B12 (cobalamin) (mine)
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
B12 names (3)
Cyanocobalamin
methylcobalamin
5-deoxyadenosylcolbalamin
B12 most critical forms
critical: methylcobalamin & 5-deoxyadenosylcolbalamin
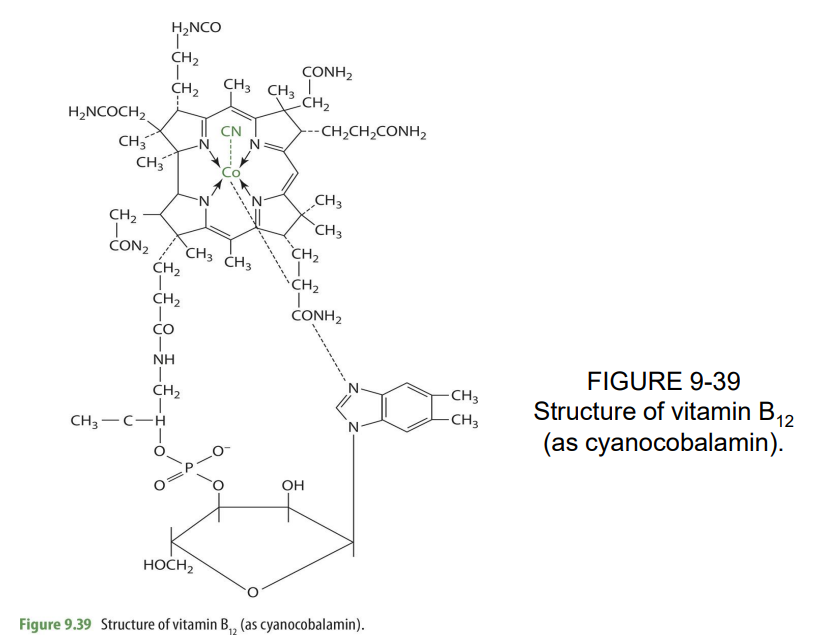
B12 structure
Macrocyclic rings made w/ 4 pyrrole rings, linked w/ colbalt
B12 is synthesized exclusively by
bacteria, fungi, algae
B12 plays a role in (2)
- maintenance of myelin sheath
- Folate metabolism
How can B12 enter the citric acid cycle (TCA)?
rearrange 3-carbon chain FA's
Cobalamin w/ a -CN group attached results in
cyanocobalamin
Cobalamin w/ a -OH group attached
Hydroxycobalamin
Cobalamin w/ a -H2O group attached
aquocobalamin
Cobalamin w/ a -NO2 group attached
Nitritocobalamin
Cobalamin w/ a -CH3 group attached
Methylcobalamin
what is a major issue with absorption of B12?
bioavailability
B12 bioavailability is impaired by
high doses of vit C
Major destruction of B12 in the presence of... (4)
ascorbate
folate
Fe
Gastric juices
salivary glands produce what
R-protein
where is B12 released from food and how?
in the stomach due to the acidic environment and pepsin
After food goes through digestion, B12 binds to ____ found in ___ & ____ to form _____
R-proteins
saliva & gastric juices
B12*R-protein complex
where is R protein found
saliva and gastric juices
made by salivary glands
the binding of B12 and R protein forms
B12-Rprotein complex
B12*R-protein complex travels from the...
stomach to the duodenum
what environment in the duodenum is the R protein digested & releases B12
alkaline
what enzyme releases R-protein from B12?
trypsin
In the duodenum, B12 binds & forms a complex w/ ____
IF (intrinsic factor)
IF is made by _____
gastric parietal cells
what does B12 binding to IF form?
to form the B12-IF complex
B12*IF complex travels through the ___ to the ___
jejunum and ileum
what occurs to B12-IF complex in ileum
B12 is absorbed via binding with receptor called cumbam complex
this process is facilitated by
calcium
cubam complex composed of
cubulin & amnionless, megalin)
After binding of B12-IF complex to receptor, appearance in the blood has a delay period of ___ and peak levels at are attained at___
4hrs
peak at 8hrs
what results in lack of IF production (like what would cause a lack of IF)
destruction of parietal cells
what does destruction of parietal cells lead to?
leads to B12 malabsorption & pernicious anemia
difference between megaloblastic and pernicious anemia
Macrocytic anemia = lack of folate or B12 intake
Pernicous anemia= lack of IF production
In older adults, malabsorption may result in....
inability to release food bound cobalamin
what is zollinger ellison syndrome
tumors associated w/ beta cells of pancreas
zollinger ellison syndrome what does it result in
results in overactivity of parietal cells (because of lack of bicarbonate secreted form pancreas), increasing acidity in SI & impair B12 release from R-protein
if R protein and B12 cannot separate…
B12 cannot be absorbed properly (because it cannot bind to IF —> cannot be absorbed through receptor)
absorption occurs through
active transport
absorption at high concentrations occurs through
passive diffusion
rate of absorption at low concentrations is
as high as 80%
rate of absorption at high concentrations is
as low as 3%
B12 binds too what carrier proteins
transcobalamins (I, II, III)
about ___% of B12 is bound to what carrier protein as a circulating storage form
80%
TCI (TC one)
major transporter to tissue & %
TCII (20-30%)
TCIII function
return cobalamin from peripheral tissues back to the liver
what is the major form of B12 in the blood
60-80% methylcobalamin
what form is found up to 20% in plasma?
adenosylcobalamin
what are the other 2 forms found in the blood (very tiny amounts)
cyanocobalamin & hydroxocobalamin
even if digestion and absorption is working, what could occur that will impact B12
genetic mutation that impact transporter
what genetic mutation may occur? what does it affect?
insertion of arginine for proline, which diminishes transport capacity of TCII
the genetic mutation is found in ____% of the population
20% of population
how does the genetic mutation with TCII affect compounds of the blood (2)
results in low serum B12 & high homocysteine in blood
tissue uptake of B12 is _________ dependent
receptor
tissue uptake of B12 is dependent with what receptors?
TCII receptors (bind to TCII-B12) and non-specific receptors (that bind to TCI-B12)
these receptors bind to what
TCII-B12 complex
Upon binding to receptor, B12 enters cells via ____ & ___ for _____
endocytosis AND fusion to lysosomes for degradation of TCII
what facilitates transport within cell organelles
chaperones & other transport proteins
storage of B12 is similar to
fat-sol vitamins
how much B12 is stored and length of storage
stored in larger quantities and retained for long periods of time (very low turnover rate)
how long before deficiency can arise
3-5 years
B12 is mainly store in ___, lesser amounts in the __
liver
muscle, bone, heart, brain etc.
primary form stored in the liver
adenosylcobalamin (70%)
main form associated w/ blood
methylcobalamin
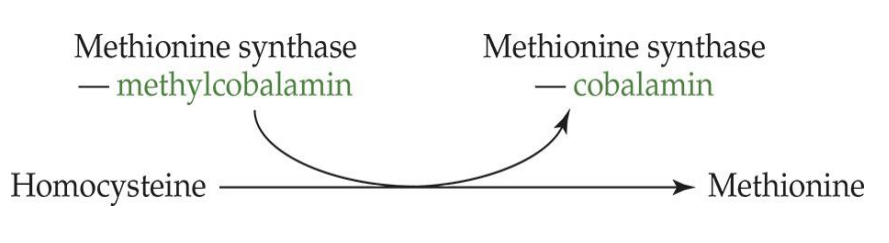
What is required for the synthesis of methylcobalamin? (what pathway)
Homocysteine metabolism
what are the functions of B12?
homocysteine metabolism
adenosylcobalamin helps convert methylmalonyl CoA to succinyl CoA (citric acid cycle).
Two specific reactions catalyzed by mutase enzymes in the mitochondria requiring adenosylcobalamin are (methylmalonyl CoA mutase and leucine aminomutase)
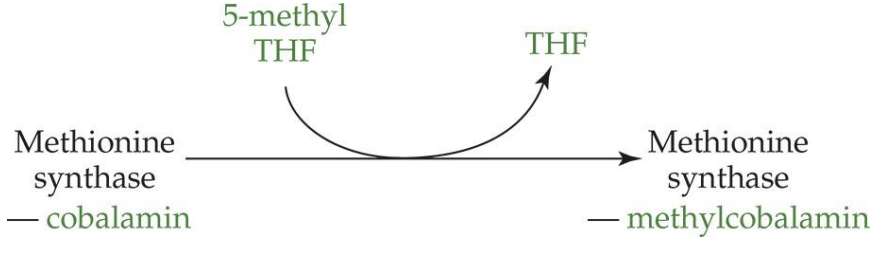
how is methylcobalamin made (process)
cobalamin is converted into methylcobalamin in homocysteine metabolism
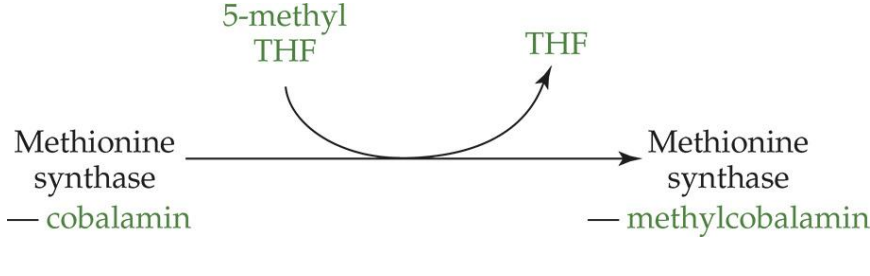
what is the enzyme in this reaction?
methionine synthase
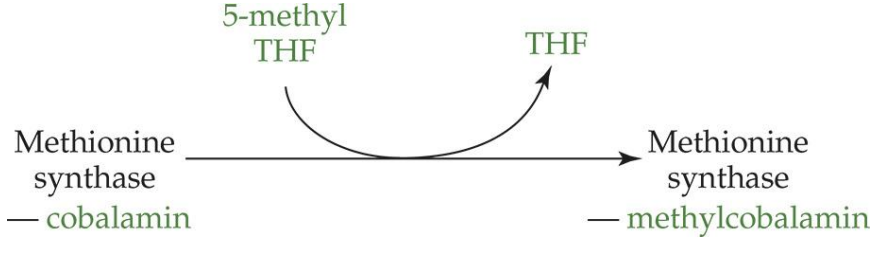
what other vitamin is involved in this process?
folate (5-methyl THF and THF)
when converving cobalamin to methylcobalamin, what occurs (enzyme, coenzyme)
reaction: cobalamin —> methylcobalamin
enzyme: methionine synthase
cofactors: 5-methyl THF —> THF
how does homocystine become methionine
reaction: homocysteine—> methionine
enzyme: methionine synthase
coenzyme: methylcobalamin —> cobalamin
What does adenosylcobalamin convert?
Methylmalonyl CoA to succinyl CoA
what form of B12 helps convert methylmalonyl CoA to succinyl CoA?
adenosylcobalamin
what does adenosylcobalamin do? (regarding reaction)
it oxidizes methylmalonyl CoA
methylmalonyl CoA requires what enzyme to become succinyl CoA?
methylmalonyl CoA mutase (requires x2 units of 5'deozyadenosyl cobalamin)
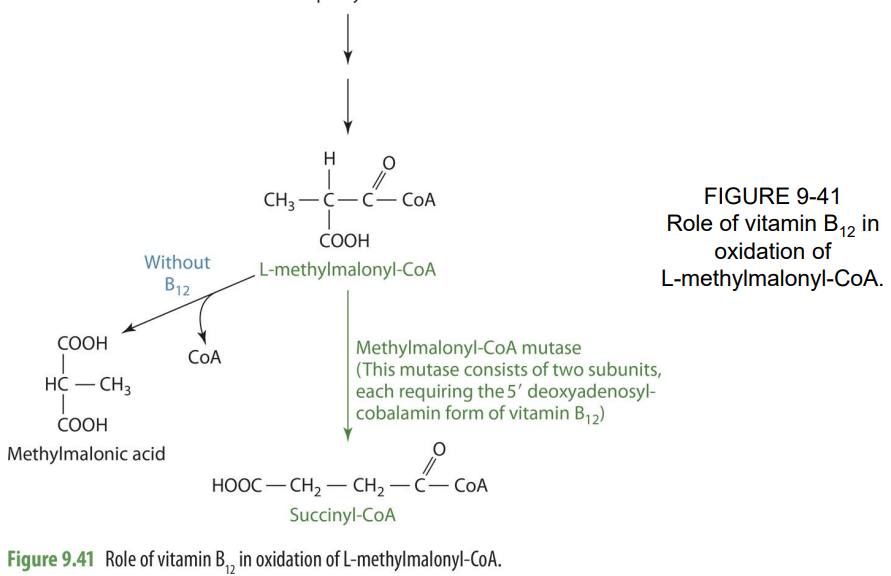
if B12 is not available, what occurs to methylmalonyl coA?
it becomes methylmalonic acid (loses CO2
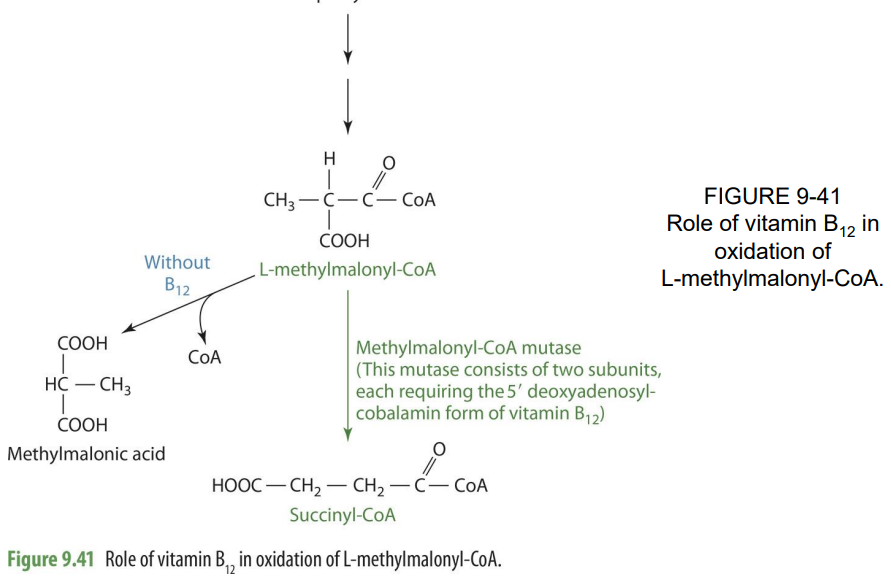
Where do reactions catalyzed by mutase enzymes requiring adenosylcobalamin occur within the cell?
In mitochondria
mutase enzymes requiring adenosylcobalamin are (2)
methylmalonyl Coa mutase & leucine aminomutase
what is associated w/ B12 deficiency (think symptom,effect)
neuropathy
how does B12 deficiency lead to neuropathy?
because it causes degradation of the myelin sheath (related to lack of methionine and availability of s-adenosylmethionine (SAM)
what is essential for maintenance of myelin sheath
SAM
excretion of B12 requires
little to no degradation prior
0.1%/d turnover (very little)
excretion of B12 occurs primarily through
bile & fecal
therapy for ineffective absorption (3)
monthly injections
B12 nasal gel
megadoses (allow for passive diffusion)
B12 is primality synthesized by
bacteria, fungi and algae
B12 is stored primarily in the
liver
food sources
animal products
organ meat (mainly liver)
seafood
eggs
hot dogs
milk
RDA (adults, elderly, pregnancy, lactation)
2.4ug/d adults & elderly
2.6ug/d pregnancy
lactatio2.8ug/dn
non-toxic; intake tends to exceed RDA
Deficiency of B12 is associated with what disease
pernicious anemia (megablastic/macrocytic)
pernicious anemia is characterized by
lack of IF
symptoms of pernicious anemia (4)
Nerve degeneration, weakness
Tingling/numbness in the extremities (parasthesia)
Paralysis and death
looks like folate deficiency
deficiency usually occurs due to
decreased absorption
deficiency treatment
monthly IM injections
what in elderly population can lead to B12 deficiency?
achlorhydria (lack of HCL in stomach)
Assessment is based on
Serum B12 concentrations
what is gold standard to determine problems with B12 absorption
Schilling test (finds absorption prob)
used to determine problems of vitamin B12 absorption related to IF insufficiency.
what compounds can be assessed to see issues wth B12 (serum and urine)
Serum methylmalonyl CoA or methylmalonic acid & homocysteine
Urinary methylmalonic acid
MMA and homocysteine
what other test may be used?
Doxyuridine (thymidine synthesis) supression test