Chapter 19: Chest Tube Insertion and Monitoring
1/7
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
8 Terms
Chapter 19: Chest Tube Insertion and Monitoring
Purpose of Chest Tubes
Drain air, blood, or fluid from the pleural space
Reestablish negative intrapleural pressure (allows lung expansion)
Promote lung re-expansion and restore normal intrathoracic pressure
Insertion Locations
Emergency department
Bedside
Operating room via thoracotomy incision
Indications for Removal
Lung has fully re-expanded
No further drainage into the pleural space
Key Nursing Concepts
Loss of negative pressure causes lung collapse (pneumothorax)
Restoring negative pressure allows alveoli to reopen and improve gas exchange
Ongoing drainage indicates continued pleural pathology (air leak, bleeding, effusion)

Chest Tube Systems
Most commonly uses a disposable three-chamber drainage system
Three Chambers
Drainage Collection Chamber
Collects air, blood, or fluid from the pleural space
Water Seal Chamber
Acts as a one-way valve
Allows air to exit pleural space during exhalation
Prevents air from entering lungs during inhalation
Suction Control Chamber
Regulates amount of suction applied
May be wet or dry
Water Seal Chamber
Sterile fluid added to the 2 cm line minimum (follow manufacturer guidelines)
Must remain upright and below chest insertion site
Monitor water level routinely (evaporation risk)
Add sterile fluid as needed to maintain prescribed level
Wet Suction Control
Amount of suction determined by height of sterile fluid in chamber
Common prescription: −20 cm H₂O
Connected to wall suction
Adjust until gentle bubbling is present (excess bubbling increases evaporation)
Dry Suction Control
Provider sets suction level on device (typically −20 cm H₂O)
When connected to wall suction, regulator is set per manufacturer instructions
Tidaling (Normal Finding)
Spontaneous breathing
Fluid rises with inspiration
Fluid falls with expiration
Positive-pressure mechanical ventilation
Fluid rises with expiration
Fluid falls with inspiration
Abnormal Findings
Cessation of tidaling
Lung re-expansion or system obstruction
Continuous bubbling in water seal
Indicates air leak in system
Intermittent bubbling
Expected when removing air (exhalation, coughing, sneezing)
Absence of bubbling afterward indicates air removal complete
Mediastinal Chest Tubes
Used after open-heart surgery
Bubbling and tidaling not expected
Fluid level may show cardiac pulsations
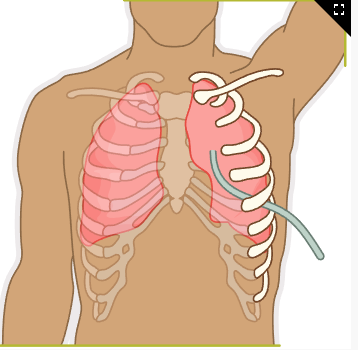
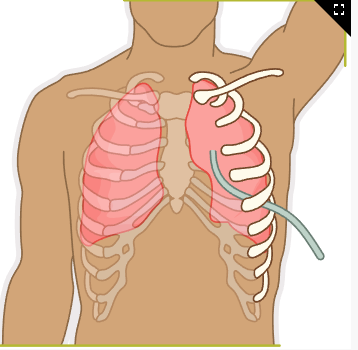
Chest Tube Insertion
Indications
Removal of air, blood, fluid, or pus from pleural or mediastinal space
Restore lung expansion and cardiopulmonary stability
Potential Diagnoses
Pneumothorax
Air in pleural space causing partial to complete lung collapse
Hemothorax
Blood in pleural space causing lung collapse
Postoperative Chest Drainage
Thoracotomy or open-heart surgery
Pleural Effusion
Fluid accumulation in pleural space
Pulmonary Empyema
Pus in pleural space due to infection, lung abscess, or infected effusion
Client Presentation
Dyspnea (impaired gas exchange)
Distended neck veins (possible increased intrathoracic pressure)
Hemodynamic instability
Pleuritic chest pain
Cough
Absent or diminished breath sounds on affected side
Hyperresonance to percussion (pneumothorax)
Dullness or flatness to percussion (hemothorax, pleural effusion)
Asymmetrical chest wall movement
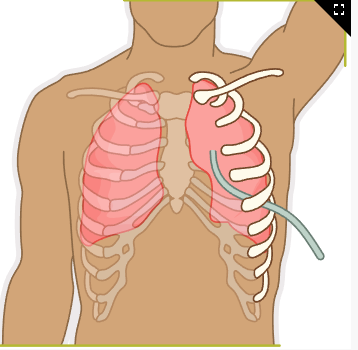
Chest Tube Insertion Consideration
Preprocedure
Verify informed consent is signed
Explain procedure and expected improvement in breathing (reduces anxiety, promotes cooperation)
Assess for allergies to local anesthetics
Position client supine or semi-Fowler’s
Prepare chest drainage system per facility protocol
Fill water seal chamber to prescribed level
Administer prescribed analgesia and sedation
Prep insertion site with povidone-iodine or approved antiseptic
Intraprocedure
Tube placement depends on indication
Fluid drainage: tip near lung base
Air removal: tip near lung apex
Assist provider with insertion, dressing application, and drainage system setup
Place drainage system below chest level
Keep tubing straight and unobstructed to promote gravity drainage
Continuously monitor vital signs and client response
Postprocedure
Assess at least every 4 hr
Vital signs
Breath sounds
SpO₂
Skin color
Respiratory effort
Encourage coughing and deep breathing every 2 hr
Keep drainage system below chest level at all times, including ambulation
Monitor chest tube placement and function
Check water seal level every 2 hr and refill as needed
Expect tidaling with respirations
Document drainage amount and color
Hourly for first 24 hr
At least every 8 hr after
Mark date, time, and level on container each shift
Report drainage >70 mL/hr, sudden increases, cloudy, or red drainage
Monitor suction control chamber and maintain prescribed level
Verify dry suction regulator setting if applicable
Ensure no dependent loops, kinks, occlusions, or loose connections
Continuous bubbling only in suction chamber, not water seal
Monitor insertion site
Redness
Pain
Signs of infection
Crepitus (subcutaneous emphysema)
Tape all connections securely
Position semi-Fowler’s to promote lung expansion
Administer pain medication as prescribed
Obtain chest x-ray to confirm placement
Keep two hemostats, sterile water, and occlusive dressing at bedside
Clamp chest tube only if prescribed
Risk of tension pneumothorax if clamped improperly
Do not milk, strip, or clamp tubing unless prescribed
Excessive negative pressure can damage lung tissue
Notify provider immediately if
SpO₂ < 90%
Chest tube eyelets become visible
Drainage stops or exceeds prescribed amount in first 24 hr
Complications occur
Chest Tube Removal
Administer pain medication 30 min before removal
Assist provider with sutures and removal
Instruct client to
Exhale and bear down (Valsalva maneuver)
Or take a deep breath and hold
(Increases intrathoracic pressure, prevents air entry)
Apply airtight sterile petrolatum gauze dressing
Secure with heavy tape
Obtain follow-up chest x-ray as prescribed
Monitor for
Excessive drainage
Infection
Recurrent pneumothorax
Chest Tube Insertion Complication
Air Leaks
Often caused by unsecured connections
Nursing Actions
Monitor water seal chamber for continuous bubbling
Check and tighten all connections
Notify provider if air leak persists
If prescribed, briefly clamp tubing with padded clamp to locate leak
Remove clamp immediately after assessment
Accidental Disconnection, System Breakage, or Removal
Medical emergency requiring immediate provider or rapid response notification
Nursing Actions
If tubing disconnects
Instruct client to exhale and cough
If drainage system is damaged
Submerge chest tube end in sterile water to reestablish water seal
If chest tube is removed
Cover site with dry sterile gauze and occlusive dressing
Tension Pneumothorax
Causes
Sucking chest wound
Prolonged clamping
Kinked or obstructed tubing
High PEEP mechanical ventilation
Assessment findings
Tracheal deviation
Absent breath sounds on one side
Distended neck veins
Severe respiratory distress
Chest asymmetry
Cyanosis
Notify provider or rapid response team immediately
A nurse is caring for a client who has a chest tube and drainage system in place. The nurse observes that the chest tube was accidentally removed. In what order should the nurse perform the following actions?
1
Assess respiratory status.
2
Obtain a chest x-ray.
3
Apply sterile gauze to the insertion site..
4
Place tape around the insertion site.
When prioritizing hypothesis, the nurse should identify the greatest risk to the client is injury from air entering the pleural space and causing the development of a tension pneumothorax.
Application of a sterile gauze to the site is the first action the nurse should take. This prevents air from entering the pleural space and reduces the risk for development of a tension pneumothorax.
The nurse should, next, place tape around the insertion site to ensure the sterile gauze remains intact.
Next, the nurse should assess the client’s respiratory status for indications of respiratory distress.
After assessing the client, nurse should obtain a chest x-ray to determine if the lung is inflated or if the client has a pneumothorax after the chest tube was accidentally removed.
1
Apply sterile gauze to the insertion site.
2
Place tape around the insertion site.
3
Assess respiratory status.
4
Obtain a chest x-ray.
A nurse is assessing a client who has a chest tube and drainage system in place. Which of the following are expected findings?
Select all that apply.
a
Continuous bubbling in the water seal chamber
b
Gentle constant bubbling in the suction control chamber
c
Rise and fall in the level of water in the water seal chamber with inspiration and expiration
d
Exposed sutures without dressing
e
Drainage system upright at chest level
b Gentle constant bubbling in the suction control chamber
c Rise and fall in the level of water in the water seal chamber with inspiration and expiration
A nurse is assisting a provider with the removal of a chest tube. Which of the following actions should the nurse take?
a
Instruct the client to lie prone with arms by the sides.
b
Complete a surgical checklist on the client.
c
Remind the client that there is minimal discomfort during the removal process.
d
Place an occlusive dressing over the site once the tube is removed.
d
Place an occlusive dressing over the site once the tube is removed.