Lecture 9: Eating disorders 2
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
45 Terms
Lillienfeld (evidence based practice vs actual practice)
-identified some concerns about treatment of eating disorders
-over 600 therapies were identified
-a few were wacky
-many were described as ‘evidence-based’ → very few were evidence'-based
-most clinicians do not deliver evidence-based treatments
review of studies of clinical practice (Lillienfeld)
-only 38% reported using the strongest therapy
-even if they do use the strongest therapy, take out key elements
-only 6% report using evidence-based treatment manuals
-more deliver unevidenced therapies
-many are untrained in the therapy they are using
-clinician characteristics get in the way
empirically grounded interventions
-links between clinical guidelines, evidence, theory and actual practice
-start with theory → then do experimental studies to test theory → use to develop treatments → then do feasibility and RCTs → then wider efficacy and cost-effectiveness trials
matching interventions to the condition
-different therapies have focused on different elements in the aetiology and maintenance of EDs
biology
genes
family interaction
sociocultural influences
trauma
bullying and teasing
negative life experiences
maintenance factors
-most effective interventions focus on maintenance factors:
safety behaviours
cognitive patterns
emotional patterns
social maintenance
family accommodation of symptoms
nutrition
prevention of EDs
-ideal for implementation in late childhood/early adolescence
-inoculate the individual against the development of eating pathology
-massive potential benefits for limited investment
potential targets of prevention of EDs
-lowering of eating and other concerns in the present
-a lower level of future development of EDs
risks of prevention strategies
-Carter and Baronowski & Heatherington
-psychoeducation about dieting and EDs
-in both cases the level of pathology got worse
Baronowski - short term
Carter - long term
-Carter reported this as a problem and suggested not doing this sort of psychoeducation
-but Baronowski did not and reported it as a success
Le (meta-analysis on prevention strategies)
-many of the studies were weak
-media literacy approaches reduce shape and weight concerns for everyone in the whole young population
-cognitive dissonance approaches reduce eating behaviours and attitudes in high-risk groups
-CBT interventions reduce risk of dieting
-weight management interventions reduce some risk factors
effectiveness of prevention strategies
-some evidence for reduction of risk factors and developing eating disorders → dissonance-based approaches
-need to get better at reducing numbers of cases to justify the effort spent on prevention work
NICE - obesity recommendations
-family interventions involving schools, local government, families, policies such as taxation → rather than specific psychological interventions
-encouraging lifestyle changes healthy eating - amounts and choices, routine exercise
obesity rates
-3/4 people aged 45-74 are overweight or obese
-proportion has risen from 14.9% to 28% since 1993
NICE guidelines
-strongest evidence
-match most other guidelines internationally
-primary differences are between:
adults vs children/adolescents
underweight vs non-underweight patients
effective treatments for anorexia - adults (NICE)
individual CBT - 40 sessions
Maudsley anorexia nervosa treatment for adults (MANTRA) - 20-30 sessions
specialist supportive clinical management (SSCM) - 20-30 sessions, case management approach to reduce problematic eating behaviour
similar level of effectiveness to behaviour therapy
effective treatments for anorexia - children and adolescents (NICE)
-AN-focused family therapy
non-blaming
stop accommodating patterns
family starts by taking control of the child’s eating
then moves to giving that control back to the child
finishes with relapse prevention
-CBT-ED or adolescent-focused psychotherapy as a second option
effective treatments for BN and BED - adults and adolescents (NICE)
-group CBT-ED or individual CBT-ED - 16-20 sessions
effective treatments for BN - children and adolescents (NICE)
-family therapy
-CBT-ED as a second line therapy
effective treatments for atypical cases (NICE)
-use the therapy recommended for the most similar full syndrome
effective treatments for ARFID (NICE)
-not addressed by NICE → too new to have an evidence base
-some early evidence for CBT-avoidant/restrictive
correcting common myths
-briefer therapies can be as effective for non-underweight EDs
-therapeutic alliance does not work in the way that clinicians assume
-early change is critical
-no evidence that severity or duration reduces effectiveness
common elements of effective treatments
-start with food as the key element
single most important element is nutrition/exposure to foods
-underweight cases → not clear whether the rest of these therapies does much more
-non-underweight cases → extra value in the psychological element of therapy
effective treatments (NICE)
-covers the therapies that are most strongly supported by the evidence
so is what should be used as a priority and in a resource-limited setting
drives commissioning advice for NHS
addresses issues around case management and patient experience
-some other approaches may have evidence to support them
not meeting the NICE criteria of enough high-quality research
not as effective as what the guidelines recommend
still not including very weak research or unsupported clinician opinion
need for case management
-medical monitoring and management
-intensive treatments varies across cultures
-necessary for management of high-risk cases
-can be good for weight restoration
-almost no evidence of establishing recovery
-very expensive
-risk of creating dependence
weaker evidence (for certain treatments)
-therapies that have been recommended in the past but have not been retained because they were overtaken by stronger evidence
SSRIs (weaker evidence for use)
-at high does for BN can:
enhance functional serotonin
reduces binges for some people while taking, but not for long-term
potential withdrawal effects → SSRI discontinuation syndrome
novel antipsychotics (weaker evidence for use)
-for AN
-reduce anxiety
-have dampening effect, range of side effects such as weight gain through metabolic slowing
neuromodulation (weaker evidence for use)
-transcranial stimulation methods seem to reduce depression slightly
-no evidence that this works specifically in ED
leucotomy (weaker evidence for use)
-brain surgery, rarely used
-has been used for chronic AN with extreme OCD
-evidence is anecdotal
dialectical behaviour therapy (weaker evidence for use)
-reduces impulsive behaviours in BED/BN, but little change in core pathology
-evidence for AN is very limited
interpersonal psychotherapy (weaker evidence for use)
-works for BN
-slower and less effective than CBT
focussed psychodynamic approaches (weaker evidence for use)
-effective for AN in a German study
-needs to be replicated in other countries
integrative cognitive-affective therapy (weaker evidence for use)
-less effective than CBT
mentalisation-based therapies (weaker evidence for use)
-mainly used in personality disorders
-effectiveness for EDs lower than CBT - takes 18 months
acceptance and commitment therapy (weaker evidence for use)
-small number of studies - only 5 RCTs but poorly designed
-mindfulness-based approaches
-family therapies that are not food/eating focussed
mean effectiveness of evidence-based therapies (adult psychological disorders)
50% recovery
25% improvement
20% unchanged
5% deteriorate
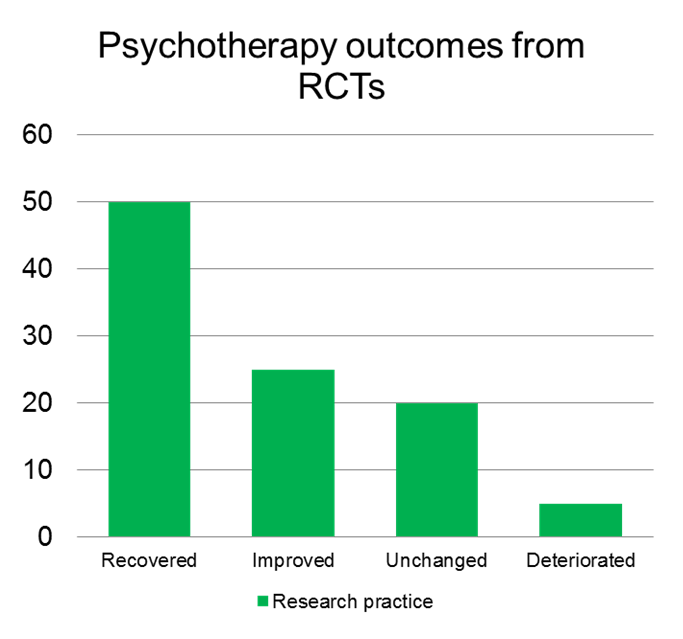
mean effectiveness of evidence-based therapies (eating disorders)
-can still hit 50% recovery rate in treating EDs → only for non-underweight cases
-lower for underweight cases - 30%
CBT targets (where therapies have impact)
-targets areas to break cycle perfectionism
-low self-esteem, need for control, starvation, restriction, fear of loss of control
family therapies targets (where therapies have impact)
-target low self-esteem, need for control, restriction, starvation, positive outcome and sense of control
homeostasis
-encourage the person to overcome their reasons for not eating healthily
-supporting the person to eat in response to biological need
not to toxic environment or to inner psychological psychological concerns
-aim to restore homeostasis
addressing nutrition
-wide range of effects:
reduces anxiety, depression, impulsivity, compulsivity → serotonin levels in particular
reduces alcohol levels → mood stability plus reduction in starvation
enhances cognitive flexibility, social skills → reduction in starvation effects and safety behaviours
normalises and stabilises weight
enhances quality of life
factors contributing to obesity
factors contributing to hunger → genetics, learning, social learning
satiety → social pressures, food industry, toxic environment
Jeffrey (psychological therapies have poor outcomes)
-can support people to lose weight in the short term
-but poor at keeping weight down in the long term, whatever the therapy
issues with treating obesity
-even a 5-10% loss of weight can have major health benefits
-but have trouble achieving that
-biology meets the toxic environment, and obesity is difficult to change
supporting people with obesity
political/social changes - but does carry risk of fat shaming
lifestyle coaching → food choices and exercise
longer therapy → relatively limited benefits
continuing care model seems most likely to work
bariatric surgery
-most effective long-term route to weight loss
-different methods and only to be conducted by surgeons
-most issues about adaptation to lifestyle changes and making slow progress → requires psychological preparation and maintenance strategies
-where psychologist can be usefully involved