RSPT 1311 2d and 2e exam review
1/89
Earn XP
Description and Tags
Combined with intubation lab quizz
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
90 Terms
Indications for intubation
Provide and maintain patency of an airway,
facilitate tracheal suctioning,
protect the airway from aspiration or obstruction,
and need for mechanical ventilation.
Preparing for Intubation: Physical Assessment
Signs of Respiratory Distress/Impending Respiratory Failure
Assessment and Auscultation
Mallampati Score
Diagnostic Testing
What type of blood gas would indicate the need for intubation. What would you see?
Respiratory acidosis - They have a high CO2. The more acidotic the gas, the more hypercapnic the patient. Indicates an increased need to establish an airway and provide mechanical ventilation and blow CO2 off.
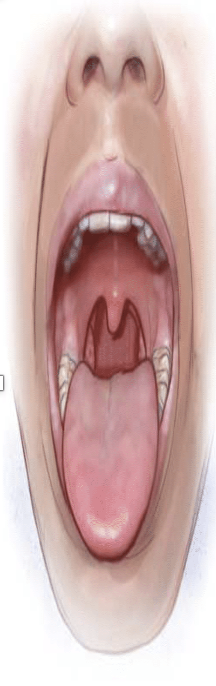
Mallampati 1 score
indicates that the entirety of the uvula can be visualized.

Mallampati 2 score
indicates that half of the uvula can be visualized
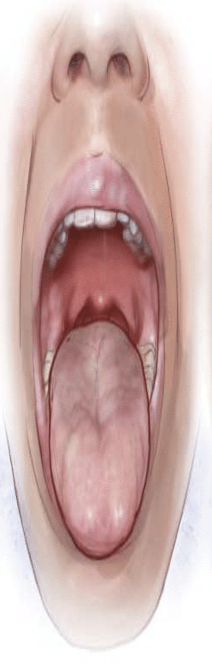
Mallampati 3 score
indicates that only the base of the uvula can be visualized.
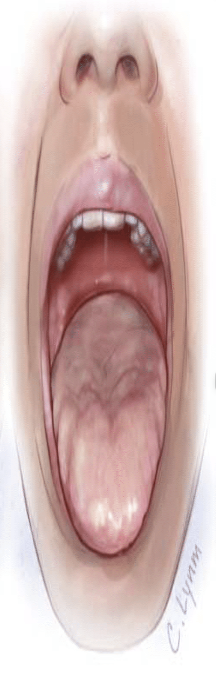
Mallampati 4 score
indicates that the uvula cannot be visualized.
Et tube is placed directly into
glottis
ID on ET tube refers to
internal diameter
ID measurement is in
mm
Murphy’s eye is important because
allows for ventilation should the distal end become obstructed
What is bevel for on ETT
for better visualization during intubation and to facilitate airway passage.
What is vocal cord guide for on ETT
to ensure proper placement of the endotracheal tube within the trachea.
Magill curve radios on ETT
refers to the curvature of the endotracheal tube designed to navigate around anatomical structures during intubation.
what can help combat nosocomial infection
humidification
radiolucent marking on ETT is used to
determine proper placement on trachea
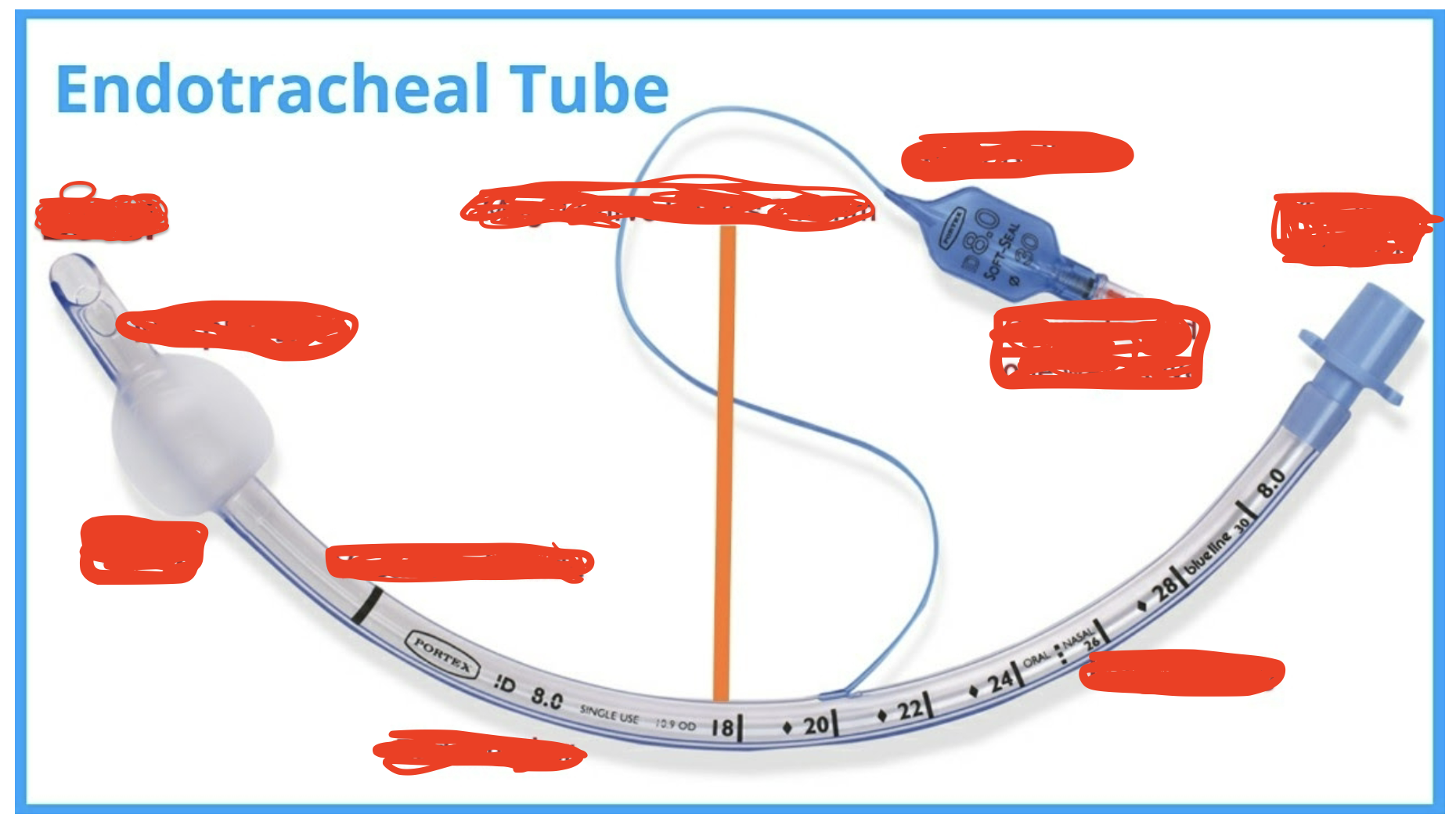
Parts of ETT
Bevel
cuff
Murphy’s eye
Vocal cord guide
Radiomarker
Magill curve radius 140mm
I’d number
Spring loaded one way valve
Pilot balloons
15mm adapter
first thing you do prior to tube placement
inflate the cuff
who has to be present at an intubation
RT
RN
MD
ventilator is alarming high pressures. patient is biting the tube. what is the appropriate action
insert bite block
how long should you hyperoxygenate a patient prior to extubation
5min
Suction equipment purpose during intubation
To suction out secretions and debris
to open the airway for good visualization and intubation.
Position for intubation
Head positioned with a towel roll under shoulders and neck flexed, with the head tilted back for a 'sniffing' position.
Miller laryngoscope blade
(straight) lifts the epiglottis directly, used for pediatrics/neonates;
Macintosh laryngoscope blade
(curved) lifts epiglottis indirectly, used for larger pediatrics and adults.
Methods for bedside assessment of tube position
Auscultation,
CO2 reader,
condensation,
and X-ray.
Clinical situations for nasotracheal intubation
Severe airway trauma that does not permit oral intubation and
oral surgery.
List the order of medicine for intubation
Induction Agent
Paralytic Agent
Sedative Agent
Steps of intubation
Assemble equipment,
position patient,
preoxygenate,
insert laryngoscope,
visualize glottis,
displace epiglottis,
insert tube,
assess tube placement,
stabilize tube.
Equipment required for intubation
O2 flowmeter and tubing,
resuscitation bag,
laryngoscope,
suction apparatus,
sterile suction catheters,
tongue depressor,
lubricant,
syringe,
endotracheal tubes,
stylet,
Yankauer,
Co2 detector
stethoscope,
tape/ETT holder,
Magill forceps,
local anesthetic.
Low CO2 reading after intubation suggests
The tube is likely in the esophagus.
CO2 reading indication for in the trachea
6%
Action for ET tube cuff leak during ventilation
Instill air into the cuff for a pressure of 20-25 cm H20.
During accidental extubation cuff leak is ….
Primarily problem for patients receiving mechanical ventilation
What is included in Appropriate Cuff Care
Cuff Inflation
Cuff Pressure
20 to 30 mm Hg
Minimal Occluding Volume
Minimal Leak Technique
Low Pressures
High Pressure
With cuff leaks tidal volumes will…
Be Reduced
Risk factor for ET tube cuff causing mucosal damage
Maintaining intracuff pressure of 38 cm H20 and using a low-volume, high-pressure cuff.
Indications for an oropharyngeal airway
Unconscious patient at risk of airway obstruction,
soft tissue obstruction,
bite block for intubation,
and facilitating suctioning.
Indications for a nasopharyngeal airway
Need for frequent NT suctioning and those recently extubated after facial surgery.
Determine ET tube in the right mainstem bronchus
CO2 reader changes color,
but auscultation shows breath sounds only in the right lobe;
visual asymmetrical chest rise.
Laryncoscope
Used with intubation to provide direct visualization of glottis
Laryngoscope blade size for 6-12years old
Miller 2
Macintosh 3
Laryngoscope blade size for adults
Miller 3
Macintosh 3
ETT size 12 years
6.0-7.0
Distance at teeth 17-19 cm
ETT size age 16/small women
6.5-7.0
Distance from teeth: 18-20cm
ETT size women
7.5-8.0
Distance from teeth: 19-21cm
ETT size men
8.0-9.0
Distance from teeth: 21-23cm
For blind insertion with nasotracheal intubation, patient must…
Breathe spontaneously
Nasotracheal Intubation
Indicated in cases of inability to clear secretions,
visible secretions,
increased work of breathing,
or suspected aspiration.
Normal Cuff Pressure
The normal cuff pressure is 20-25 mm Hg.
Name artificial airway complications?
Tube obstruction
Herniation of cuff over tip
Obstruction of tube orifice against tracheal wall
mucus plugging
Cuff leaks
Include tracheal and esophageal perforation,
laryngeal abrasion,
vocal cord trauma,
how to troubleshoot tube obstruction
kinking or biting tube – obstruction is reversed by moving patients head or repositioning tube
troubleshooting Herniation of cuff over tip
deflate cuff,
if deflating fails to overcome obstruction, try to pass suction catheter through tube
troubleshooting mucus plugging
suction tube if installation of sterile normal saline is not necessary
troubleshooting cuff leaks
if pilot tube or valve is leaking, tube needs to be changed asap
ruptured cuff requires extubation and re-intubation or using endotracheal tube exchanger
What to keep at bedside for emergency airway troubleshooting?
Additional trach of current size
TT one size smaller
manual resuscitation bag and mask
Gauze pads (for pts with tracheostomies)
Vallecula
An anatomical depression immediately beyond the base of the tongue.
Epiglottis
A flat cartilage that extends from the base of the tongue backward and upward.
Maximum Intubation Attempt Time
The maximum time allotted for an intubation attempt is 30 seconds.
Ventilation Between Intubation Attempts
Ideally, 3-5 minutes should be spent ventilating a patient between intubation attempts.
Cuff leak during accidental extubation will……
cause reduced delivery of tidal volume
Partial displacement of airway out of trachea can be detected by:
Decreased breath sounds
Decreased airflow through tube
Decreased ability to pass catheter past end of tube
during accidental extubation you may hear what…
With positive pressure ventilation, airflow through mouth and nose or into stomach may be heard
Preventing Nosocomial Infection
Strategies include humidification,
sterile suction,
minimizing circuit breaks,
and oral care.
What are the 4 indicators for extubation readiness?
RSBI
MIP
Vital Capacity
Cuff Leak
Rapid Shallow Breathing Index (RSBI) Calculation
RSBI = respiratory rate / Tidal Volume;
<105 = Success,
>105 = Failure.
Cuff Leak Calculation
Cuff Leak = (cuff inflated volume - cuff deflated exhaled volume) / cuff inflated volume; leak must be >15%.
Define Maximum inspiratory pressure.
aka Negative inspiratory force.
How is MIP utilized to determine extubation
readiness?
This helps us see if muscles are working.
The amount of negative pressure a patient can generate in 20sec when inspiring against an occluded measuring
What value is indicative of weaning success with MIP
< -30 cm H2O
Can be obtained from ventilator maneuvers or manual maneuvers
Define vital capacity.
The amount of air that can be exhaled after a maximum inspiration
What is vital capacity measuring?
The sum of:
the inspiratory reserve volume
tidal volume
expiratory reserve volume
In the medically ventilated patient, it is the measurement of a patients largest VT over a 40second period
What measurement in Vital Capacity indicates extubation readiness?
>10ml/kg
Clinical Indicators for Weaning from Ventilator
-when original need for the artificial airway no longer exists.
-Ability to maintain adequate oxygenation and ventilation without mechanical support
-Decreased quantity and thickness of secretions
-Presence of Upper airway patency
-Presence of intact gag reflex
-Ability to clear airway secretions
Weaning
the gradual transition from full invasive ventilatory support to spontaneous ventilation with minimal support
Liberation
discontinuation of mechanical ventilatory support
Wean + extubate leads to it.
Vent settings for weaning readiness?
minimal FiO2 (<50%)
Minimal PEEP (<8 cm H2O)
PaO2 >60 mm Hg
pH 7.35 – 7.45
PaCO2 35-45 mm Hg (approx. 50 for COPD pt)
Vd/Vt <60%
MV <10 L/min
Provide the contraindications of extubation
Acute respiratory failure
inability to maintain patent airway
impairment of mental status, oxygenation, ventilation, and expectoration (MOVE)
Hemodynamic instability
Plan to return to operating room in the next 24hours (safer to not take them off, and put them right back on)
Use of paralytic agents (no control of their muscles for breathing)
Process of extubation
-assembly the needed equipment
-suction the ETT and pharynx above the cuff
-oxygenate patient well after suctioning
-deflate the cuff
-remove the tube
-apply appropriate oxygen and humidity therapy
-assess and reassess the patient
What does suctioning ETT and Pharynx above cuff for extubation help with?
-assists in prevention of aspiration of secretions after deflating cuff
-minimizes possibility of ventilator associated pneumonia (VAP)
Why do we oxygenate patient well after suctioning prior to extubation?
-Hypoxemia is often a side effect of extubation due to stress of cardiovascular side effects
-suggested administration of increased FiO2 for a minimum of 5min prior to extubation
appropriate oxygen and humidity therapy after extubation
ensure oxygen and aerosol supplies are at hand
cool mist may be indicated to minimize stridor
Hazards of Extubation
Include hypoxemia,
stridor,
hoarseness,
sore throat,
and complications like vocal cord paralysis.
Laryngospasm
Purpose of Coughing Before Extubation
To prevent swallowing any secretions during the extubation process.
Why is cuff leak test performed?
Helps assess the presence of glottic edema, or the possibility of stridor post extubation
Helps assess the success of extubation.
It should be performed on individuals with a high-risk of post extubation issues (history of airway trauma, prolonged intubations, presence of factors that may lead to laryngeal swelling)
Cuff leak test steps
Oral care
Subglottic suctioning
Completely deflate the cuff – this determines the presence of laryngeal edema (no leak is bad)
what percentage of leak should lead to considering extubation?
A significant leak will be present in a patent airway indicated by a leak >15%
Equipment for extubation
-sunctioning kits (2)
-yaunker
-10-20ml syringe
-oxygen therapy and aerosol therapy equipment
-manual resuscitator and mask
-nebulizer, racemic epinephrine, and normal saline
-intubation cart or box
no leak during extubation means
possible swelling in airway
stop + reinflate cuff + talk to the team
patient might need more time, steroids
Extubation to trach is indicated with who?
In those where respiratory failure may be resolved, but airway patency is an ongoing issue
Patients with prolonged ventilation needs, difficulty weaning off mechanical ventilation, or chronic respiratory conditions.
Airway patency is the main concern → long term airway needed