Physiology- Pulmonary System
1/92
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
93 Terms
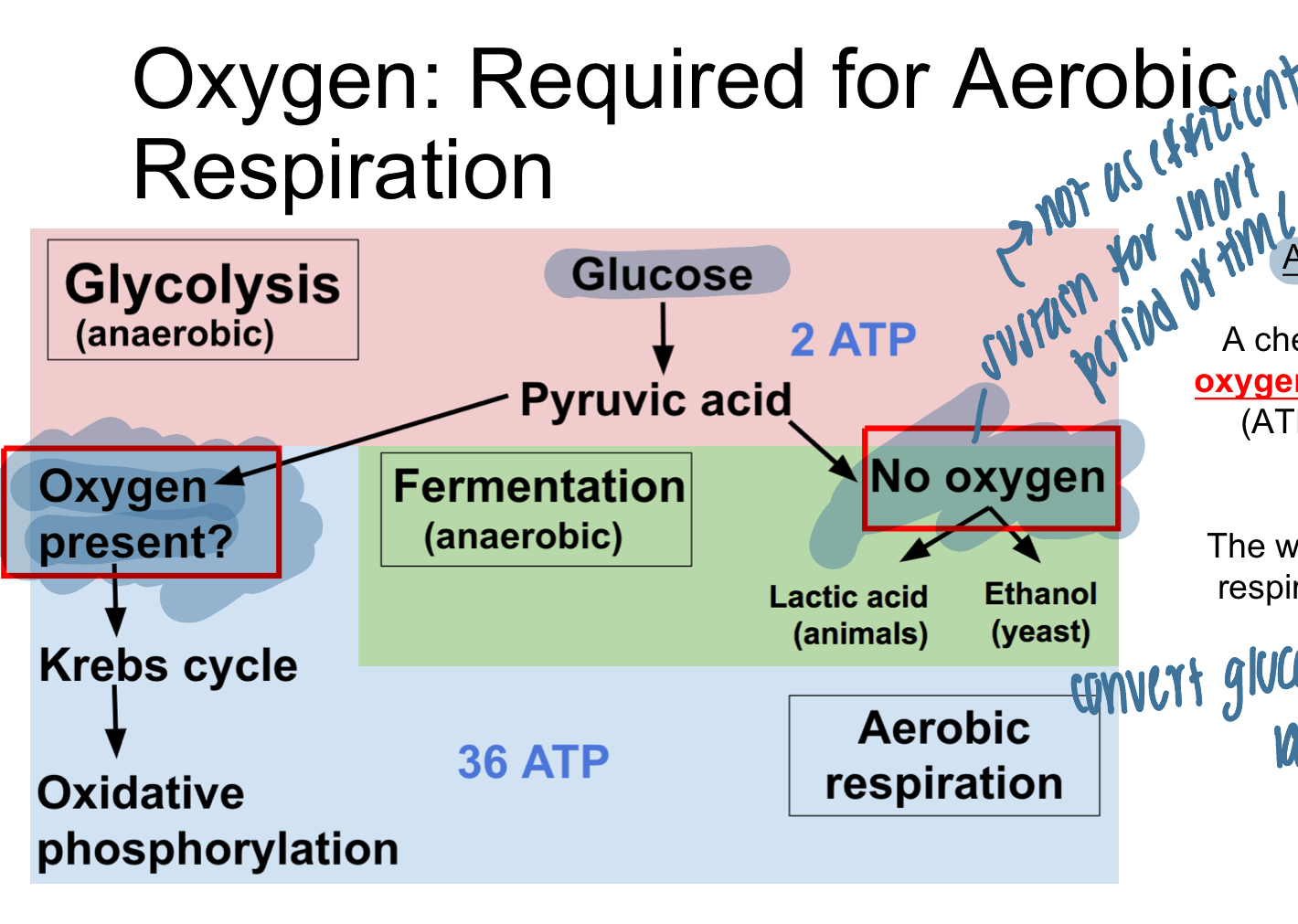
what is required for aerobic respiration?
oxygen
aerobic respiration
chemical process in which oxygen is used to make energy (ATP) from glucose
waste products= CO2 and H20
function of pulmonary system
facilitate exchange of gases btwn environmental air and blood
breathe O2 IN
cells use oxidative phosphorylation to make ATP (cellular/aerobic metabolism
breathe CO2 OUT
CO2 is byproduct of cellular metabolism
needs to get out bc directly affects pH
pH
measure of concentration of free hydrogen ions
lower pH= MORE H+=more acidic (acidosis)
higher pH= less H+= more basic (alkylosis)
how does CO2 cause acidosis?
CO2 acts as a weak acid with H2O; carbonic acid can donate H+→ bicarbonnate and H+=acid
CO2 + H2O ←→ H2CO3 (carbonic acid)←→ HCO3- + H+
pH=…
pH= 1/[H+]
pH= [HCO3-]/ [CO2]
concentration of base/concentration of acid
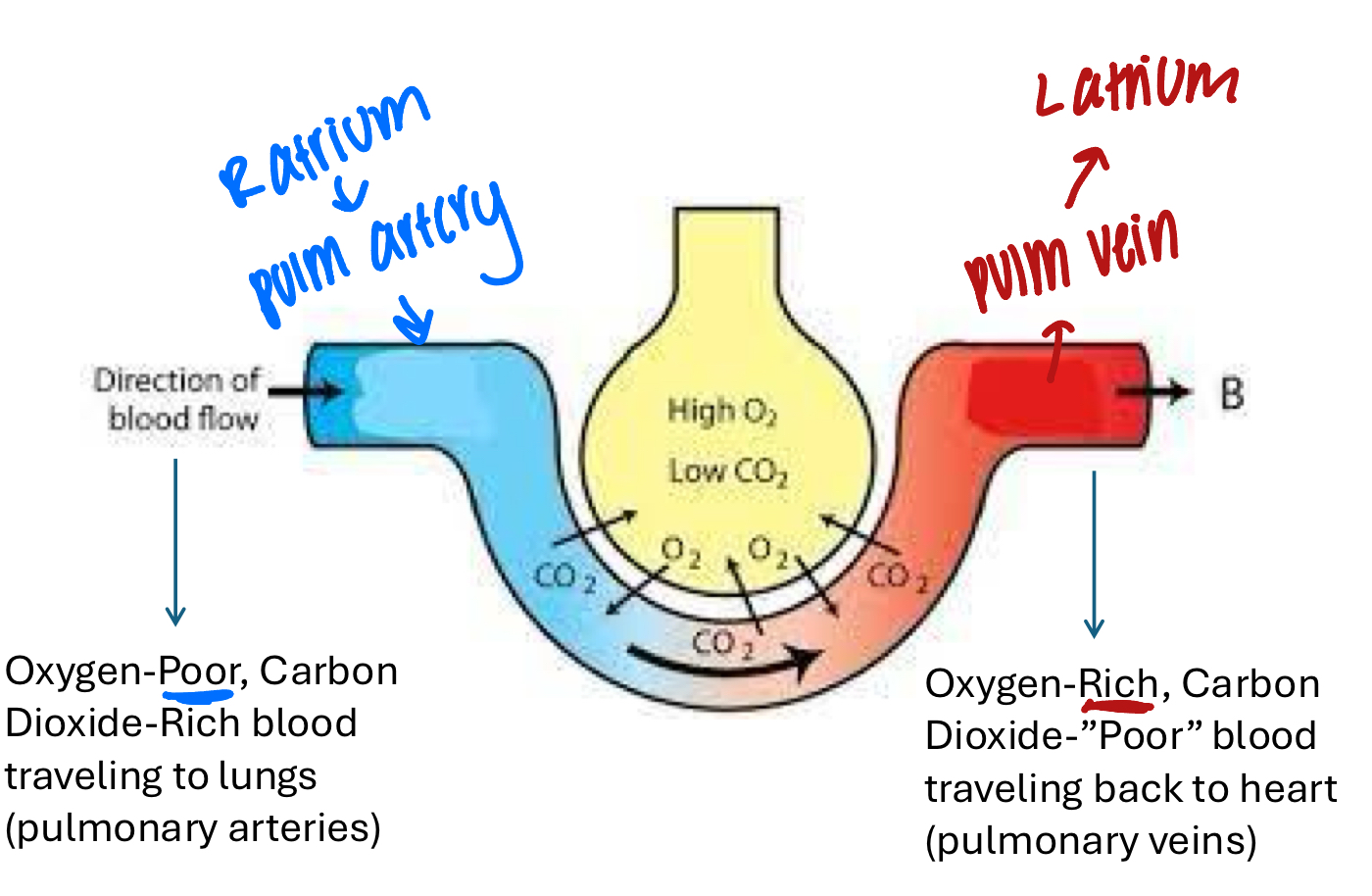
pulmonary flow
1) fresh oxygen-rich air is brought into lungs and travels to the heart via pulmonary VEINS
2) left side of the heart pumps O-rich blood to the body via ARTERIES
3) skeletal muscle uses O2 to create energy and produces CO2 as waste
4) O2-poor and CO2 rich blood enters right side of heart and is pumped to the lungs via pulmonary ARTERIES
5) pulmonary arteries release CO2 into airway for expulsion into environment
structure of respiratory system
1) conducting airways leading to the lungs; nO GAS EXCHANGE
nasal passages
pharynx
larynx
trachea
bronchi
bronchioles
2) Respiratory zone: GAS EXCHANGE
alveoli
3) respiratory muscles of chest and abdomen
components of pulmonary tree
1) conducting zone: conduct, clean, warm, filter, and humidify air
dead space: no gas exchange
2) respiratory zone: alveoli and some terminal bronchioles
pulmonary tissue interfaces pulmonary capillaries where gas exchange occurs
surface area increases→ easier diffusion
alveoli
specialized structures with very THIN walls (simple squamous epithelial) and very high surface area for the job of AIR EXCHANGE
smooth muscle surrounds terminal bronchioles
concentration of blood from pulmonary ARTERY
deoxygenated (high CO2 and low O2)
going to ALVEOLI to become oxygenated
concentration of blood from pulmonary vein
oxygenated (high O2 and low CO2)
leaving alveoli→ heart to be pumped to tissues
steps to accomplish air exchange
1) ventilation
exchange of gases btwn lungs and environment by MECHANICAL act of breathing
2) diffusion
mvmt of air btwn lungs and pulmonary capillaries
O2 diffuses down concentration gradient
3) perfusion
maintaining adequate blood supply to pulmonary capillaries
ventilation
mechanical mvmt of air or gas into and out of the lungs
minute ventilation
volume of gas inhaled or exhaled per minute
minute ventilation (L/min)= respiratory rate (RR) x tidal volume
respiratory rate
how frequnely inhale/exhale, measured in breaths per minute
“how many”
tidal volume
volume of air per breath
“how much”
alveolar ventilation rate (AVR)
RR X (TV-dead space)
volume of air moving in and out of the alveoli that is actively participating in gas exchange
how much is available for gas exchange
usually same as MV
primary ways to affect ventilation
1) affecting the RATE and DEPTH of breathing
depth increases TV
2) affecting size/diameter of airway
larger airway= < resistance, therefore more air comes through
both are under control of autonomic NS
chemoreceptors
signal respiratory center int he brain to increase or decrease RATE and DEPTH of breathing
central chemoreceptors
located in the BRAINSTEM
sense pH of CSF
peripheral chemoreceptors
locate din the AORTIC ARCH and CAROTID BODIES
sense CO2 and O2
primarily Oq in the blood
ex. detect hypoxia→ signal brain to increase resp rate and depth
what happens when a central chemoreceptor detects a pH of 7.29 on the CSF
the ventilatory rate and depth INCREASE
what happens when a peripheral chemoreceptor detects low levels of oxygen in the blood?
ventilatory rate adn depth will increase
how/why are signals sent to respiratory muscles from ANS?
via EFFERENT nerves to adjust ventilation to maintain homeostasis
effect of airway resistance on ventilation
resistance to air flow has a DIRECT effect on ventilation
resistance is determined by the diameter of the conducting airways (inverse)
larger diameter= less resistence= easier to ventilate
smaller diameter= more resistance= harder to ventilate
major site of airway resistance…
bronchi
bronchioles are surrounded by smooth muscle to allow for vasoconstriction/dilations
bronchodilation/constriction with Sympathetic nervous system
when sympathetic nervous system (fight or flight) is activated→ bronchodilation
epinephrine NT binds to BETA-2 receptors that cause dilation→ increase in air
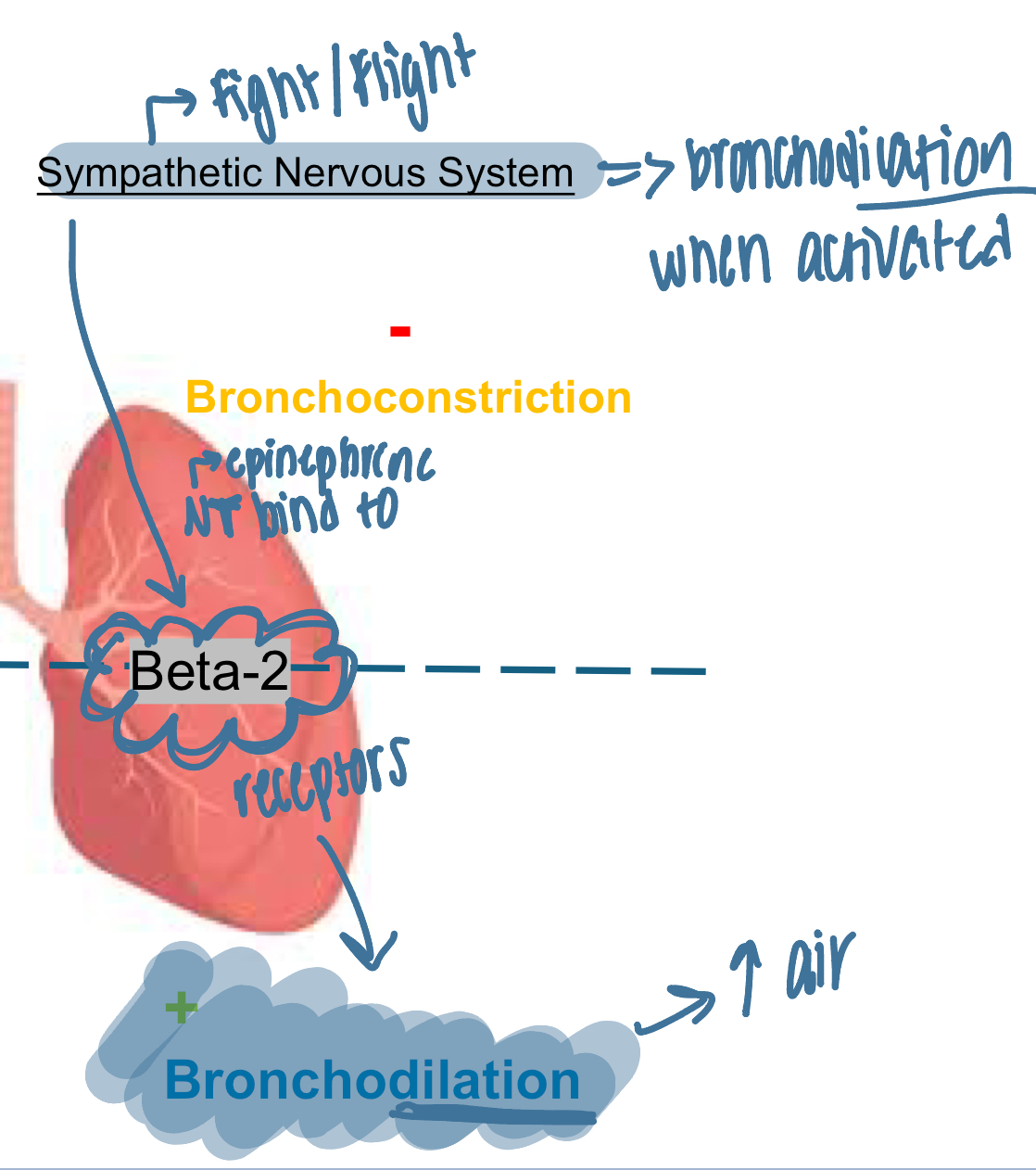
bronchodilation/constriction with Parasympathetic nervous system
resting, therefore don’t need as much air
acetylcholine binds to MUSCARINIC receptors to constrict brochioles
ex. antimuscasrinic helps with asthma to dilate
key factors that influence breathing mechanics
changes in pressure
1) respiratory muscle use
2) pleural fluid and intrapleural pressure
3) elasticity and compliance of the lungs
4) airway resistance
function of respiratory muscles
intercostals and diaphragm expand or contract to manipulate the volume of the intrathoracic space
INHALATION: diaphragm contracts (move down) and ribcage expands as rib muscles contract
increase volume and decrease pressure
EXHALATION: diaphragm releases (moves up) and rib cage gets smaller as rib muscles relax
decrease volume and increase pressure
boyle’s law
1) increasing VOLUME will decrease the pressure in the container
2) air will move from area of high pressure to low pressure
diffusion down concentration gradient
utilizing pressure gradients
intrapulmonary pressure during INHALATION= atmospheric pressure of -1
increased volume and decreased pressure inside the lungs (lower than atmospheric) therefore O2 travels down concentration gradient and into lungs
intrapulmonary pressure during EXHALATION= atmospheric pressure +1
decrease volume and increase pressure; drives O2 and gas out
muscles of inhalation
active process therefore muscles must be activated to perform inhalation
PRIMARY muscles: diaphragm and external intercostal
ACCESSORY muscles: abdominal muscles, anterior scalene, sternocleidomastoid
greatly used in instances of respiratory distress
elasticity and compliance
ELASTICITY
tendency of tissue to return to its OG change and volume
greater elasticity= greater recoil
lungs coming back “in”
COMPLIANCE
change in volume that occurs per unit change in pressure OR the ease with which an elastic structure stretches in response to pressure
lungs going “out”
more elasticity= less compliance
elastic recoil
acts as a force causing lungs to move INWARD
allow EXHALATION to be PASSIVE process under normal conditions
do not need to engage muscles due to natural elasticity
compliance
compliance of lungs and chest wall allows expansion OUTWARD resulting in ability to appropriately inspire
factors that combat lung compliance
1) elasticity of the lungs
2) surface tension of alveoli
forces act to pull lung tissue INWARD
increase in either will lead to a decrease in lung compliance/more difficult to inhale
surface tension in the airway
greater the surface tension in the airway, the more collapsed tje alveoli (less compliance)
importance of surfactant
alveoli have a thin layer of fluid/water to protect thin epithelial cells (TYPE 1 ALVEOLAR CELLS) from irritants
fluid creates surface tension
water wants to stick together, therefore pulling inward on the alveolous→ wants to collapse
surfactant: lipoprotein produced by TYPE 2 ALVEOLAR CELLS
inserts itself btwn water molecules to reduce surface tension→ makes alveoli more compliant and able to expand
clinical relevance: pulmonary fibrosis
lungs become scarred→ inhibit compliance, therefore cannot expand and cannot bring in air→ hypoxia
clinical relevance: emphysema
elastin is damaged therefore airway is schronically stretched/enlarged, therefor cannot breathe out→ increased CO2
obstructive disease
pleural space
maintain negative pressure relative to the lungs to prevent lungs collapsing inward
contains pleural fluid
lubricant to prevent friction btwn lungs and chest wall with mvmt of inhalation dn exhalation
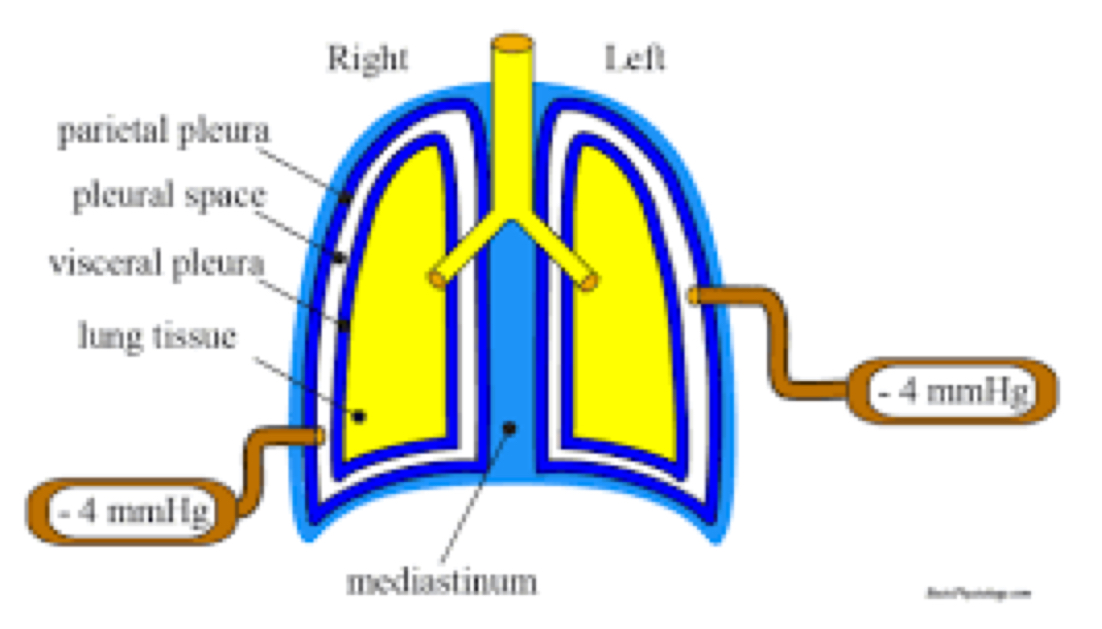
how is the intrapleural space (or pressure within pleural space) maintained negative relative to the intrapulmonary pressure?
1) elastic recoil of lungs (IN)
2) surface tension of the alveoli (IN)
3) chest wall elasticity (OUT)
Airway resistance
resistance to airflow is increased with a decrease in airway diameter
bronchoconstriction
ex. asthma: smooth muscle around bronchioles with tighten and constrict airway causing increased reistance
inflammation
ex. bronchitis or pneumonia: infected airway becomes inflamed→ decreased airway diameter
obstruction
ex. swallow foreign body
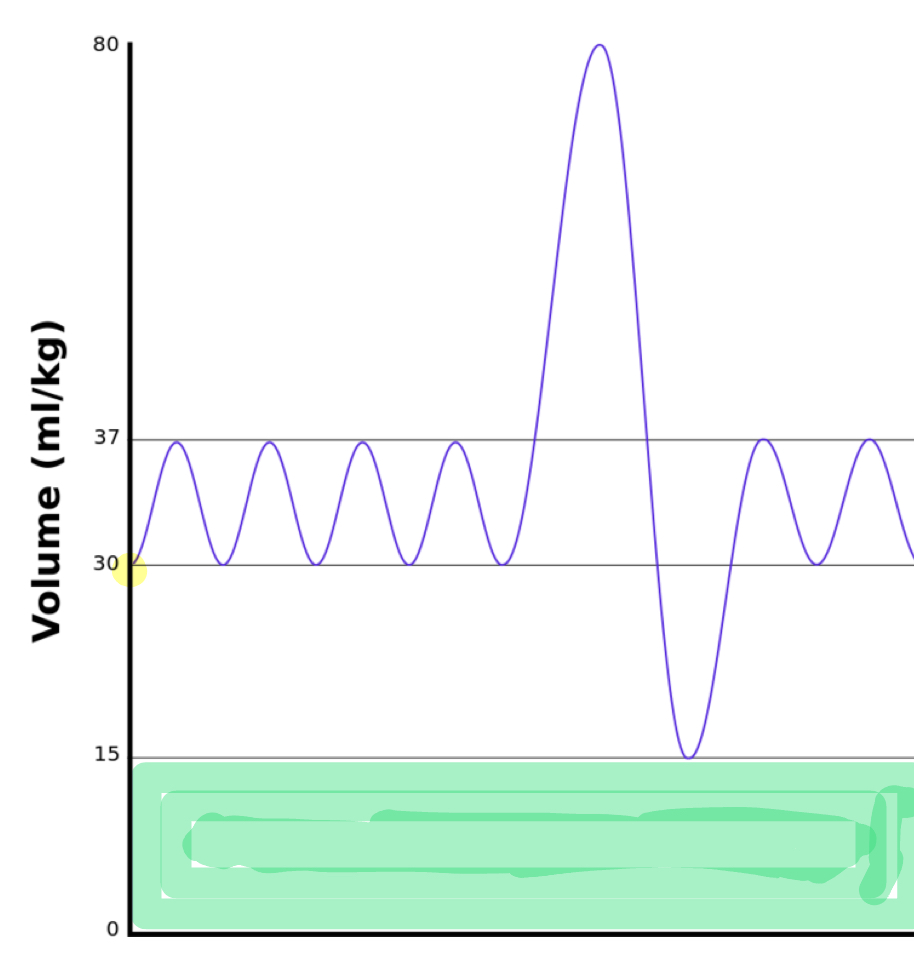
spirometry
pulmonary function test that tests ventilation ONLY
measure VOLUME and FLOW of air inhaled adn exhaled against time
useful in diagnosing different type of pulmonary diseases
restrictive vs obstructive
aspects of spirometry
tidal volume
vital capacity
residual volume
tidal volume
volume of air moving in or out with each NORMAL breath
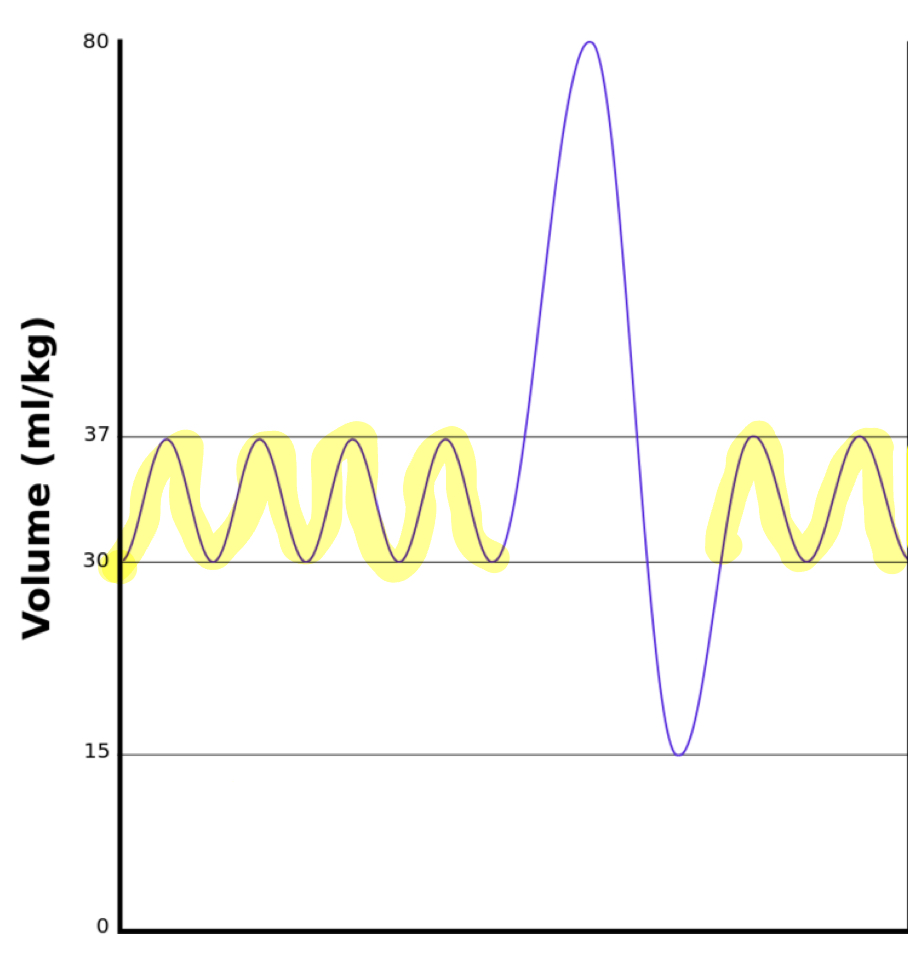
vital capacity
MAXIMUM tidal volume with DEEPEST inhale and exhale
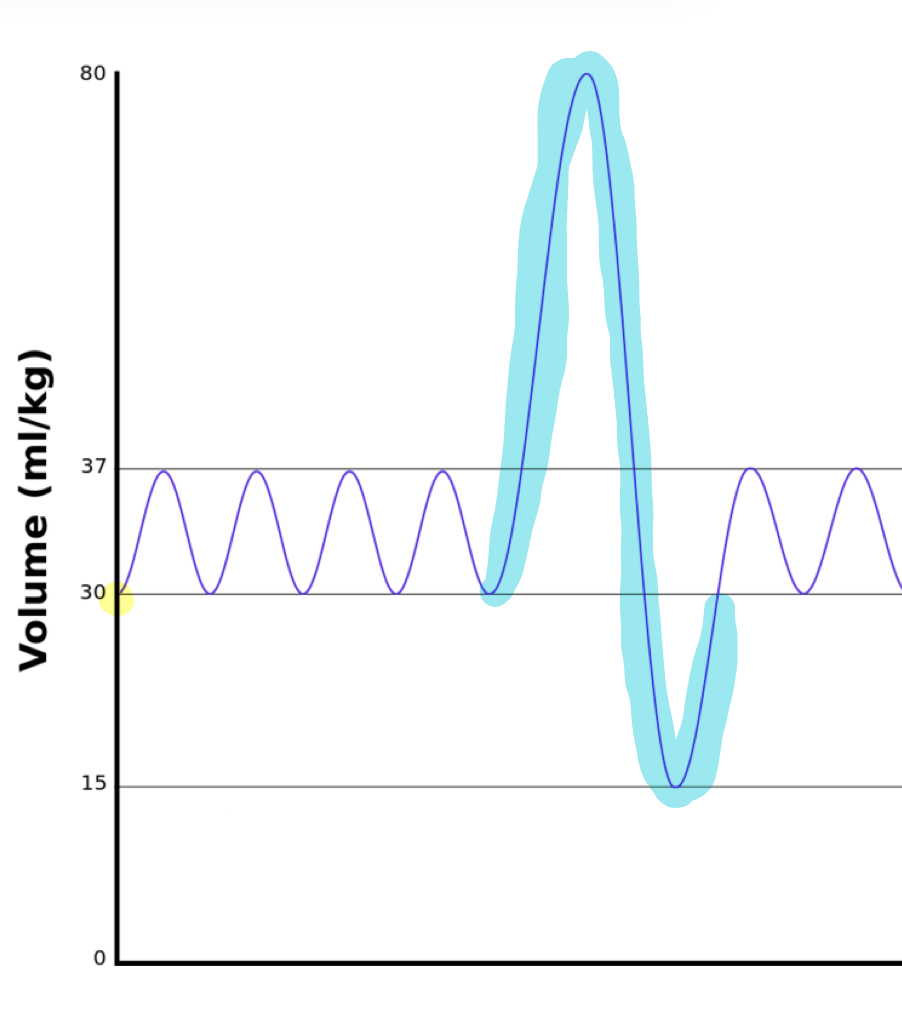
residual volume
the amoutn of air REMAINING IN THE ALVEOLI after max exhalation
keeps alveoli from complete collapse
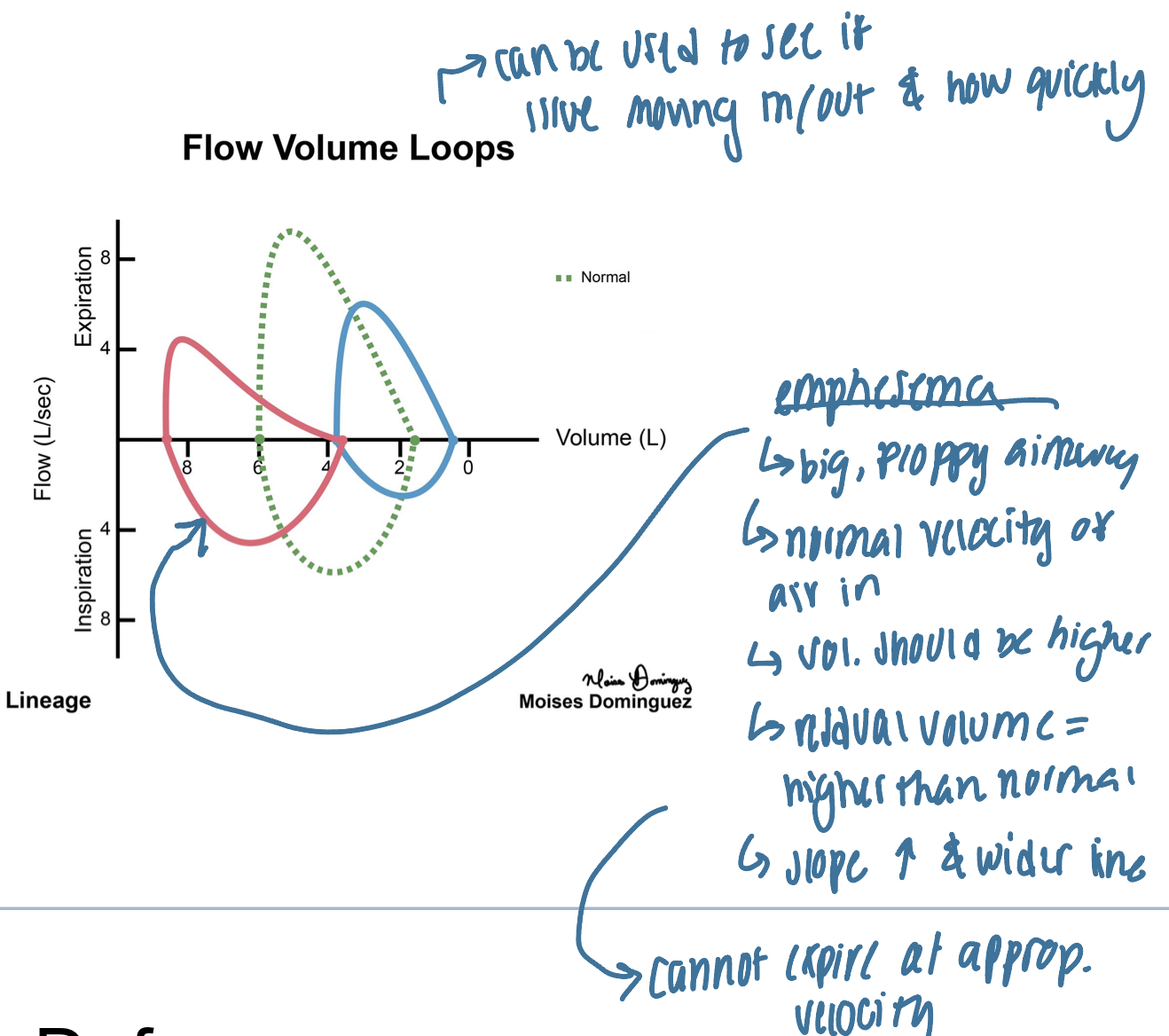
flow volume looops
traces velocity of air mvmt and volume of lungs through max inhalation adn exhalation
changes in VELOCITY can indicate INCREASED airway resistance or elastic recoil
slows air mvmt (in or out)
changes in VOLUME can indicate DECREASED compliance, elastic recoil, or increased airway resistance
cannot fully inhale or exhale
why is the airway a potential route of infection for pathogens?
it is in constant contact with external environment
irritant receptors
epithelium of conducting airways
sensitive to noxious (pollen, dust, bacteria, etc)→ stimulate cough
cough reflex
protective reflex that helps clear airways by explosive exhalation—closing off; decreasing volume and increase pressure→ open and expel irritant
inhalation
closure of glottis
exhalation muscle contraction
abdominal muscles
opening of glottis→ expel irritant
can be stimulated by higher brian (voluntary( or reflex pulmonary irritant stimulation
what is the goal of the mucociliary escalator?
protect the sensitive thin-walled tissue of the alveoli that are vital fro gas exchange
muscociliary escalator
epithelial lining of bronchi contains:
goblet cells and mucus glands
goblet cells: trap irritants/pathogens
cilia:hairlike projections that move mucus
up and out”
alveoli defenses
1) alveolar macrophages
highly prevalent
engulf pathogens
initiate adaptive immune response
stimulate inflammation
2) surfactant
bacteriostatic properties
limit bacterial growth/proliferation
perfusion
bring blood to lungs and out to the body
diffusion
mvmt of molecules (CO2 and O2) across alveolar membrane
process of diffusion
1) O2 will diffuse DOWN it’s concentration gradient from the alveoli to the vasculature (PULM VEIN)
2) CO2 will diffuse down it’s concentration gradient form the vasculature into the alveoli (from PULM ARTERY)
respiratory membrane
*where gas exchange via diffusion occurs
site of EXTERNAL RESPIRATION
contains:
type 1 alveolar cells
thin connective tissue
capillary wall
diffusion is optimized due to small area
external respiration
mvmt of O2 and CO2 across the respiratory membrane
O2: moves into cap
inhaled air as high PO2
deoxygenated blood in pulm ARTERIAL capillaries have LOW PO2
CO2: moves into alveoli
deoxygenated blood in pulm ARTERIAL capillaries have HIGH CO2
inhaled air has LOW CO2
partial pressure of oxygen (PO2) in blood from heart and system circ
low; 40mmHg
partial pressure of oxygen (PO2) from fresh air
high; 100mmHg
pressure gradient for oxygen btwn alveolar air and deoxygenated blood is …..
~60mmHg
what factors impact the process of diffusion?
1) surface area of membrane
2) MAGNITUDE of partial pressure gradient
larger=increase drive of diffusion
3) thickness of semi-permeable membrane
4) solubility of gas (CONSTANT)
O2 and CO2 must move through thin layer of alveolar fluid, interstitial fldid, and plasma
CO2 is 20x more soluble than O2
lower magnitude of change due to higher solubility
why administer oxygen therapy to patients with hypoxia?
to manipulate the pressure gradient at the alveolocapillary membrane
improved diffusion due to increased magnitude
internal respiration
mvmt of O2 and CO2 btwn TISSUES and systemic capillaries
CO2: CO2 moves out of tissues into blood (VEINS)
systemic arterial cap have low CO2
tissue cells have HIGH CO2
oxygen: O2 moves into cells of tissue (from arteries)
systemic arterial cap have HIGH PO2
tissue cells have low PO2
oxygen-hemoglobin dissociation curve
heme affinity for oxygen changes depending on environment:
1) O2 rich-> heme binds O2 more readily
2) O2 poor→ heme releases O2 more readily
O2 rich environment (high PO2)
heme grabs and HOLDS on to as much O2 as possible when available and tissues are not demanding
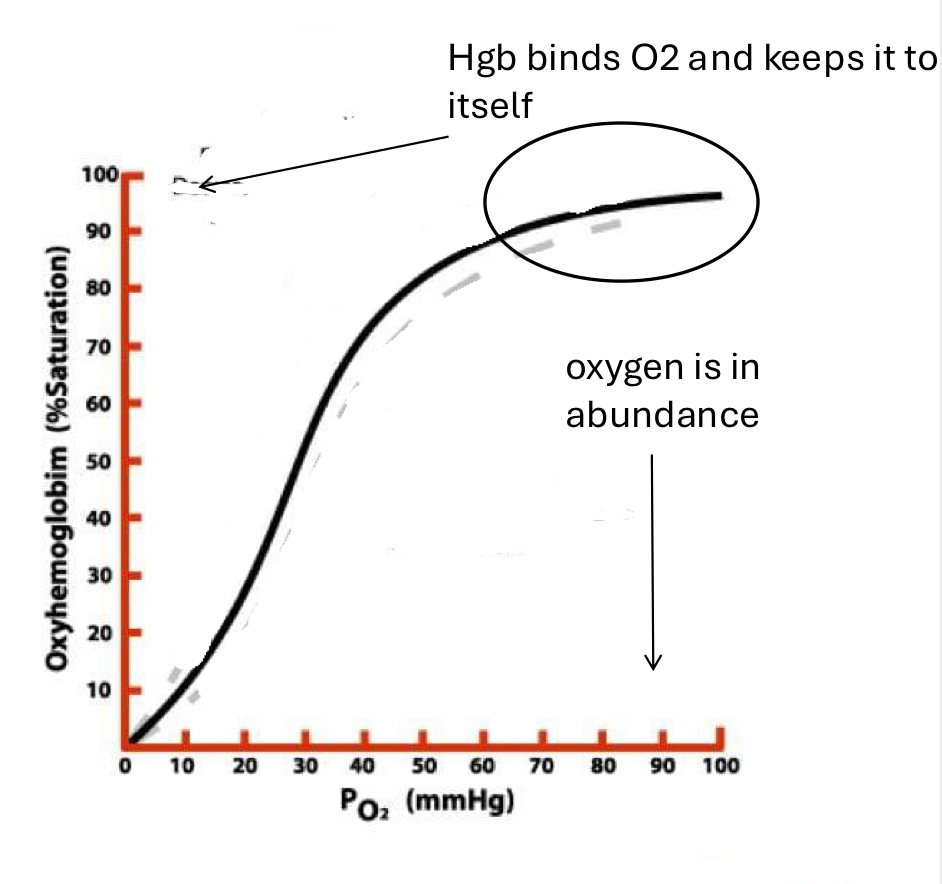
why does heme bind/release oxygens based on environemnt?
cooperative/allosteric binding
when O2 binds one subunit→ conformational change in adjacent peptide subunits to make them have HIGHER affinity for O2 binding → adjacent subunit changes shape and now binds O2 with higher sffinity, etc
O2 poor environment (low PO2)
hemem readily gives up O2 to the tissue that need it
decrease in cooperative binding due to low conc of O2
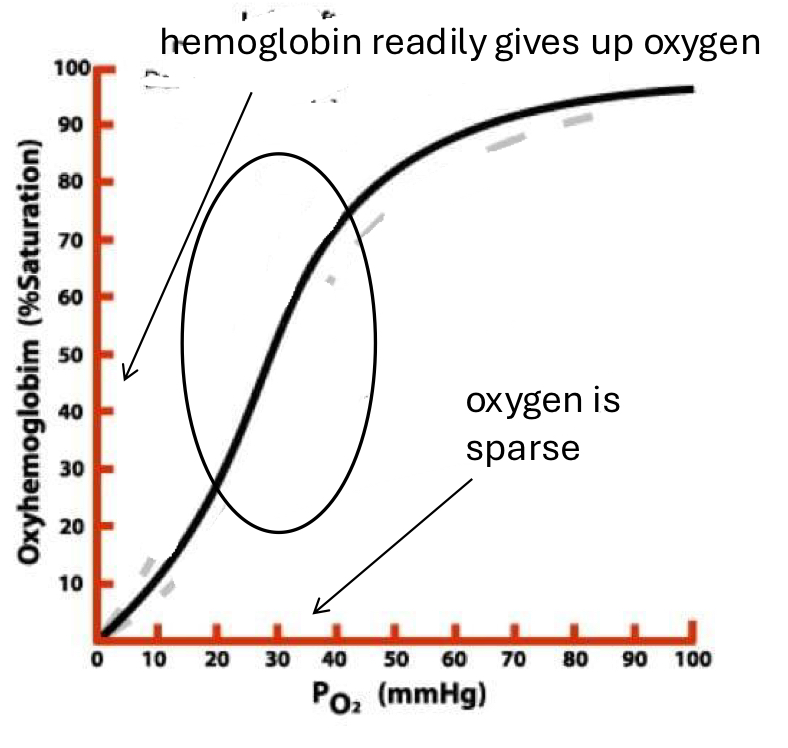
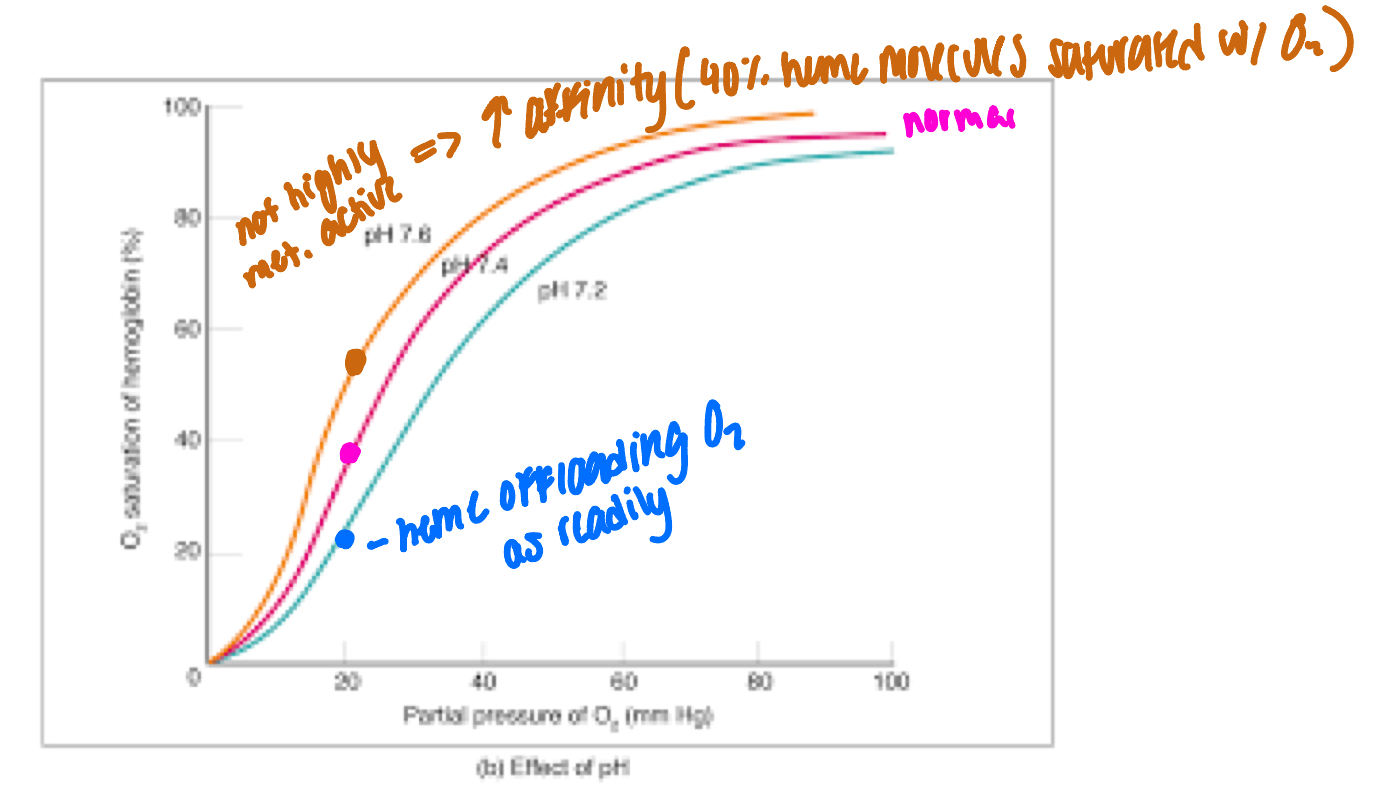
why does increase in CO2 decrease affinity for O2
CO2 as a product→ decreased Ph (more acidic)→ decrease affinity for O2
right shift
factors that cause LEFT shift in heme-O2 curve
INCREASED afffinity for O2
1) decr. pCO2
2) decr. [H+]
3) decr temp
4) HbF
factors that cause RIGHT shift in heme-O2 curve
DECREASED affinity for O2
1) incr pCO2
2) incr [H+]\incr temp
pH effect on heme conformation
H rich environments (low pH) heme molecules will bidn O2 with LOWER affinity
metabolically active tissues (which prod more CO2), heme is more likely to drop off O2 and deliver to tissue
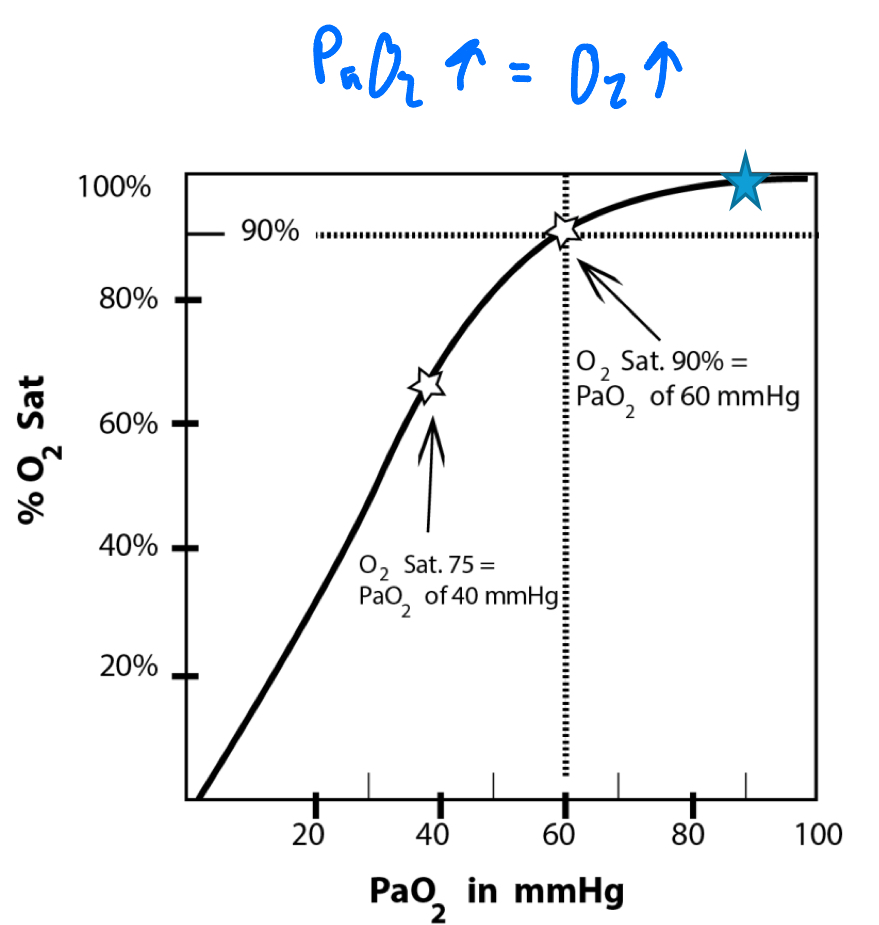
PaO2
actual O2 content in arterial blood
only small amnt and invasive procedure that only gives quick snapshot
O2 saturation (SPO2)
percent o fheme binding to sites in blood that are carrying O2
cons: if decreased heme (anemic), O2 carryign capacity is cut, therefor all heme will try to adhere to more O2→ false high saturation
relationship btwn PaO2 and O2 sat
PaO2 of 70-90 is normal
correlates with O2 sat ~90%
direct correlation: incr PaO2=incr O2
what influences perfusion?
1) CARDIAC OUTPUT
vol of blood pumped by heart per minute
R ventricle feeds pulmonary ARTERY circulation
2) pulmonary vessel diameter
pulm vasoconstriction/dialtion
dilation: INCR perfusion
constriction: DECR in perfusion
what major process can be manipulated by the body for appropriate oxygenation
ventilation and perfusion
ventilation-perfusion matching
vent and perf both require energy adn effort
waste of energy to vent area with poor perf and vice versa
goal= MATCH vent and perf
avoid wasting energy and maximize gas exchange
matching vent and perf
ratio of Vent/perf shoud be ~1
V-how much air into lung
Q- how much blood into air space
V/Q=1
vent and perf ratio
flow of O2 into alveoli (vent) is almost equal to the flow of deoxygenated blood ip the alveolar cap
vent and perf mismatch
1) area receiving O2 well (vent well) but the blood flow through the capillary is decreased (not perf well)— V/Q>1
ex. PE→ not enough vent
2) areas receiving adequate blood flow (perfusing well) but isnt bringing enough O2 to the alveoli (vent poorly)- V/Q<1
matching V/Q: increased AVR
increased AVR (V=6L.min)
V/Q=6/5=1.2
wasted air mvmt
how keep matched?
Incr AVR=incr PpO2
O2 diffusing across resp membrane stimulates N2O prod by capillaruy endothelial cell
N2O causes smooth muscle to RELAX→ vasoDIALITON→ incr perfusion
matching V/Q: hypoxic pulm vasoconstriciton
poorly ventilated alveolus
V/Q=3/5=0.6
wasted perfusion
how keep matched?
decr AVR=decr PO2
decreased O2 diffusing across resp membrane suppresses N2O prod
absence of N2) causes smootj musclecontraction/CONSTRICTION
decrease perf
pulm adaptations: acid-base balance
immediate responder to acid/base disorders to regulate pH
pH=[HCO3-]/[CO2]
pt is in respiratory failure and cannot properly exhale CO2 rich air into the environment. WHat is the effect on pH?
decrease/become more acidic
RESPIRATORY ACIDOSIS
pt hyperventilating and expiring immense amnts of CO2 into atmosphere. What is the effect on pH?
increase pH/more basic
RESPIRATORY ALKALOSIS
pt is in renal failure and cannot properly re-absorb HCO3- effectively in the kidneys? what is the effect on pH?
decrease in pH/more acidic
METABOLIC ACIDOSIS
pulm response to acidosis
acidosis = LOW pH
how fix?—incr CO2 exhalation
chemoreceptors (brainstem and aorta/carpotsi) detect low pH
resp center of brainstem proccesses afferent signals, triggers:
INCR depth o ventilation
INCR resp rate
pulm response to alkalosis
alkalosis= HIGH pH
how do we fix? incr CO2
chemoreceptors detect high pH
proccess afferent signals, triggers
decr depth of vent
der resp rate