Block 3B - Gynecological Cancers (Vulva, Vaginal)
1/102
Earn XP
Description and Tags
ONCOL 310 - Clinical Oncology II. University of Alberta
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
103 Terms
vulva cancer epidemiology
___% of all cancers diagnosed in women
__ cases per 100 000
____ cases per 100 000 over age of 75
incidence is higher in ______
1% of all cancers diagnosed in women
2.5 cases per 100 000
15.5 cases per 100 000 over age of 75
incidence is higher in white women than black
what is the exact cause of vulva cancer
unknown
etiological factors of vulva cancer
increasing age, HPV, smoking, weakened immune system, precancerous conditions, skin conditions of vulva
what is the precursor condition to vulvar cancer
vulvar intraepithelial neoplasia (VIN)
what are the two most common histologies of vulva cancer
90% SCC
5% melanoma
others indlude adenocarcinoma, sarcomas, basal cell carcinoma
what are the two most common sites of vulva cancer
labia majora and minora
what features of vulva cancer are associated with nodal metastasis
tumor thickness, histologic grade, depth of invasion, location of tumor, tumor size
where can vulva cancer spread locally?
Along the vulva and perineum, Urethra, Vagina, Anus , Bladder, Rectum
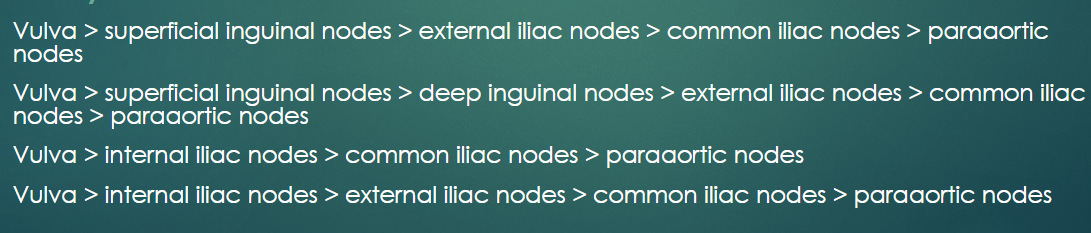
what are the two primary LN involved in vulva cancer
superficial inguinal nodes and internal iliac nodes
what are the three most common metastatic sites of vulva cancer
liver, lung, bone
rare, later, and will occur after LN involvement
how will vulva cancer present clinically?
pruritus, soreness, burning, tingling sensation or pain in the vulva
Wart-like growths, thickened skin, or lumps on the vulva or on either side of the opening to the vagina
Raw patches or ulcers, fluid leaking out from growth
Changes in the appearance of a mole on the vulva
Unusual bleeding or discharge that is not menstruation
Pain during urination or sexual intercourse
One or more swollen or hard lymph nodes in the groin
what is done during a physical exam when diagnosing vulva cancer
Feel uterus, ovaries, cervix, and vagina for anything irregular. Doctor will also look at vagina and cervix and may do a Pap test and an HPV test.
what biopsy is done if abnormal area is small? large area?
small area = excisional biopsy
large area = punch biopsy
what imaging tests can be done to diagnose vulva cancer
Chest X-ray
CT
MRI
PET
Ultrasound +/- FNAC (fine-needle aspiration cytology)
Referral to gynecologic oncologist
what is the most important prognostic indicator of vulva cancer
stage
earlier = more favourable
other prognostic indicators of vulva cancer
Tumour size , Tumour volume, Local extent
Pathology
SCC most favourable
Grade
Spread to lymph nodes
Location of the tumour
Symptoms
Women who present with symptoms = less favourable
Age & General health (younger women better outlook than >60 yrs + good health)
Hysterectomy status
Studies have shown an advantage for earlier hysterectomy
Stage I Vulva Cancer
Tumor confined to the vulva
IA—Tumor size ≤ 2 cm and stromal invasion ≤ 1 mm *
IB—Tumor size > 2 cm or stromal invasion > 1 mm *
Stage II vulva cancer
Tumor of any size with extension to lower one-third of the urethra, lower one-third of the vagina, lower one-third of the anus with negative nodes
Stage III vulva cancer
Tumor of any size with extension to the upper part of adjacent perineal structures or with any number of nonfixed, nonulcerated lymph nodes
IIIA—Tumor of any size with disease extension to upper two-thirds of the urethra, upper two-thirds of the vagina, bladder mucosa, rectal mucosa, or regional lymph node metastases ≤ 5 mm
IIIB—Regional ** lymph node metastases > 5 mm
IIIC—Regional ** lymph node metastases with extracapsular spread
Stage IV vulva cancer
Tumor of any size fixed to the bone or fixed, ulcerated lymph node metastases, or distant metastases
IVA—Disease fixed to the pelvic bone or fixed or ulcerated regional ** lymph node metastases
IVB—Distant metastases
what is the primary treatment of vulva cancer
primarily surgical
based on staging and risk of nodal involvement
treatment of stage I-II vulvar cancer
conservative surgery
treatment of stage III-IV vulvar cancer
RT or chemoRT
what surgery is used to treat early stage lateral vulvar tumors?
Radical or hemivulvectomy +/- unilateral or bilateral lymphadenectomy
what surgery is used to treat early stage central vulvar tumors?
Radical vulvectomy + bilateral lymphadenectomy +/- reconstruction
what is added to surgery if the early stage vulva cancer has close margins or positive LNs
adjuvent RT
what surgery is done for stage III and IV vulvar cancer
fairly individualized
+/- vulvectomy +/- bilateral or unilateral lymphadenectomy +/- >1 LN MET…
list some of the rist factors that RT will be added to surgery for?
“+” margins
Lymphovascular invasion
“-” BUT close tumor margins (< 8 mm)
Tumor size
Depth of invasion > 1 mm
Spray or diffuse pattern of invasion
Nodal involvement (“+” sentinel LN, “+” LN’s post-inguinofemoral node dissection, > 1 metastatic LN &/or presence of extracapsular LN)
Whatis the primary treatment for Stage III-IV vulva cancer who is not a surgical candidate
radiation therapy ± concurrent chemo
Stage III-IV vulvar cancer RT
energy
technique
treatment site
D/F
use of bolus
6 MV (or 15 if seperation > 24 cm)
POP
RT to primary site + pelvis + inguinal nodes
50 Gy / 25-28 fractions
eliminate cold spot on the vulva + inguinal nodes
what are the sup, inf, and lat borders for RT to vulva cancer
Sup = L4/L5 (common iliacs) or L5/S1 (int/ext iliacs)
inf = 2-3 cm below vulvar marker (entire vulva)
lat = 1.5 cm lat to pelvic brim (to invlcue inguinal nodes)
when would PORT be used for vulva cancer and what is the typical D/F
PORT is used to local recurrences in tumors with “+” margins, tumor > 4cm OR depth of invasion >7 mm
D/F = 45-50 Gy / 20-25 fr
what is the typical set-up for RT for vulva cancer patients
supine, head on 10 cm sponge, hands on chest, ‘frog leg’ position for larger patients
Historical Phase I RT treatment of vulva cancer
technique
D/F
equally weighted POP (wider AP and narrow PA field)
AP treats pelvic and inguinal area, PA treats pelvis only)
45-60 Gy / 2 fractions
Historical Phase II RT treatment of vulva cancer
technique
depth
electron boost to inguinal nodes (direct abuttment)
depth to inguinal nodes = 3-4 cm ± bolus
modern vulva cancer RT treatments use IMRT/VMAT to spare OARs. What OARs are spared?
IMRT improves tumor coverage while sparing femoral necks, small bowel, rectum, bladder, skin
vulvar cancer modern treatment
energy
technique
D/F
6 MV
VMAT with 1 CW and 1 CCW arc
54 Gy / 30 fractions
what are the two main chemotherapies used in treating vulvar cancer
5-FU (alone or with cisplatin or mitomycin-c)
platinum based (alone or with 5-FU)
cisplatin, carboplatin, paclitaxel, erlotinib
what are some vulva cancer RT related acute side effects
mucocutaneous reaction in the vulva, perineum, and inguinal folds
Fatigue
Erythema, dry desquamation, moist desquamation
Diarrhea
Radiation cystitis
Vaginal narrowing, dryness and painful intercourse
what are some vulva cancer surgery related acute side effects
wound infection
hematomas
seromas
hemorrhage
deep vein thrombosis
pulmonary embolism
osteitis pubis
loss of sensory perception in the anterior aspect of the thigh secondary to femoral nerve injury
what are some vulva cancer RT related chronic side effects
telangiectasis
atrophy of the skin
dryness of the mucosa of the vagina and vulva
narrowing of the vaginal introitus
avascular necrosis
what are some vulva cancer surgery related chronic side effects
lymphedema
chronic cellulitis of the inguinal areas
stenosis of the introitus
femoral hernias
rectovaginal or rectoperineal fistulas
sexual dysfunction
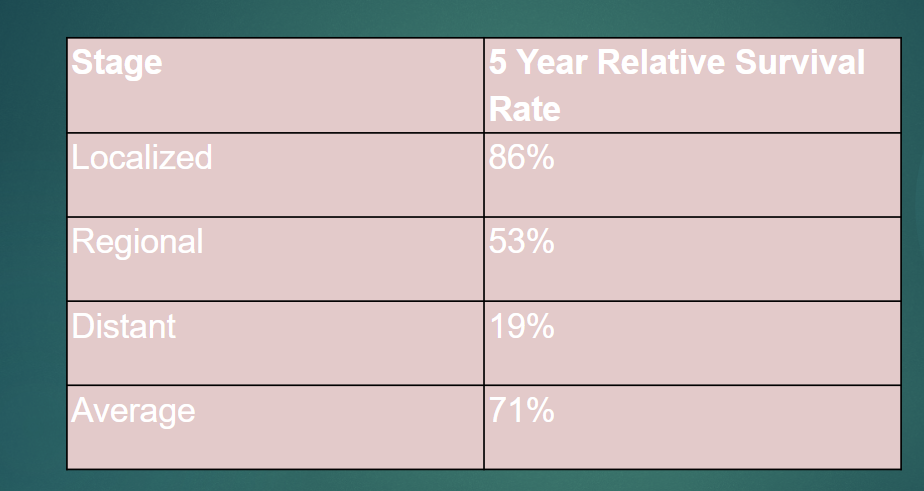
overall 5 year survival of vulva cancer
71%
most malignancies of the vagina are due to…
invasion from nearby tumors (cervix and vulva)
vaginal cancer epidemiology
% of all gynecological malignancies
age of peak incidence
why increased incidence in younger women
race effects
1-2% of all gynecological malignancies
mean age is 65
increased incidence in younger women due to HPV infections
incidence higher in african american women, lowest for asian
what is the most common cause of vaginal cancer
HPV
other etiological risk factors of vaginal cancer
Previous cervical cancer
In-utero exposure to diethylstilboestrol (DES)
Previous hysterectomy
Smoking - 2x risk of vaginal cancer
Older than 60 years old
Having HIV
what is the most common pathology of vaginal cancer
squamous cell carcinoma - cells lining the inside of the vagina
what pathology of vaginal cancer is most likely to spread
adenocarcinoma - glandular cells in the lining of the vagina
what is the precurso lesion to SCC of the vagina
vaginal intraepithelial neoplasia (VAIN)
VAIN 1: low grade, changes limited to upper ⅓ of the epithelium
VAIN 2: changes in lower ⅔ of the epithelium
VAIN 3: changes involving full thickness of epithelium, carcinoma in situ
vaginal cancer most commonly involves the _____ of the vaginal canal
superior 1/3 of vaginal canal
lateral walls less involved
anterior wall vaginal lesions infiltrate ____
posterior wall lesios infiltrate _____
anterior wall: infiltrates vesicovaginal septum or urethra
posterior wall: infiltrates rectovaginal septum or rectal mucosa
advanced vaginal cancer will infiltrate ….
parametrium, paracolpi tissues, urogenital diaphragm, levator ani muscles, pelvic fascia, pelvic sidewall
what are the three most common sites of vaginal cancer distant mets
lung, liver, bone
what are some clinical presentations of vaginal cancer
Abnormal bleeding from the vagina - post-coital, post-menopausal or between menstrual periods
Vaginal discharge that smells foul or has blood in it
Painful sexual intercourse
Lump in the vagina that can be felt
Constant pain in the pelvis, back, legs and perineum
Change in bladder habits - pain, burning or trouble urinating, the need to urinate often, blood in the urine and urgent need to urinate
Change in bowel habits - blood in the stool, constipation and painful bowel movements
Swelling in the legs or groin
in a physical exam that assists in diagnosing vaginal cancer, what is done?
Pelvic exam (DR/vaginal exam if suspected spread into rectum) and Pap test to check for abnormalities that may indicate vaginal cancer
Based on those findings, your doctor may conduct other procedures to determine whether you have vaginal cancer
what is the gold standard for diagnosing vaginal cancer
biopsy
what imaging tests can be done to diagnose vaginal cancer
colposcopy, CXR, CT, MRI, FDG-PET
what can imaging cancers be used for after diagnosis of vaginal cancer
to learn more about the cancer and see if it has spread
what is the most prognostic indicator of vaginal cancer
stage
earlier stage = more favorable
other prognostic indicators of vaginal cancer
Tumour size
Tumour volume
Local extent
Pathology
SCC most favourable
Grade
Spread to lymph nodes
Location of the tumour
middle and lower ⅓ of vagina or those on the back wall have a less favourable prognosis
Symptoms
women who present with symptoms = less favourable
Age & General health
younger women better outlook than >60 yrs + good health
Hysterectomy status: studies have shown an advantage for earlier hysterectomy
what sites can vaginal cancer spread locally to?
urethra, bladder, cervix, rectum, parametrial tissues, and paracolpial tissues (vascular and connective tissue)
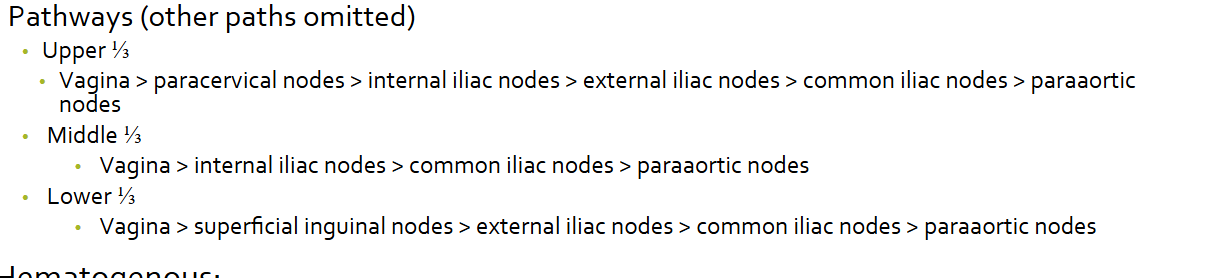
what are the three most involved LNs in vaginal cancer
paracervical nodes, internal iliac nodes, superficial inguinal nodes
vaginal cancer blood spread will occur after …
LN involvement
rare and later
Stage 0 vaginal cancer
carcinoma in situ
stage I vaginal cancer
tumor confined to the vagina
stage II vaginal cancer
invasion o the paravaginal tssiues but no extension beyond pelvic side walls
stage III vaginal cancer
extension to pelvic side walls
stage IV vaginal cancer
spread beyond the true pelvis
stage IVa: invasion of bladder/rectal mucosa and/or extension beyond the true pelvis
stage IVb: distant metastatic disease
Vaginal cancer TNM staging - T
primary tumor (T)TX - primary tumor cannot be assessed
T0 - no evidence of primary tumor
T1 - tumor confined to vagina
T1a - tumor confined to vagina, measuring ≤ 2 cm
T1b - tumor confined to vagina, measuring > 2 cm
T2 - tumor invading paravaginal tissues but not to pelvic sidewall
T2a - tumor invading paravaginal tissues but not to pelvic sidewall, measuring ≤ 2 cm
T2b - tumor invading paravaginal tissues but not to pelvic sidewall, measuring > 2 cm
T3 - tumor extending to pelvic sidewall (defined as muscle, fascia, neurovascular structures, or skeletal portions of bony pelvis; on rectal examination, there is no cancer-free space between the tumor and pelvic sidewall)
T4 - tumor invading mucosa of bladder or rectum and/or extending beyond true pelvis (bullous edema not sufficient evidence to classify tumor as T4)
Vaginal cancer TNM staging - N
NX - regional lymph nodes cannot be assessed
N0 - no regional lymph node metastasis
N0(i+) - isolated tumor cells in regional lymph node(s) ≤ 0.2 mm
N1 - pelvic or inguinal lymph node metastasis
Vaginal cancer TNM staging - M
M0 - no distant metastasis (no pathologic M0; use clinical M to complete stage group)
M1 - distant metastasis
what is the treatment of vaginal cancer based on?
based on clinical staging and risk of nodal involvement
what are the two goals of treatment of vaginal cancer
treat to cure
vaginal preservation of anatomy and function
what is the most common treatment of vaginal cancer
radiation therapy
what is the primary treatment of vaginal cancer with unfavourable factors?
neoadjuvent chemo + radical surgery
what are some unfavourable factors that chemo and sx would be used to treat vaginal cancer
cervix primary site, large lesion, extensive disease
what is the treatment of small superficial stage I and minimal stage II vaginal cancer
brachytherapy (interstitial and intracavitary)
what is the treatment of large stage I and II vaginal cancer
EBRT + intracavitary brachytherapy
what surgery may be used to treat stage I and II vaginal cancer and why?
radical hysterctomy + lymphadenectomy
preserve ovarian and sexual function
what is the primary treatment for advanced stage vaginal cancer
definitvie RT
what is the treatment plan for stage III and IVA vaginal cancer
interstitial + intracavitary brachy + EBRT
what surgery can be used for stage IVA vaginal cancer
Primary pelvic exenteration + pelvic lymphadenectomy OR neoadjuvant chemoRT
what is the treatment plan for stage IVB vaginal cancer
palliative EBRT and concurrent CT
what chemotherapies are used in the treatment plans of vaginal cancer
cistplatin or 5FU
overal chemo adds minimal 5 year survival benefit, but there seems to be increased benefit in stages ….
II-IV
why may surgery be chosen for early stage vaginal cancer (I-II: tumor limited to vaginal mucosa)
preserve ovarian and sexual function
eliminate risk for radiation-induced malignancies
what surgical procedures (3) can be used for disease in the upper vagina for patients with an intact uterus
radical hysterectomy
vaginectomy with 1 cm dx-free margins
pelvic lymphadenectomy
what surgical procedure can be used for disease in the lower vagina
Radical wide local excision with 1 cm margin + bilateral groin node dissection
what surgical procedure can be used for stage IV disease with vesical or rectal-vaginal fistulas
bilateral inguinofemoral lymphadenectomy
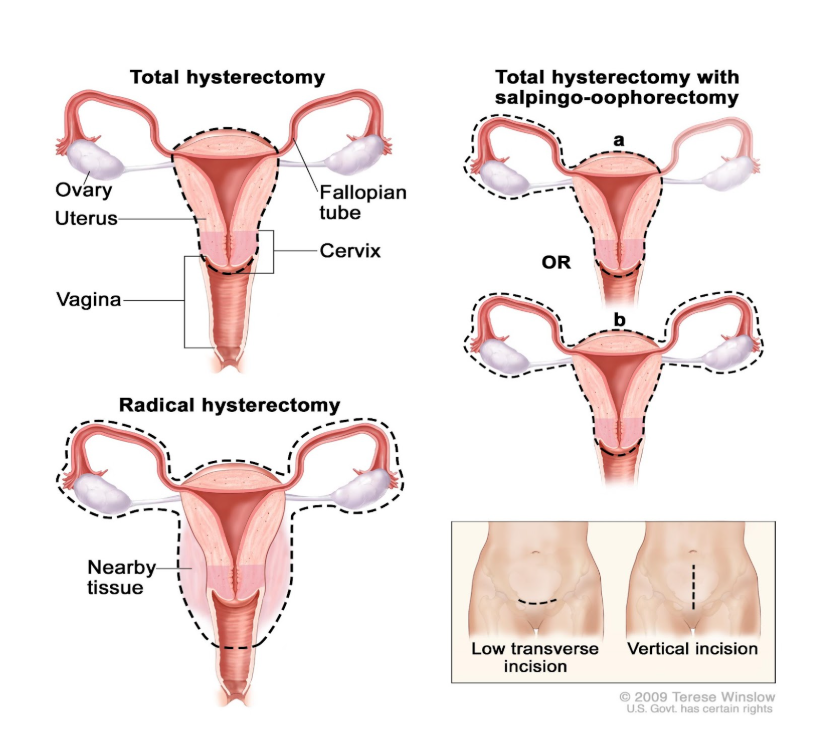
what hysterctomies performed open or laparoscopically?
laparoscopically
what is the primary benefit of doing EBRT and brachy therapy?
organ preservation
vaginal cancer EBRT
energy
technique
field size
D/F
accessories
15 MV (6 MV potentially for diff field weight)
AP/PA (unequal weighting) or 4FB
15×15 cm or 15 × 18 cm
45-50.4 Gy / 25-28 f
2 cm bolus for clinically palpable LNs
what should the EBRT fields include?
Encompass entire vagina, paravaginal area to pelvic sidewalls, LN’s at risk
distal common iliac, internal iliac, external iliac, obturator, presacral (+ inguinals if distal 1/3 to ½ of vagina)
what are two options for the boost added to EBRT for vaginal cancer? what does should tumor receive after the boost?
brachy or IMRT
boost primary tumor to 70-80 Gy
what are the sup, inf, lat borders for the AP/PA fields of EBRT treatment of early stage vaginal cancer
sup = L5/S1
inf = bottom of obturator foramen
for lower 1/3 vaginal lesions we extend length inferiorly to include inguinal nodes
lat = 1.5 cm lat of pelvic brim
what are the ant and post fields for the lat fields of EBRT treatment of early stage vaginal cancer?
ant = mid pubic symphysis
post = S2-S3
brachytherapy is indicated for all patients with ….
primary or recurrent vaginal cancer
Brachytherapy vaginal cancer treatment
Dose rates (2)
source
D/F for intracavitary (<0.5 cm thick)
D/F for interstitial (> 0.5 cm thick)
HDR or PDR
Ir-192
60-65 Gy / 3 fractions (10-20 mins long)
70-85 Gy / 3 fractions (10-20 mins long)
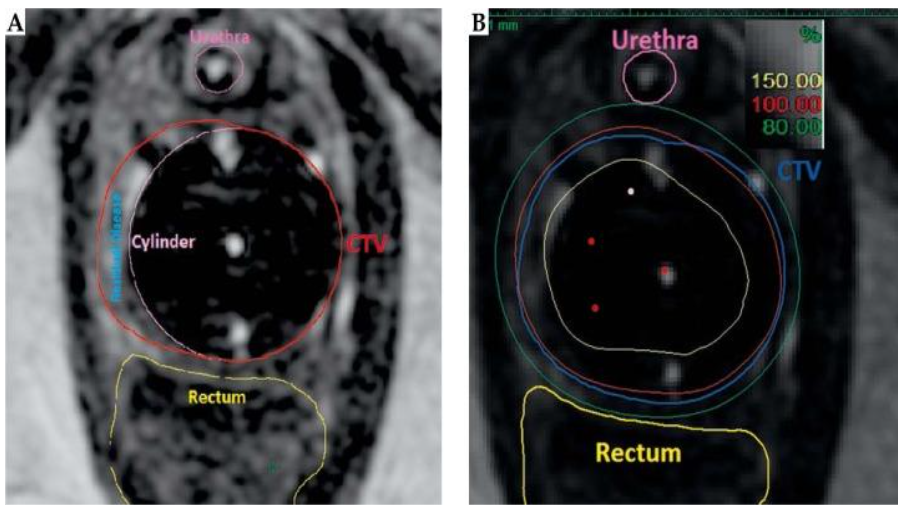
give an example typical dose prescription for a EBRT + brachy boost for vaginal cancer
45 Gy in 25 fractions EBRT and 5.5 Gy x 5 fractions HDR brachytherapy with CTV D90 = 79.8 Gy