Biology II Lesson 4: Kidney Regulation Part II
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
Do alpha-intercalated cells or beta-intercalated cells try to hold on to acids (protons)?
Beta-intercalated cells try to hold on to acids (lower blood pH), while alpha-intercalated cells try to get rid of acids (elevate blood pH).
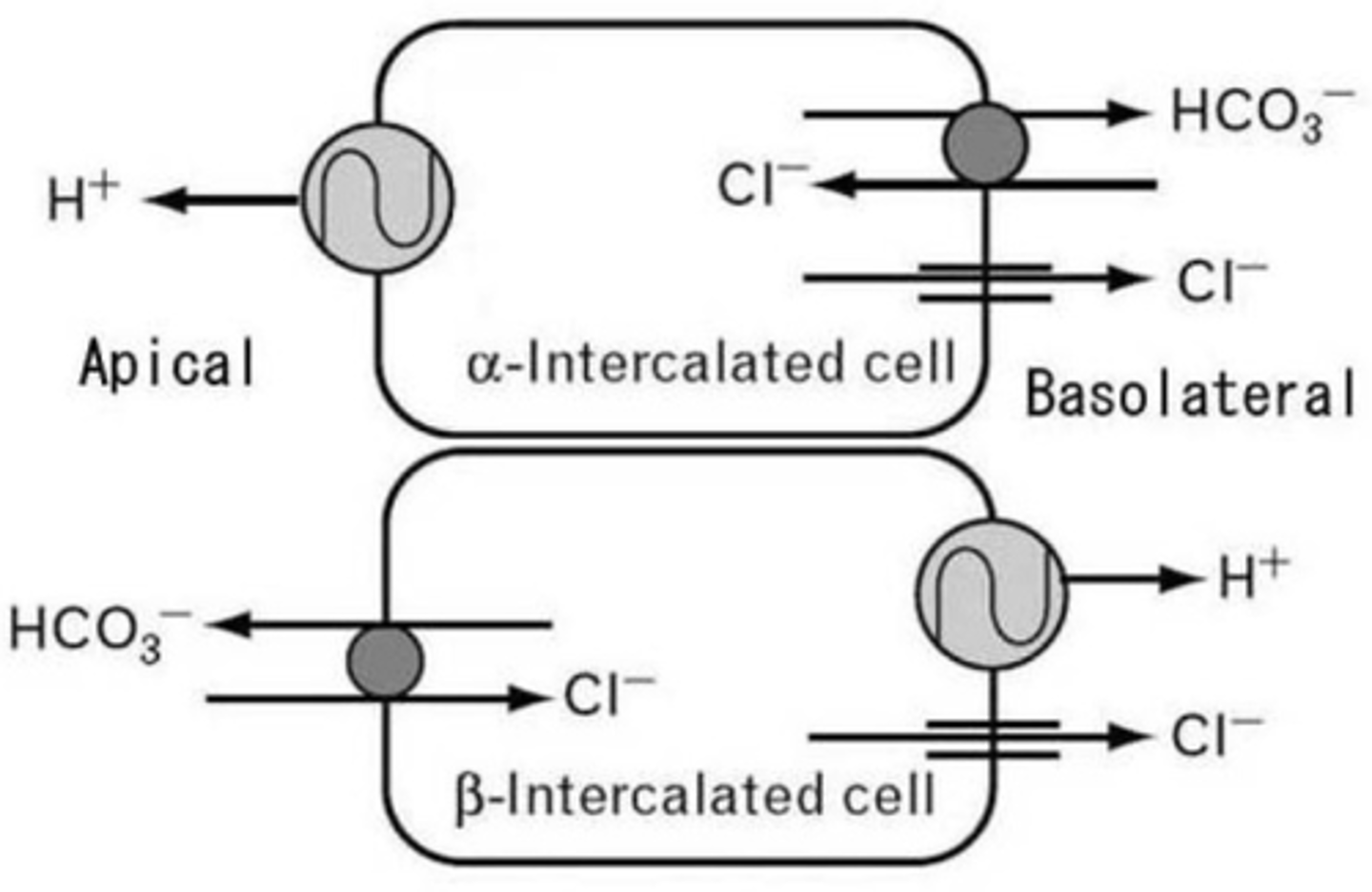
In the basolateral surface of an alpha-intercalated cell and a peritubular capillary there is a transporter that transports chloride into that cell in exchange for which of the following molecules into the interstitium (leading to absorption by the capillary)? Why does this make sense considering the role of an alpha-intercalated cell?
(A) HCO3-
(B) H+
(C) H2CO3
(D) K+
(A) HCO3-
Cl- is transported into the alpha-intercalated cell while HCO3- is transported into the capillary via the interstitium. Because HCO3- is a base, it will increase the pH of the blood.
In the bloodstream, bicarbonate will cause the formation of which of the following products?
I. CO2
II. H2O
III. H+
(A) III only
(B) II only
(C) I and II only
(D) I and III only
(C) I and II only
HCO3- will combine with a proton to form CO2 and water.
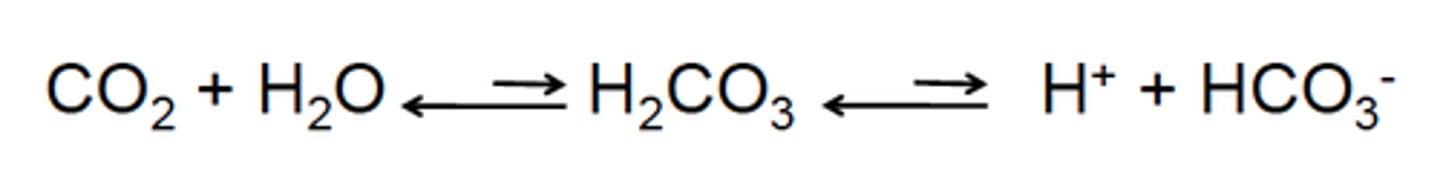
CRB Adding Bicarbonate to the Bloodstream to increase H2O and CO2 is an example of what general chemistry principle? Then apply that principle to this example.
(A) Aufbau's Principle
(B) Le Chatelier's Principle
(C) Hund's Rule
(D) Henderson-Hasselbalch Principle
(B) Le Chatelier's Principle
Le Chatelier's Principle is that when you add a stress to one side of the equilibrium, then the system will compensate to relieve that stress. By adding more HCO3-, the equilibrium is stressed, and some is converted to H2O and CO2 to relieve that stress.
CRB To reinforce the Bicarbonate Buffer System, draw out the Bicarbonate Buffer System Equilibrium.
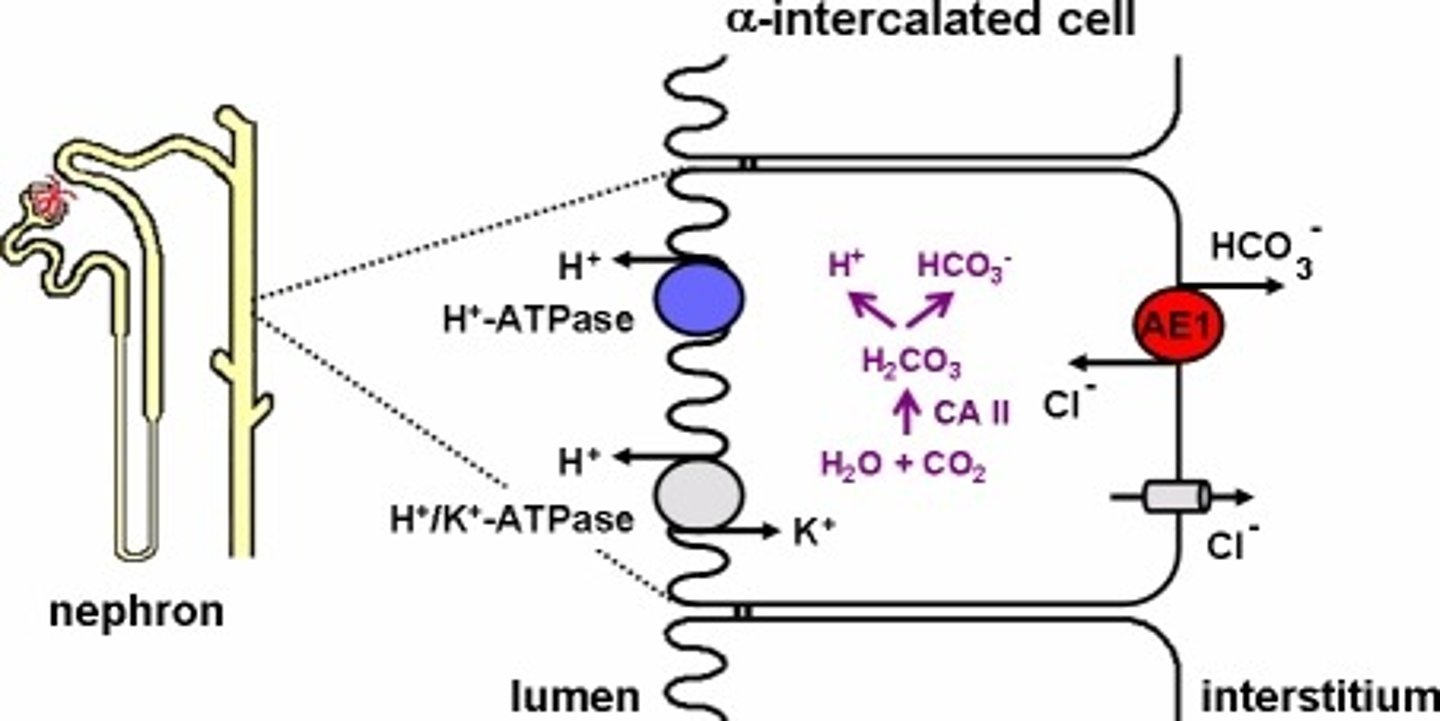
CRB In which of the following places would you expect to find lots of Carbonic Anhydrase, which can catalyze reactions in the Bicarbonate Buffer System?
I. Red Blood Cells
II. Epithelial cells in Nephron
III. Alpha-Cells in the Pancreas
(A) I only
(B) I and II only
(C) II and III only
(D) I, II and III
(B) I and II only
I would expect to find lots of Carbonic Anhydrase in the Red Blood Cells and in the Epithelial cells in Nephron.
In the apical surface of the alpha-intercalated cell, there are a variety of transporters for pumping which of the following ions into the nephron for excretion? Why does this make sense considering the role of an alpha-intercalated cell?
(A) HCO3-
(B) H+
(C) H2CO3
(D) K+
(B) H+
This will decrease the concentration of H+ in the body, raising the pH of the blood.
CRB Which of the following can the kidney selectively increase or decrease, depending on the pH of the blood?
(A) H+
(B) HCO3-
(C) Both A and B
(D) Neither A nor B
(C) Both A and B
Both H+ and HCO3- can be selectively increased or decreased by the kidney to return to homeostasis.
CRB Compared to the respiratory response to altered blood pH levels, how fast is the Renal response to pH levels?
(A) Slower than the respiratory response.
(B) The same speed as the respiratory response.
(C) Faster than the respiratory response.
(D) This depends on where the affected blood is.
(A) Slower than the respiratory response.
The respiratory response is faster than the renal response to changes in pH.
Does aldosterone inhibit or enhance the acid-removing function of the alpha-intercalated cell?
Aldosterone enhances the acid acid-removing function of the alpha-intercalated cell.
ADH is also known as:
(A) Vasopressin
(B) Vasorelaxin
(C) Hydropressin
(D) Hydrorelaxin
(A) Vasopressin
ADH is also known as vasopressin because it increased blood pressure via the vasoconstriction of blood vessels.
ADH is released from the anterior or posterior pituitary?
ADH is released from the posterior pituitary.
Which of the following trigger the release of ADH from the pituitary gland?
I. Increased Blood Osmolarity
II. Increased Blood Volume
III. Increased Blood Pressure
(A) I Only
(B) II Only
(C) I and II Only
(D) I and III Only
(A) I Only
The triggers of ADH release are as follows:
- Increased blood osmolarity (increased number of dissolved particles in the blood).
- DECREASED blood volume.
- DECREASED blood pressure.
- Also remember that angiotensin II will trigger the release of ADH.
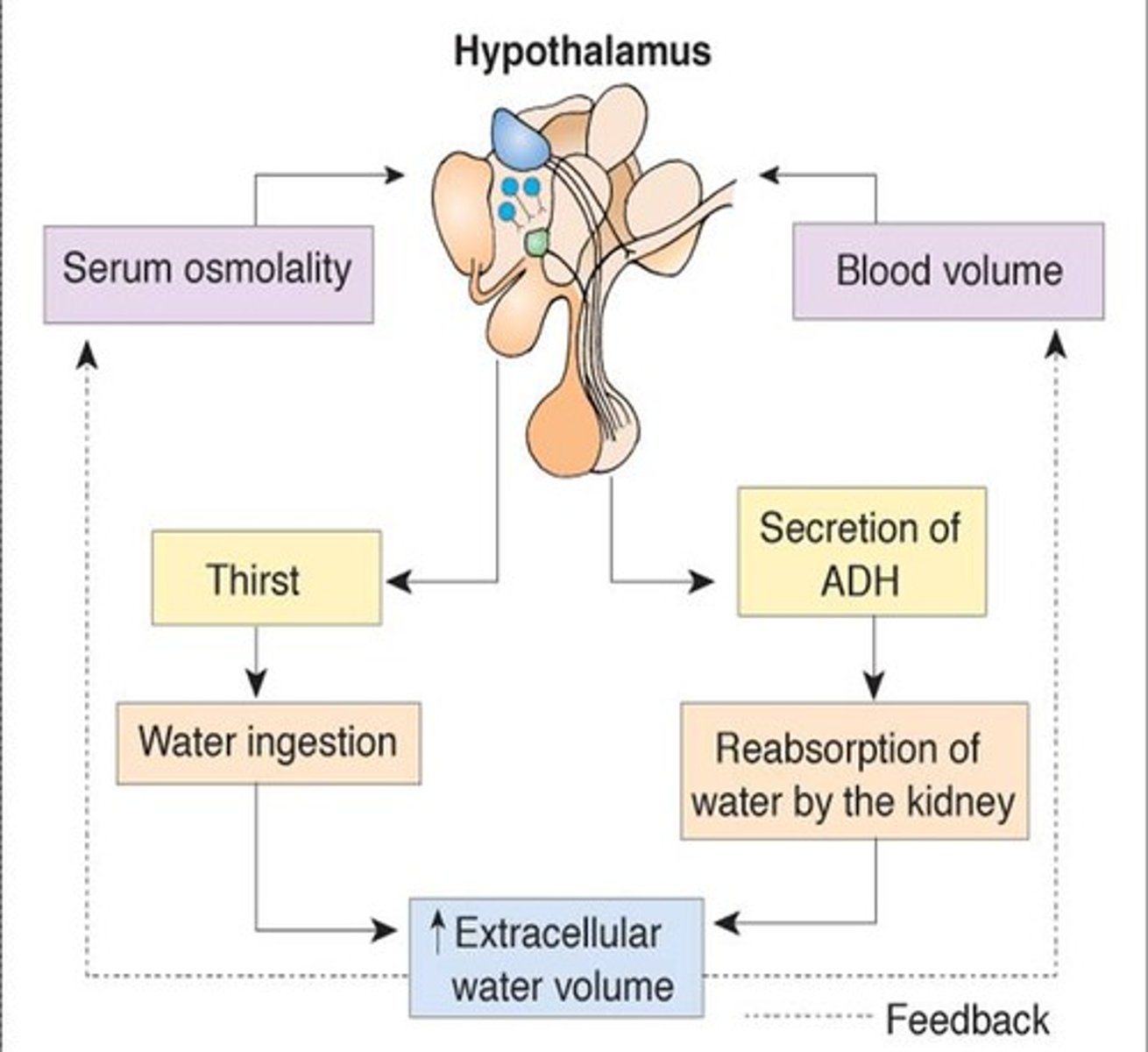
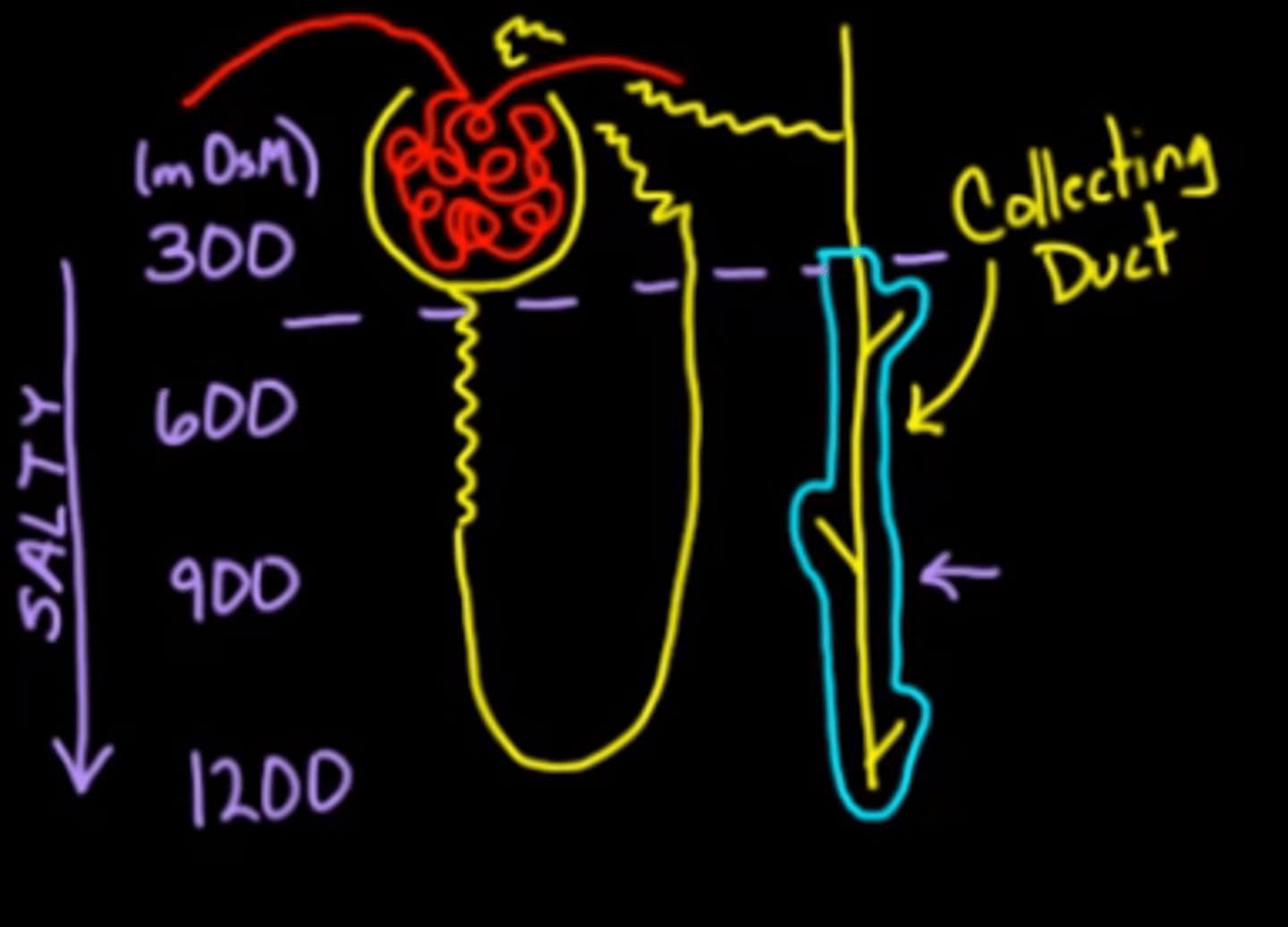
What is the role of the collecting duct and how is that role enhanced by increasing osmolarity as the collecting duct dives deeper and deeper into the medula of the kidney?
The role of the collecting duct is to concentrate our urine (increase the solute-to-water ratio). The increasing osmolarity of the medulla serves to pull more and more water out of the filtrate, concentrating it.
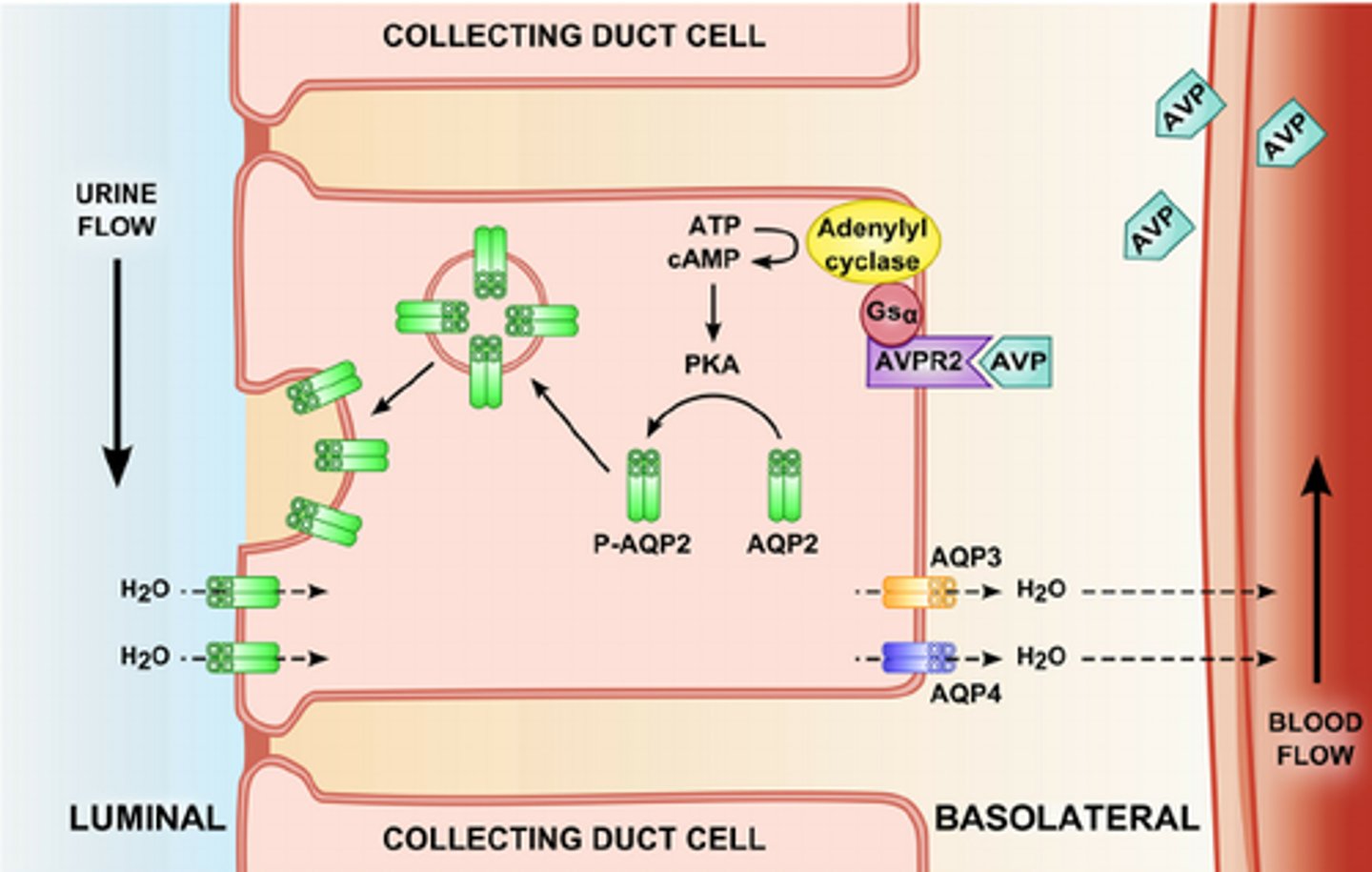
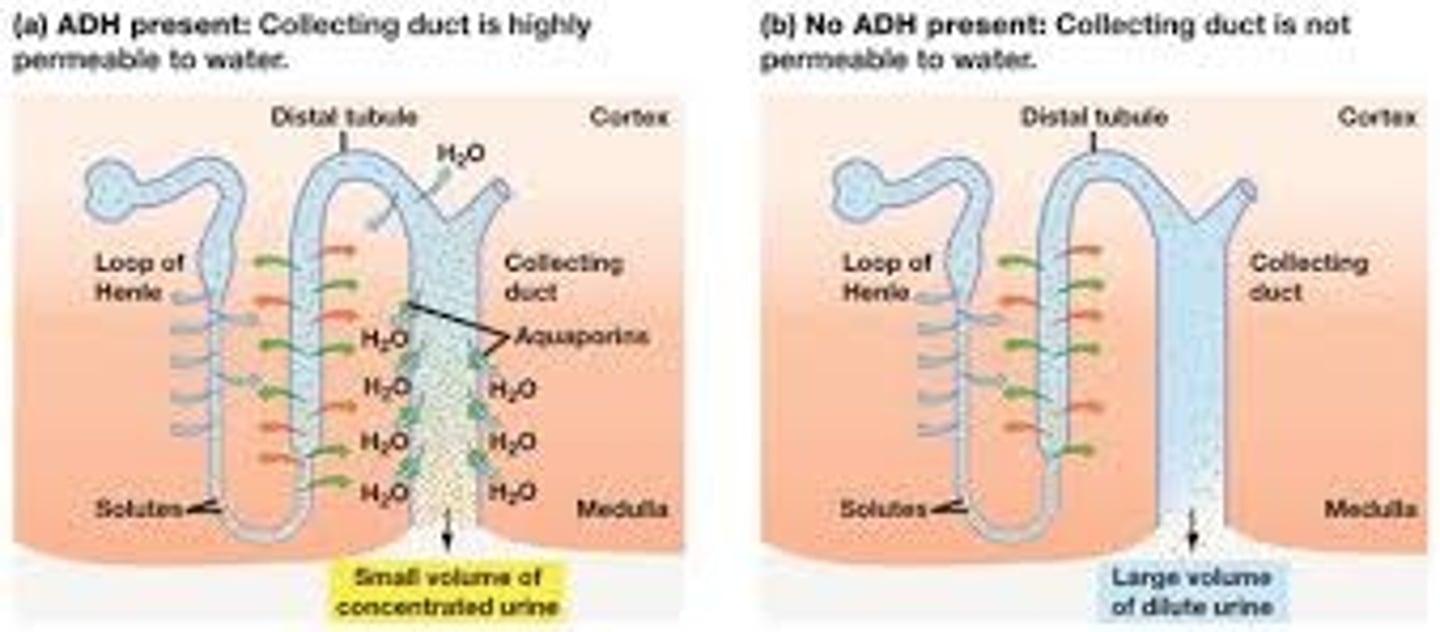
What is aquaporin and how does it relate to ADH?
Aquaporins are water channels located in the cells of the collecting duct. ADH causes the aquaporins to fuse with the apical surface, increasing the number of water channels pumping water out of the collecting duct.
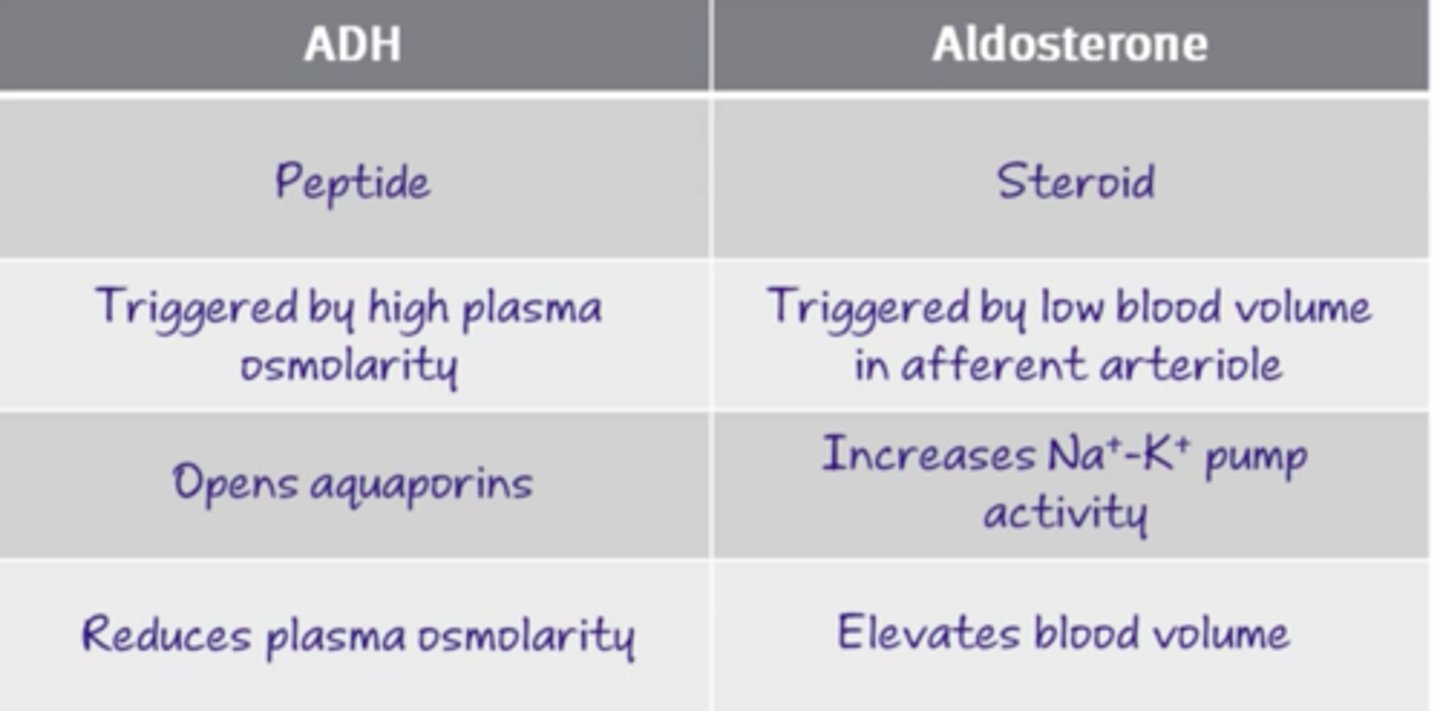
Aldosterone and ADH work on different parts of the nephron. Which hormone works on a water permeable membrane?
Aldosterone works on the water permeable membrane part of the nephron. Aldosterone increases the reabsorption of Na+, which results in the passive diffusion of water back into the bloodstream.
ADH is specifically working in areas that are not permeable to water. It works by increasing the number of water channels in the apical surface, enabling water to get reabsorbed.
Between aldosterone and ADH, they both increase the amount of water being reabsorbed, but which one changes the osmolarity?
ADH changes the osmolarity since only the water is being reabsorbed; thus, the solute-to-water ratio will decrease, lowering the osmotic pressure of the blood.
In contrast, aldosterone increases the reabsorption of both sodium and water; thus, the solute-to-water ratio will remain unchanged, leaving the osmotic pressure of the blood the same.
If your body needed to increase the blood volume while maintaining the blood osmolarity, how would your body regulate the concentrations of aldosterone and ADH?
If your body needed to increase the blood volume while maintaining the blood osmolarity, it would secrete aldosterone and not ADH.
If your body needed to increase the blood volume regardless of the blood osmolarity, how would your body regulate the concentrations of aldosterone and ADH?
If your body needed to increase the blood volume regardless of the blood osmolarity, it would secrete both.
If your body needed to increase the blood osmolarity while maintaining the blood volume, how would your body regulate the concentrations of aldosterone and ADH?
If your body needed to increase the blood osmolarity while maintaining the blood volume, it would increase Aldosterone secretion and accordingly decrease ADH secretion to maintain the blood volume.
If your body needed to increase the blood osmolarity regardless of the blood volume, how would your body regulate the concentrations of aldosterone and ADH?
If your body needed to increase the blood osmolarity regardless of the blood volume, it would not affect the secretion of aldosterone and drastically decrease the secretion of ADH.