Core Stability Training (1/5)
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
what is considered the "core"?
- anatomic cylinder of the human body
what muscles make up the front of the core? (2)
- rectus abdominus
- TA
what muscles make up the sides of the core? (2)
- internal obliques
- external obliques
what muscles make up the back of the core? (3)
- erector spinae
- multifidi
- quadratus lumborum
what muscles make up the top of the core? (1)
diaphragm
what muscles make up the bottom of the core? (1)
pelvic floor
what is core stabilization?
- the ability of the passive and active stabilizers of the lumbo-pelvic region to balance and control proper hip and trunk position during functional movements
what is the difference between passive core stabilizers and active core stabilizers?
- passive = spine, bones, ligaments
- active = muscles, diaphragm
what 3 things is core stability based on?
- co-activation of muscles
- coordination
- sensory-motor control
is refinement of trunk control and coordination more important than strength and endurance=?
yes
who is A. Bergmark?
- mechanical engineer
- studied lumbar spine from mechanical model approaches
- developed global vs local muscle systems for equilibrium of the spine
who coined the concept of prime movers vs prime stabilizers of the spine?
A. Bergmark
what are global muscles of the core? (2)
- RA
- erector spinae
what are local muscles of the core? (3)
- TA
- obliques
- multifidi
Who is M. Panjabi?
- looked at stabilizing systems of the spine through active, passive, and neural subsystems
- there are separate but inter-related systems to provide spine stability, especially intersegmental stability
who coined "neutral zone" to minimize spine injury?
M. Panjabi
who postulated that injury/insufficiency of one system can be compensated by another system?
M. Panjabi
is there controversy in treatment for the core? why?
- yes
- no consistency in patient categorizing
- lack of uniformity in PT training
what did early studies find in terms of -- core exercises having significant benefit for pain, disability, and recurrence rates?
- segmental stability exercises are more effective than GP only, but not more effective than other PT interventions
what did early studies find in terms of -- core stability exercises providing benefits after 1 year when compared to general PT exercises?
- no single trunk muscle has a dominant role in spinal stability
did early studies believe that core stability was a myth?
yes
instead of strong vs weak when assessing core muscles, what should be used?
active vs inactive
T/F: lumbar multifidi provide 2/3 of spinal stability in the neutral zone?
true
T/F: lumbar multifidi atrophy after first episode of LBP and do not recover even if pain is no longer present?
true
T/F: multifidus atrophy is bilateral and fatty infiltration associated with adult LBP and referred LE pain
- false
- multifidus atrophy is UNILATERAL
T/F: pain from a facet joint inhibits muscles innervated by the same nerve root level?
true
T/F: patients with chronic LBP have increased ability to contract multifidus?
- false
- significantly decreased ability to contract
T/F: patients with LBP have delayed firing of transverse abdominis and multifidus during limb movements and postural changes?
true
T/F: history of LBP will have delayed core activation with anticipatory responses?
true
T/F: patients with LBP have altered muscle activation patterns? explain.
- true
- increased rectus abdominis and erector spinae, less activation of deeper muscles
what does it mean for abnormal muscle function to be a possible cause or consequence of back pain?
- LBP patients activate and pre-activate erector spinae to a greater degree than non LBP patients
- can cause back pain
T/F: kinesthesia is impacted by LBP? what might be the implications of this?
- true
- will have poor trunk alterations in activities such as gait
T/F: dynamic balance is altered with LBP? why?
- true
- timing and sequencing alterations decrease dynamic balance
what does "bend but dont break within neutral zone" mean?
- correction of underlying joint dysfunction first, then likely regression of common core stability exercises
T/F: trunk stability requires muscle stiffness associated with appropriate timing and magnitude of activation of muscles?
true
what is the capacity model?
- global muscle approach
- S. McGill
- stability of the spine is dependent on contribution of muscle
according to capacity model, which muscles act as the guy wires to stabilize the intervertebral and pelvic joints?
larger "global" muscles
according to capacity model, should loads be applied during limb movements?
yes
according to capacity model, what are the 3 target muscles?
- erector spinae
- gluteal muscles
- rectus abdominus
what is the motor control model?
- local muscle control approach
- hodges, Hides, Richardson
- lumbopelvic health and function are dependent on accurate interplay of trunk muscles
what does control model put an emphasis on?
- CNS and PNS to determine requirements for stability during movement demands
- sensorimotor / neuromuscular approach
according to control model, what is segmental control essential for?
- spinal stability for fine tuning of spine motion
what are the 3 target muscles of control model?
- multifidi
- transverse abdominis
- posterior glute med
which core exercise model focuses on the whole movement?
capacity model
which core exercise model focuses on small parts of the movement?
motor control model
how to differentiate if an exercise is focusing on the motor control model?
- local or small muscle approach
- focus will be on maintaining a neutral spine with a distal movement occuring
what are movement impairment syndromes?
- repetitive use of movements that over time become impaired and lead to pathoanatomical changes in tissue and joint structure
T/F: there are a variety of movement impairment syndromes in the spine and extremities?
true
what is the most common movement impairment syndrome of the spine?
- lumbar extension/rotation syndrome
what is lumbar extension/rotation syndrome?
- mechanical LBP
- pain increases when they are moved into extension and rotation
> REMEMBER: Shirley Sahrmann MIS model is named by the motion that causes pain
what muscular components are often associated with extension/rotation syndrome of the lumbar spine?
- poor control of pelvic and lumbopelvic movement'
- asymmetries in muscles activation of hamstring and erector spinae
- prone knee flexion increases pain
will lumbar extension-rotation syndrome have an anterior or posterior pelvic tilt?
anterior
what 3 positions and movements will be painful for a lumbar extension rotation syndrome?
- prone knee bend
- hip rotation
- rocking in quadruped
how is lumbar extension rotation syndrome diagnosed?
- movement and alignment tests
- symptoms will decrease when extension and rotation of the spine are restricted
what 3 things should treatment for lumbar extension rotation syndrome be focused on?
- controlling movement
> lumbopelvic movement with less extension and rotation
- muscle re-education
> address underlying imbalances and activation
- correction of posture
> restoring ideal alignment and correcting positions that may induce pain
what 3 ways do PTs identify lumbopelvic dysfunction and aberrant motions?
- observe functional movements
- palpate muscles
- joint mobility testing
what might you observe from a test-retest during treatment of lumbar extension rotation syndrome?
- retest will be worse because you have taken away their compensation after the initial test
what should you observe for low back pain?
- hyper or hypo kyphotic/lordotic
- aberrant motions during gait, SLS, prone knee flexion
what should you palpate for low back pain?
- dominant/tight erector spinae, hip flexors, TFL, hamstrings
what should you assess with joint mobility testing for low back pain?
- likely SI, hip, and lumbar facet HYPOmobility
what are 5 core stability exercises to start with?
- prone knee flexion
- bent knee fall out
- heel slides
- march
(all are done with a neutral pelvis and TA activation)
what exercise should be done to target posterior glute med?
- clamshell
what is a common compensation patients will use during clamshell?
rolling backwards
what should you palpate during clamshell exercise to ensure proper muscle activation and sequencing?
- palpate posterior glute med and TFL
- should feel posterior glute med activate first and stronger than TFL
> if not, try rolling them anteriorly, bringing feet up higher, using towel roll to bolster between knees 1-3inches
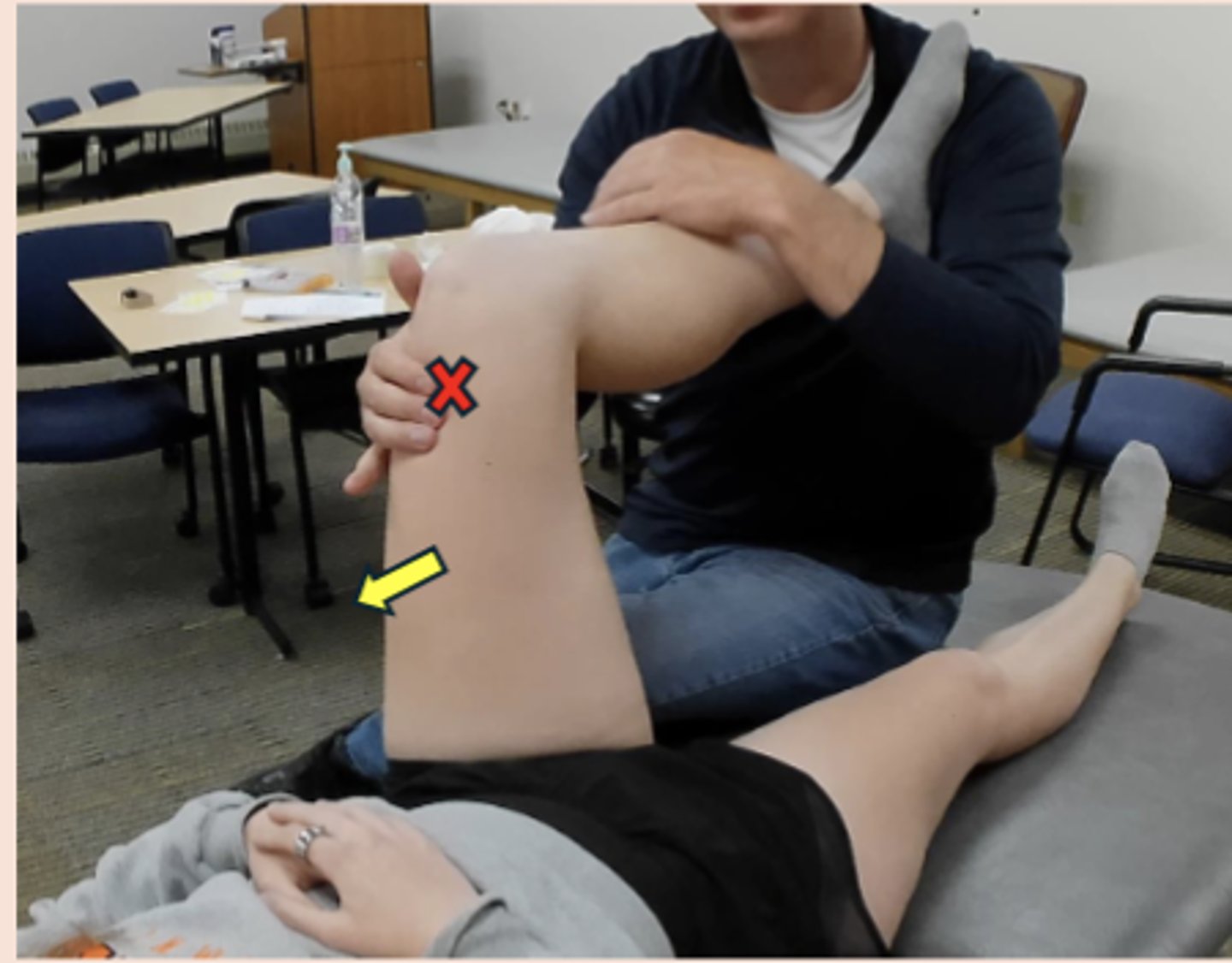
what is the flick test?
- alternative to the sheer test to help identify SI hypomobility
- stabilize the lumbar spine by palpating fingers into sacral sulcus, with other hand, flick the ilium posteriorly to assess for hypomobility on each side
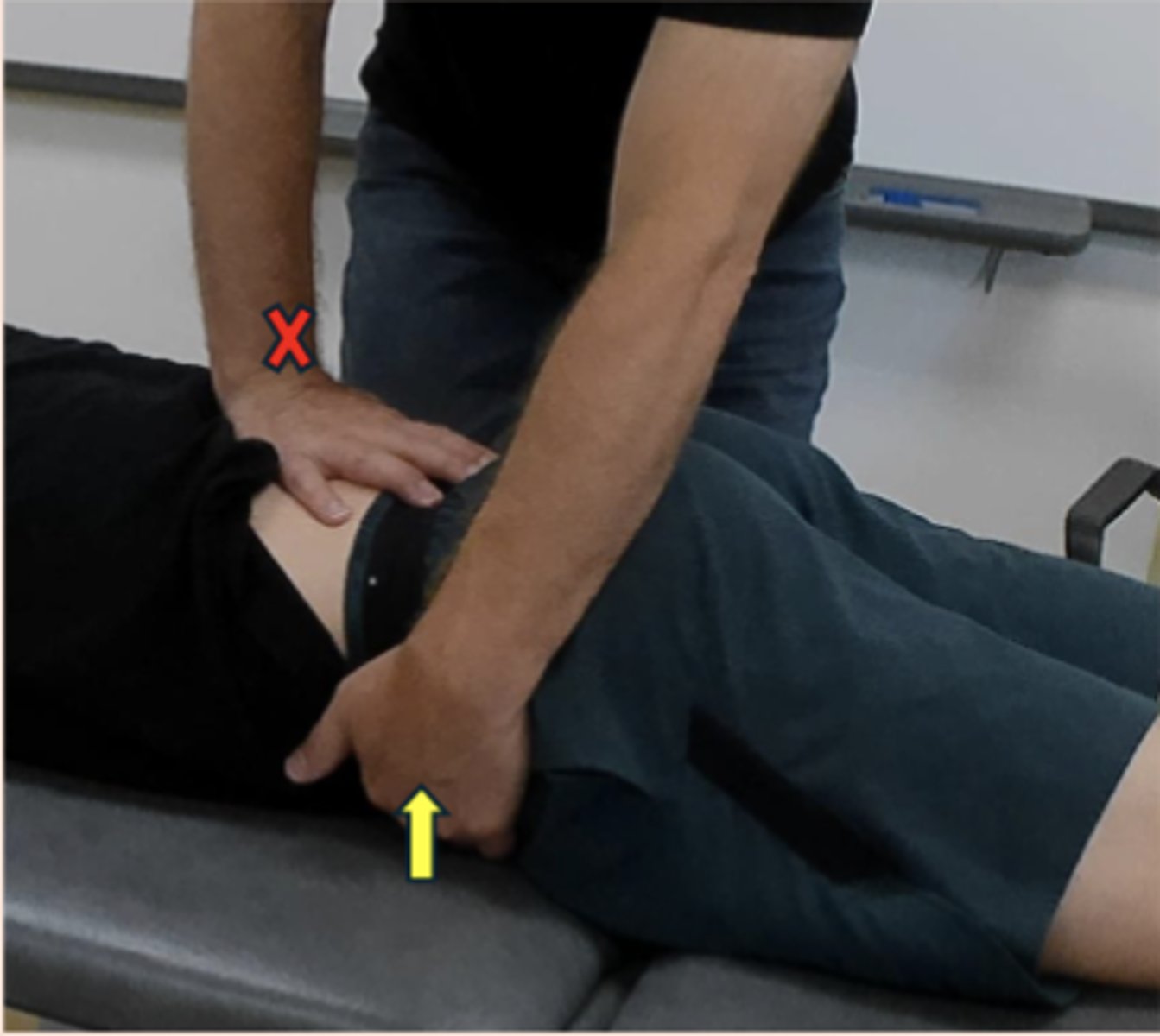
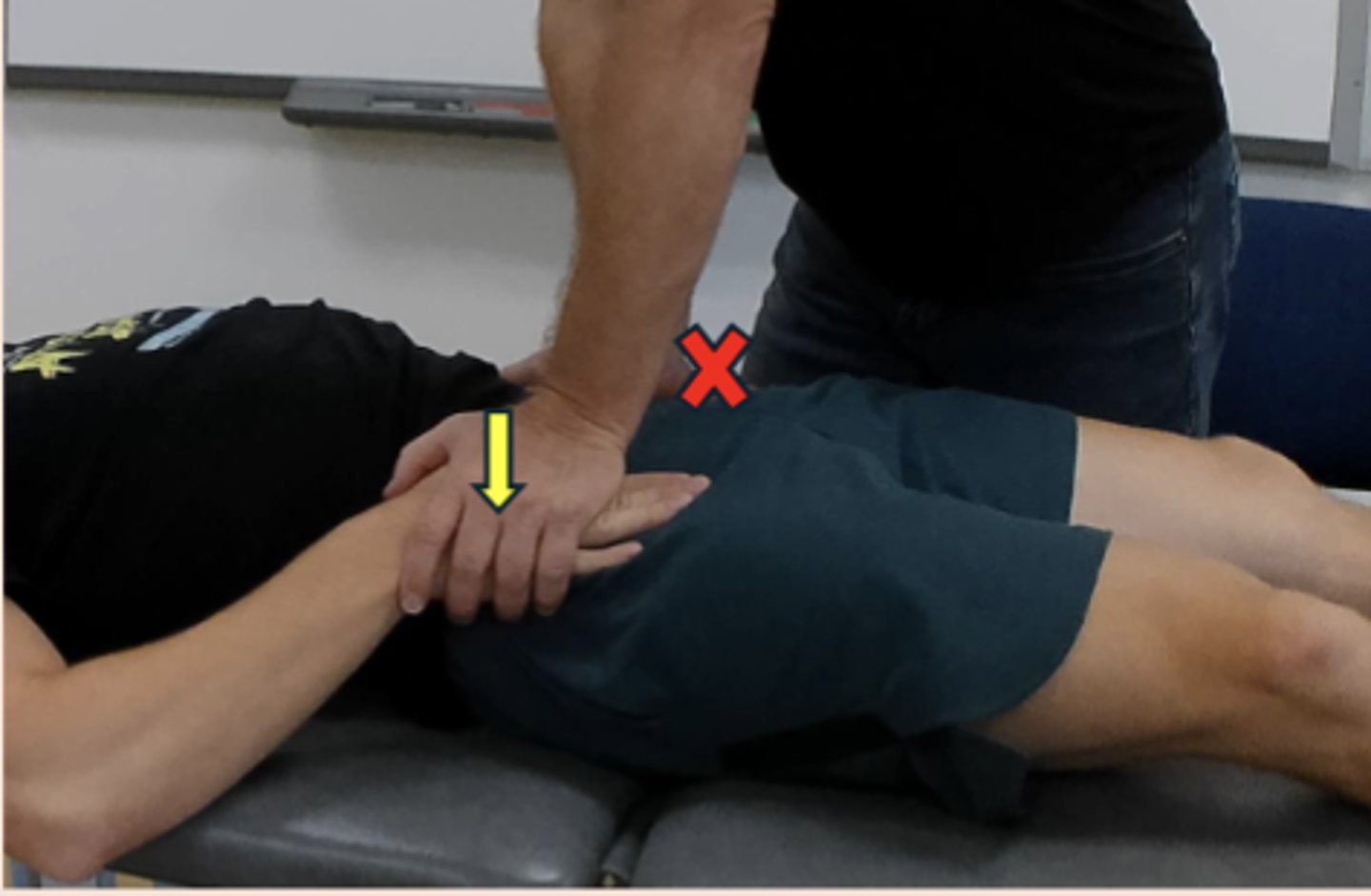
what is sheer/squish test?
- used to assess sacroiliac mobility
- with heel of one hand, stabilize the opposite ilium over the ASIS, use the other hand to slide the ilium posterior
what is the supine to sit test?
- used to identify anterior vs posterior innominate
- posterior = short to long
- anterior = long to short

how to correct an anterior innominate
- muscle energy technique
- patient in 90-90 position
- activate only glutes
- PT prevents HS or TFL from activating
- 3x10 seconds

how to correct a posterior innominate?
- muscle energy technique
- patient in 90-90 position
- activate rectus femoris only
- PT prevents HS or TFL from activating
- 3x10 seconds
what should always be done to the contralateral side when treating for anterior or posterior innominates?
- perform the opposite treatments to the contralateral side
what is recommended STM for all of these treatments? (2)
TFL and HS