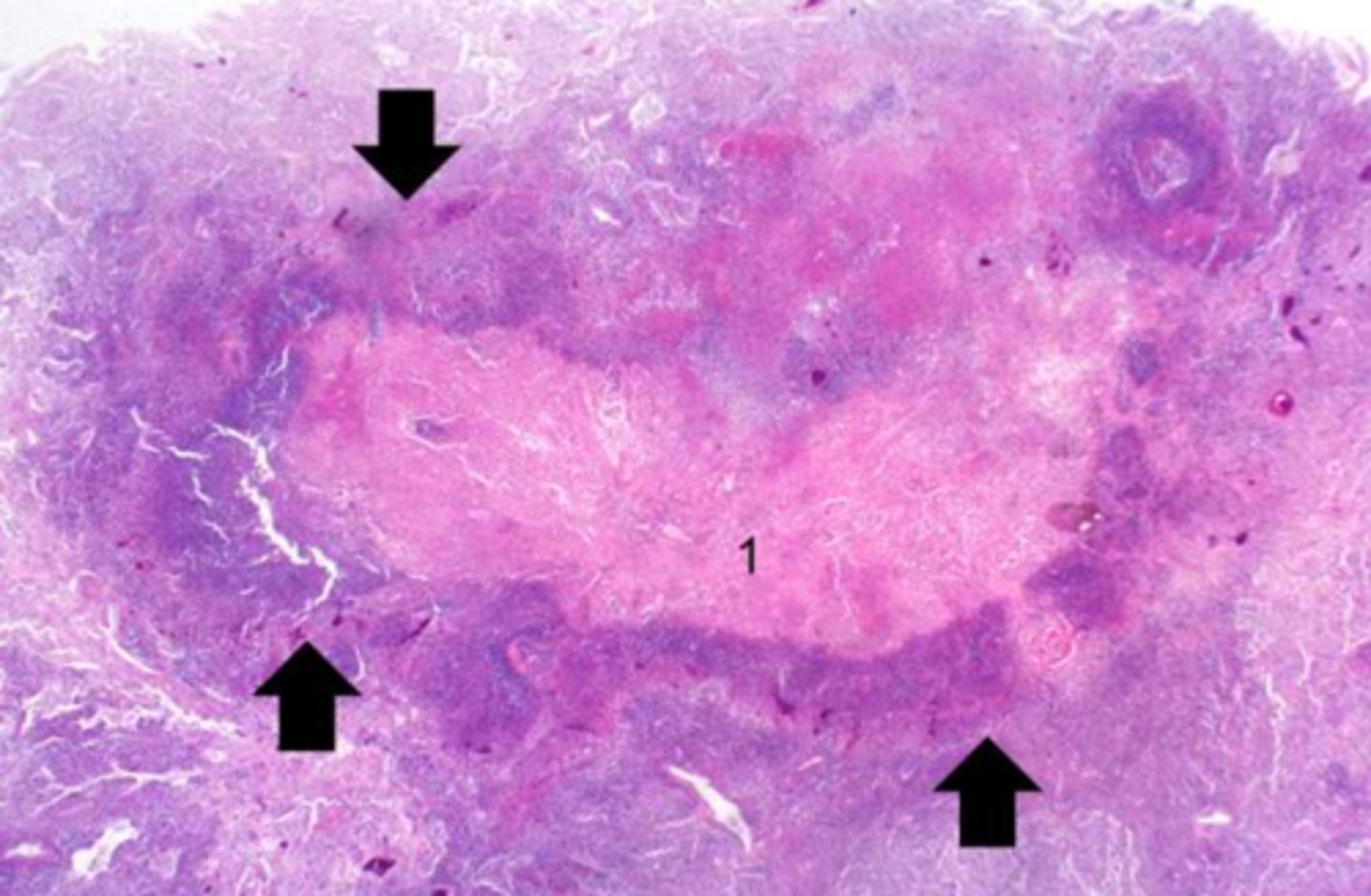
How does caseous necrosis occur?
- Liquefactive necrosis over time becomes dehydrated *"inspissated" as the water is reabsorbed.
Caseous necrosis involves old area of ______________ often with _____________ _________________.
- Liquefaction
- Dystrophic mineralization
Describe the gross appearance of caseous necrosis.
- "Feta cheese texture"; Dry, crumbly, chunky, or granular
How is caseous necrosis distinguished from liquefactive necrosis histologically?
- Not clearly distinguishable
Caseous necrosis has a strong associated with what?
- Granulomatous inflammation (macrophages) (i.e. tuberculosis is the "prototype" caseating lesion)
What type of necrosis is extremely common in non-mammals?
- Caseous necrosis
Explain the example of caseous lymphadenopathy which occurs in goats/sheeps discussed in class.
- Contagious chronic bacterial disease of small ruminant (Corynnebacterium pseudotuberculosis) is transmitted via wounds (tail docking, castration) and contact with exudate in the environment. A complex cell wall protects the bacteria from the immune system, leading to chronic infection. The bacteria is carried by macrophages to the lymph nodes where they proliferate. Massive caseous necrosis of lymph nodes occurs, leading to internal abscesses. The lymph nodes often have a "layered" appearance.
Is "fat necrosis" a true type of necrosis?
- Not really; Just describes the unique fat of necrotic adipose tissue.
Explain how "fat necrosis" occurs.
- Lipases release fatty acids from dying adipocytes. The fatty acids form a complex with calcium, forming soaps (saponification of fat).
Describe how "soaps" appear in fatty necrosis.
- White chalky deposits
How is inflammation incited in "fat necrosis"?
- Free lipid may incite inflammation (granulomatous)
Describe the appearance of tissues undergoing "fat necrosis".
- Very firm, tan to chalky-white
What are the causes of "fat necrosis"?
- Enzymatic: Pancreatitis
- Traumatic: Crush or other injury
- Idiopathic: Unknown (abdominal fat in cattle)
How does "gangrene" start?
- Starts with coagulative necrosis
What does the morphology of "gangrene" depend on?
- What happens to the tissue after it dies
What are the types of "gangrene"? Explain them.
- "Wet Gangrene": Invasion of saprophytic (environmental) bacteria resulting in tissue sloughing, gas bubbles, and stench
- "Dry Gangrene": Dry environment with no bacteria resulting in mummification of tissue; often extremities
- "Gas Gangrene": Invasion of anaerobic bacteria (clostridial species) resulting in dark red-black tissue, gas bubbles, and stench
Provide examples of "Dry Gangrene".
- Frostbite, vascular toxins like ergot/fescue
Provides examples of "Wet Gangrene".
- Putrefaction of tissues; intestines
"Dry Gangrene" almost always occurs at the _________________.
- Extremities
Is cell death always pathologic? Is necrosis?
- No - It can be physiological and beneficial to the host
- Yes
Provide examples of when cell death occurs physiologically.
- Embryogenesis, organ sculpting (tadpole tail, digits)
- Cells that have "served their purpose": Leukocytes in tissues after inflammation has resolved; Involution of tissues after hormone withdrawal (thymus)
- Elimination of potentially dangerous cells: Lymphocytes that respond to self-antigen (auto-immunity), damaged host cells that may become neoplastic, tumors cell of infected host cells
Physiologic cell death is also called "___________" cell death to differentiate from necrosis.
- Programmed
What is the major programmed cell death pathway?
- Apoptosis
What occurs with apoptosis?
- The individual cell dies for the good of the organism; Neat packaging of cell contents for disposal -> Cell and nuclear shrinkage, fragmentation -> Apoptotic bodies with "eat me" signal -> phagocytosis by macrophages
What is the incidence of apoptosis?
- All cells, but especially cells with high turnover (i.e. skin)
Provide examples of physiologic apoptosis.
- Normal embryogenesis, control of proliferating cell populations
Provide examples of pathologic apoptosis.
- Response to DNA damage, misfolded proteins, viral infections. etc.
Does apoptosis generate inflammation?
- No
Is apoptosis often appreciated at the gross or microscopic level?
- Microscopic (as opposed to necrosis); Death of individual cells cannot be appreciated grossly
The intrinsic path of apoptosis is also known as what?
- "Mitochondrial pathway"
What is the intrinsic pathway of apoptosis triggered by?
- Intracellular stress; damage to DNA; accumulation of misfolded proteins, etc.
What is the difference in the quantity of apoptotic molecules during homeostasis and cell stress?
- Homeostasis: Pro- vs. Anti-apoptic molecules
- Cell stress: Pro > Anti
How do pro-apoptotic molecules facilitate apoptosis via the intrinsic path?
- Pro-apoptotic molecules form a pore in the mitochondrial membrane (MOMP = Mitochondrial outer membrane pore), leading a release of cytochrome C from the mitochondria, activating cytoplasmic caspases. Caspases are responsible for execution of apoptosis (where pathways converge)
The extrinsic path of apoptosis is also known as what?
- "Dead receptor pathway"
What is the extrinsic pathway of apoptosis triggered by? What does this lead to?
- Triggered by external "death signal" provided by T cells or other sources (elimination of self-reactive lymphocytes, tumor cells, infected cells recognized by T cells)
- Death signal causes internal activation of caspases, which are responsible for execution of apoptosis (where pathway converge(
According to Dr. Ihms, apoptosis is death by "_____________" while necrosis is death by "____________"
- Suicide
- Misadventure
Describe what happens to the cell structure during apoptosis vs. necrosis.
- Apoptosis: Plasma membrane blebbing, vesiculation, cell shrinkage, chromatin condensation
- Necrosis: Plasma membrane rupture, cell swelling, chromatin expansion, dissolution
Describe whether inflammation occurs during apoptosis vs. necrosis.
- Apoptosis: No
- Necrosis: Yes
Describe how many cells are affected by apoptosis vs. necrosis and how many cells are often affected?
- Apoptosis: Single cells -> Not grossly visible
- Necrosis:: Miced group of cells, multiple cells -> Grossly visible
Depending on the severity and nature of the insult, a cell may do what three things?
- Degenerate (reversible)
- Die (Irreversible): Necrosis/apoptosis
- Adapt (reversible) -> Cell attempts to reach a "new normal" under the altered conditions
What type of insults commonly cause a cell to adapt?
- Mild (sublethal) but prolonged insults (the cell must have time to adapt)