(BIO 120) Chp 4 Slides Prokaryotic Cells
1/75
Earn XP
Description and Tags
In progress
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
Prokaryotes are mainly divided into 2 domains:
Bacteria
Archaea
Bacteria v.s. Archaea
Similarities
They both have…
Unicellular
Circular DNA in a nucleoid (DNA is not enclosed in a nucelus)
70S ribosomes
Reproduce by binary fission
May have flagella, plasmids, and cell walls
Differences
Feature | Bacteria | Archaea |
|---|---|---|
Cell Wall | Most have peptidoglycan (murein). | No peptidoglycan; may have pseudopeptidoglycan, proteins, or polysaccharides. |
Membrane Lipids | Fatty acids linked to glycerol by ester bonds. | Ether bonds link branched isoprenoid chains to glycerol → more stable in extremes. |
Ribosomes | 70S, sensitive to antibiotics like streptomycin and chloramphenicol. | 70S, but proteins and rRNA more similar to eukaryotes. Not affected by many bacterial antibiotics. |
RNA Polymerase | One simple type. | Multiple complex types (similar to eukaryotic RNA polymerases). |
Genetic Organization | No introns (mostly). | Some genes have introns (like eukaryotes). |
Environment | Found almost everywhere (soil, water, inside hosts). | Often extremophiles: halophiles (salt), thermophiles (heat), acidophiles (acid), methanogens (anaerobic). |
Pathogenicity | Many pathogenic species (e.g., E. coli, Salmonella, S. aureus). | No known human pathogens. |
Examples | Escherichia coli, Staphylococcus aureus, Mycobacterium tuberculosis. | Halobacterium (salt-loving), Methanobrevibacter (methane-producing), Sulfolobus (acid-thermophile). |
T or F: Prokaryotic cells ALWAYS have a cell wall.
False.
Most prokaryotic cells have cell wall, but some don’t (e.g. mycoplasmas).
(a) What are ribosomes?
(b) Compare ribosomes in prokaryotic cells v.s. eukaryotic cells.
(a) Ribosomes:
non-membrane-bound organelles responsible for protein synthesis
found in all cells (but structurally diff b/w prokaryotes & eukaryotes)
(b) prokaryotic cells v.s. eukaryotic cells
Feature | Prokaryotic Ribosomes | Eukaryotic Ribosomes |
|---|---|---|
Size | 70S (made of 50S + 30S subunits) | 80S (made of 60S + 40S subunits) |
Location | Free-floating in cytoplasm | Free in cytoplasm or attached to rough ER |
Complexity | Smaller, simpler | Larger, more complex |
Function | Protein synthesis | Protein synthesis |
Antibiotic Sensitivity | Targeted by antibiotics like erythromycin | Not affected by these antibiotics |
Q: Why can antibiotics target prokaryotic ribosomes without harming human cells?
A: Because prokaryotic ribosomes are smaller (70S) and structurally different from eukaryotic ribosomes, making them a selective target for antibiotics.
Genetically, which prokaryote — archaea or bacteria — is close to eukaryotes than the other prokaryote.
Genetically, archaea are closer to eukaryotes than to bacteria, even though both are prokaryotic in structure.
Q: What is the role of prokaryotic ribosomes in treating bacterial infections?
A: Antibiotics can bind to prokaryotic ribosomes and inhibit protein synthesis, helping eliminate bacterial infections without affecting human cells.
Q: Where are eukaryotic ribosomes located, and how does this affect protein production?
A: Eukaryotic ribosomes may be free in the cytoplasm or bound to the rough endoplasmic reticulum, allowing for compartmentalized and specialized protein production.
________ are highly diverse and medically important because many are pathogens.
Bacteria are highly diverse and medically important because many are pathogens.
________ are unique biochemically, adapted to extreme environments, and provide clues about early life on Earth.
Archaea are unique biochemically, adapted to extreme environments, and provide clues about early life on Earth.
Prokaryotes reproduced by ______________.
Prokaryotes reproduced by binary fission.
Another term for “binary fission” is “__________________” or “__________________”.
Another term for “binary fission” is “asexual reproduction” or “cell division”.
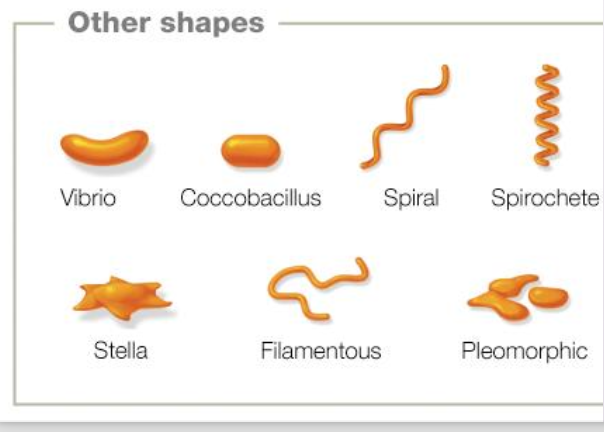
Pleomorphism
describes bacterial species that has variability in shape
these bacteria can adapt shape to survive environmental stressors
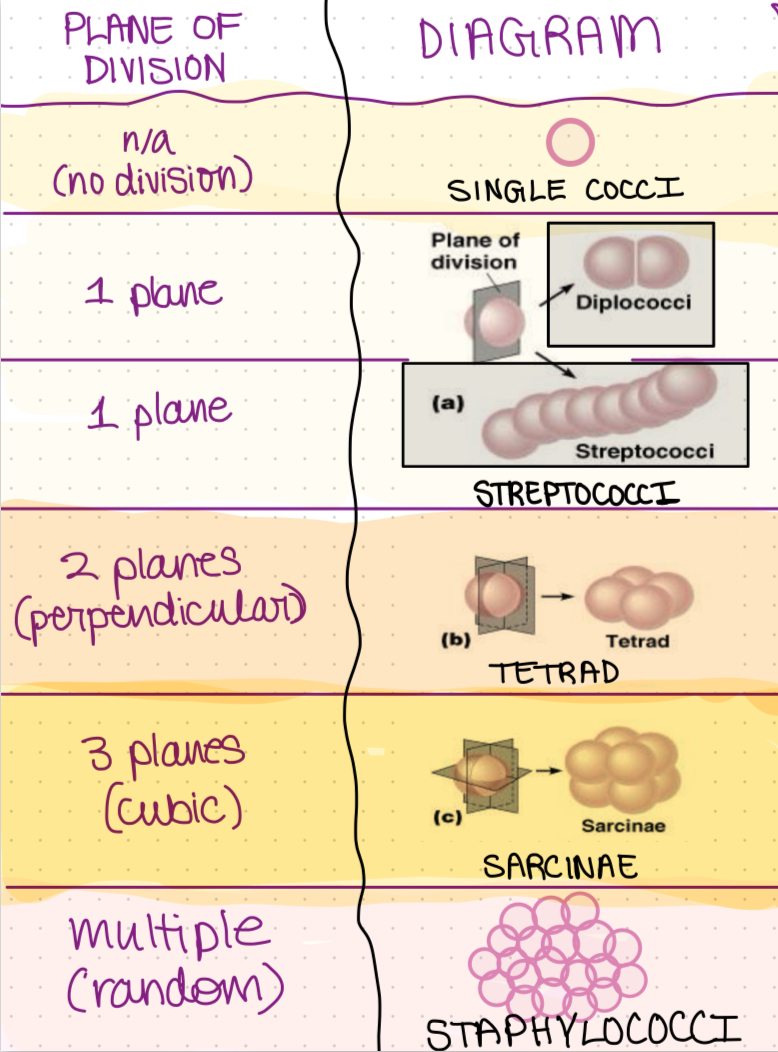
Name & describe the various arrangements on coccus-shaped prokaryotes.
Name & describe the arrangements on bacillus-shaped prokaryotes.
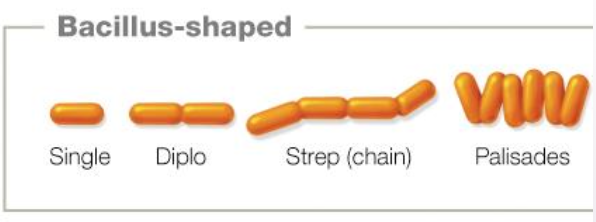
Bacilli (rods) divide in one plane and then can separate.
Sinle bacci
Diplobacci — two bacilli
Streptobacci — chain of bacilli
Palisades (less common) — rods lined up parallel or at sharp angles due to snapping division of the bacilli
Coccobacillus — A very short, oval rod that looks like a “fat bacillus” or an elongated coccus.
Appears intermediate between cocci and bacilli under the microscope.
Shape: plump, oval rods.
Arrangement: Usually occur singly, sometimes in pairs.
Size: Shorter than typical bacilli, but not perfectly round like cocci.
“coccobacillus” literally means coccus-like bacillus.
🔹 Examples of Coccobacilli
Haemophilus influenzae → causes meningitis, pneumonia.
Bordetella pertussis → causes whooping cough.
Brucella species → cause brucellosis (zoonotic infection).
Chlamydia trachomatis → obligate intracellular coccobacillus.
🔹 Clinical Relevance
Many pathogenic bacteria are coccobacilli.
Because they are hard to classify at first glance (not purely cocci or bacilli), lab tests like Gram stain, culture, and molecular methods are important for identification.
Name & describe the irregular prokaryotic shapes.
Q: Which Gram-positive cocci appear lancet-shaped and in pairs, and are commonly associated with pneumonia?
A: Streptococcus pneumoniae — Gram-positive, lancet-shaped cocci in pairs, often seen in respiratory infections like pneumonia.

Q: What Gram-negative diplococci are typically found within white blood cells in urethral discharge and are linked to sexually transmitted infections?
A: Neisseria gonorrhoeae — Gram-negative diplococci, often located inside or near white blood cells, associated with gonorrhea.
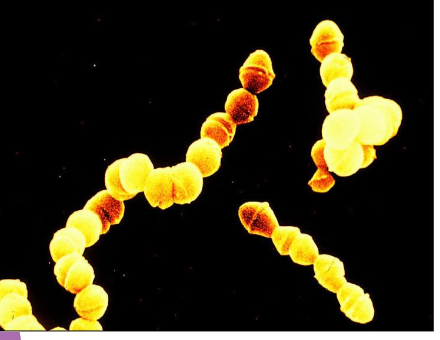
What type of shape & arrangement is this?
Streptococci
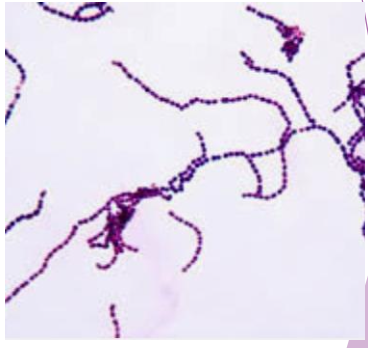
What type of shape & arrangement is this?
Streptococci
Streptococcus pyogenes is also called “____________”.
Streptococcus pyogenes is also called “Step Group A”.
Name 2 examples bacterial species that are cocci.
Streptococcus pyogenes (Strep group A)
Staphylococcus aureus
Neisseria gonorrhoeae
Streptococcus pyogenes
also called “Step Group A”
gram-positive bacteria
appears as cocci arranged in chains
causes —> pharyngitis (strep throat)
major symptom: “strawberry throat” — sore throat w/ red & swollen tonsils
can progress into scarlet fever if bacteria produces erythrogenic toxin
these toxins produce immune reaction that presents as red cheeks & rash
Streptococcus pyogenes
Description (shape, arrangement, gram+/-)
Diseases & symptoms
Significance
Also called “Step Group A”
Description
Shape: Cocci (spherical)
Arrangement: Chains
Gram-positive
Diseases it causes & symptoms
pharyngitis (strep throat)
can progress into —> scarlet fever if bacteria produces erythrogenic toxin
these toxins produce immune reaction that presents as red cheeks, red tongue, rash
if untreated —> rheumatic heart fever (RHF) which is leading cause of heart disease in children worldwide
Significance
Can lead to systemic complications if untreated.
Streptococcus aureus folliculitis
Description (shape, arrangement, gram+/-)
Diseases, symptoms, treatment, prevention
Significance
Description
Shape: Cocci (spherical)
Arrangement: Chains
Gram-positive
Diseases it causes & symptoms
Bacterial infection of hair follicles
Symptoms:
small red bumps
pustules/bumps
shaving bumps
Treatment:
mild cases —> warm compresses
severe cases —> topical & oral antibiotics/ointments
Prevention:
good hygiene
handwashing
Significance
Opportunistic pathogen
resistant strains (MRSA) cause healthcare-associated infections.
Stye
Cause
Symptoms
Treatment
Cause: Staphylococcus aureus on eyelid
What: infected/inflamed skin gland or hair follicle
Symptoms:
small painful bump on eye
redenss
swelling
tenderness
Treatment:
most cases —> condition resolves on its own w/ warm compression
severe cases —> antibiotics
Neisseria gonorrhoeae
Description (shape, arrangement, gram+/-)
Diseases, symptoms, treatment, prevention
Significance
Description
Shape: Cocci (spherical)
Arrangement: Chains
Gram-positive
Diseases it causes & symptoms
Bacterial infection of hair follicles
Symptoms:
small red bumps
pustules/bumps
shaving bumps
Treatment:
mild cases —> warm compresses
severe cases —> topical & oral antibiotics/ointments
Prevention:
good hygiene
handwashing
_______ divide in one plane, then can separate.
Bacilli divide in one plane, then can separate.
Cocci can divide in different planes (meaning _________) and how they divide determines their _________.
Cocci can divide in different planes (meaning directions) and how they divide determines their arrangement.
_____ is spherical bacteria.
Cocci is spherical bacteria.
If cocci divide in one plane —> they line up in a ______, called __________.
If cocci divide in one plane —> they line up in a chain, called streptococcus.
If cocci divide in two planes —> they form __________, called ________.
If cocci divide in two planes —> they form groups of 4, called tetrads.
If cocci divide in three planes —> they form _________________, called ________.
If cocci divide in three planes —> they form cube-like packets of 8, called sarcinae.
If cocci divide in many random planes —> they form _________________, called ____________.
If cocci divide in many random planes —> they form grape-like clusters, called staphylococcus.
(“staphylo” = cluster).
T or F: Streptococcus pyogenes are cocci in chains.
True.
Staphylococcus aureus → cocci in _________ (____ plane division).
Staphylococcus aureus → cocci in clusters (many plane division).
T or F: Unlike cocci, bacilli usually divide in one plane.
True. Results in arrangements of singles, pairs, or chains.
Coccobacilli belongs to which group of bacterial shapes?
Coccobacilli is considered part of bacilli group.
___________ is the leading cause of food-borne illnesses, hospitalizations, and deaths.
Salmonella is the leading cause of food-borne illnesses, hospitalizations, and deaths.
Salmonella
Pathogen
Transmission
Symptoms
Significance
Pathogen
Salmonella enterica
Gram-negative
Transmission
Contaminated food or water
Contact with fecal matter
Commonly associated w/ poultry & eggs
Reptiles, especially pet turtles
Symptoms
Moderate fever
Abdominal cramps
Diarrhea
Nausea
Possible septicemia (blood poisoning) —> when the bacteria enters the bloodstream
Significance
Leading cause of foodborne illness → important in food safety.
What is the normal habitat of Salmonella?
GI tract in animals/humans, but is always pathogenic to humans
What is the incubation time for Salmonella? Why is this significant?
Incubation time ~12-35 hours —> long bc bacteria needs to invade intestinal mucosa before multiplying there
T or F: Salmonella is an opportunistic pathogen.
Not classified as opportunistic, but some strains cause disease more severely and more frequently in vulnerable hosts
Can also invade bloodstream, especially in immunocompromised, very young, or elderly individuals
What foods should especially avoided in order to prevent Salmonella infection? Explain why.
Poultry & raw eggs
Even whole eggs can be infected bc Salmonella can be transmitted into them by chickens before they are laid (transovarian transmission)
So foods like mayonnaise or egg nog that contain raw eggs are risky to eat
Incubation Time
Refers to period b/w ingestion of pathogen & onset of symptoms
Curved bacilli are called _____.
Curved bacilli are called vibrio.
Name & briefly describe the main bacterial shapes.
Provide example of bacteria for each.
(1) Cocci
spherical
e.g. Streptococcus pyogenes (strep throat)
(2) Bacilli
includes cocobacilli
elongated rod-shape
Example —> Escherichia coli (normal gut flora, but also a pathogen)
(3) Spirillum/Spirochete (spiral-shaped)
Description: Curved, helical, or corkscrew-like; motile with flagella or axial filaments.
Example —> Treponema pallidum (causes syphilis)
(4) Vibrio: curved bacilli-shape
e.g. Vibrio (curved rod, comma-shaped): Vibrio cholerae – causes cholera.
(5) Coccobacilli
short, oval-shaped rod, between cocci and bacilli
Example—> Haemophilus influenzae – can cause respiratory infections and meningitis.
Sometimes bacilli and curved (i.e. spiral shapes like vibrio). Their ______ and _____________ determines what they are called.
Sometimes bacilli and curved (i.e. spiral shapes like vibrio). Their length and stiffness determines what they are called.
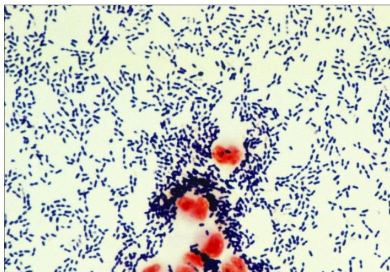
Vibrio cholerae
Shape
Transmission
Symptoms
Significance
Describe its shape.
What symptoms does it cause?
Mortality rate?
Treatment?
Pathogen
comma-shaped rod w/ single flagellum
Symptoms
vomiting
copious watery feces, “rice-water stool”
severe cases —> fluid loss of 1 litre/hr (severe dehydration)
Mortality Rate: 55% to 70%
Treatment
Oral-rehydration therapy
Significance: Flagella + toxin enable rapid colonization and fluid loss; oral rehydration therapy critical.
What is in this image?

Vibrio cholerae
The Two Major Groups of Appendages
Major Groups
Flagella & Axial Filaments —> Provide Motility
Fimbriae, pili, nanowires —> Provide attachment points or channels
Classification of Prokaryotic Cells
Unicellular → each organism is a single cell.
Peptidoglycan cell wall → provides strength and prevents osmotic lysis.
No membrane-bound organelles → DNA is free in cytoplasm (nucleoid).
Morphological diversity → shapes and arrangements aid in identification.
Divide by binary fission → rapid population growth.
Significance: Simple structure allows adaptability, rapid evolution, and survival in diverse environments.
T or F: Shape and arrangement of bacteria may relate to pathogenic mechanisms.
True.
For example, clusters are able to resist phagocytosis.
Pleomorphic translated means “____________”. It’s used to describe prokaryotes without a ________.
Pleomorphic translated means “many-formed”. It’s used to describe prokaryotes without a cell wall.
Flagella
Function
Structure
Arrangement Types
Movement Types
Example
Significance
Function: motility (movement); can also aid in attachment.
Arrangement Types:
Polar —> flagella attached at one or both ends of cell
The following 3 are all considered polar arrangements:
monotrichous —> single flagellum at one end
amphitrichous —> single flagella at both ends
lophotrichous —> tuft of multiple flagella at one end
Peritrichous —> flagella dispersed randomly over surface of cell
Movement Types:
Runs: Smooth forward motion
Tumbles: Random changes in direction
Example: Campylobacter jejuni uses flagella to burrow into intestinal mucus.
Significance: Motility enhances invasion and colonization.
Chemotaxis
Movement of flagella in response to chemical signals (toward nutrients or away from toxins)
Fimbriae
Function
Structure
Example
Significance
Structure: Short, numerous, hair-like structures (protein-based)
Function: Attachment/adhesion
Help bacteria stick to surfaces, host cells, and each other
Crucial for forming biofilms (communities of bacteria on surfaces)
Contribute to pathogenicity by allowing bacteria to colonize host tissues
Example: E. coli and Neisseria gonorrhoeae require fimbriae to infect.
Significance: Essential for colonization; without them → reduced pathogenicity.
Pili
Structure
Function
Significance
Pili (Sex Pili)
Structure:
Long, rigid, tubular projections.
Fewer in number (1–2 per cell).
Longer than fimbriae.
Functions:
Attachment (limited role, minor surface adhesion).
Conjugation (horizontal gene transfer / bacterial sex):
Form a bridge between two bacteria.
Transfer plasmids (small circular DNA).
Spread genetic traits such as antibiotic resistance and virulence factors.
Significance:
Critical for bacterial evolution and adaptation.
Major mechanism by which resistance genes spread through bacterial populations.
How is flagella related to pathogenicity?
Allow bacteria to invade tissues by moving through mucus or fluids
Help bacteria escape immune responses by changing direction
Some pathogens use flagella to reach target cells (e.g., Helicobacter pylori uses flagella to burrow into stomach lining)
How is fimbriae related to pathogenicity?
Essential for initial attachment to host cells
Without fimbriae, many bacteria can't colonize or cause infection
Example: Neisseria gonorrhoeae uses fimbriae to attach to urogenital tract cells
How is pili related to pathogenicity?
Conjugation pili allow bacteria to share virulence genes
This can increase a population’s ability to cause disease
Also play a role in adhesion, though less than fimbriae
Surface Coatings: Glycocalyx
Slime layer – loose, protects from drying and nutrient loss.
Capsule – dense, thick layer; prevents phagocytosis and aids in adhesion.
Example: Streptococcus pneumoniae → capsule is its main virulence factor.
Significance: Encapsulation makes bacteria more virulent and harder to clear.
Biofilms – communities attached to surfaces, encased in glycocalyx.
Found on teeth (plaque), catheters, implants.
Significance: Protect bacteria from immune system & antibiotics.
Function of Cell Wall & Envelope
Functions:
Maintains shape, prevents osmotic lysis, protects from host defenses.
Determines Gram reaction → critical for identification and treatment.
Gram+ bacteria
Thick peptidoglycan, teichoic acids, exotoxin production.
Sensitive to penicillin and lysozyme.
Significance: Simpler structure makes them more vulnerable to certain antibiotics.
Gram– bacteria:
Thin peptidoglycan, outer membrane with LPS (endotoxin).
Barrier to antibiotics and detergents.
Significance: Outer membrane contributes to antibiotic resistance and immune evasion.
Plasma Membrane
selective barrier
site of transport
enzyme activity
ATP production
Cytoplasm
site of metabolism
contains enzymes
cytoskeleton for shape
Nucleoid
houses DNA
controls cell function & growth
Plasmids
extra DNA
carry virulence or resistance genes
ribosomes (70S)
perform protein synthesis by translating genetic instructions provided by plasmids into proteins
target for some antibiotics (e.g. tetracyclines)
Endospores
Produced by Gram+ Bacillus & Clostridium.
Trigger: nutrient depletion (C, N).
Extremely resistant to heat, freezing, radiation, disinfectants.
Sporulation → dormancy; Germination → return to vegetative state.
Example: Clostridium difficile → healthcare-associated diarrhea.
Significance: Hard to eradicate; important in hospital infection control & food sterilization.
Q: What is bacterial conjugation and why is it important?
Conjugation = DNA transfer between bacteria via pili (sex pilus).
Transfers plasmids (extra-chromosomal DNA).
Often carries genes for antibiotic resistance or virulence.
A form of horizontal gene transfer (not reproduction).
Significance: Major contributor to rapid bacterial evolution and spread of resistance.
What is the structure and function of the prokaryotic plasma membrane?
Structure: Phospholipid bilayer (fluid mosaic), proteins (enzymes, transporters, receptors).
Functions:
Selective barrier → regulates nutrient/waste/gas exchange.
Site of ATP production (no mitochondria in prokaryotes).
Houses enzymes for metabolism.
Damage: Alcohols, disinfectants, and antibiotics can disrupt it → leakage and cell death.
Significance: Essential for survival; key antibiotic target.
Q: What is the prokaryotic cell envelope and why is it important?
Layers:
Cell wall (peptidoglycan).
Cytoplasmic membrane.
Outer membrane (Gram– only).
Gram+ bacteria:
Thick peptidoglycan, teichoic acids, exotoxin producers, penicillin-sensitive.
Gram– bacteria:
Thin peptidoglycan, outer membrane with LPS (endotoxin), resistant to many antibiotics.
Significance:
Protects cell from osmotic lysis.
Determines Gram stain reaction (diagnosis/antibiotic choice).
Virulence factor (LPS/endotoxin in Gram– bacteria).
Q: What is a PPD test and what does it indicate?
PPD (purified protein derivative) test = tuberculin skin test.
Small injection under skin → read 48–72 hours later.
Positive test = person exposed to Mycobacterium tuberculosis.
Indicates either latent TB infection or active TB disease (requires further testing).
Significance: Screening tool for TB; identifies infected individuals before symptoms progress.
Q: What is a biofilm and why is it clinically significant?
Biofilm = community of bacteria attached to a surface, embedded in glycocalyx (slime/capsule).
Formation: Attachment → growth → secretion of protective extracellular matrix.
Examples: Dental plaque, catheter/implant infections.
Advantages for bacteria:
Protection from antibiotics, disinfectants, and immune cells.
Allows communication & genetic exchange between cells.
Significance:
Major source of chronic, hard-to-treat infections.
Common cause of healthcare-associated infections.