OPT 329 Corneal Transplants
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
recalcitrant corneal edema due to...
Fuchs’ endothelial dystrophy
Pseudophakic Bullous Keratopathy (PBK)
Aphakic Bullous Keratopathy (ABK)
Iridocorneal Endothelial (ICE) Syndromes
congenital corneal disorders/dystrophies
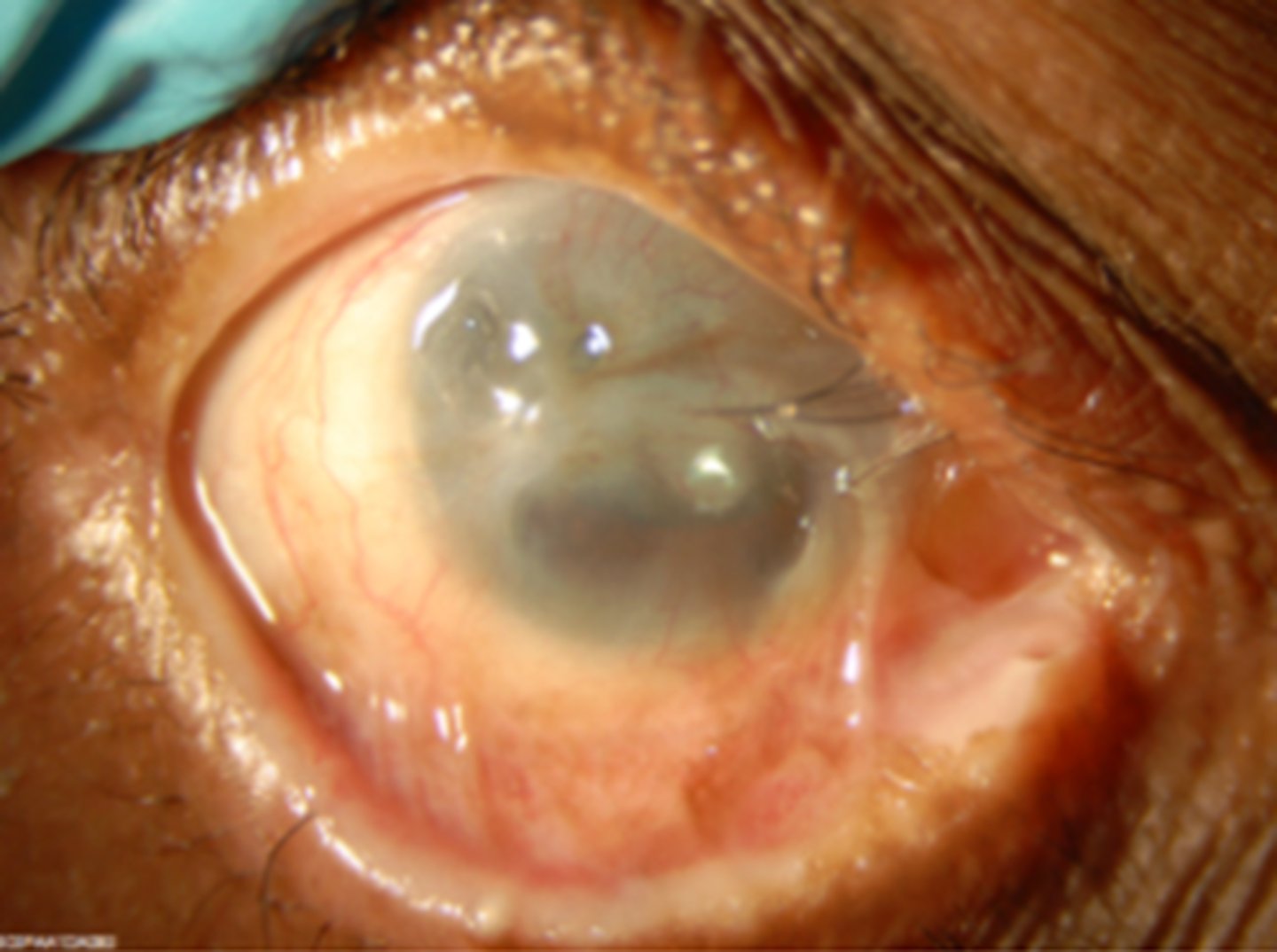
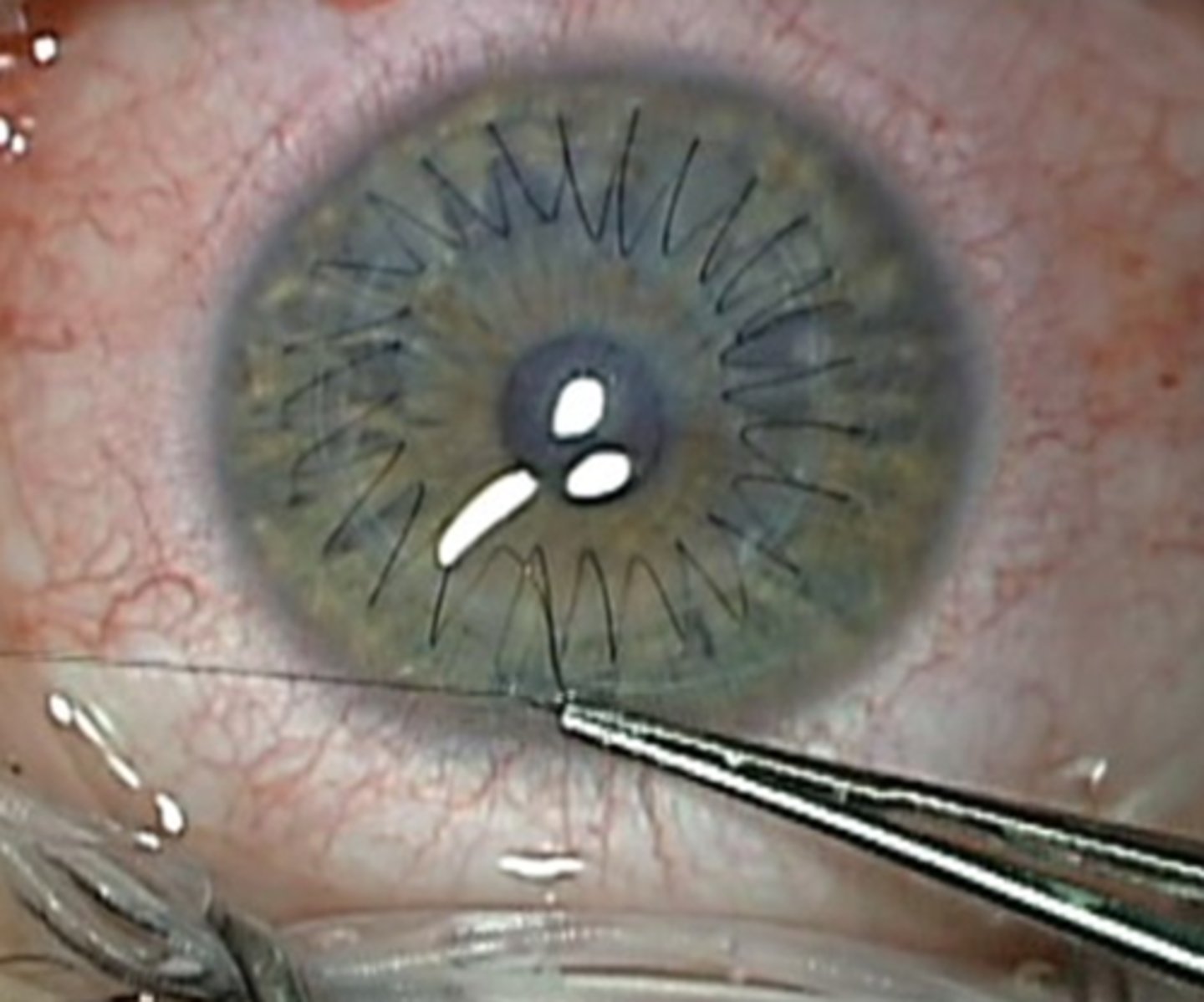
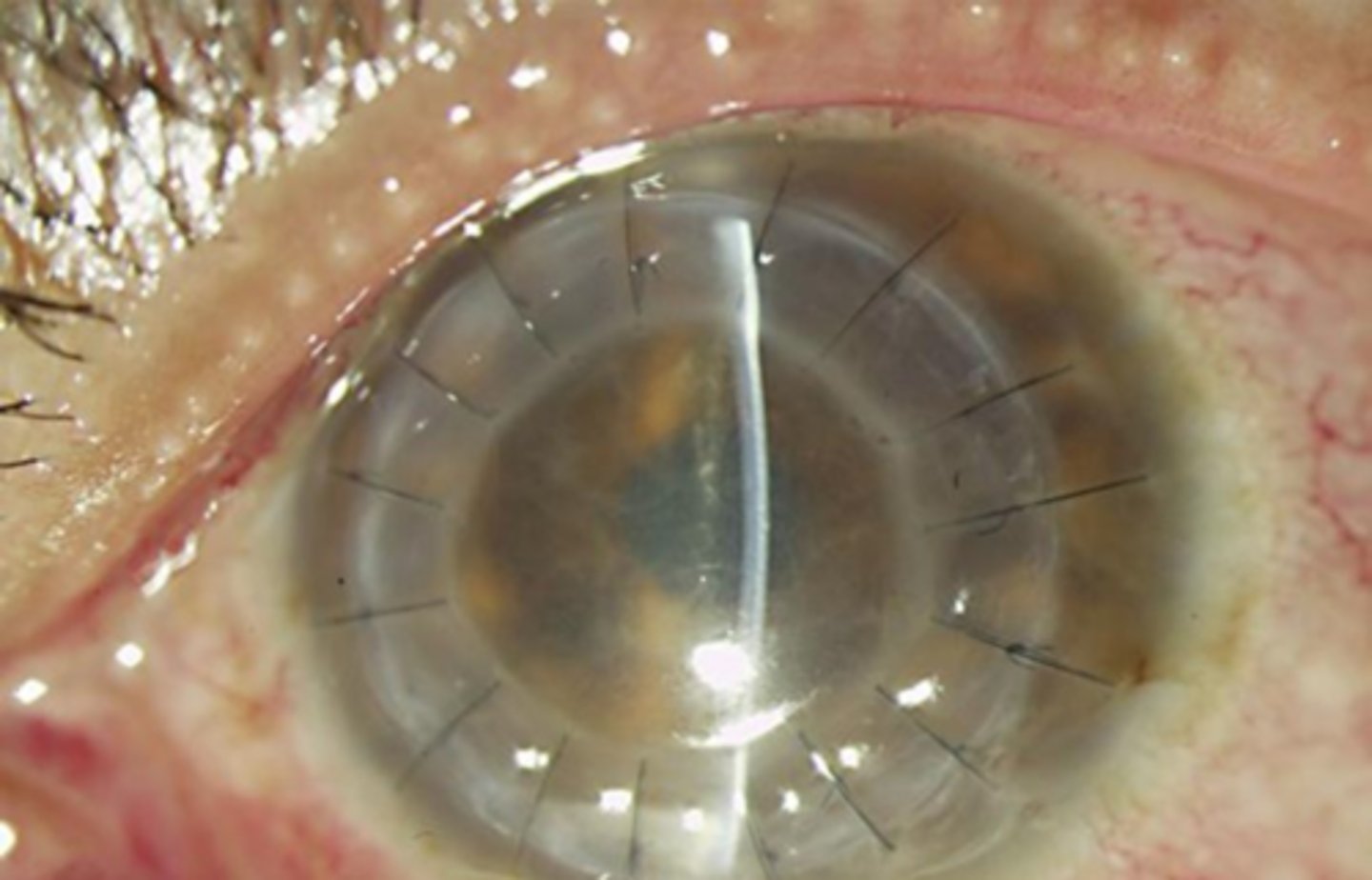
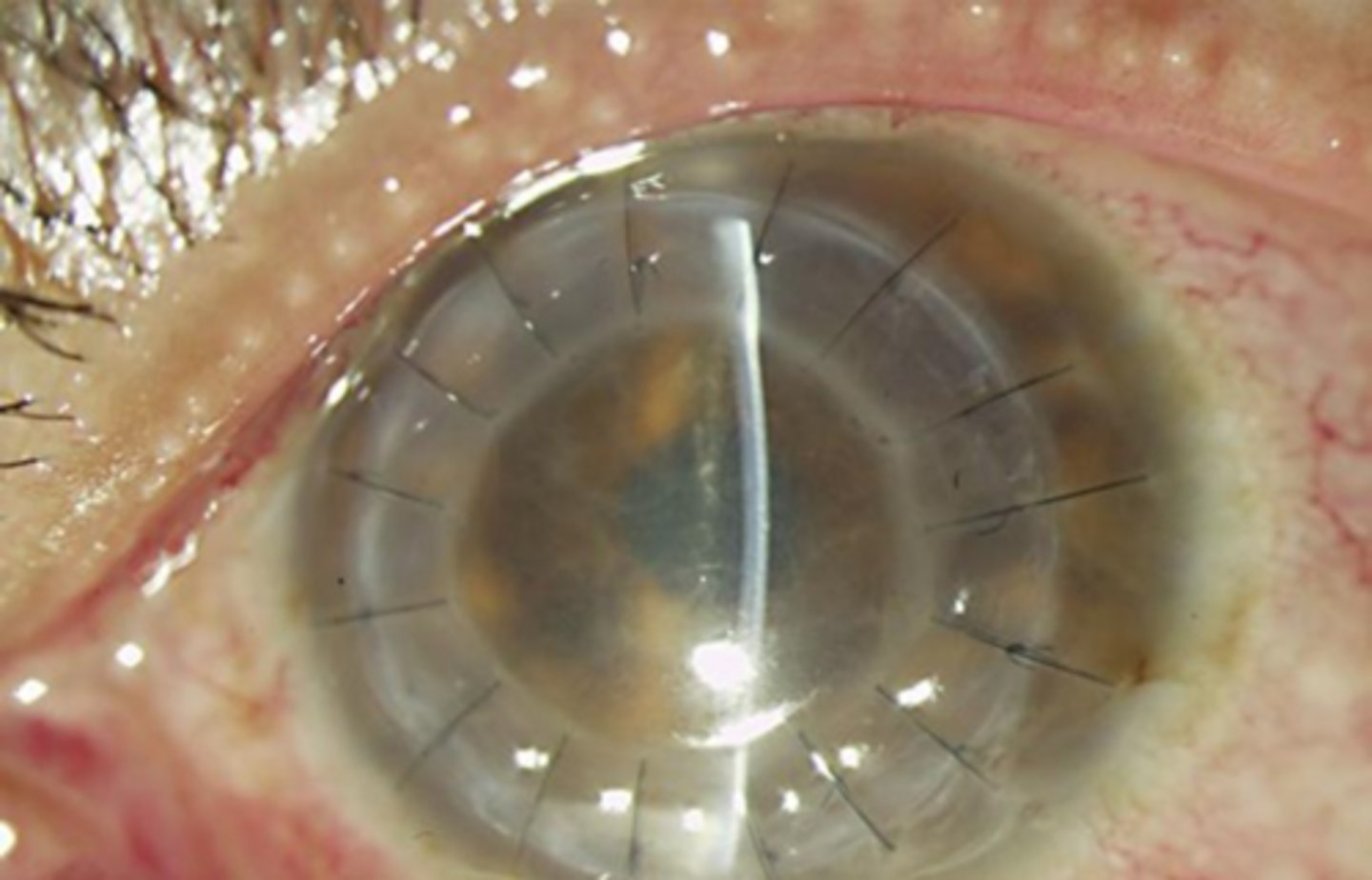
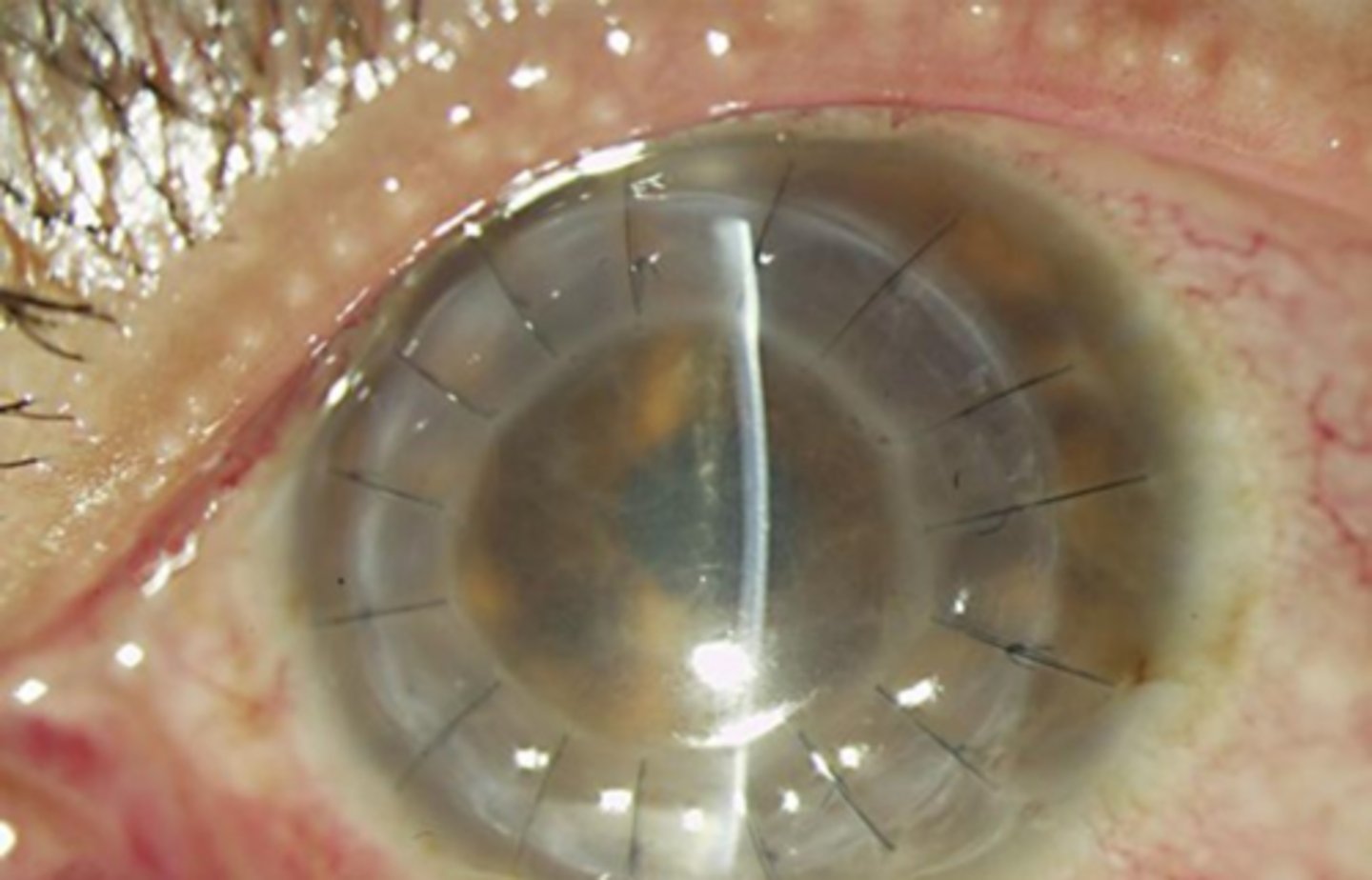
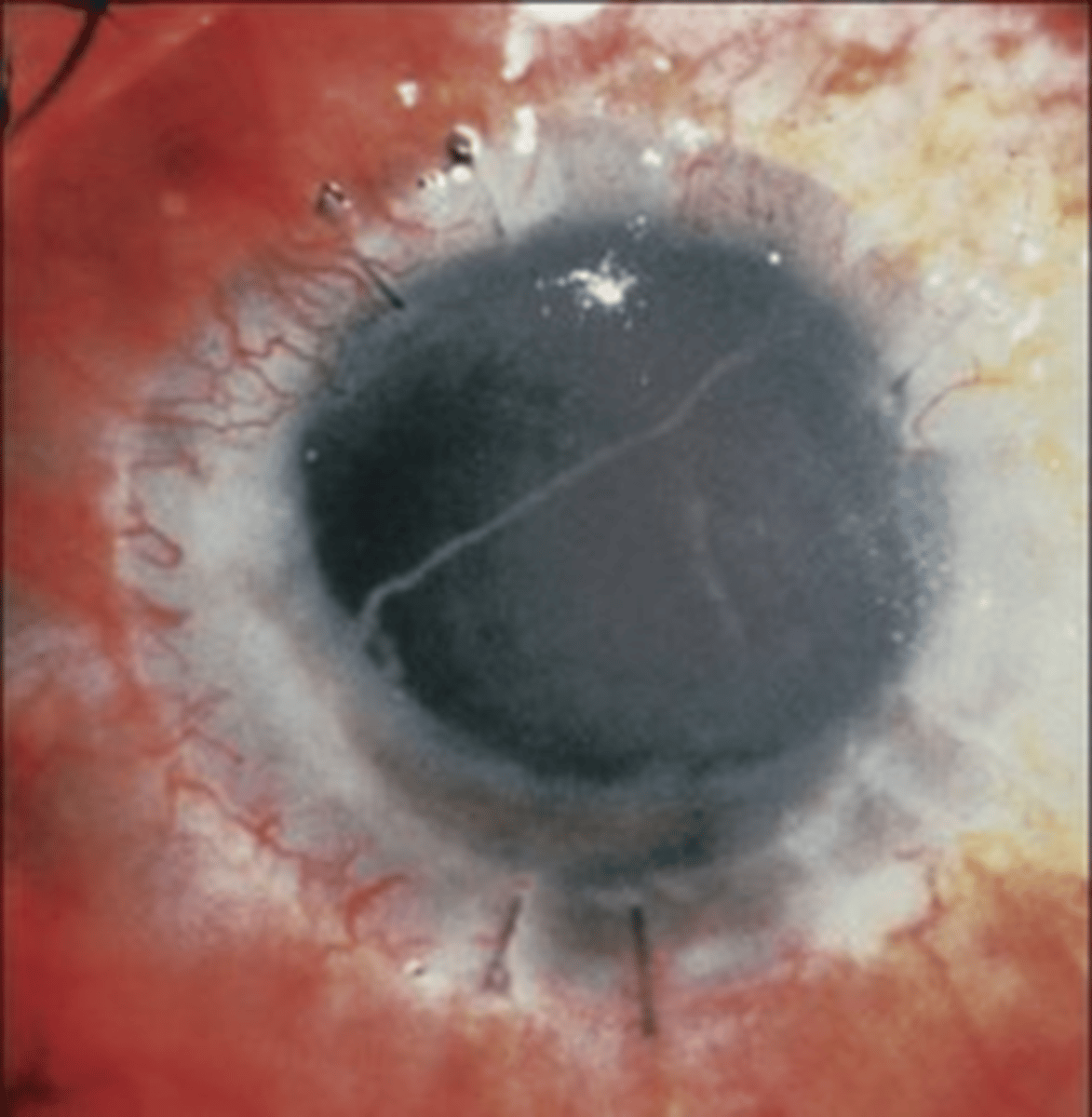
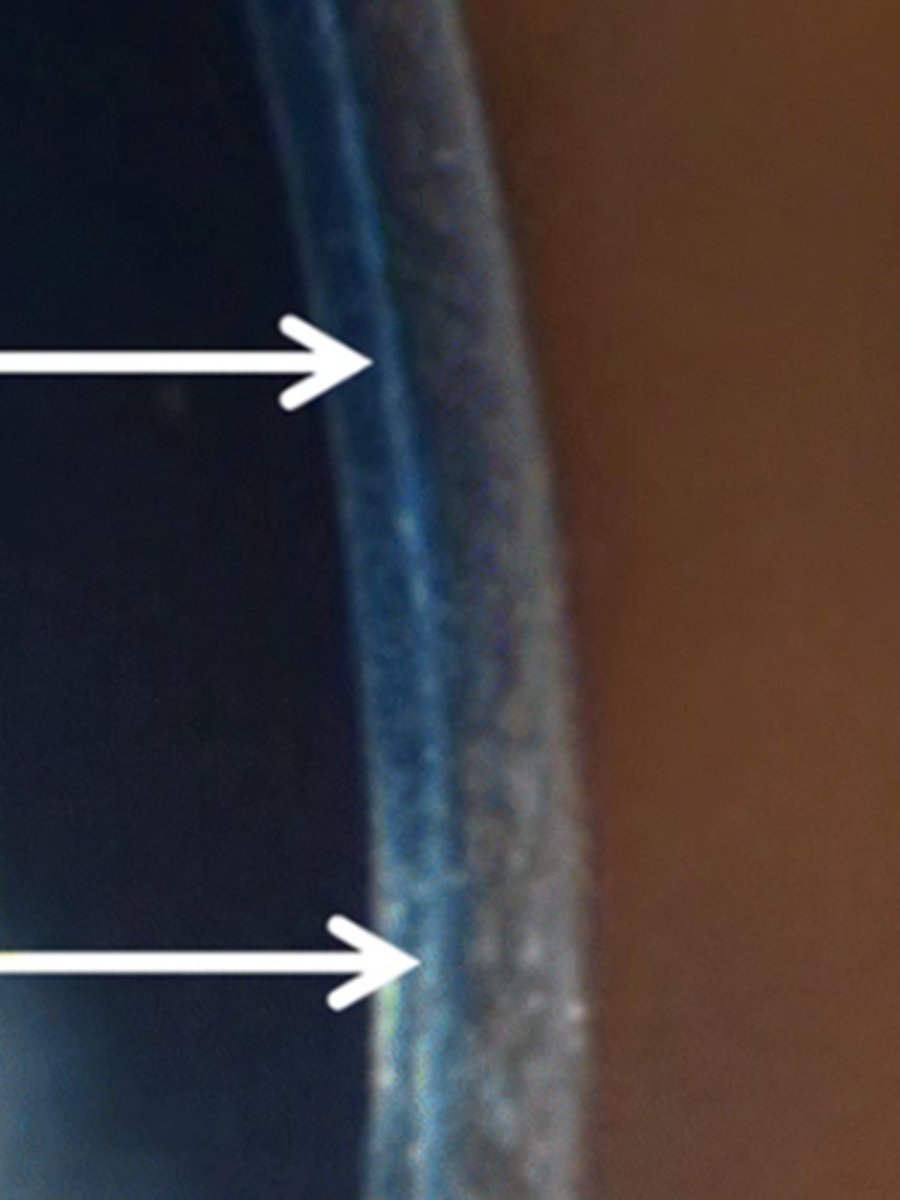
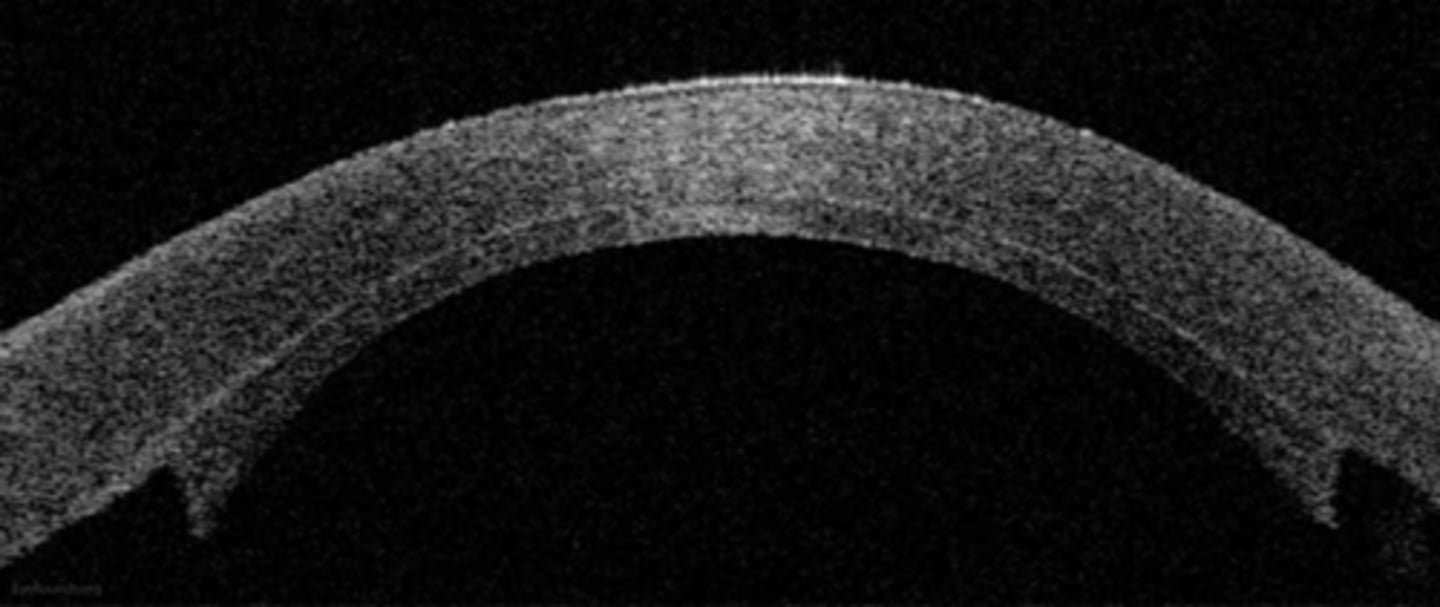
What indication for corneal transplant is seen here?
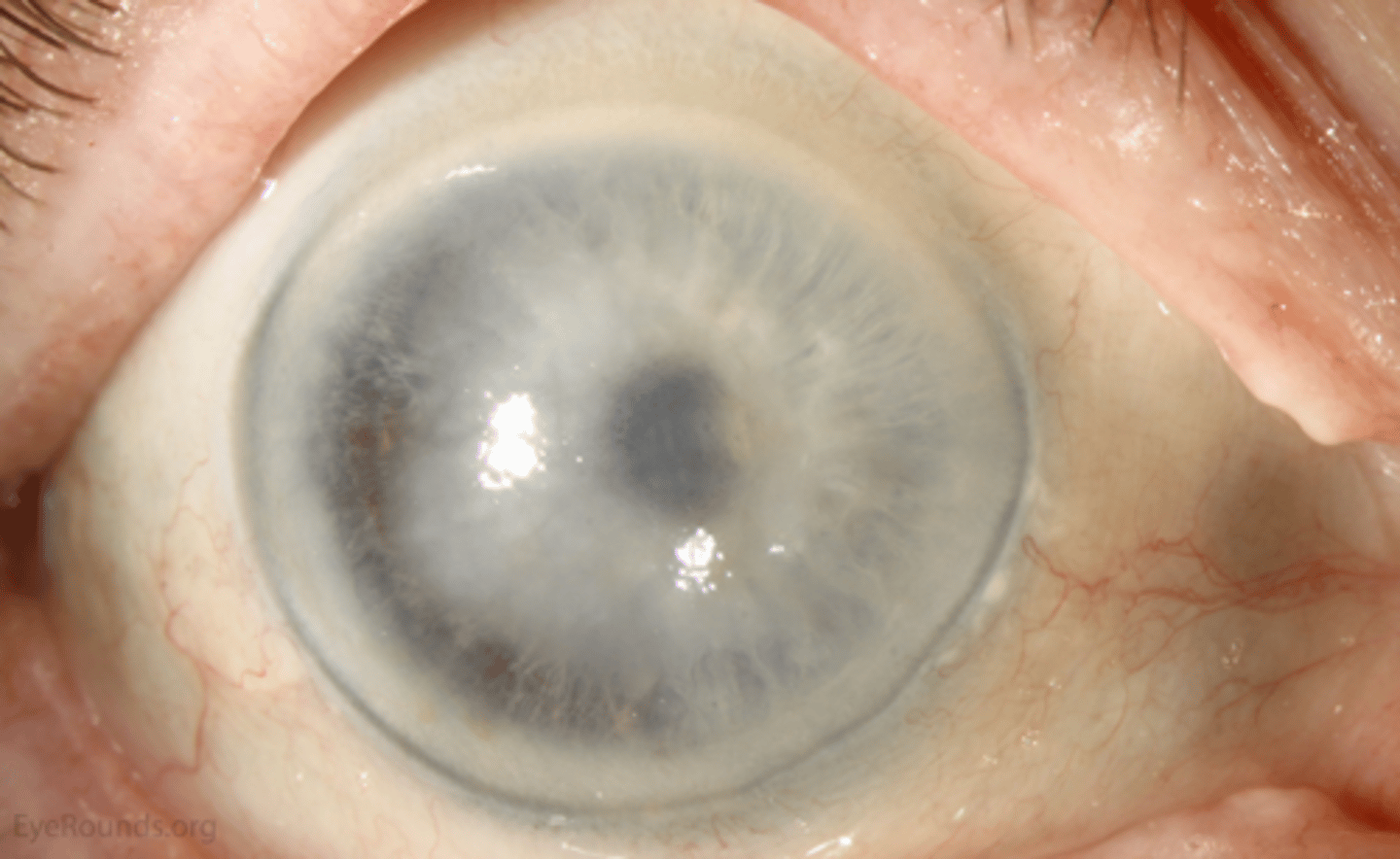
dense stromal corneal opacification due to...
acquired scarring (trauma, chemical injury, burn, SJS, OCP, trachoma, HSV, ulcers)
stromal dystrophies (granular, lattice, macular)
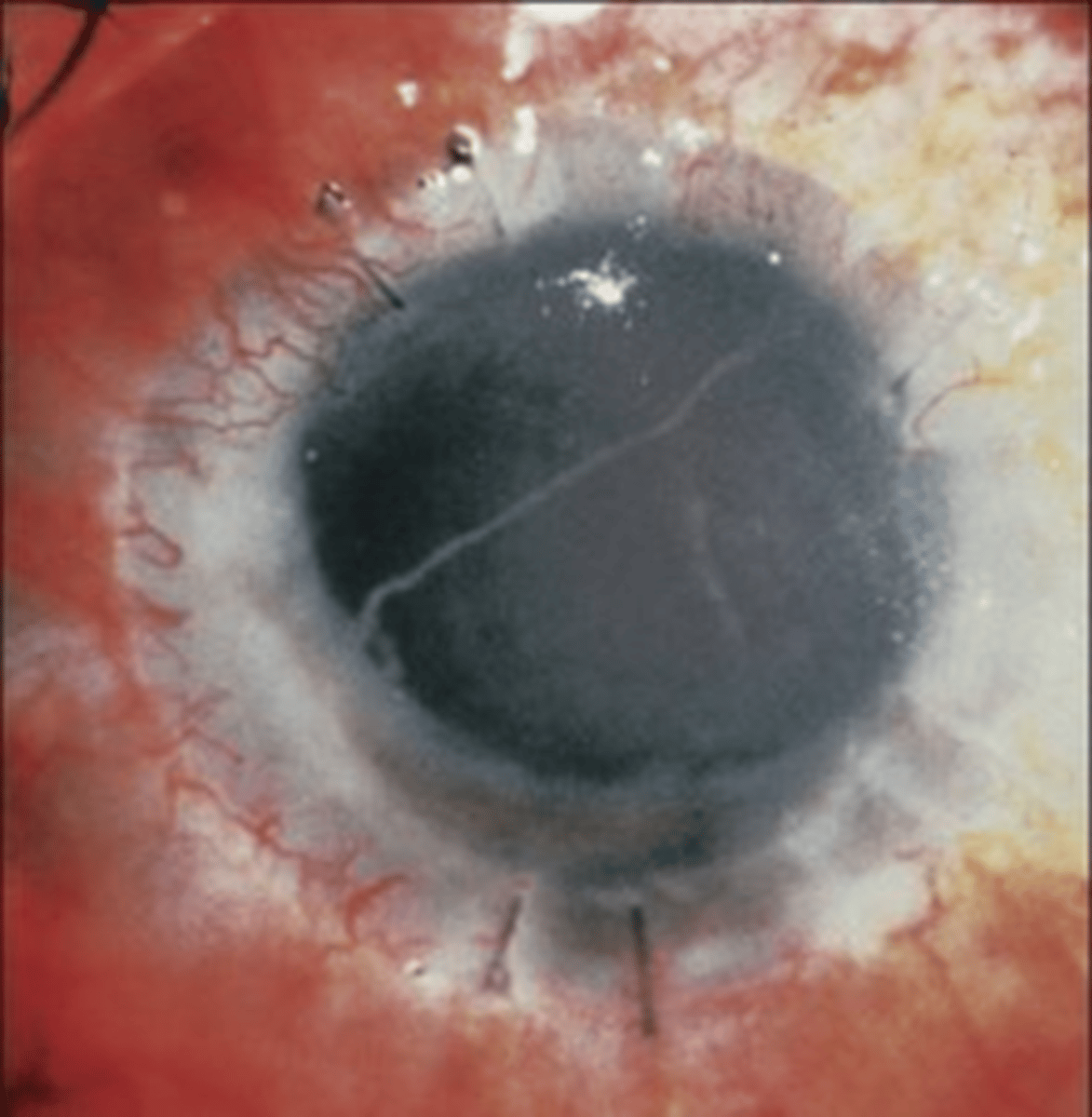
What indication for corneal transplant is seen here?
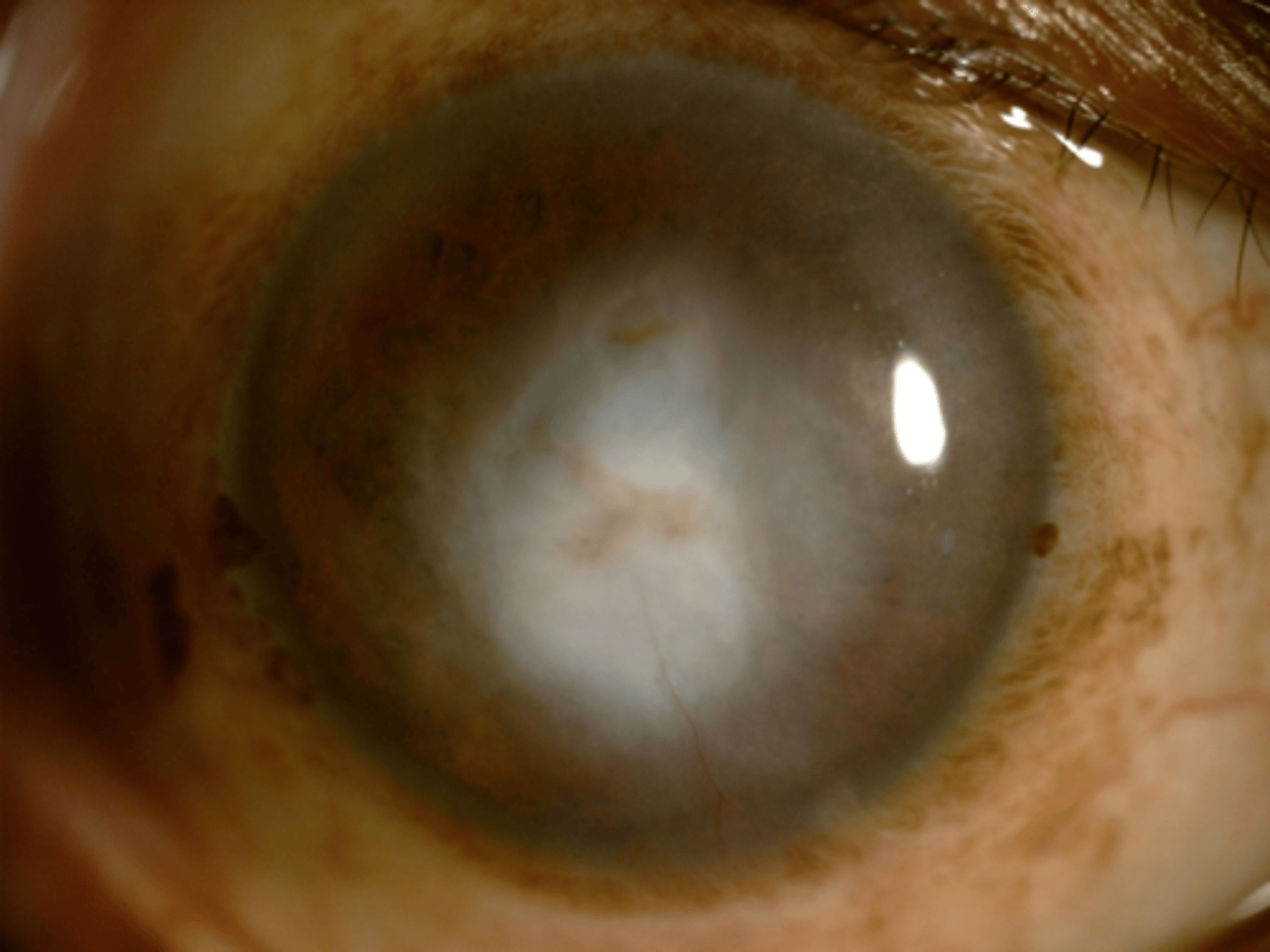
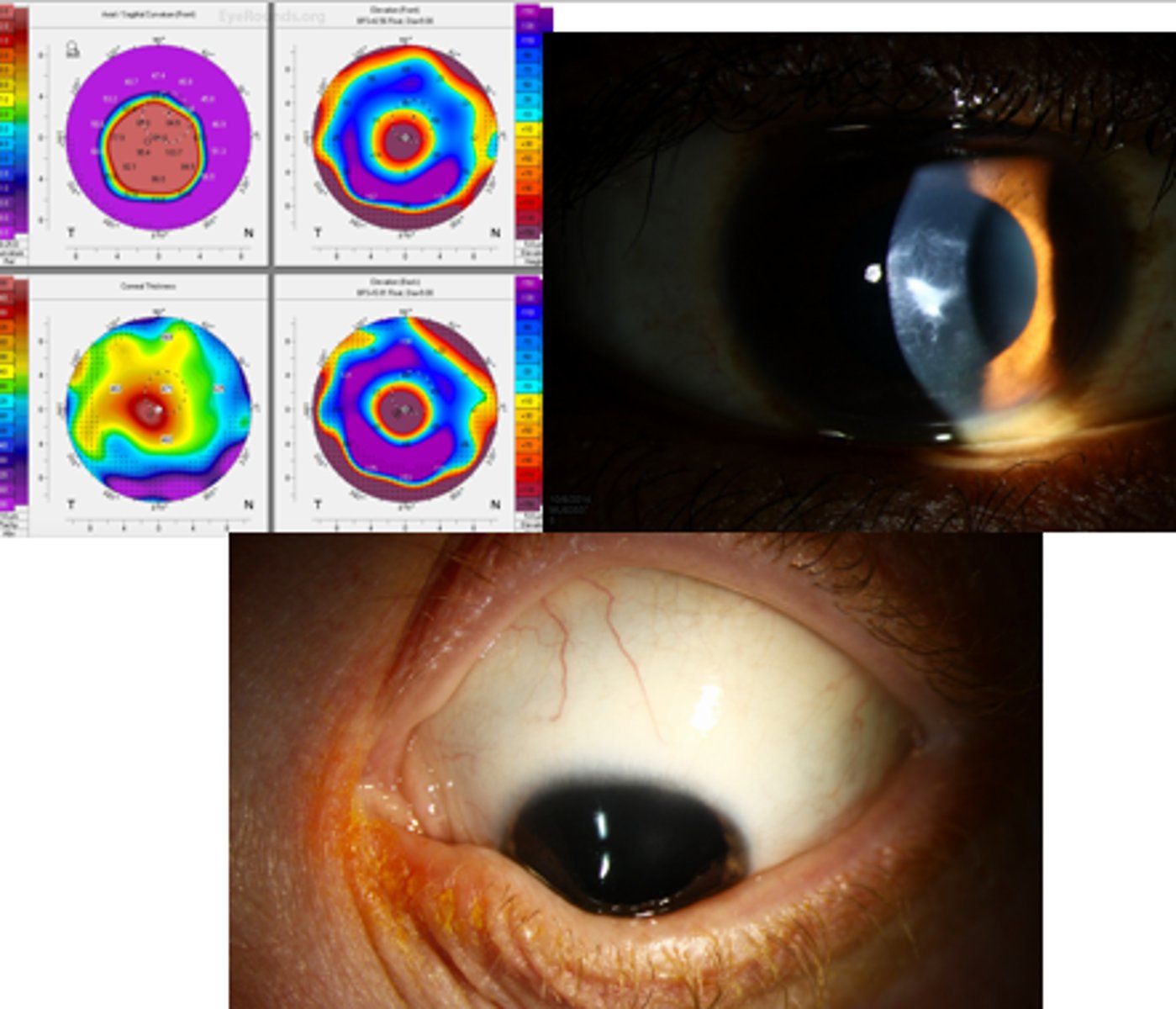
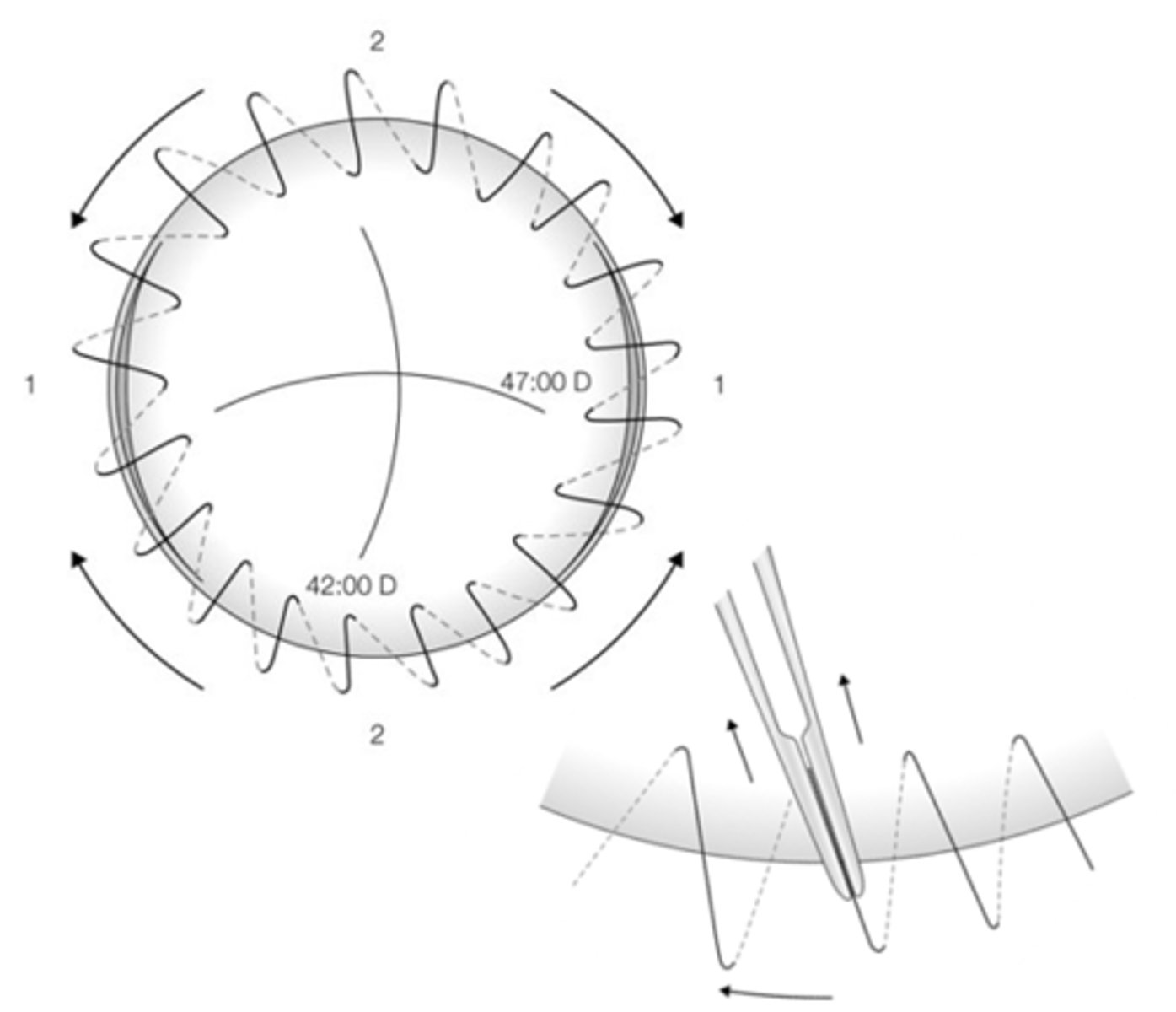
decreased vision from irregular astigmatism such as...
KCN
post-LASIK ectasia
post-RK
What indication for corneal transplant is seen here?
chronic eye pain from corneal disease
What indication for corneal transplant is seen here?

pupils - APD?
Maddox rod orientation
dilated PH acuity similar to CAT Sx
B scan to assess retina, vitreous, ONH
electrodiagnostics ERG, VEP
How can we determine expected visual outcome during pre-op evaluation?
confirm pain is due to corneal pathology
What do we want to consider with pain during pre-op evaluation?
abnormalities need to be treated surgically first = trichiasis, entropion, ectropion, lagophthalmos, symblepharon
What do we want to consider with eyelid health during pre-op evaluation?
significant neo, cicatrization, loss of limbal stem cells will increase risk of graft rejection = may benefit from keratoprosthetics device
What do we want to consider with ocular surface health during pre-op evaluation?
HSV Hx = start antivirals
inflam disease or graft failure Hx = start oral prednisone
corneal neo = start topical steroid
What do we want to consider with prophylactic medications during pre-op evaluation?
is pt able to comply with maintaining head position, using medications, follow-up visits for life
What do we want to consider with post-op compliance during pre-op evaluation?
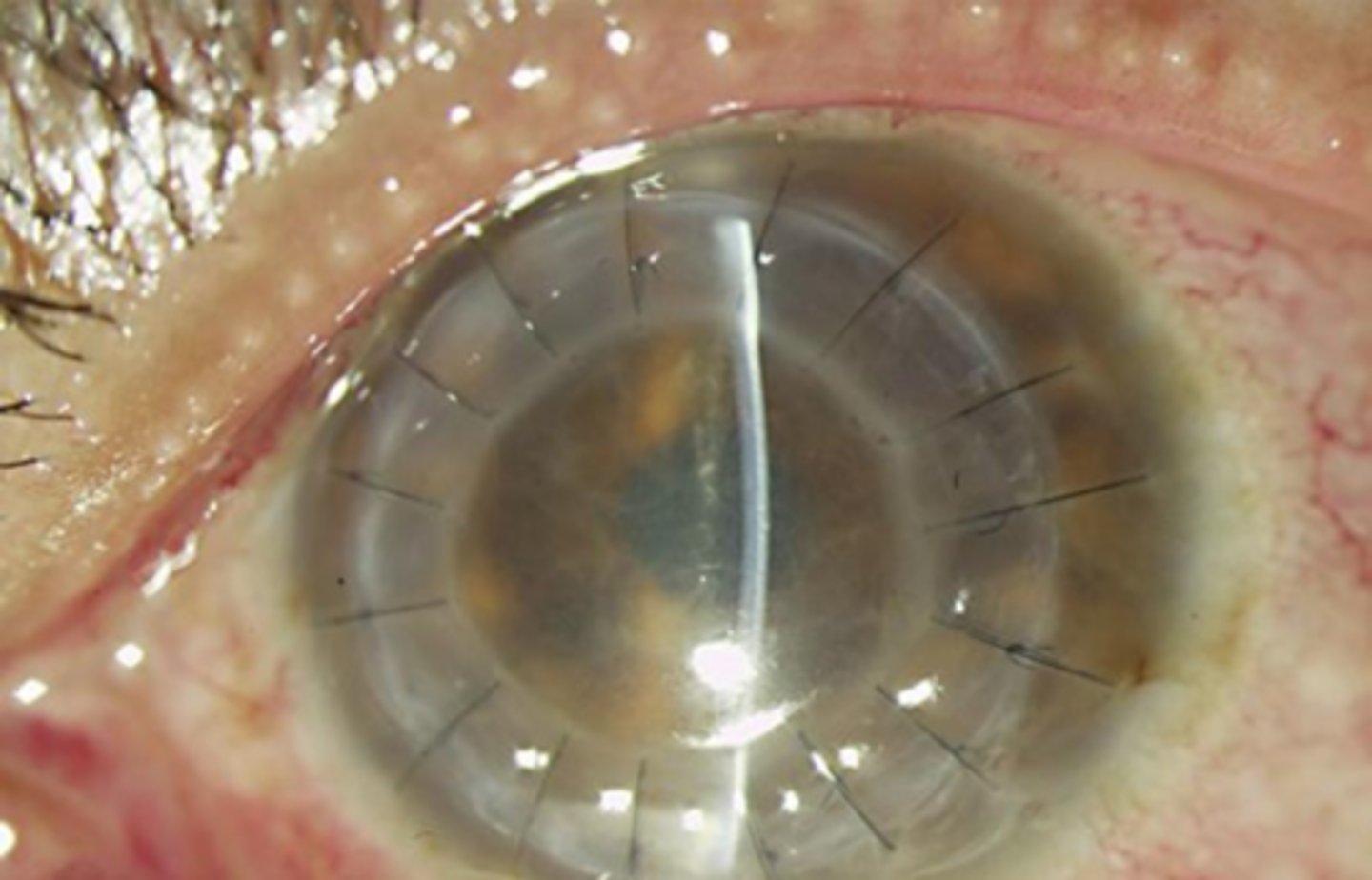
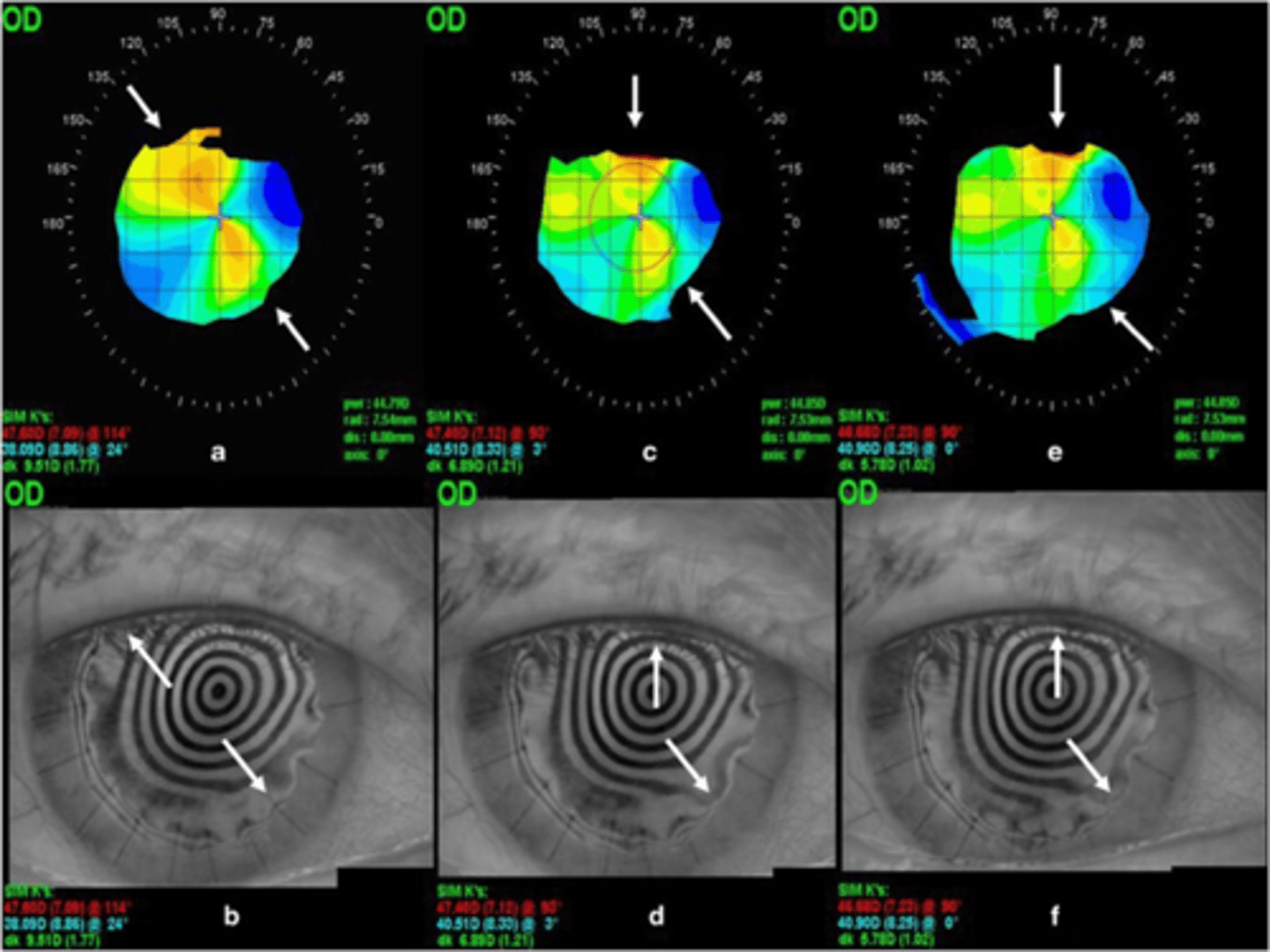
full thickness keratoplasty of all layers with "open sky" = eye is completely open while circular button is removed
What is a penetrating keratoplasty (PKP)?

monitored anesthesia care with sedation, topical anesthetics, retro or peribulbar block - rarely general anesthesia
What type of anesthesia is used for PKP?

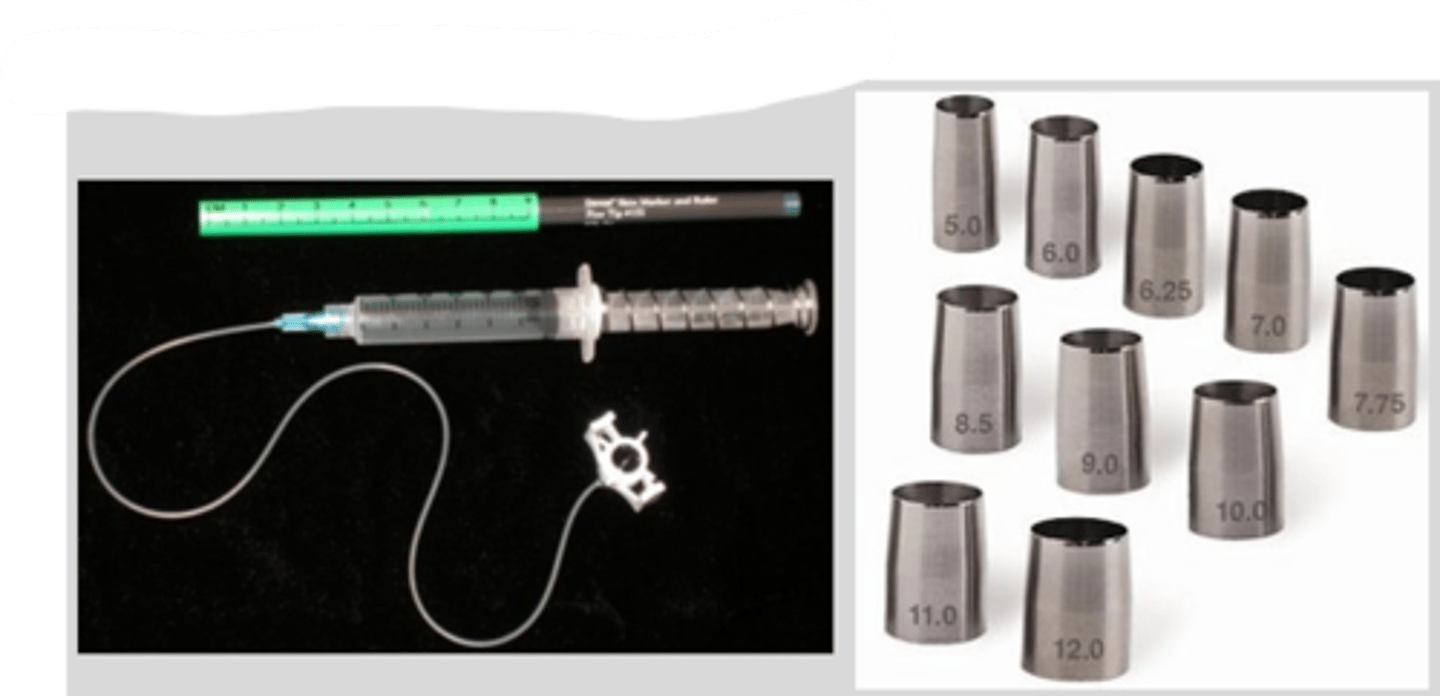
corneal trephine = basically like a donut hole maker
corneal scissors finish off
What is mostly commonly used to make the full thickness cut in PKP?
femtosecond laser
What is alternatively used to make the full thickness cut in PKP?
7.75 to 8.50mm diameter = graft is typically 0.25-0.50mm larger than recipient's opening
How large are the grafts typically in PKP?
promote more astigmatism bc sutures closer to visual axis
What is the downside of smaller grafts used in PKP?
higher risk for rejection bc closer to limbal vessels
What is the downside of larger grafts used in PKP?
quicker
less astigmatism early in healing
What are the 2 pros of a continuous suture used in PKP?
suture can break or abscess = difficult to fix bc need to replace entire line = not common anymore today
What is the con of a continuous suture used in PKP?
best for corneal neo
good for peds, mentally impaired, obese pt's bc easier to fix any ruptures from eye rubbing, etc.
What are the 2 pros of 16-30 interrupted sutures used in PKP?
induces more astigmatism initially
What is the con of 16-30 interrupted sutures used in PKP?
VA typically poor
assess graft for edema, abrasions/defects
sutures should have junctional integrity (-)Seidel
AC depth and rxn
IOP with iCare or NCT = NO Goldmann for several weeks
What exam components should be performed at the 1 day post-op for a PKP?
high IOP if retained viscoelastic
low IOP if hypotony/wound leak
Why might we see high vs low IOP post-op with PKP?
abx broad spectrum x 2 weeks
steroid QID like Pred forte, Durezol x 1 month, then slow monthly taper to qday for life
topical and/or oral immunosuppressive
What are the 3 post-op medications dictated by the surgeon for PKP?
NO rubbing
NO bending or Valsalva movements
shield while sleeping x2 weeks
eye protection at all times
NO water in eye
clean environments (avoid dust, dirt, smoke)
What some important post-op pt limitations we need to educate on?
VA still may be poor
ASeg - assess graft, sutures, AC
IOP with iCare or NCT
fundoscopy may be difficult
What exam components should be performed at the 1 week post-op for a PKP?
S/S of graft rejection and to RTC asap to avoid graft failure = pain, decreased vision, redness, photophobia
In addition to the post-op limitations, what is 1 other thing we should educate our pt on at the 1 week post-op for a PKP?
VA
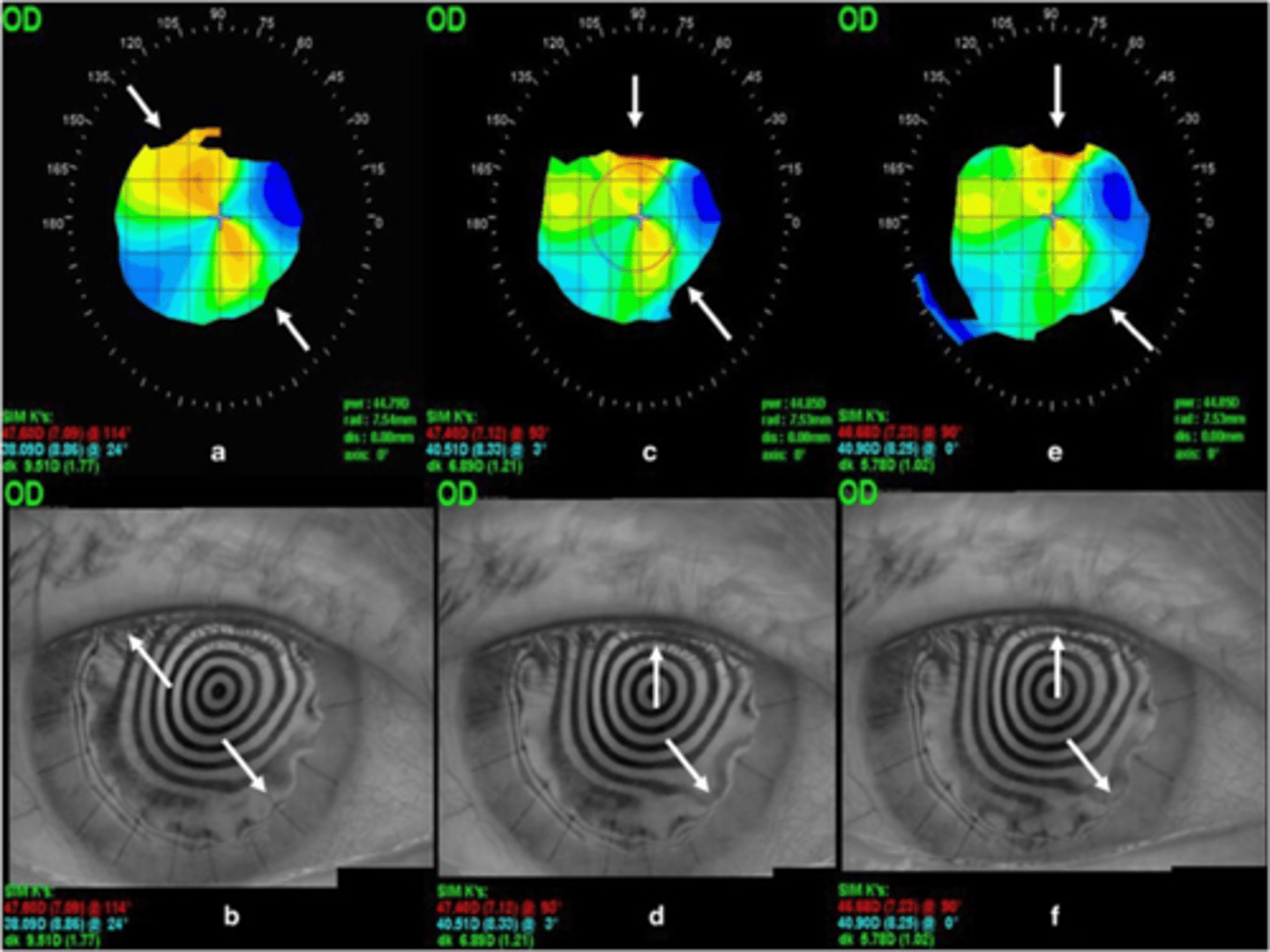
refraction and topography
ASeg - assess graft, sutures, AC - esp concerned with edema, surface integrity
IOP with iCare or NCT
fundoscopy
What exam components should be performed at the 1 month post-op for a PKP?
1 month post-op
When can a pt begin activity and light exercise after PKP?
3 months
For how long should we monitor astigmatism before making adjustments after PKP?
donor/host tissue
underlying disorder = KCN, PMD
placement of trephination
graft size
donor and host corneal thickness disparity
suturing technique
post-op wound healing, inflammation, medications, vascularization
What can affect the astigmatism changes after PKP?
5D or more
15-31% of post-PK patients will develop at least how much astigmatism?
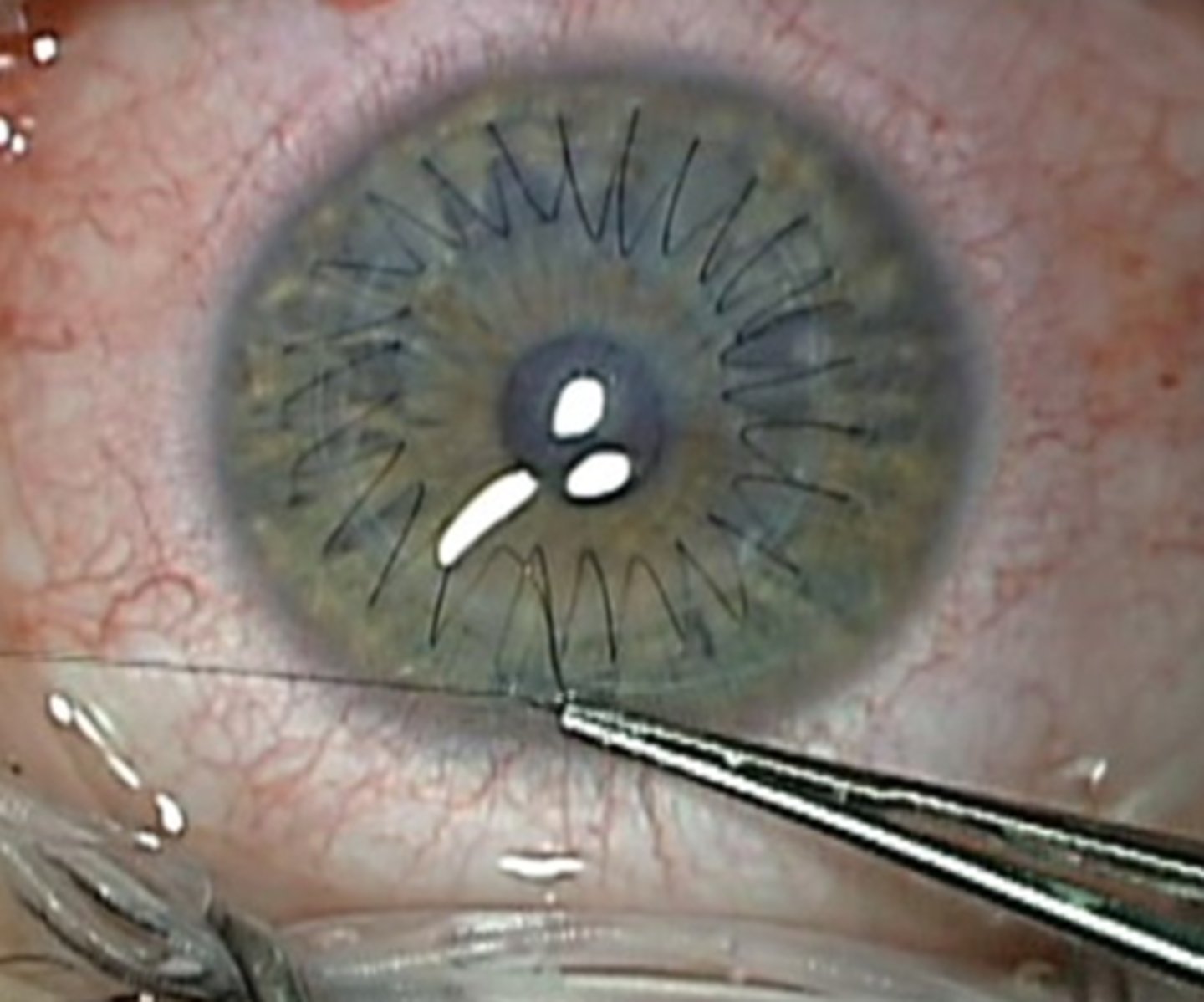
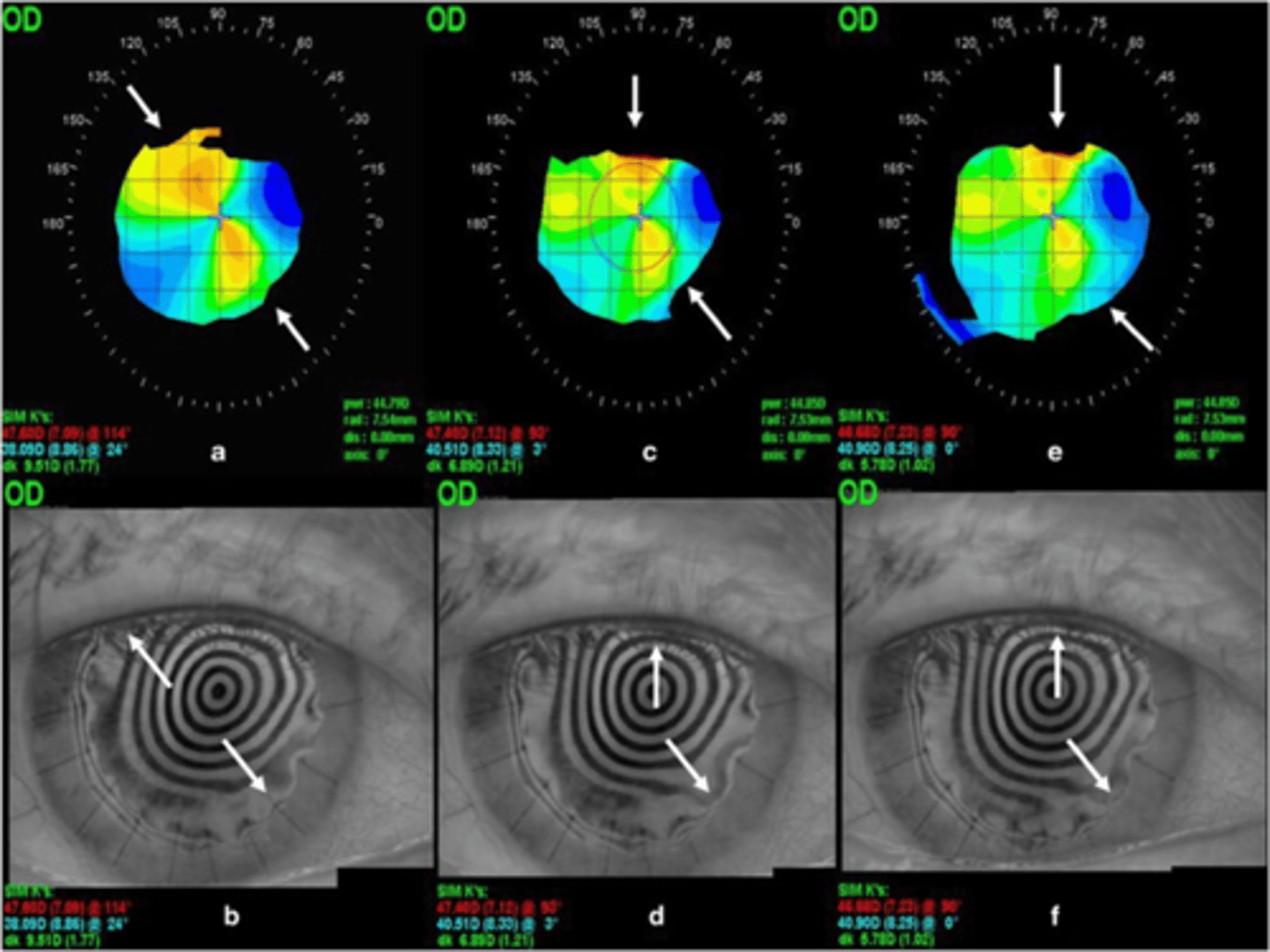
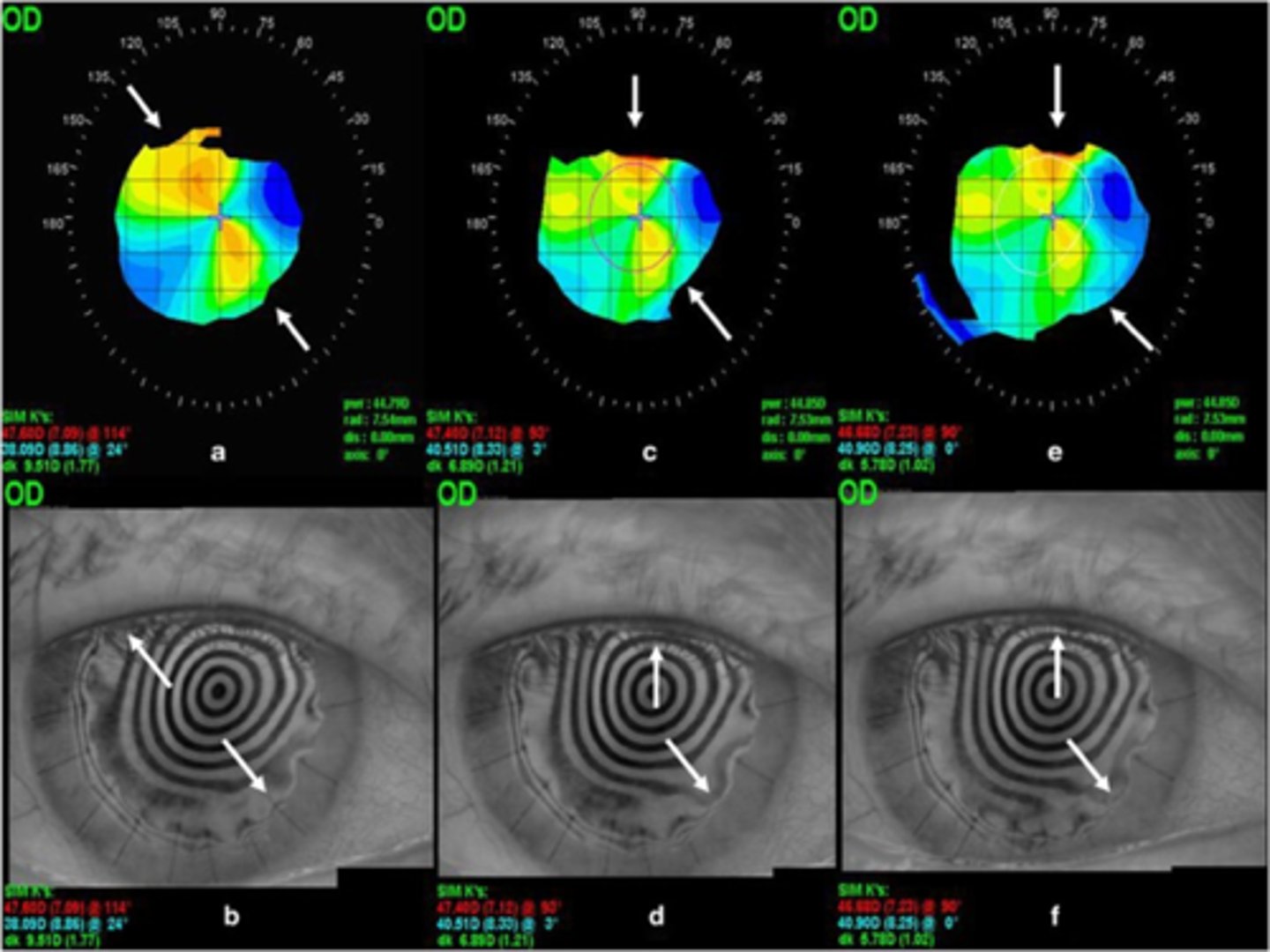
use refraction and topography to determine steep axis = remove 1-2 sutures at a time along the steep axis = relaxes/flattens that axis
How can we manage/tweak astigmatism after PKP with interrupted sutures (more common)?
use refraction and topography to determine steep axis = loosen suture tension along the steep axis = relaxes/flattens that axis
NOTE: be careful not to cut or else entire suture must be removed
How can we manage/tweak astigmatism after PKP with continuous sutures (less common)?
opposite
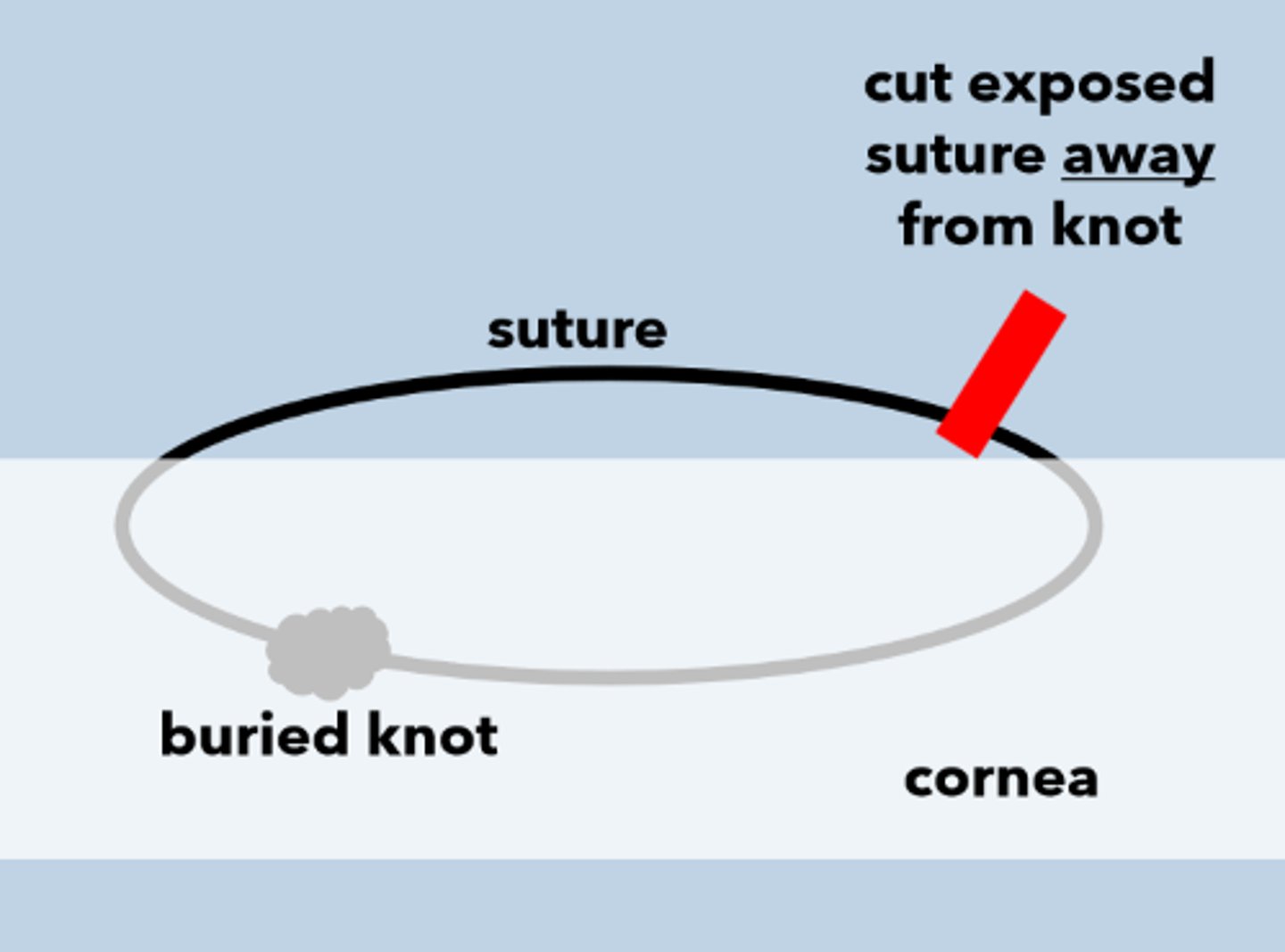
When we remove sutures after PKP, the pt needs to look in the ________________ direction of the suture being removed.
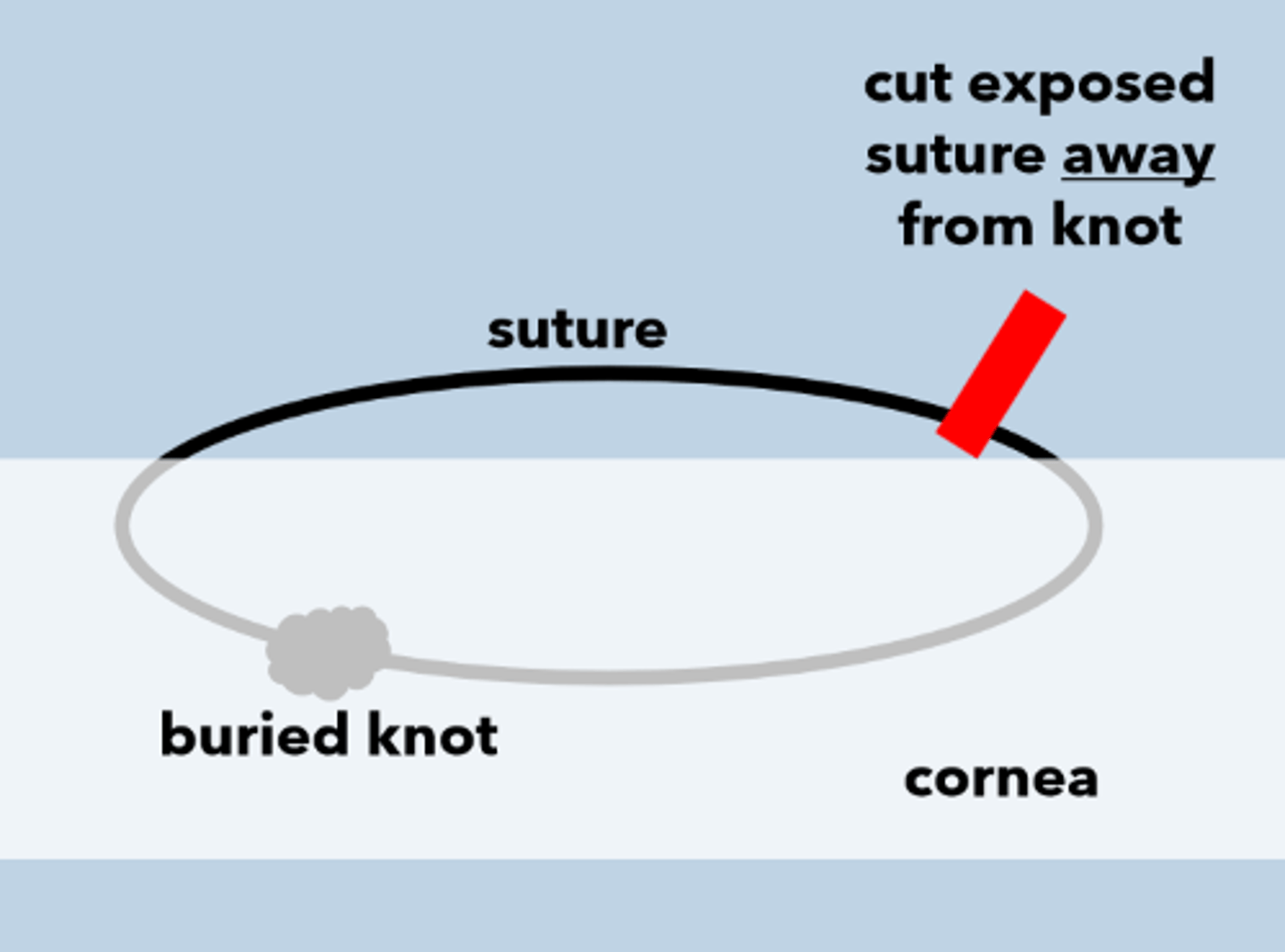
proparacaine OU +/- povidine-iodine 5%
26 gauge needle or beaver blade inserted under suture, bevel up
cut suture away from knot with a bold, steady motion
forceps to grab long end of suture and tug gently
instill and Rx abx
Explain the process for removing sutures after a PKP.
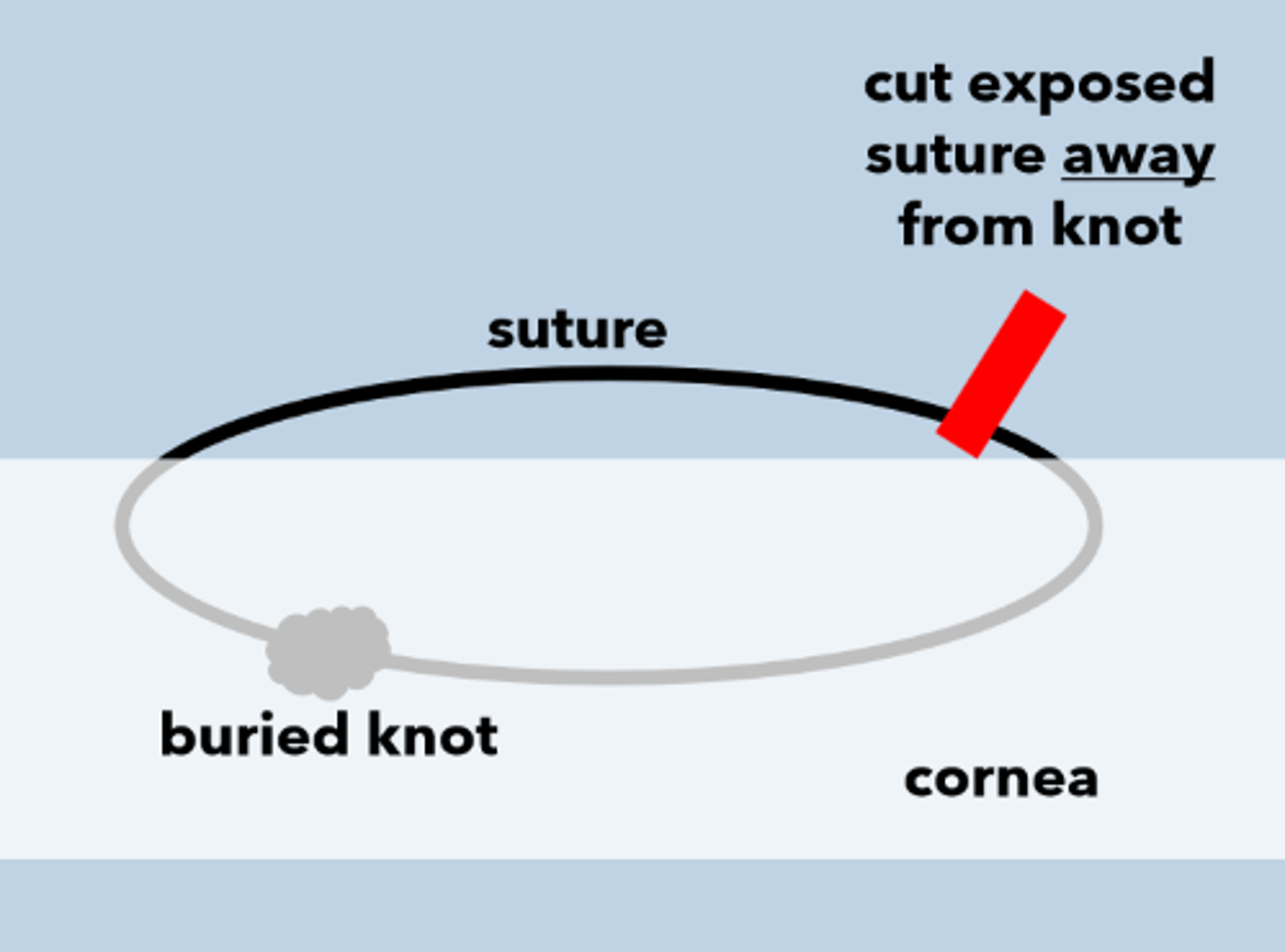
limit how far the knot travels in the cornea
AND
limit how much of the exposed suture enters cornea
When removing a suture after PKP, we want to limit which 2 things?
relaxing incision in the steep meridian if < 6D
relaxing incision with compression suture(s) in the flat meridian if > 6D
toric ICL
RLE with toric IOL
femtosecond incisions
PRK with mitomycin-C (better than LASIK)
wedge resection = remove tissue from certain quadrants
regraft
If adjusting sutures does not adequately adjust astigmatism after PKP, what other techniques can we use?
80-90%
According to Lam and Reza (2009), PKP is the most successful solid tissue transplant procedure with a success rate of up to ______%.
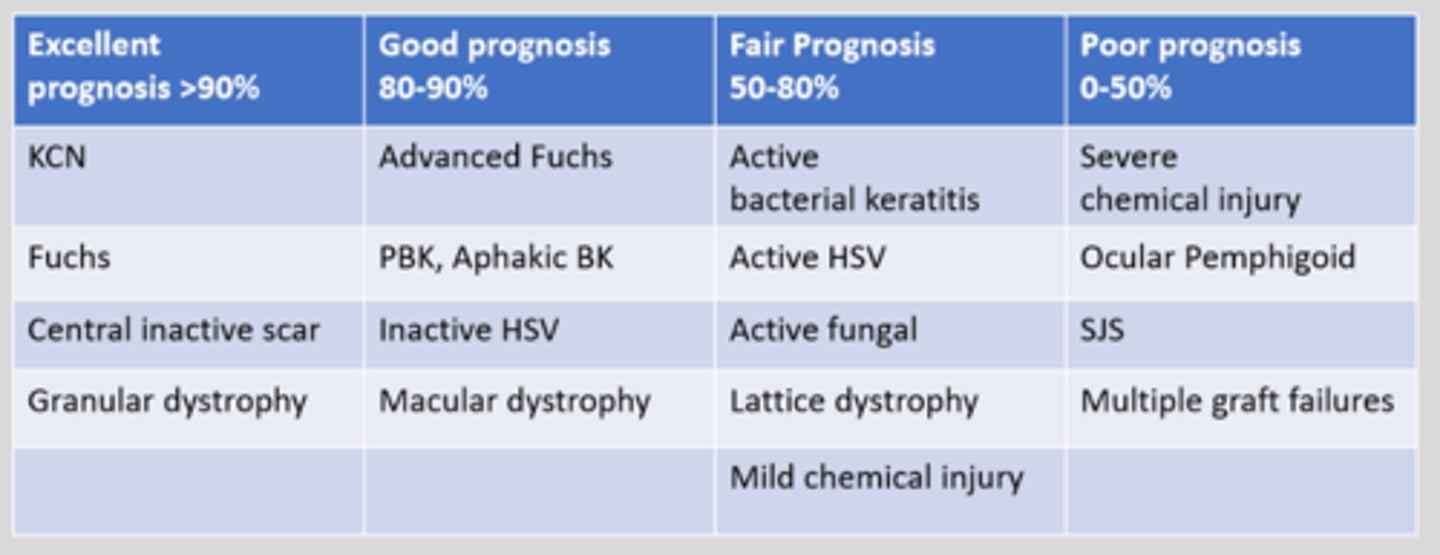
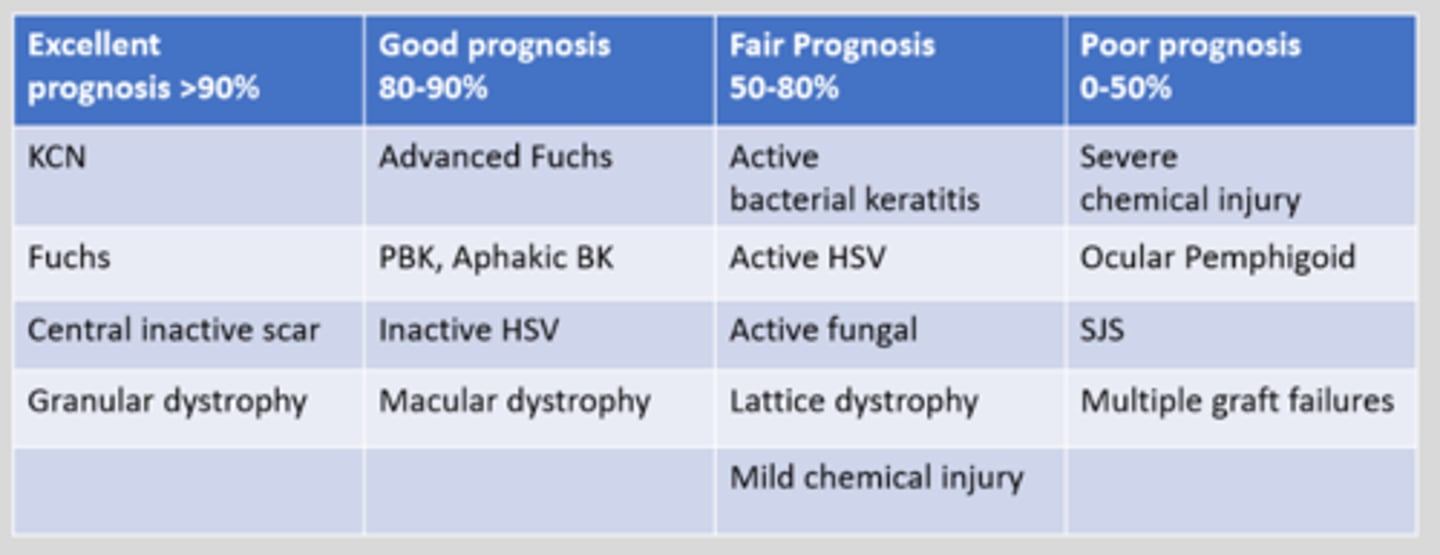
KCN
Fuch's
central scar
granular dystrophy
According to Lam and Reza (2009), which 4 pre-op conditions have an excellent prognosis >90% for PKP?
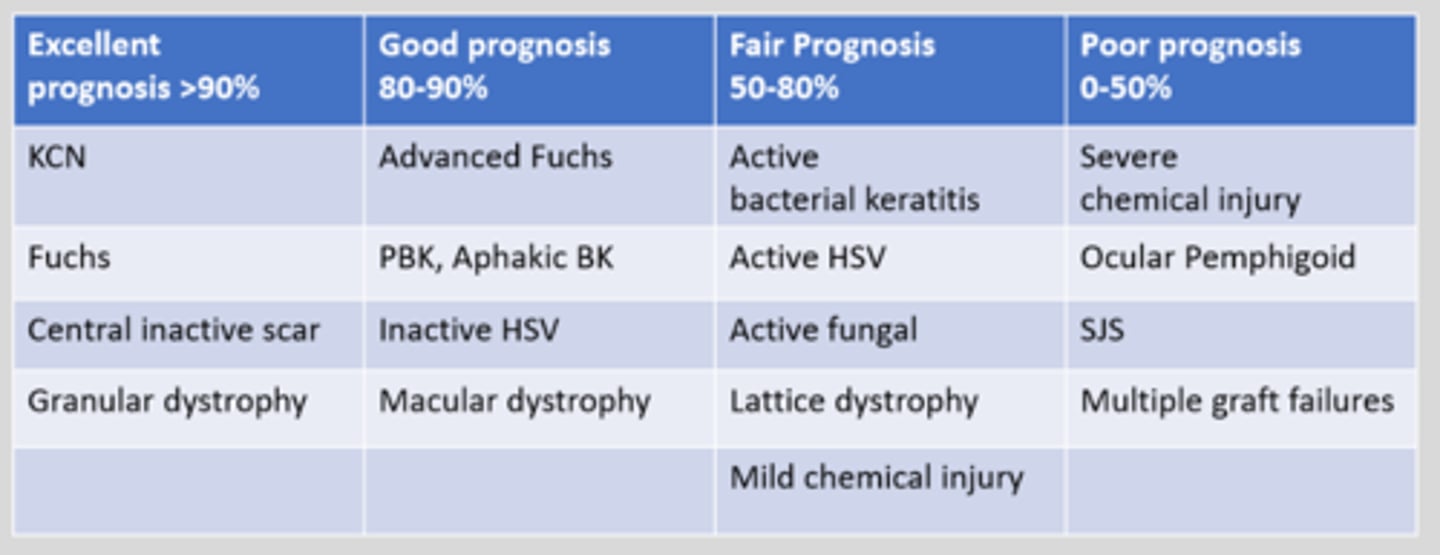
advanced Fuch's
PBK or aphakic BK
latent HSK
macular dystrophy
According to Lam and Reza (2009), which 4 pre-op conditions have an good prognosis 80-90% for PKP?
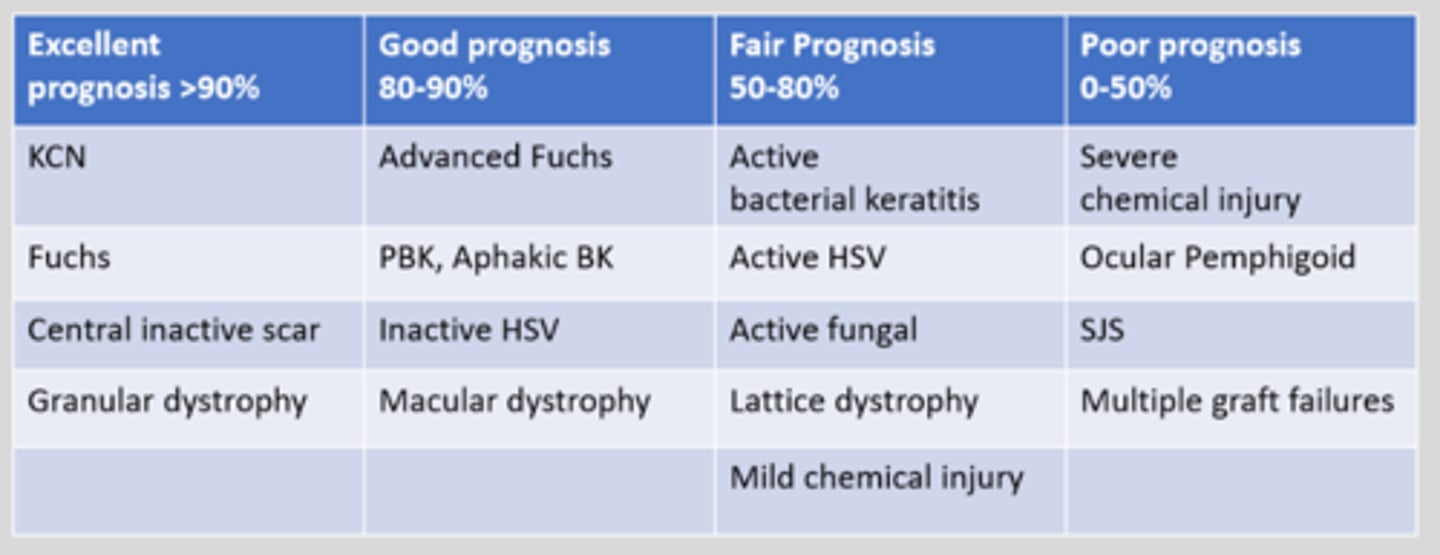
active bacterial keratitis
active HSK
active fungal infection
lattice dystrophy
mild chemical injury
According to Lam and Reza (2009), which 5 pre-op conditions have an fair prognosis 50-80% for PKP?
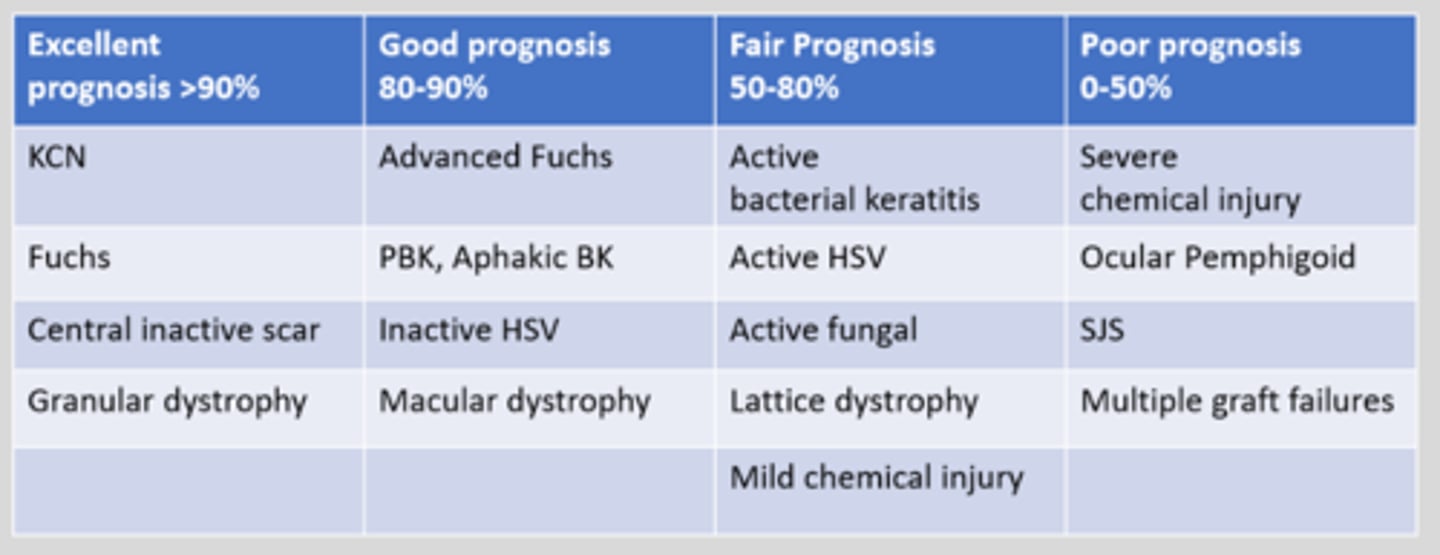
severe chemical injury
OCP
SJS
multiple graft failures
According to Lam and Reza (2009), which 4 pre-op conditions have an poor prognosis 0-50% for PKP?
immunologic response of host to the donor tissue = graft is clear for 2 weeks after surgery, then becomes edematous with KP's on graft only, neo, infiltrates, Khadadoust endo rejection line, epi rejection line, SEIs
What is graft rejection, a complication of PKP?
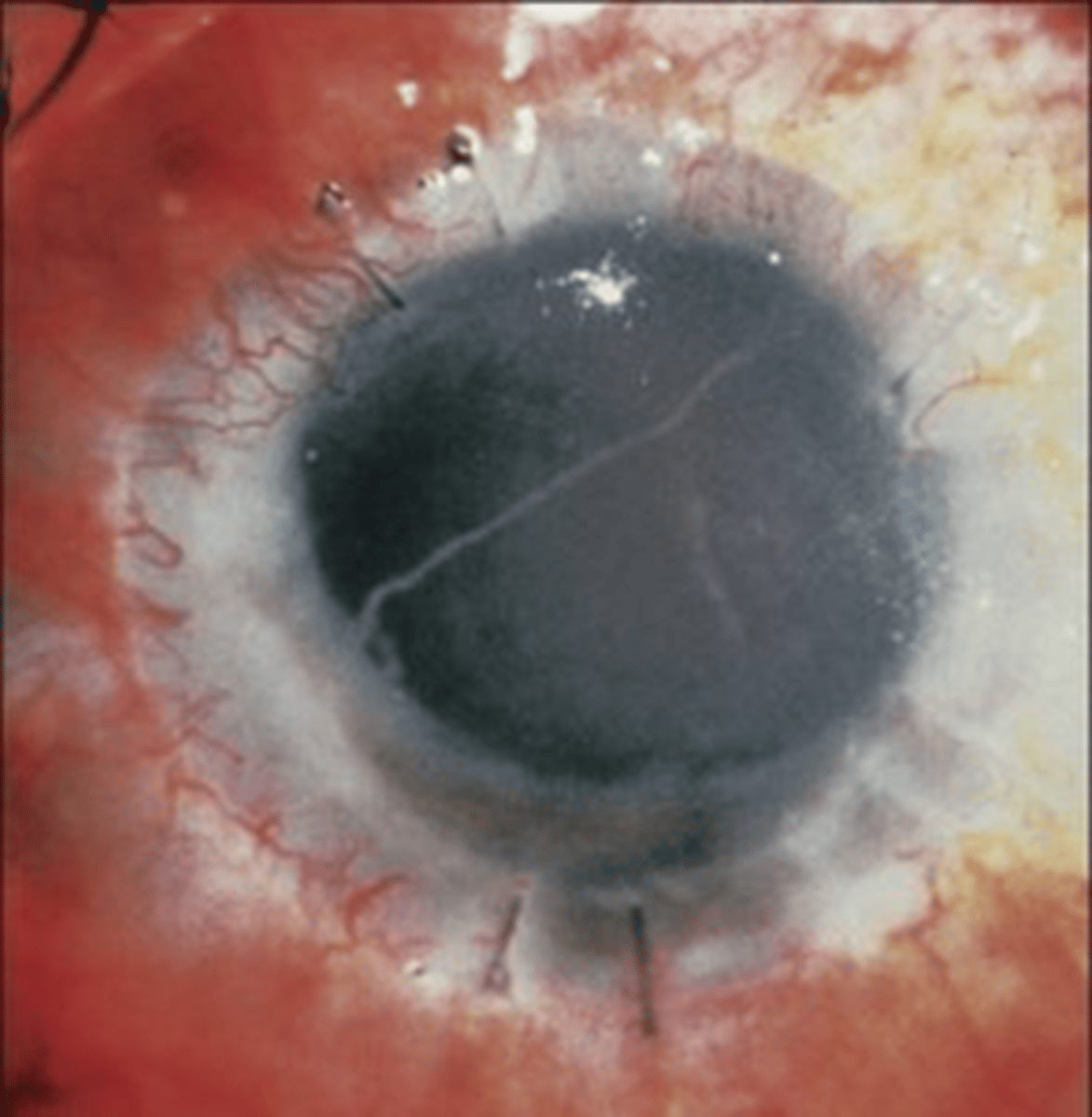
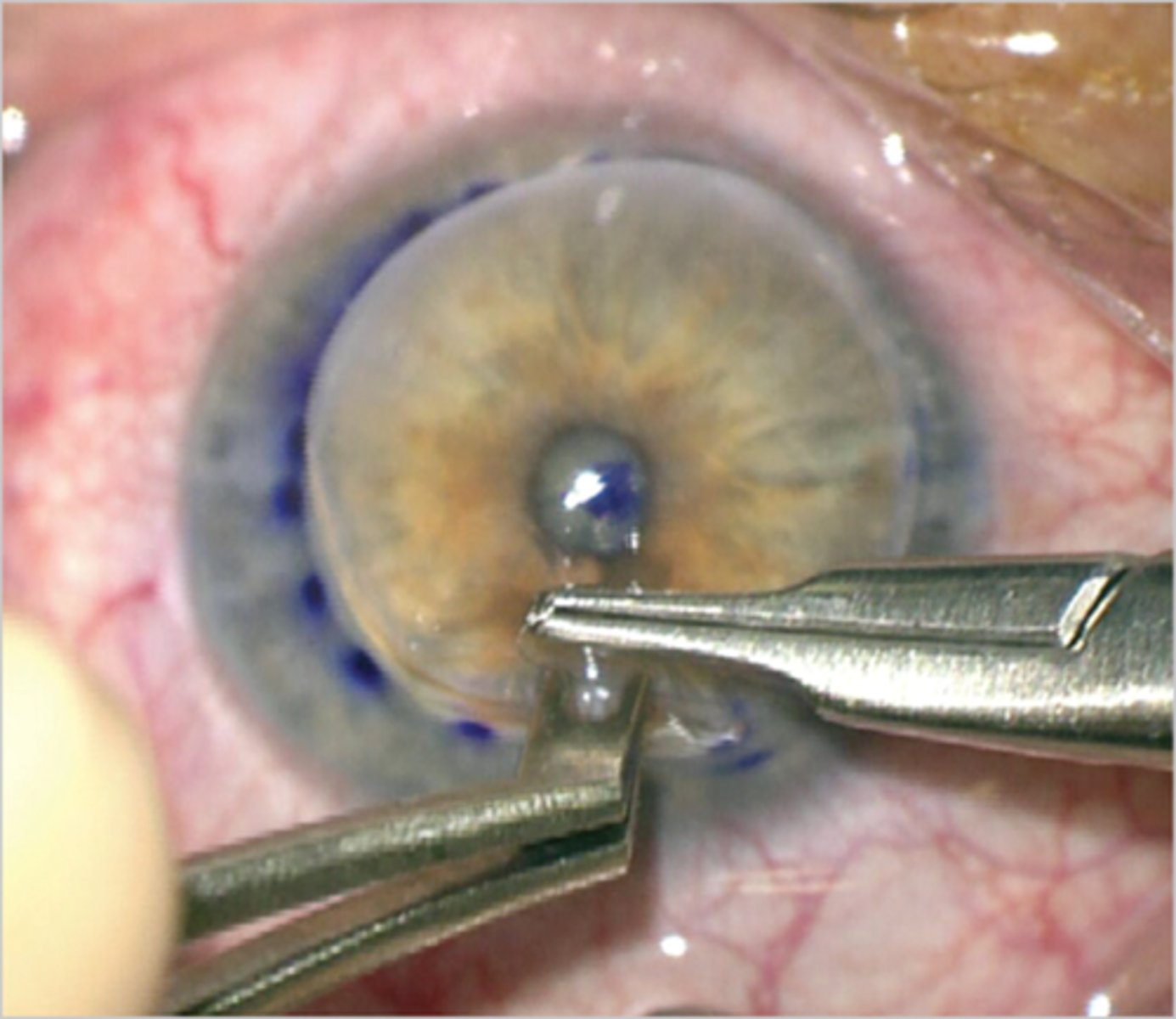
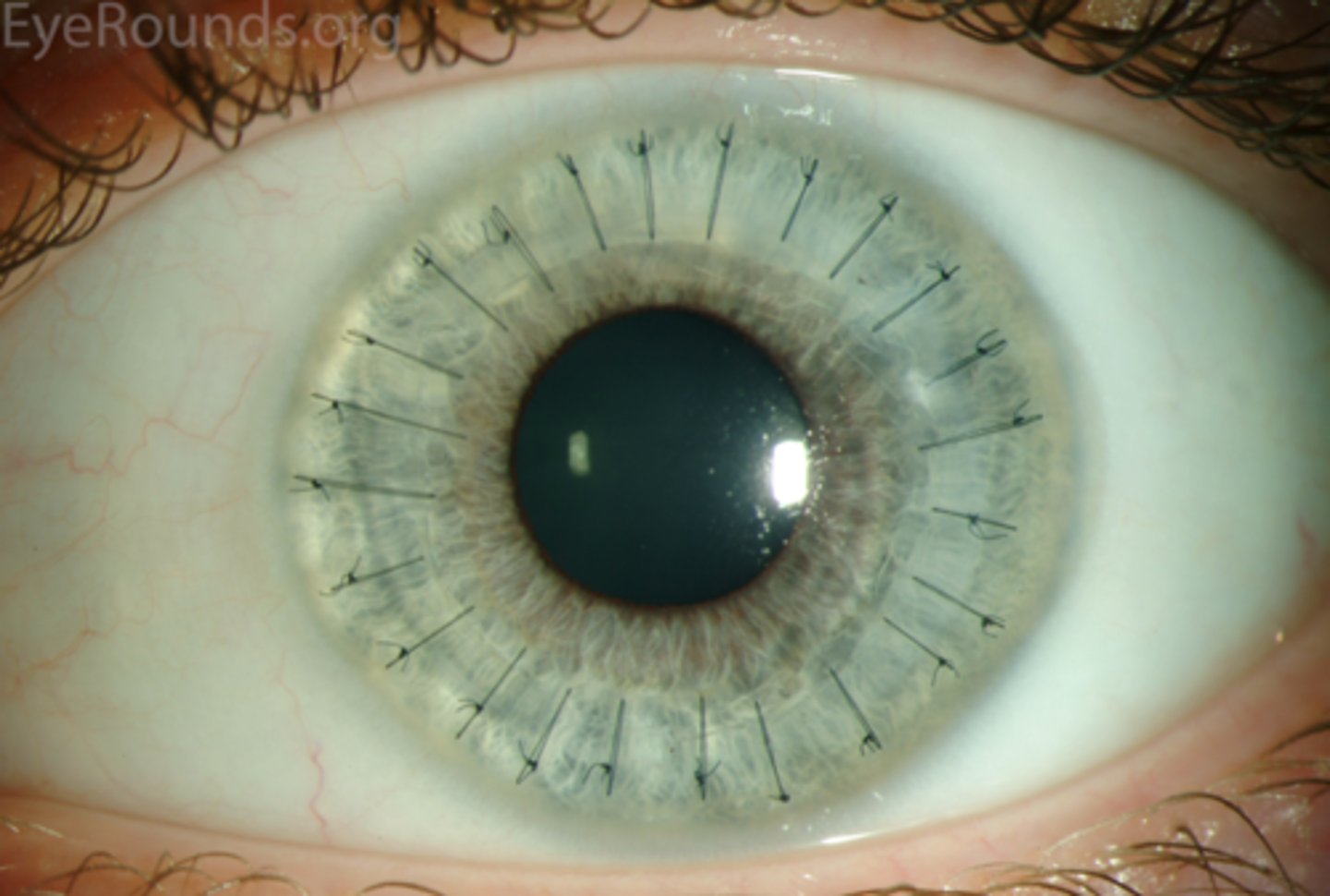
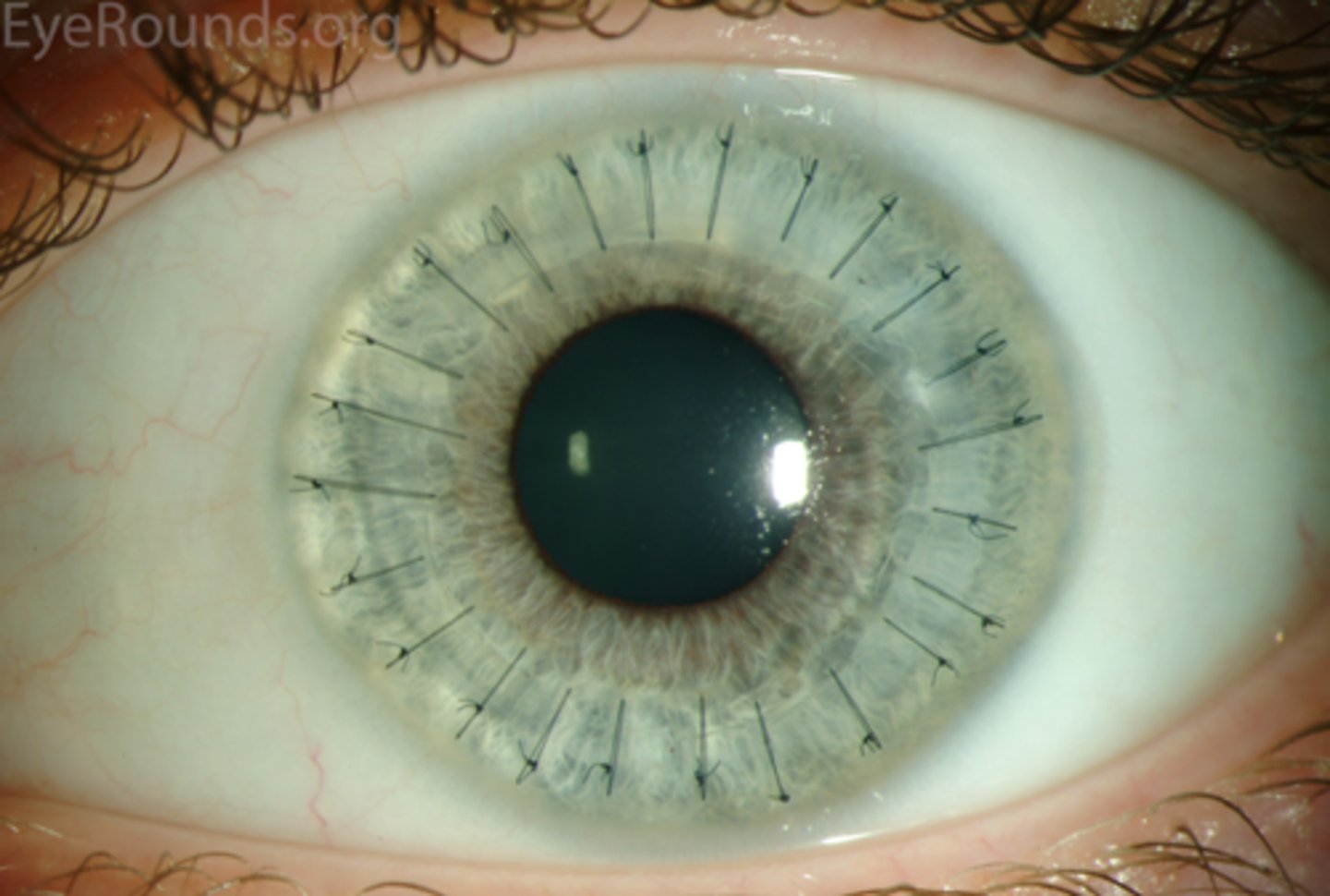
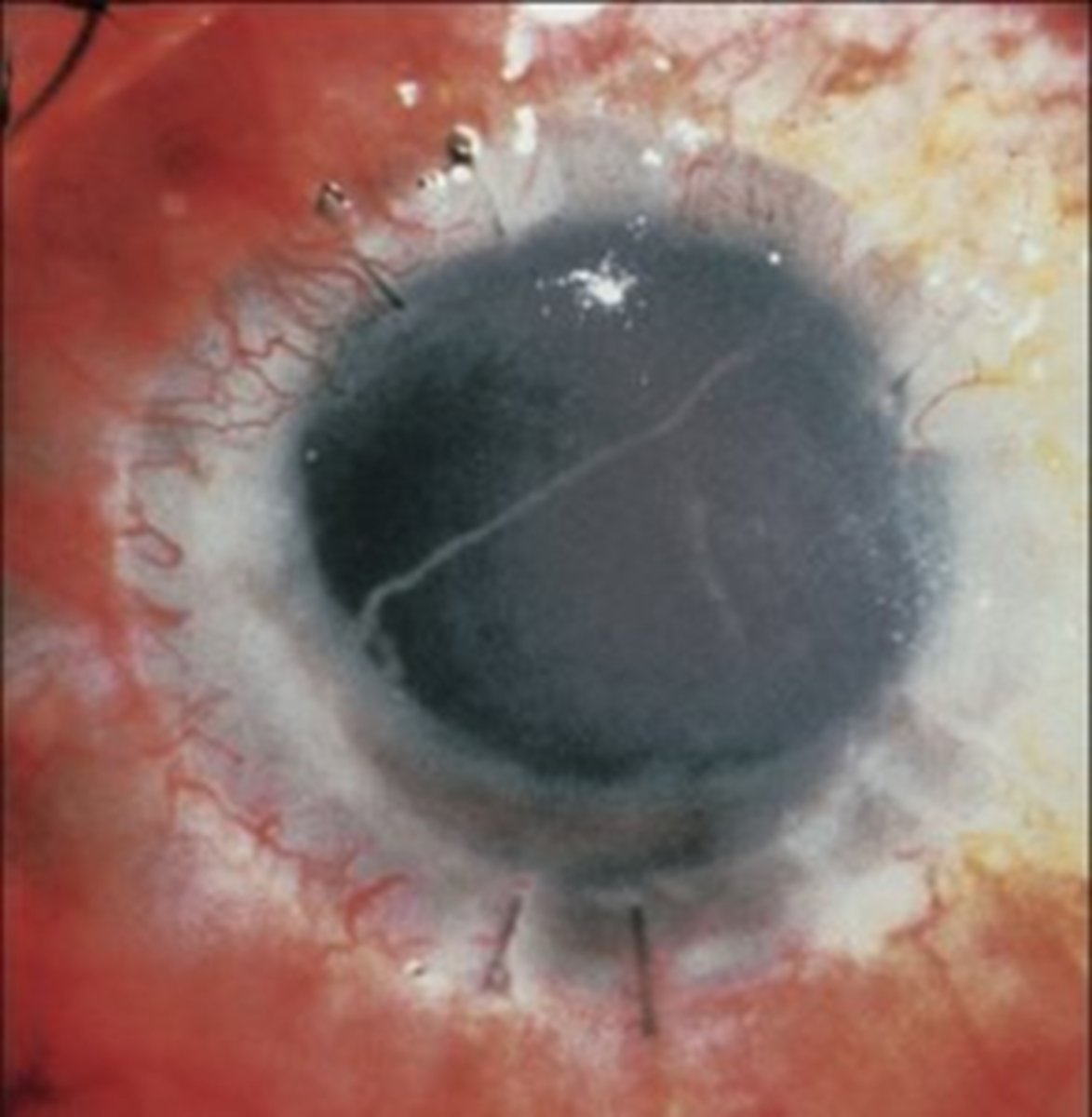
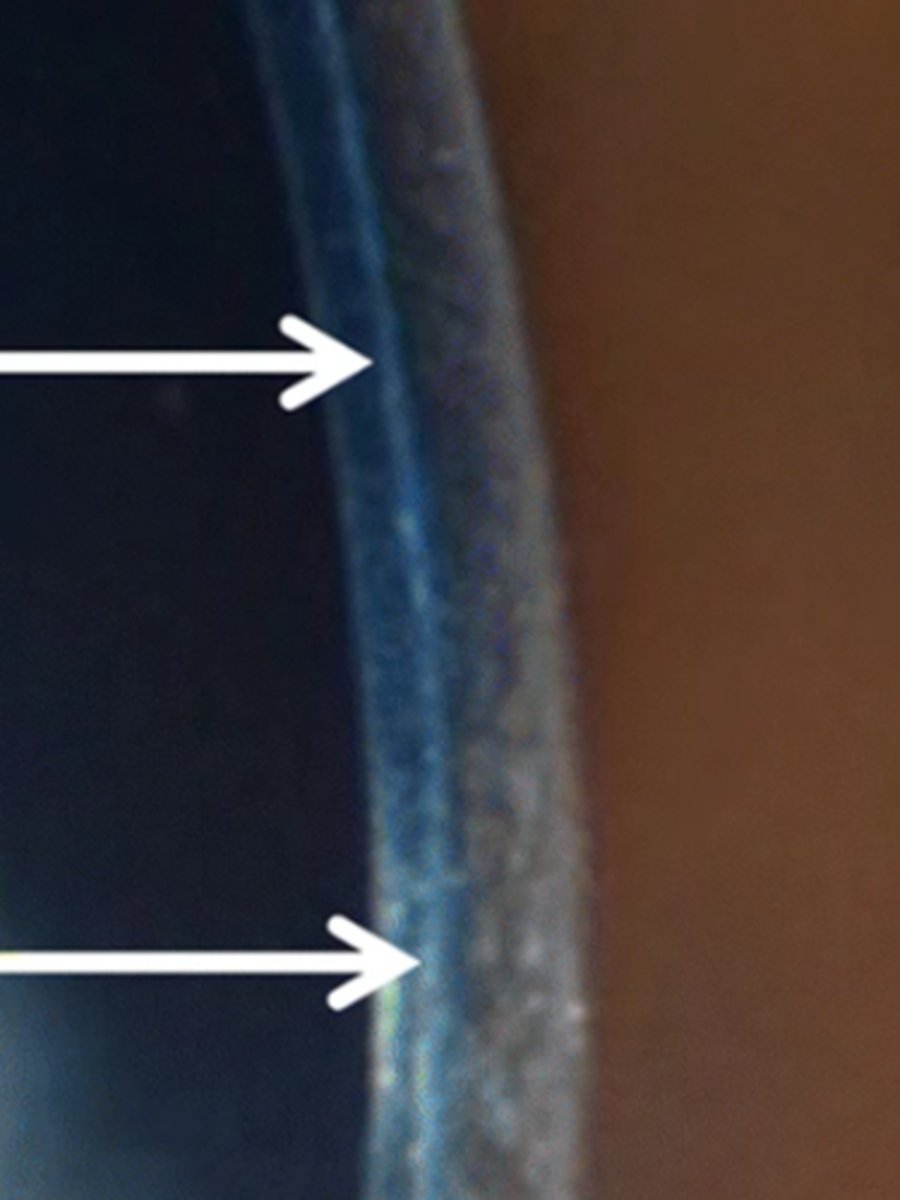
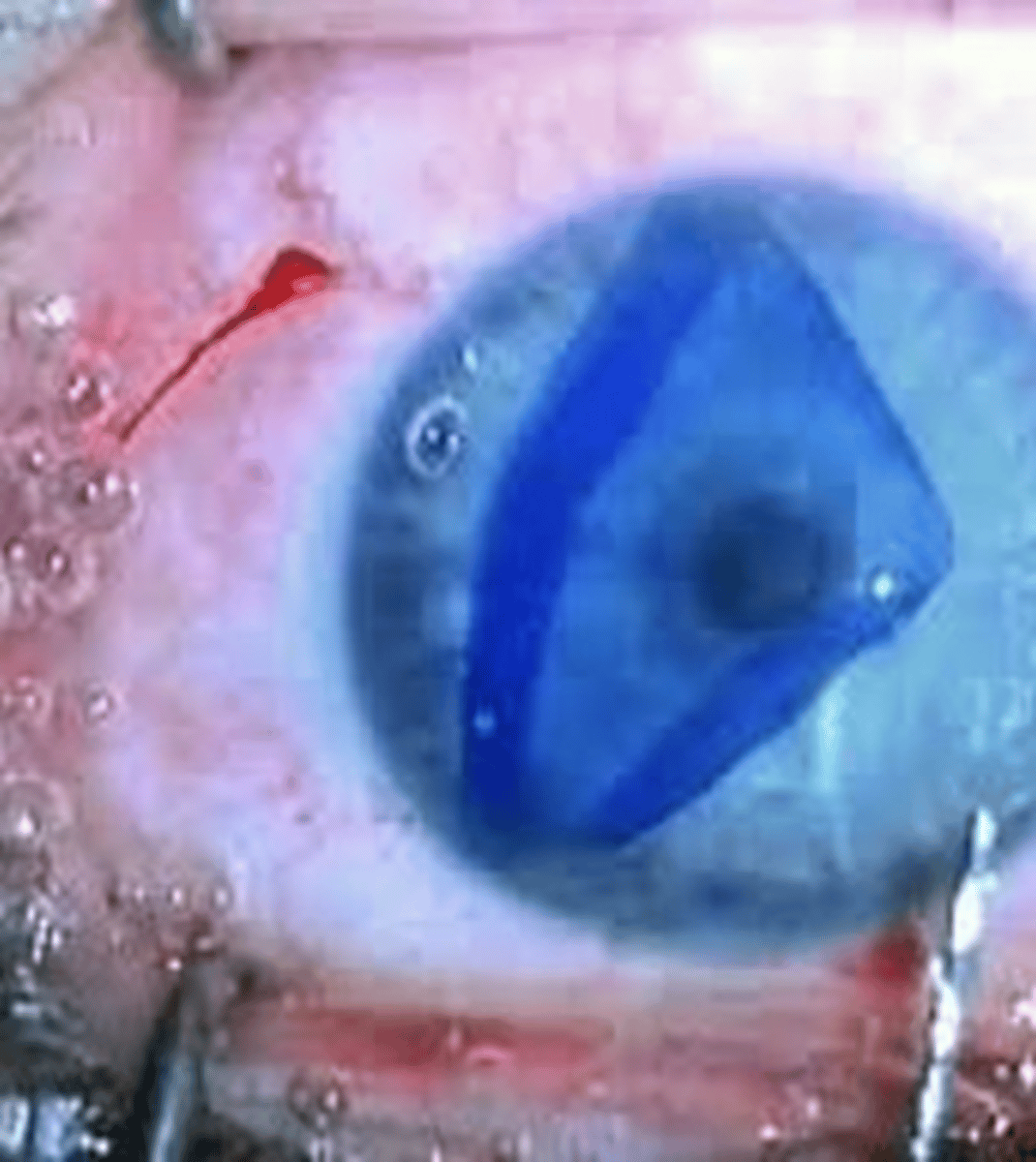
stromal infiltrates
What sign of graft rejection, a complication of PKP, is seen here?
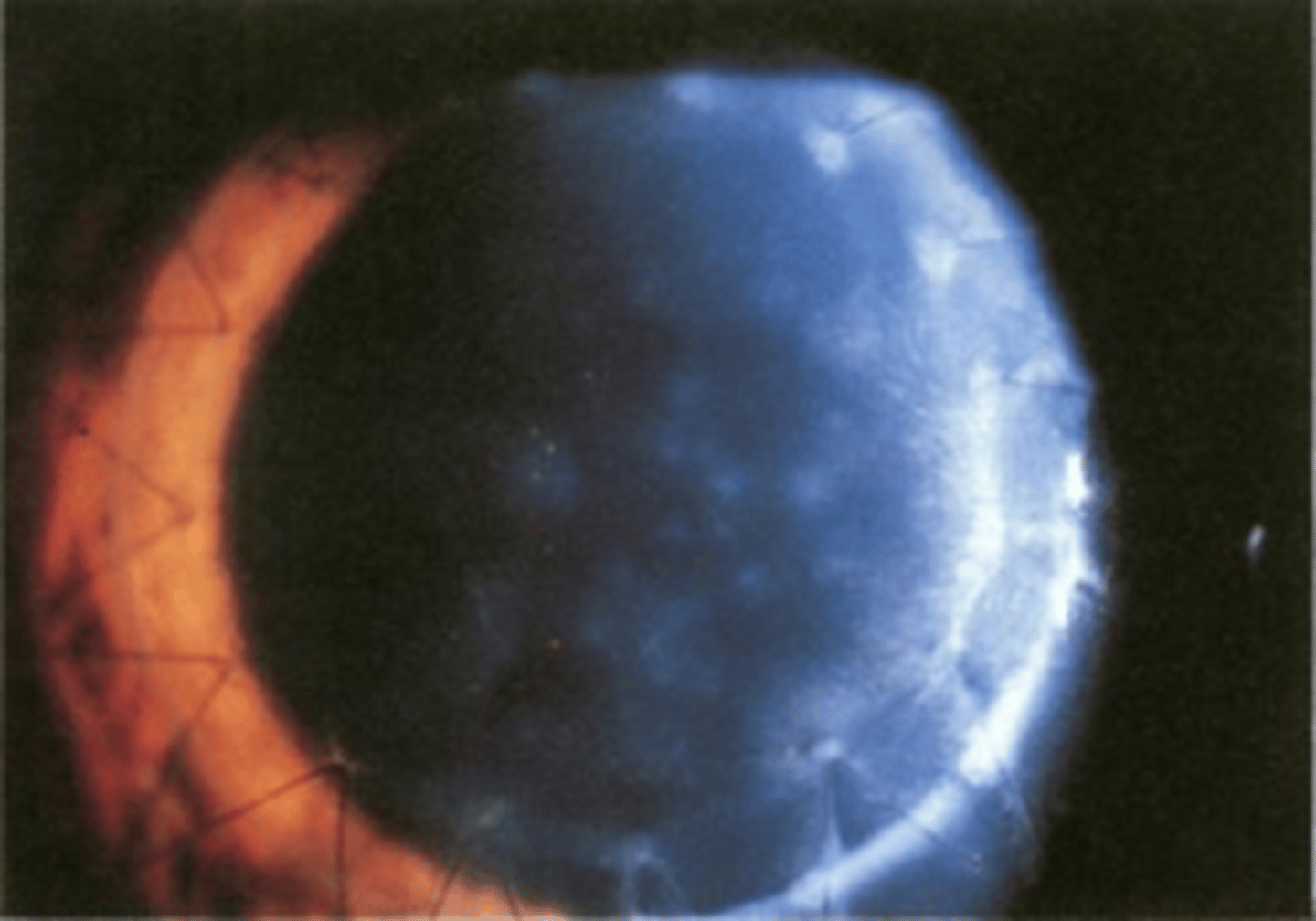
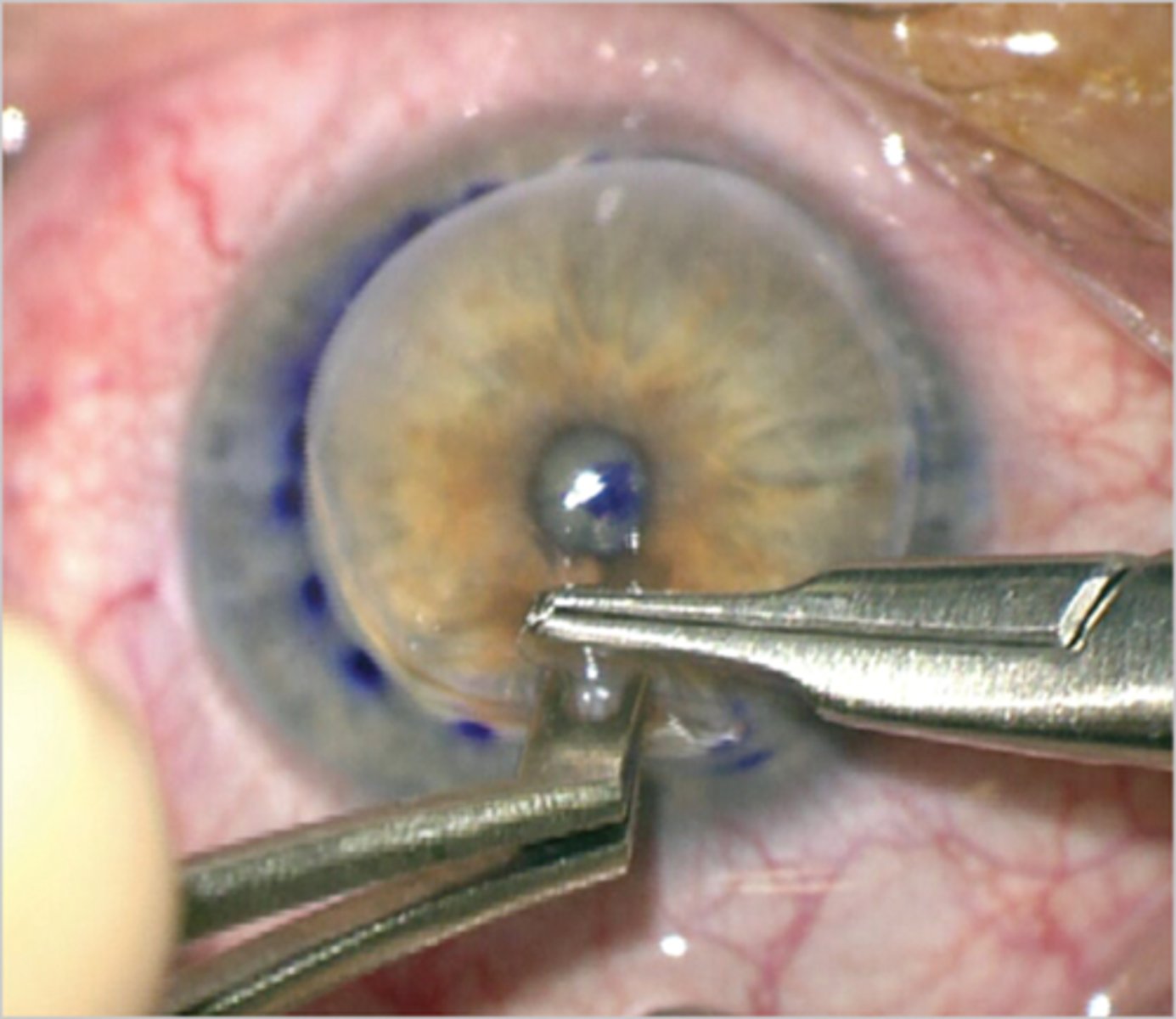
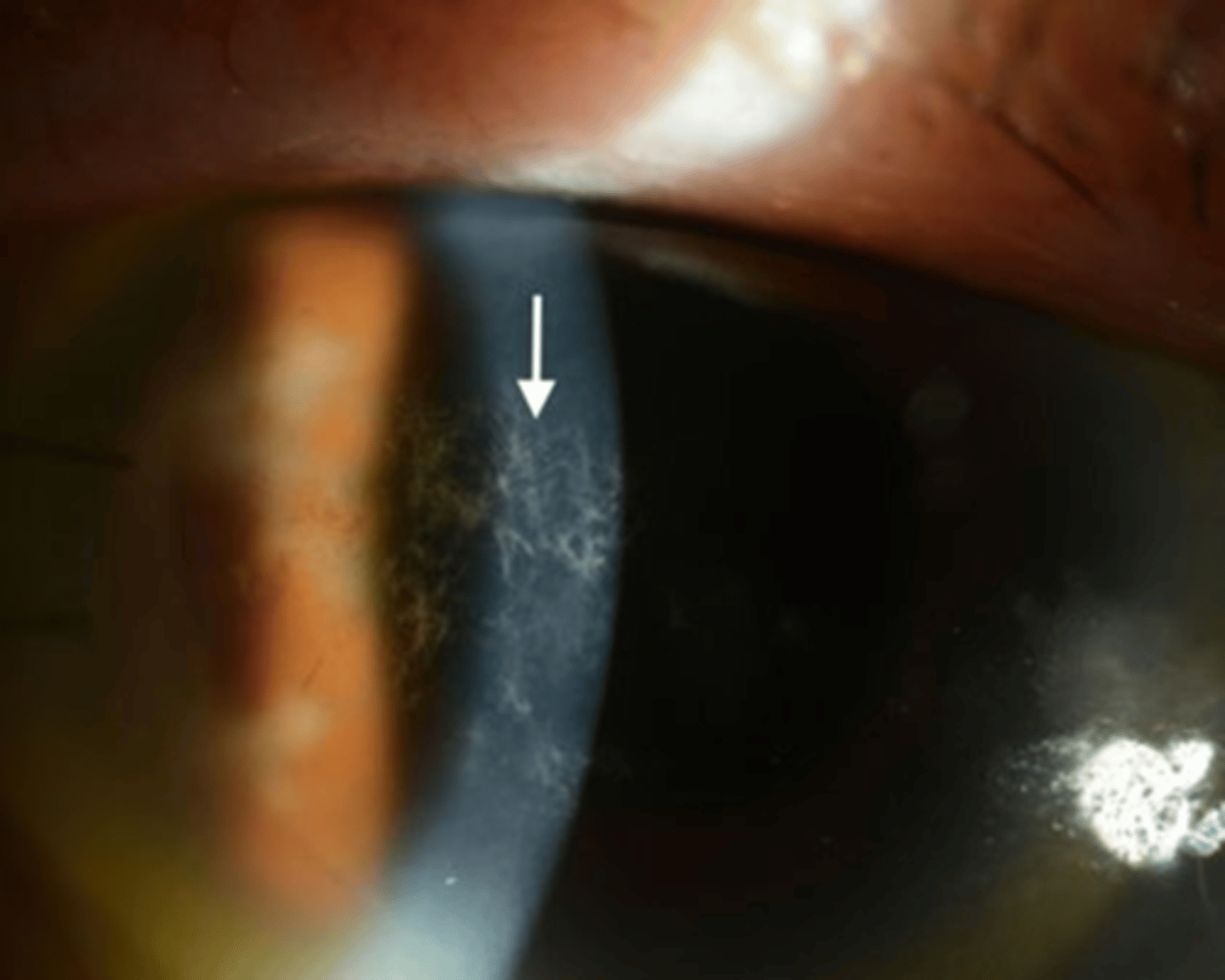
Koudadoust endothelial rejection line = line of WBC on endo that will migrate = literally separates immunologically damaged endo from healthy
What sign of graft rejection, a complication of PKP, is seen here?
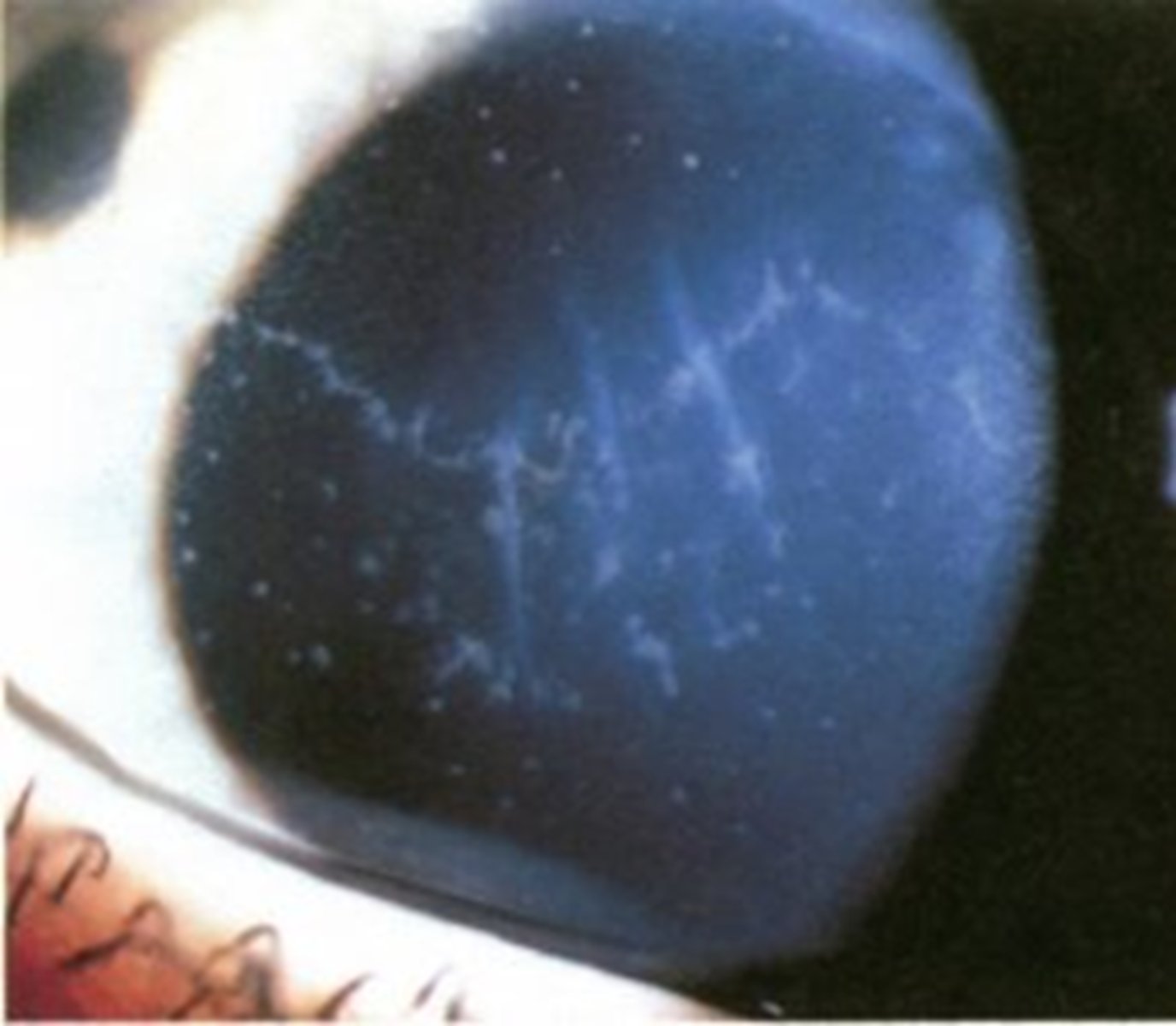
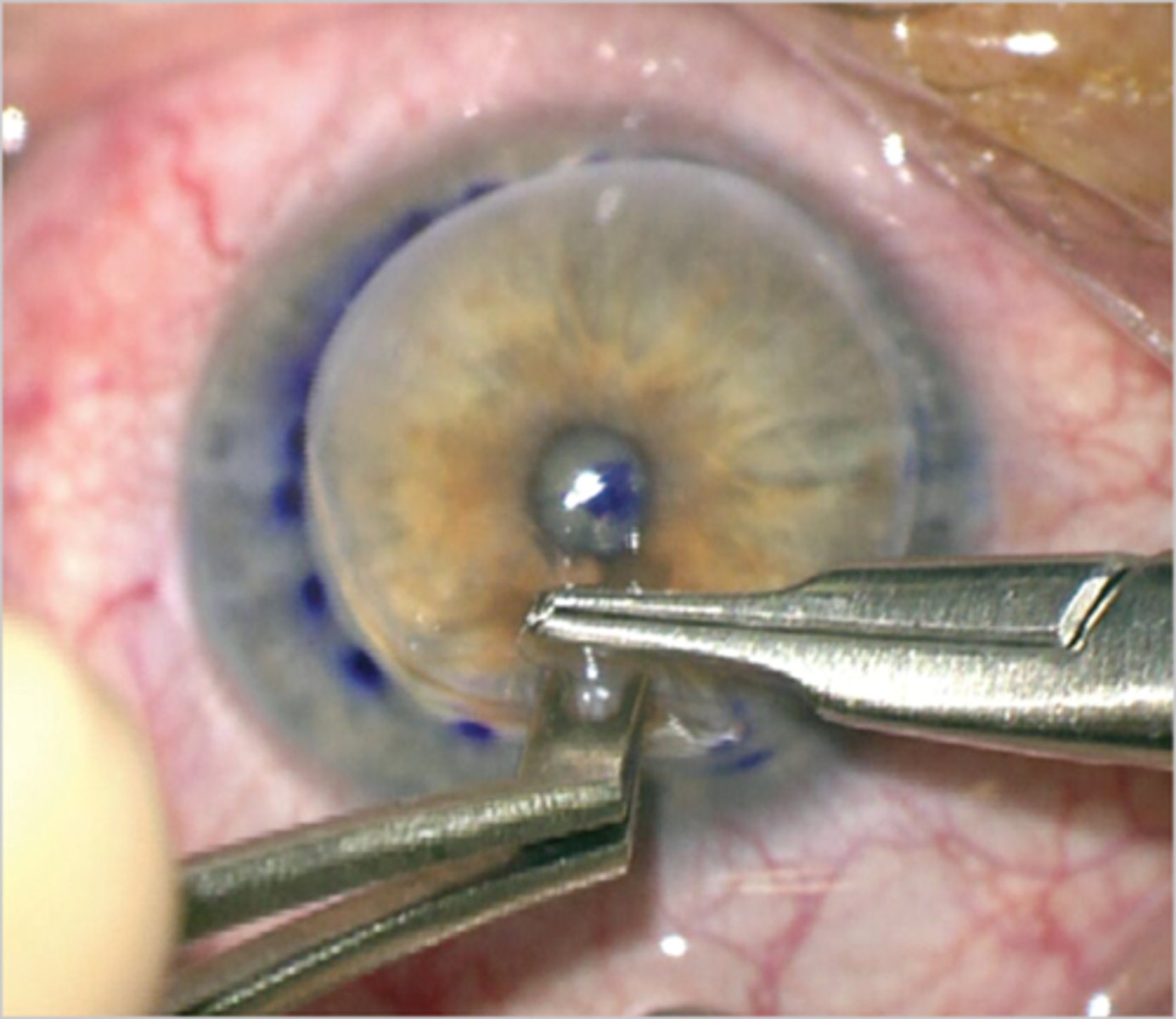
epithelial rejection line = destruction of donor epithelium, defect is covered by host epithelium
What sign of graft rejection, a complication of PKP, is seen here?

pre-op or Hx of inflam
corneal neo
young host
iris synechiae to the margin of the graft
large graft
prior ocular surgery
loose sutures
prior graft rejection
prior use of glaucoma meds
What are some risk factors for graft rejection in PKP?
topical steroids or ung, sub-tenon's if necessary
epi and subepi rejection = Pred forte or Durezol q1hr = easily reversed
endo rejection = topical q1hr and oral = more difficult
What is the mainstay tx for graft rejection, a complication of PKP?
CATs
glaucoma
impaired healing
immunosuppression = risk of infectious keratitis (bacterial, viral, fungal)
crystalline keratopathy
While topical steroids are the mainstay tx for graft rejection in PKP, what are some S/E of their chronic use?
gray-white branching stromal opacities due to Viridans streptococci biofilm
What is crystalline keratopathy that occurs from chronic topical steroid use?
calcineurin inhibitors = Immunosuppressants that inhibiting the enzyme that activates T-cells of the immune system (e.g. 1-2% cyclosporine gtts, oral tacrolimus)
anti-VEGF pretreatment in high immune risk and corneal neovascularization patients (e.g. Avastin (bevacizumab)
While topical steroids are the mainstay tx for graft rejection in PKP, what are 2 other options for tx?

non-immune mediated failure of donor tissue/graft itself (improper storage, surgical trauma, etc) = corneal edema immediate post-op that never clears
What is graft failure, a complication of PKP?
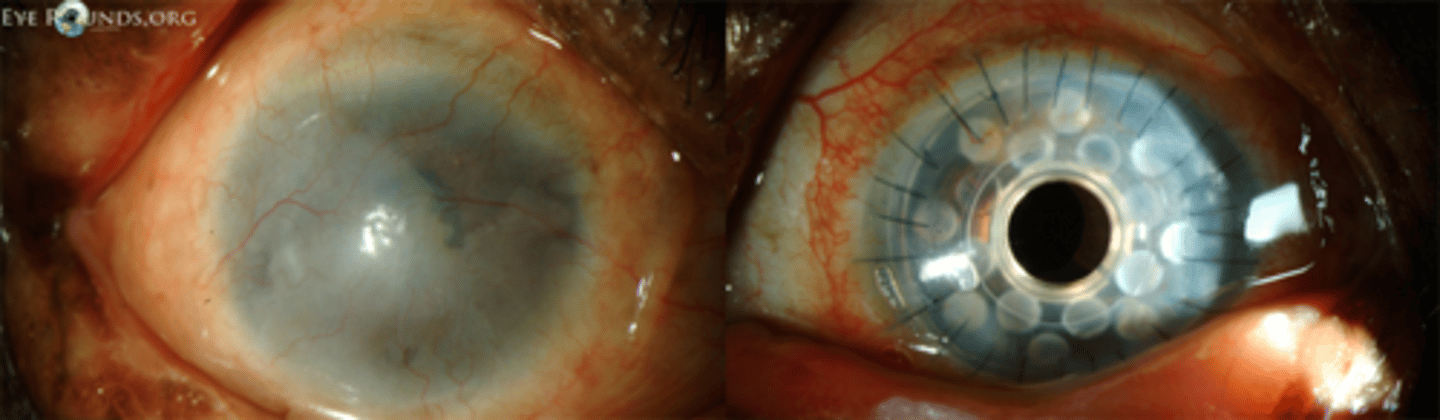
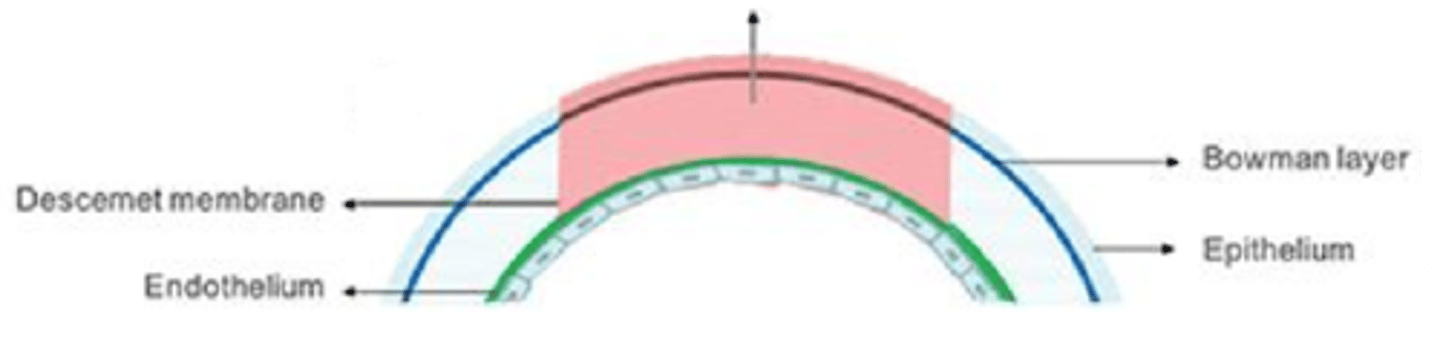
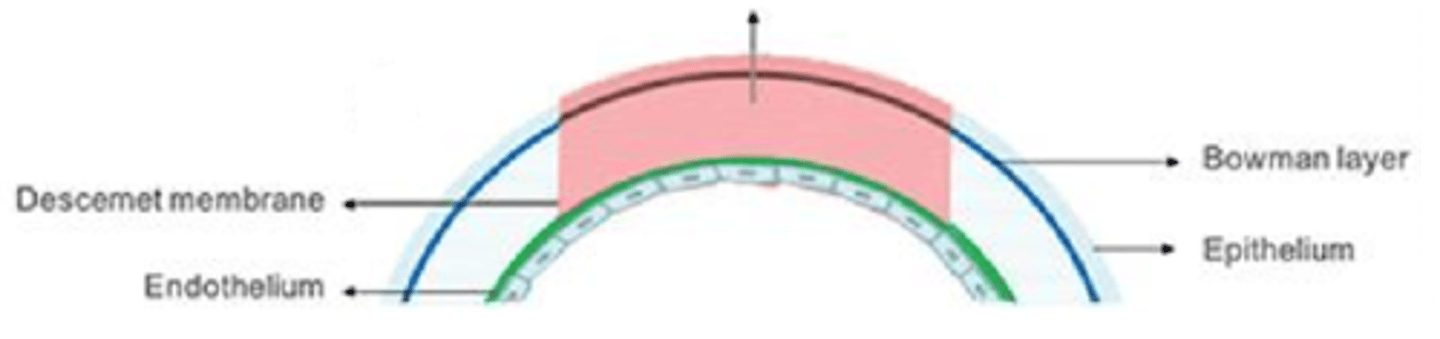
replaces diseased stroma while preserving Descemet's and endo = good for advanced keratoconus, dense stromal scarring, stromal dystrophies
What is a deep anterior lamellar keratoplasty (DALK) and what conditions is it indicated for?
“Big Bubble” technique = injection of air
How does the surgeon dissect the host stroma and Descemet's membrane in DALK?
lower risk of endophthalmitis
lower risk of expulsive hemorrhage
no risk of endothelial rejection
increased wound integrity
What are some advantages of DALK?
very challenging to learn and master
time consuming
high rate of Descemet’s rupture = convert to PK
What are some disadvantages of DALK?
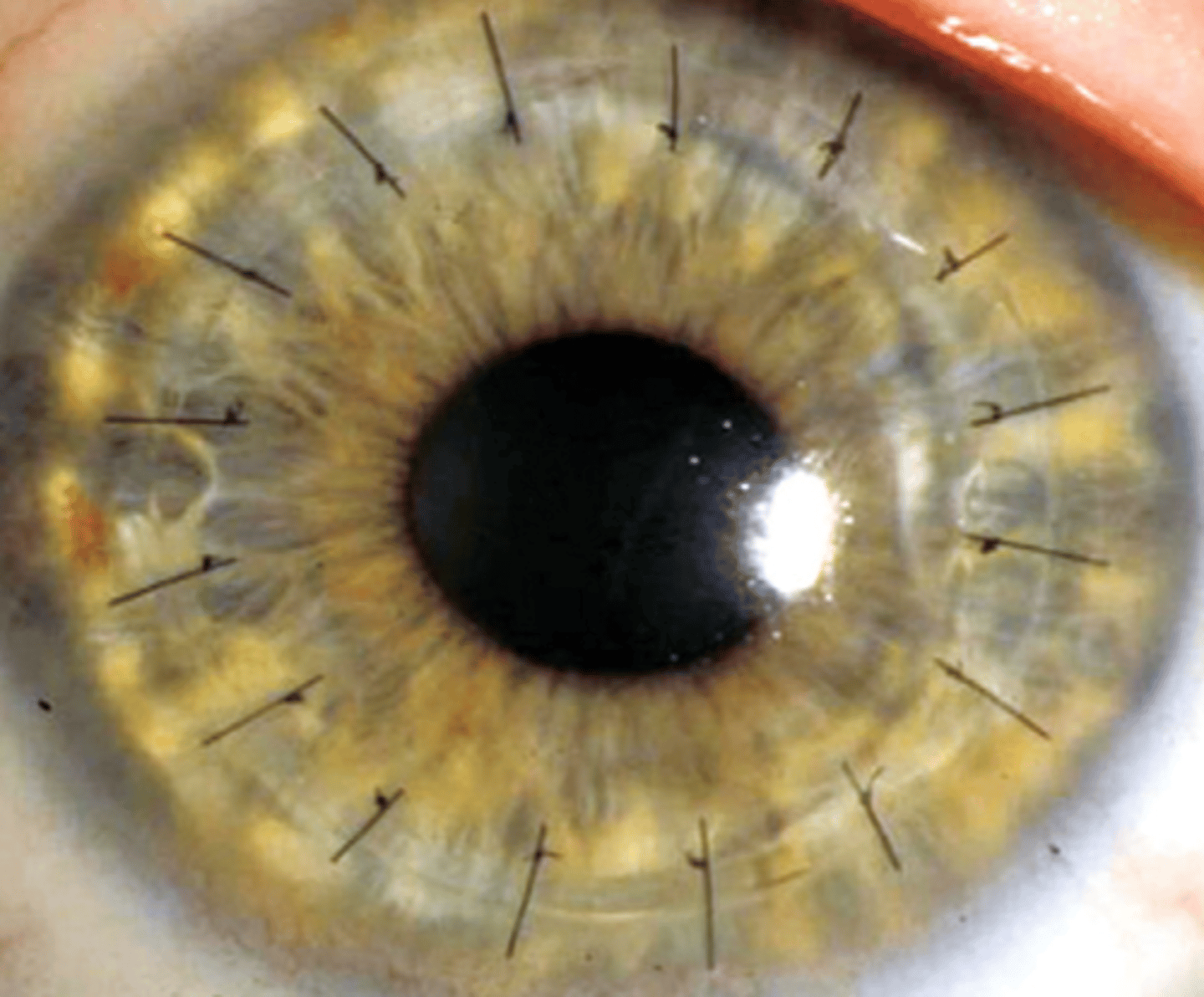
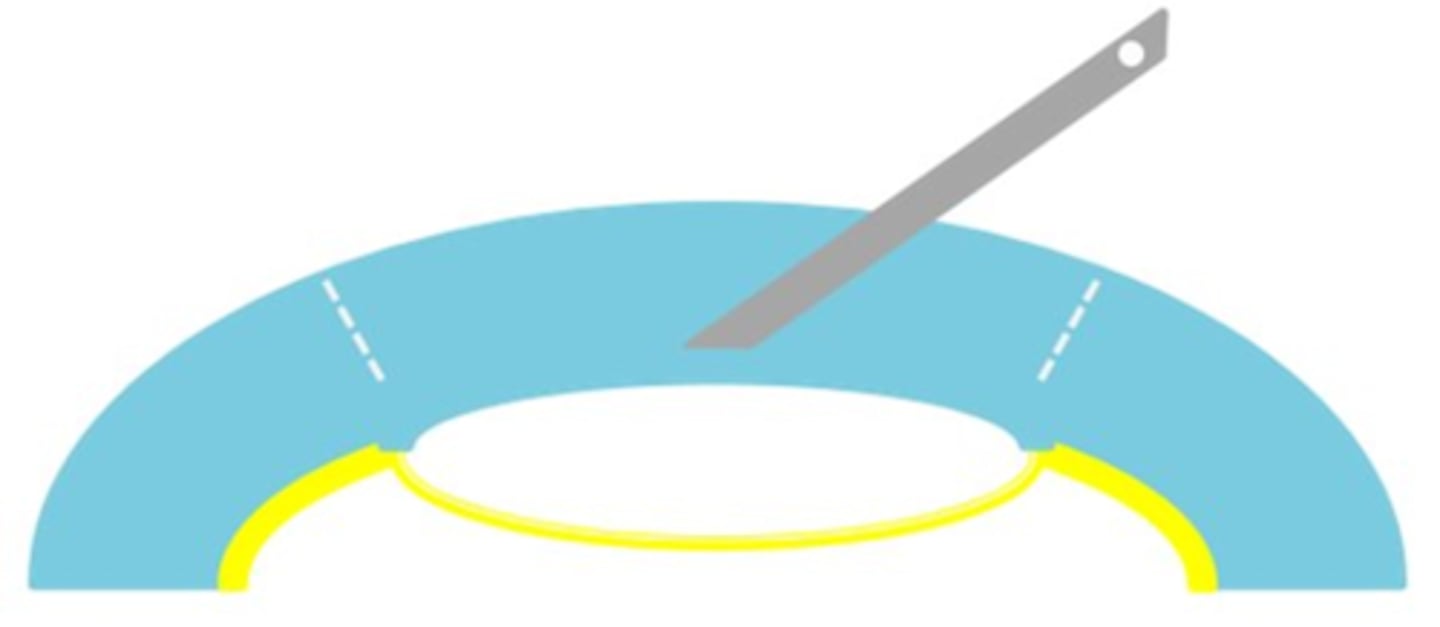
newer surgery = implant of a mid-stromal Bowman's layer graft = flattens and strengthens an abnormally steep cornea
What is a Bowman's layer transplantation (BLT)?
inlay = graft into mid-stroma for tx of advanced KCN
onlay = tx of persisent sub-epi haze after PRK (almost like a permanent amniotic membrane for a diseased cornea)
What is the difference between an inlay vs onlay graft in a Bowman's layer transplantation (BLT)?
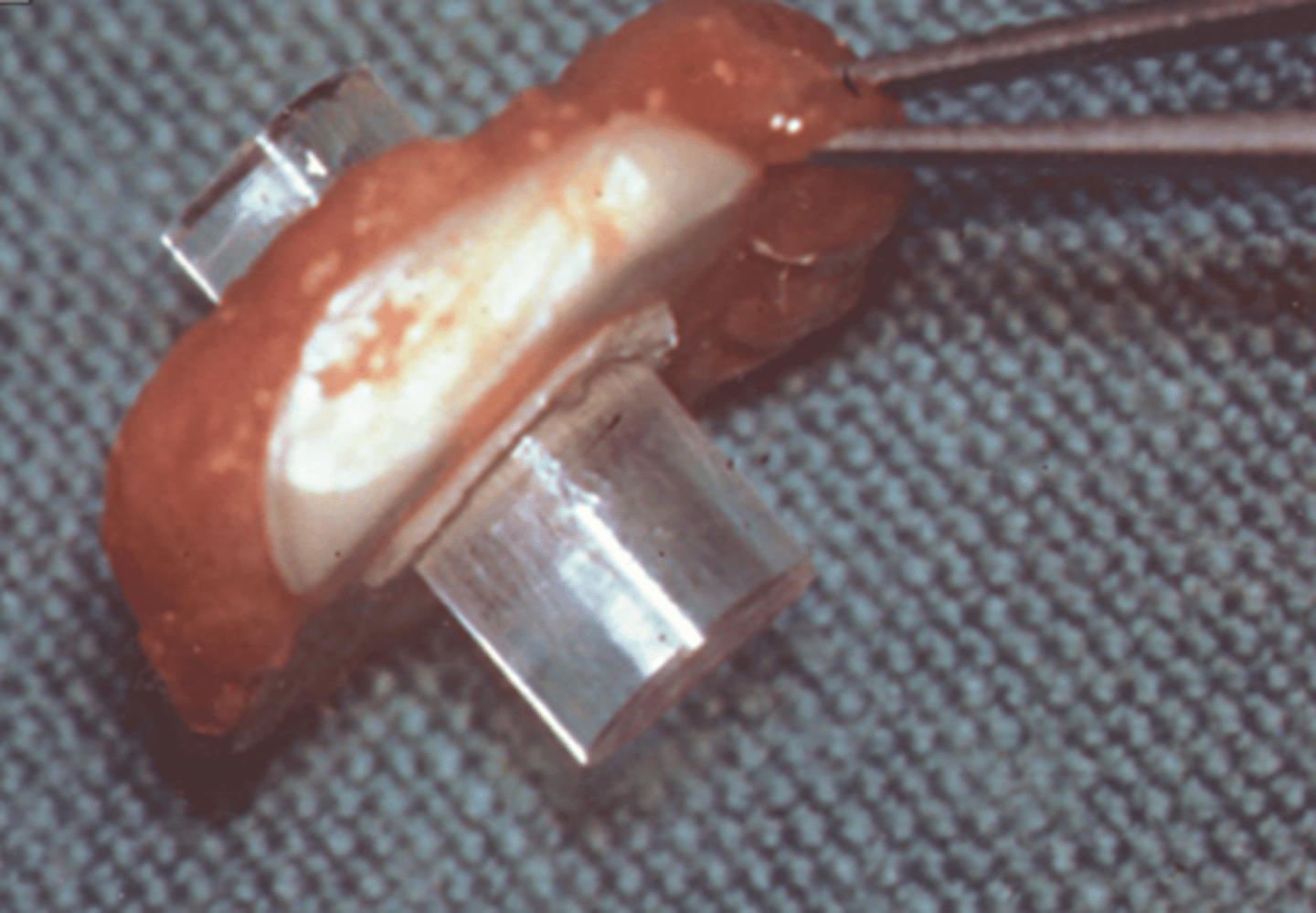
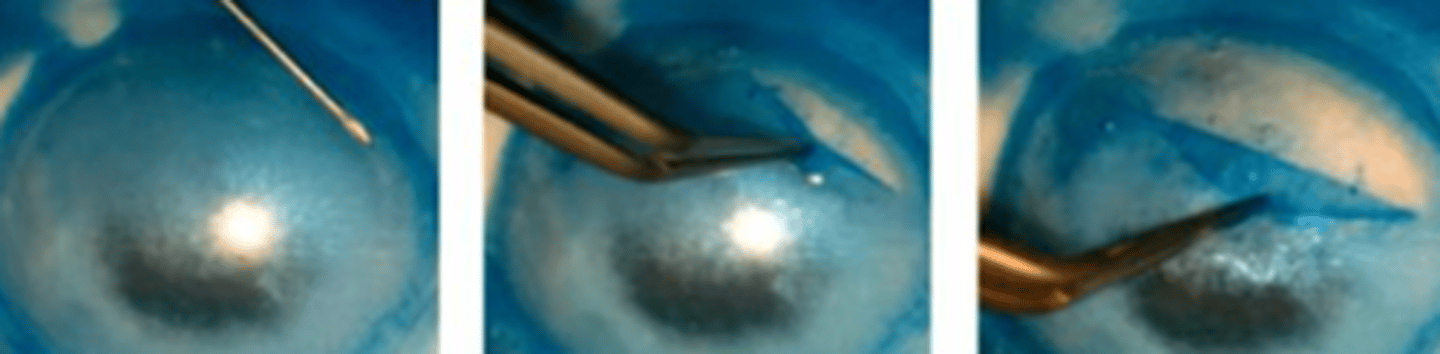
donor corneoscleral button mounted onto artificial AC
epi and BM debrided with sponge, spatula
stroma inflated with air (opaque now) to visualize Bowman's
Tryptan blue stains Bowman's to visualize
Bowman's is scored with a 360deg with 30g needle, then peeled off
Explain the general process of retrieving donor Bowman's in a BLT.
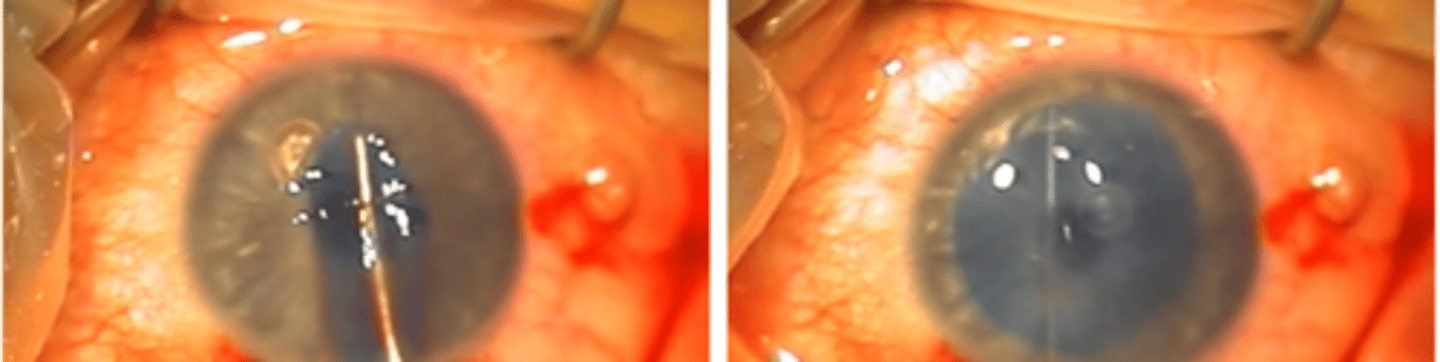
corneoscleral tunnel created
AC filled with air through paracentesis
mid-stromal pocket created limbus-to-limbus
graft inserted into pocket on a surgical glide
AC reformed
wound closed w/ 1 suture = good structure maintained
Explain the general process of inserting Bowman's into host in a BLT.
up to 8 D
BLT can reduce astigmatism in a KCN pt by how much?
minimally invasive
NO surface incisions are made
NO sutures to fixate the graft
Bowman’s layer is acellular, graft rejection unlikely
What are some advantages of BLT?
Bowman's perforation (10%) but easily aborted and allowed to heal
What is the main complication of BLT?

posterior lamellar transplant for endothelial disease, such as Fuch's, Pseudophakic Bullous Keratopathy (PBK) or Pseudophakic Corneal Edema (PCE), Iridocorneal Endothelial Syndromes (ICE)
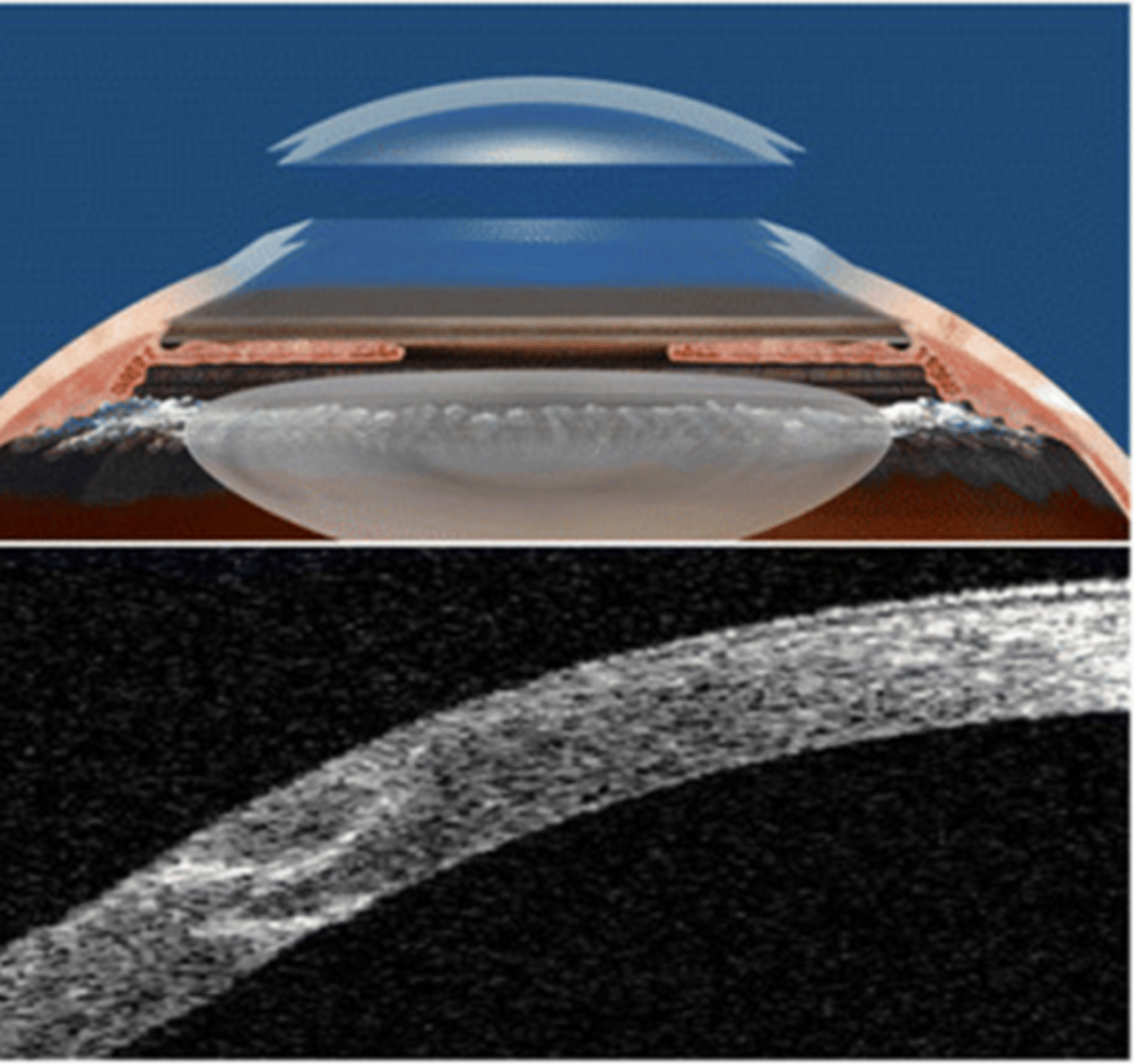
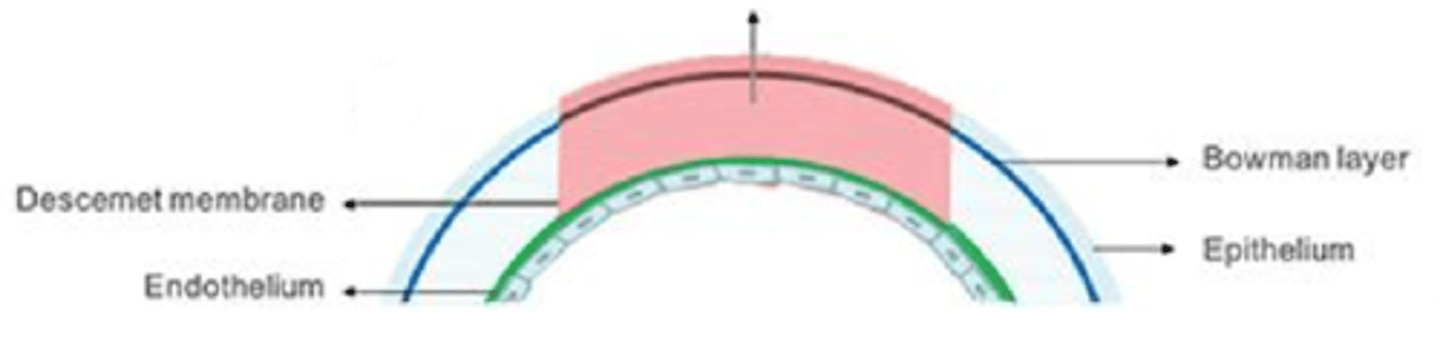
What is a Descemet's stripping automated endothelial keratoplasty (DSAEK) and when is it used?
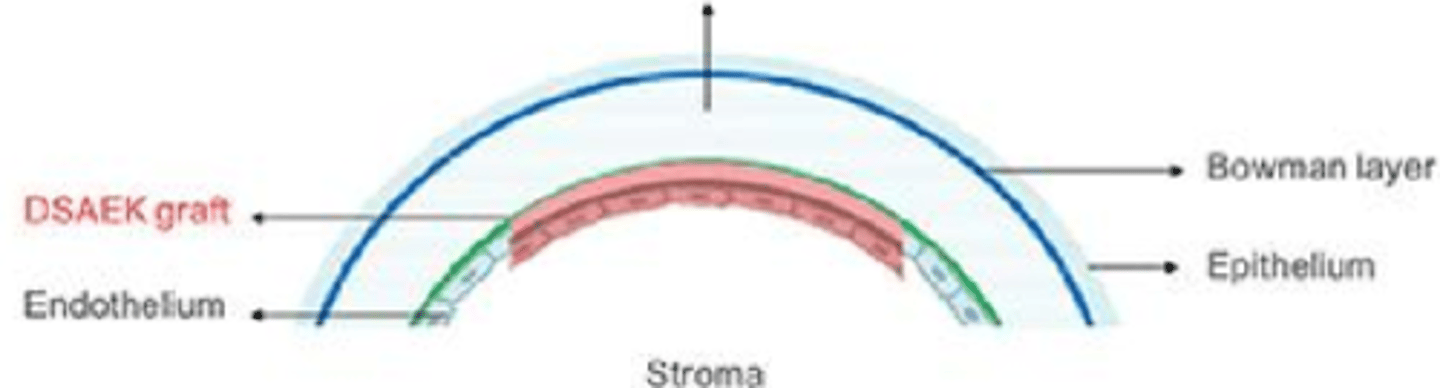
Descemet's is stripped from the stroma with microkeratome
posterior lamellar graft of post stroma, Descemet's, endo is inserted
AC air bubble helps adherence
Explain the process of DSAEK.
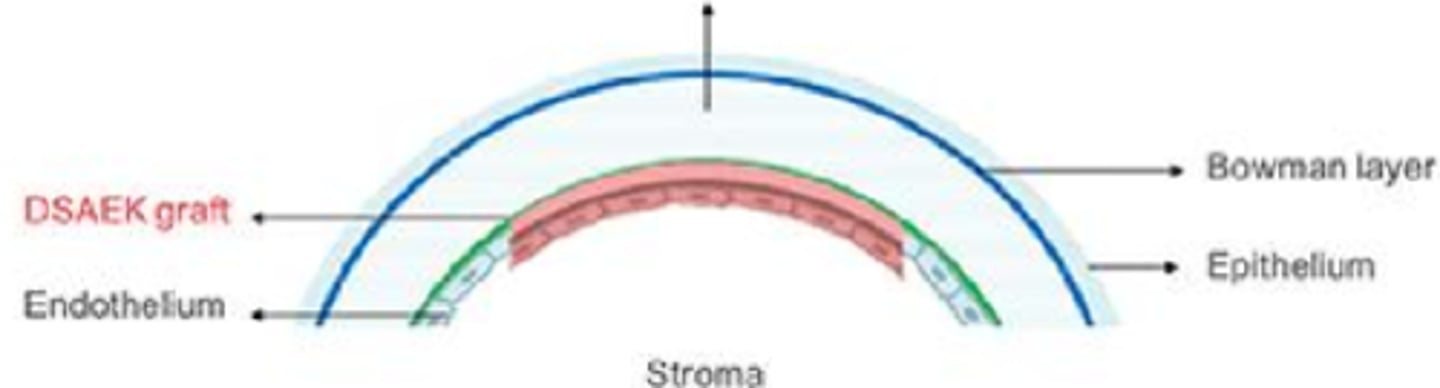
graft tissue is thicker than tissue removed
creation of a new optical interface in the cornea
induces astigmatism, scatter and aberrations
What are the 3 main optical drawbacks of DSAEK?
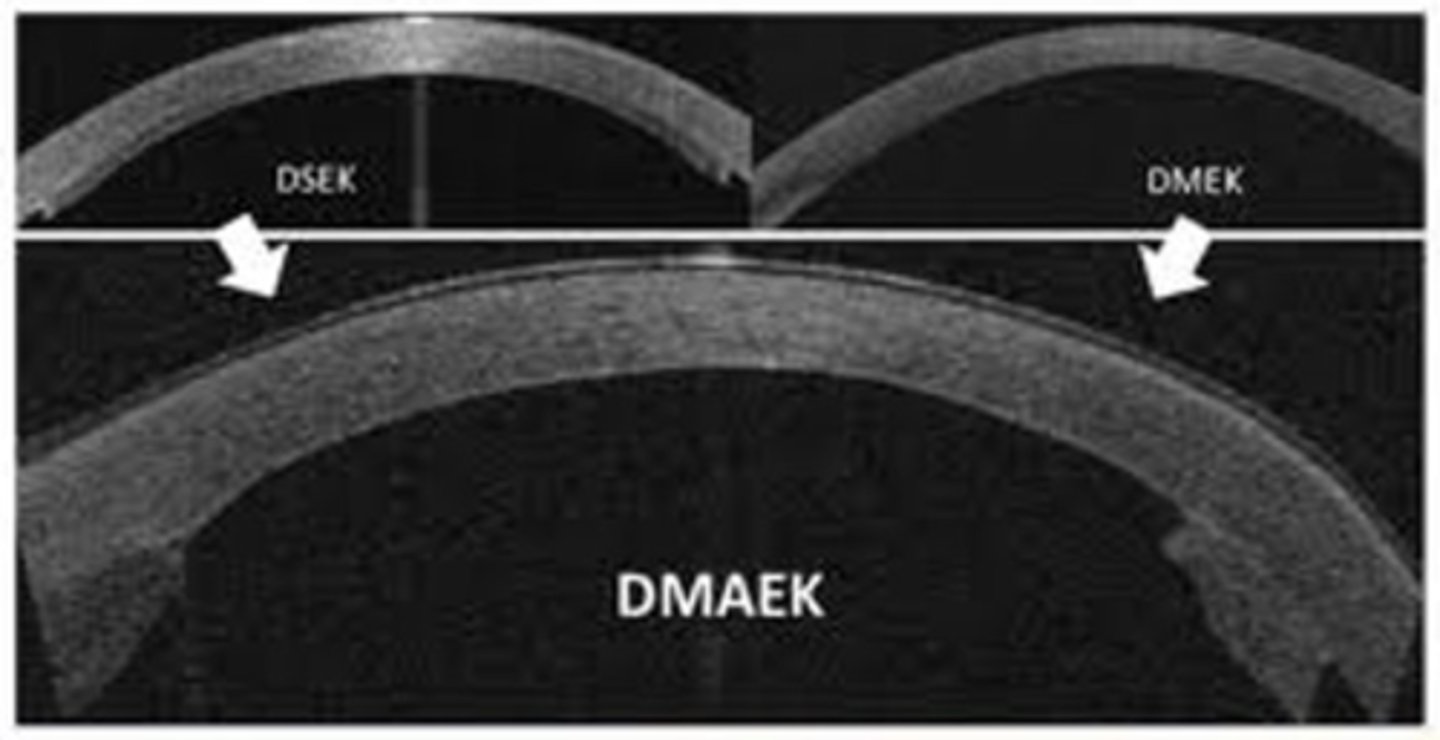
transplantation of only Descemet's and endo
What is a Descemet's membrane endothelial keratoplasty (DMEK)?
improved visual outcome
less astigmatism compared to PK or DSAEK
reduced rejection rates
What are the advantages of Descemet's membrane endothelial keratoplasty (DMEK)?
more difficult graft preparation bc easy to tear
more difficult surgical technique bc tendency to "scroll"
increased graft dislocation rates if pt sits up, rubs eye
pt must remain supine for 48hrs until bubble dissolves
What are the disadvantages of Descemet's membrane endothelial keratoplasty (DMEK)?
center of graft is only Descemet’s membrane and endothelium while the periphery of graft has a small portion of stromal tissue
What is a Descemet's membrane automated endothelial keratoplasty (DMAEK)?
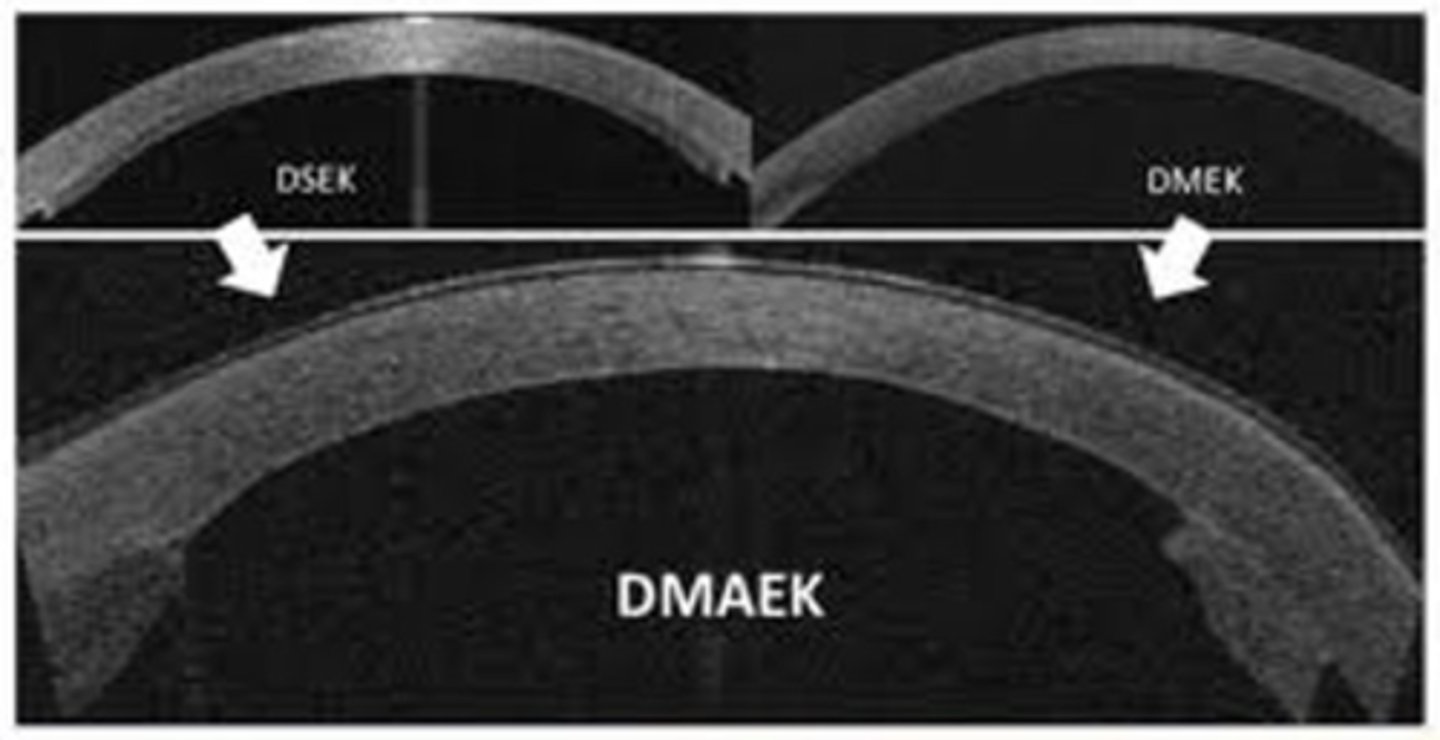
good optics along visual axis, while reducing the difficulty of the surgery and dislocation of the graft
Why was the DMAEK created from a hybrid of DSAEK and DMEK?
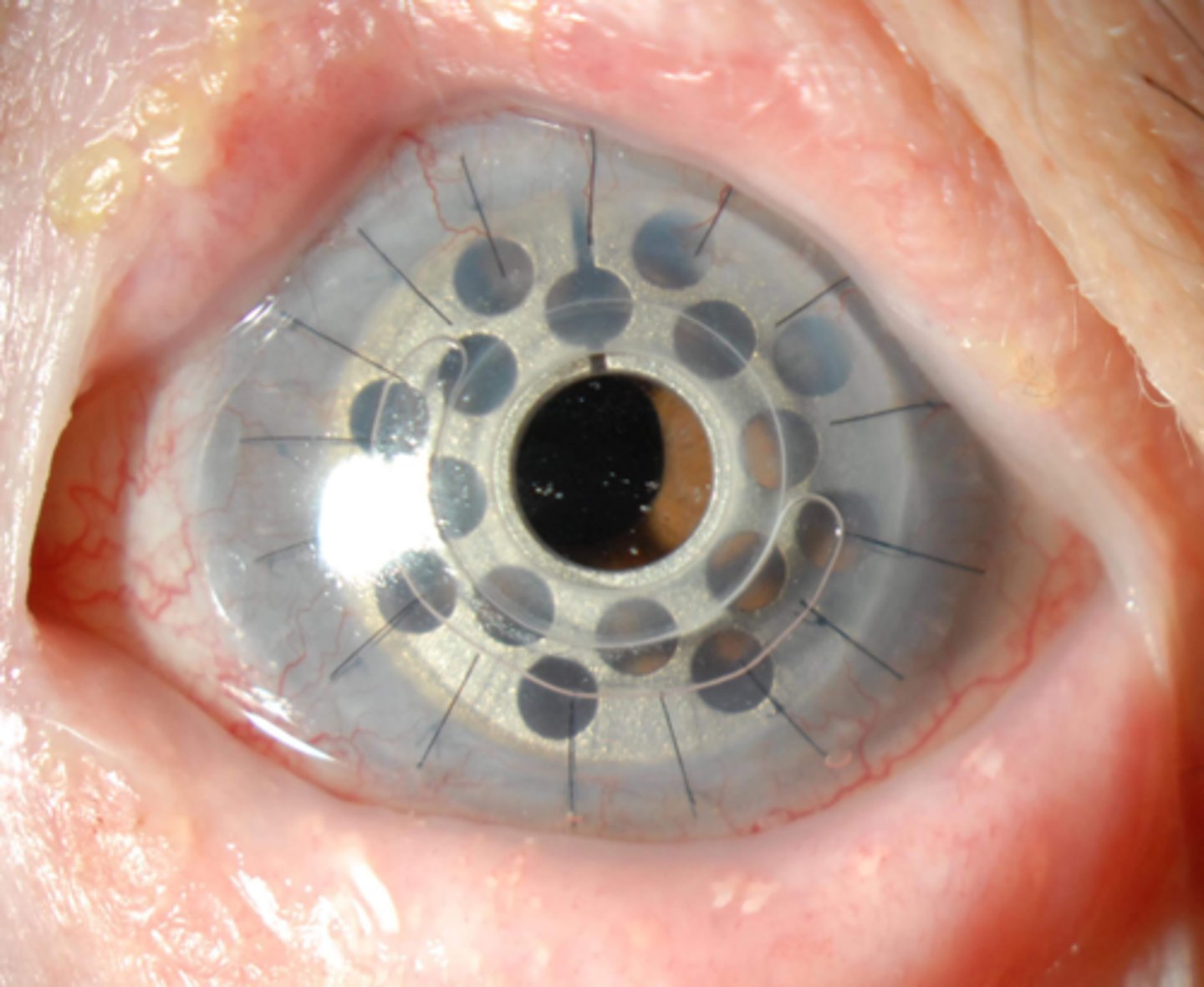
artificial corneal transplant = surgeries of last resort!
What is prosthokeratoplasty (Kpro)?
may restore vision to otherwise blind individual = life-changing
What are some advantages of prosthokeratoplasty (Kpro)?
very complicated with high rate of complications (endopthalmitis, glaucoma, RD)
greatly decreased VF
multiple surgeries over months to years
life-long follow-up
cosmetically unattractive
What are some disadvantages of prosthokeratoplasty (Kpro)?
true
True or False: the Boston K-Pro uses a donor corneal graft between the front optical stem and the back plate.
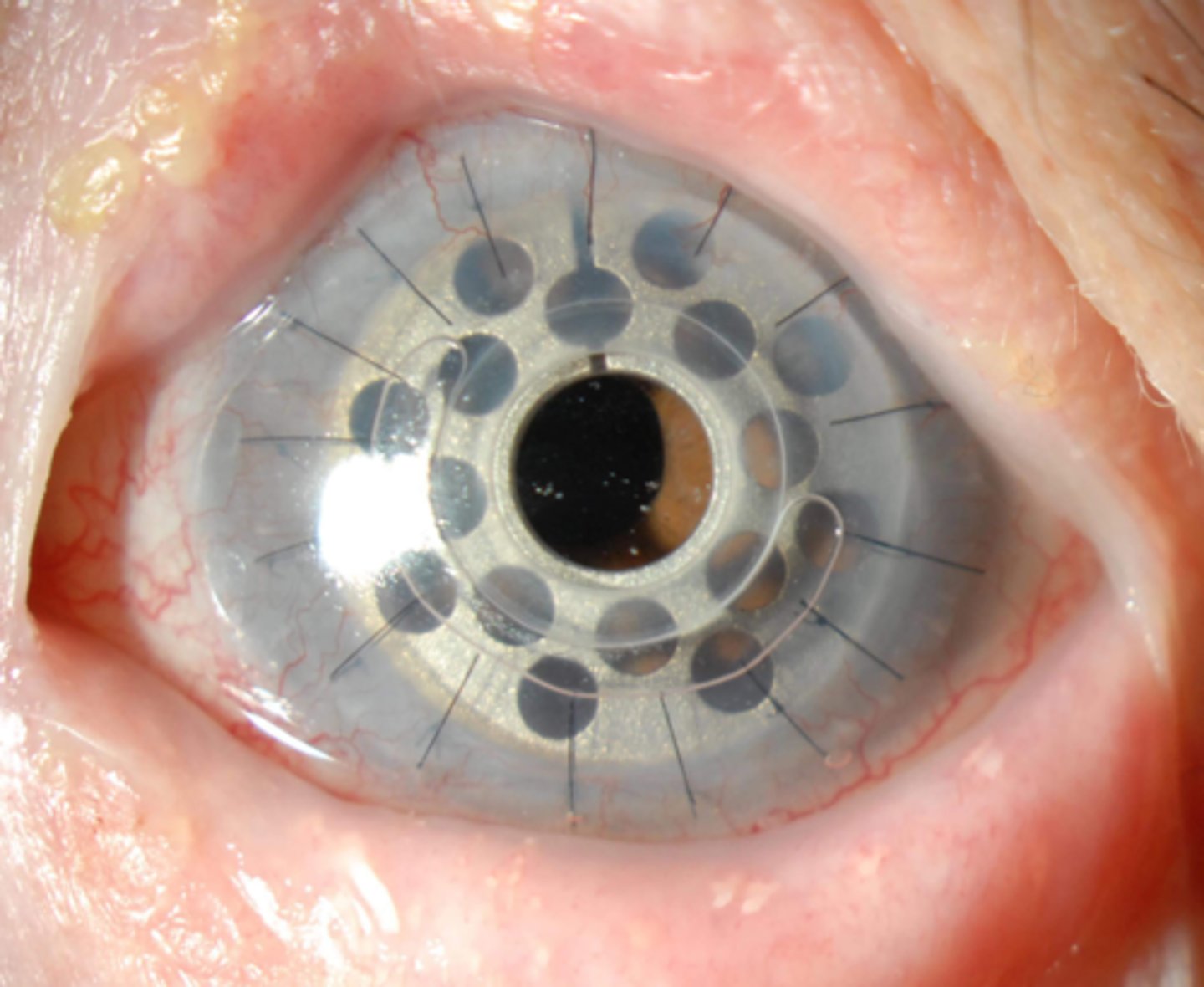
optics of visual axis maintained even if the graft fails and becomes opaque
can be implanted in children 1-year and older to prevent amblyopia
What are some advantages of the Boston K-Pro?
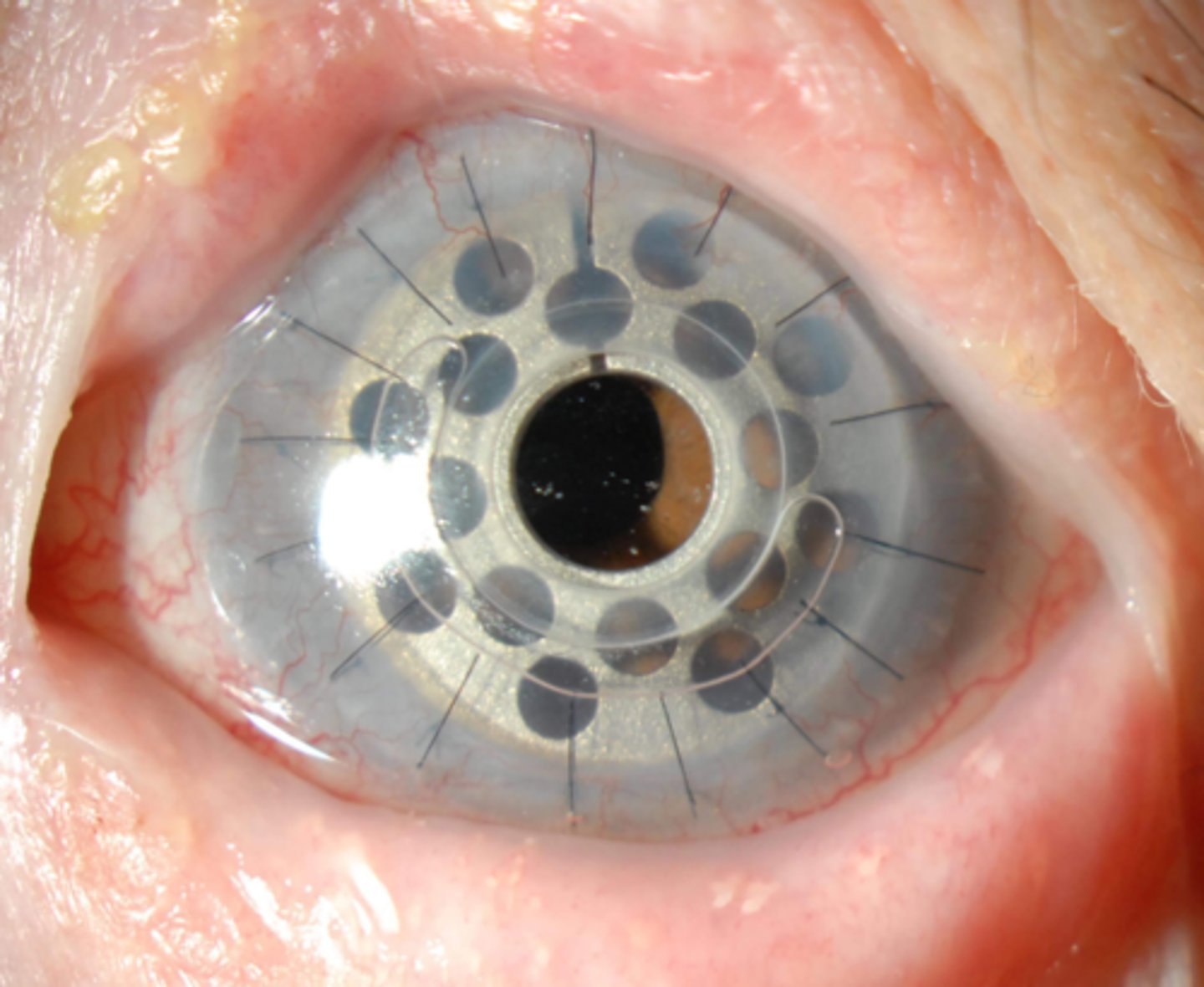
unable to check IOP
fortified antibiotic drops must be applied daily to prevent infection
50% complication rate at 5-years
What are some disadvantages of the Boston K-Pro?
one-piece, non-rigid synthetic corneal implant = implanted into stromal pocket and covered with graft/amniotic membrane for 2 mos, then overlying conj and cornea are removed via trephination
What is the AlphaCor Kpro?
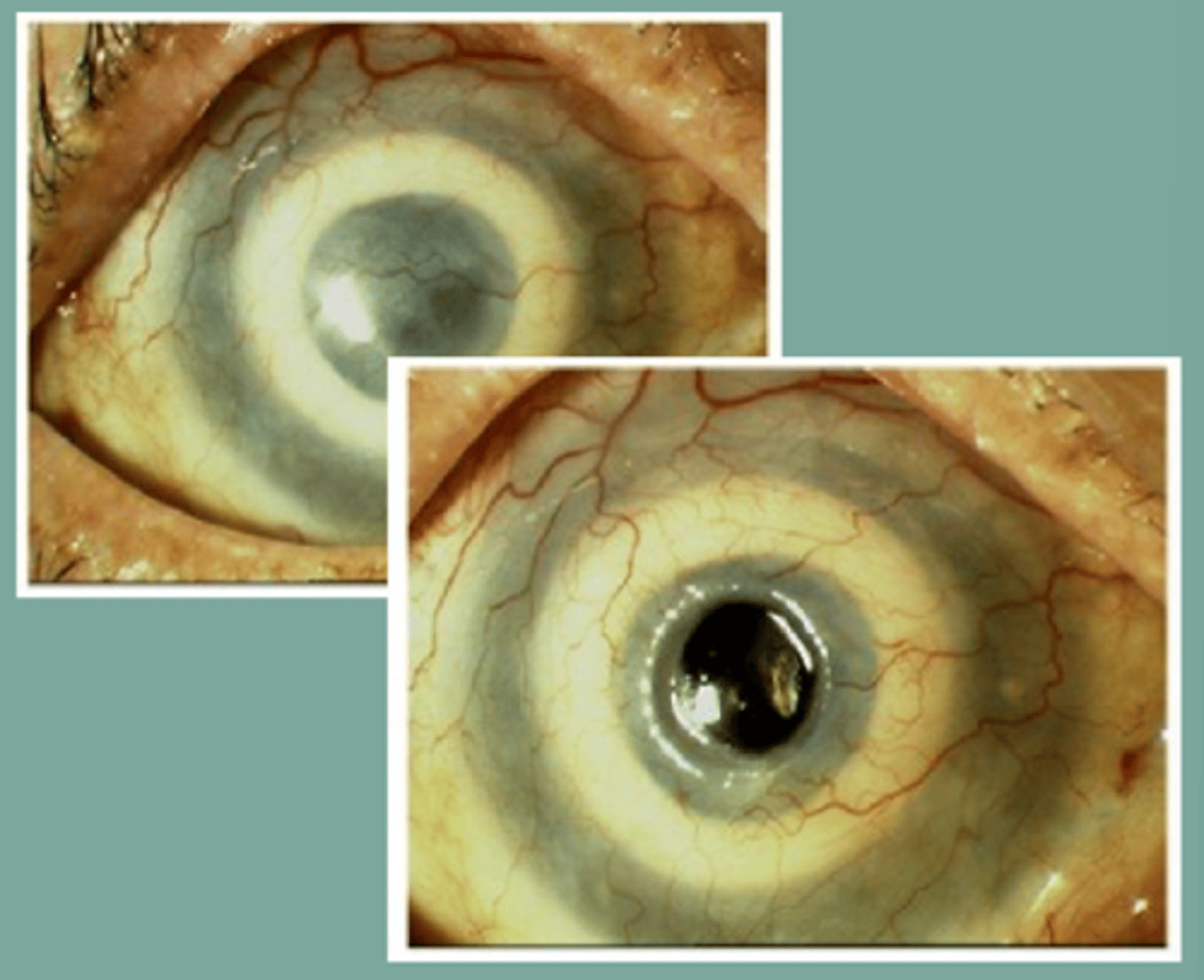
uses a single root tooth, some jaw bone, and buccal mucosa to create a new ocular surface and foundation for a PMMA optical cylinder
What is the Osteo-Odonto-Keratoprosthesis (OOKP)?