Conduction Disorders pt. 2 - Clin Med
1/131
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
132 Terms
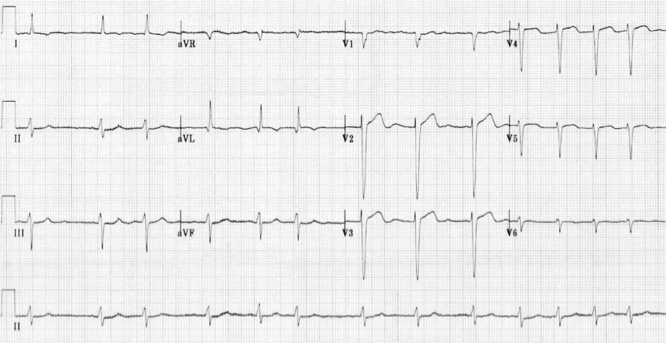
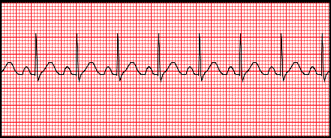
What does this refer to
A 68-year-old male presents with palpitations, lightheadedness, and weakness.
These symptoms appear to worsen with increased alcohol intake.
Medical history is significant for hypertension being treated with hydrochlorothiazide.
On physical exam, the patient appears uncomfortable.
There is an irregularly irregular pulse when palpating the radial artery.
On cardiac auscultation, the first heart sound (S1) is of variable intensity.
There is mild bibasilar crackles on pulmonary auscultation and an absence of peripheral edema.
An electrocardiogram is obtained.
Atrial Fibrillation (A-Fib)
What does this refer to
Supraventricular Tachyarrhythmia due to uncoordinated atrial contractions
Quivering or irregular (arrhythmia)
Types
Normal rate < 100 bpm
Rapid Ventricular Response (RVR) = ventricular rate > 100 bpm
A-fib is irregularly irregular
Atrial Fibrillation (A-Fib)
What does this refer to
normal ventricular response (< 100 bpm) Atrial Fibrillation (A-Fib)
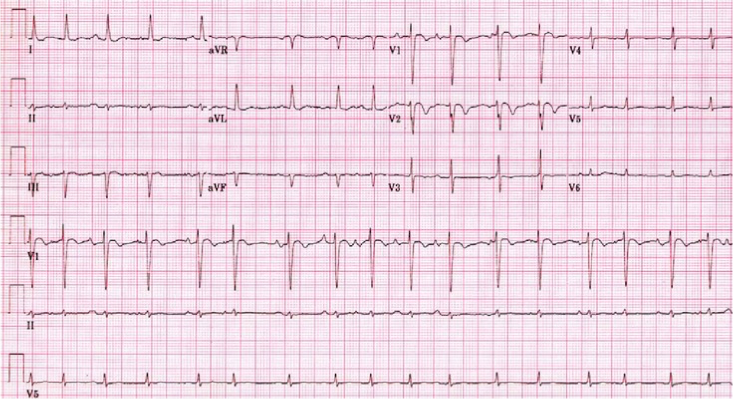
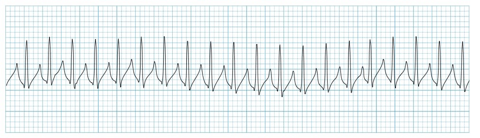
What does this refer to
rapid ventricular response (RVR) > 100 bpm) Atrial Fibrillation (A-Fib)
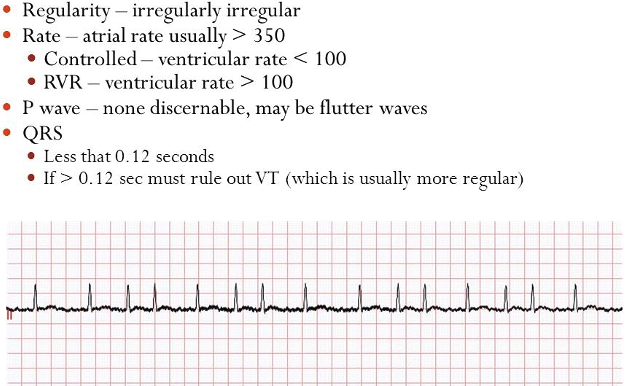
Atrial Fibrillation
What does this refer to
Atrial fibrillation (AF) is the most frequently encountered cardiac arrhythmia
Prevalence
< 55 yo 0.1%
> 60 yo 3.8%
> 80 yo 10%
M > F
Caucasians > AA
May occur in the absence of comorbidities
Epidemiology of Atrial Fibrillation (A-Fib)
What does this refer to
Structural abnormalities – left atrial enlargement
Mitral and aortic stenosis, mitral and aortic regurgitation
Conduction abnormalities
WPW
Medications
Theophylline and Digitalis
Cardiac function abnormalities
MI, PE or CAD
Hyperthyroidism
Electrolyte disturbance
Cardiomyopathies
Etiology Atrial Fibrillation (A-Fib)
What does this refer to
Supraventricular tachyarrhythmia due to uncoordinated atrial contractions
Often due to atrial enlargement, inflammation or infiltrative diseases of the atrium
Non-repetitive pattern of the RRi
Strong associations with other cardiovascular diseases
Risk Factors
Hemodynamic stress
Atrial ischemia
Inflammation
Alcohol – drug use
Endocrine disorders
Neurologic disorders
Genetic factors
Etiology of Atrial Fibrillation (A-Fib)
What does this refer to
Asymptomatic OR symptomatic
Palpitations
Dyspnea/DOE
Syncope
Fatigue
Dizziness
Angina
Decompensated heart failure
Clinical history of Atrial Fibrillation (A-Fib)
What does this refer to
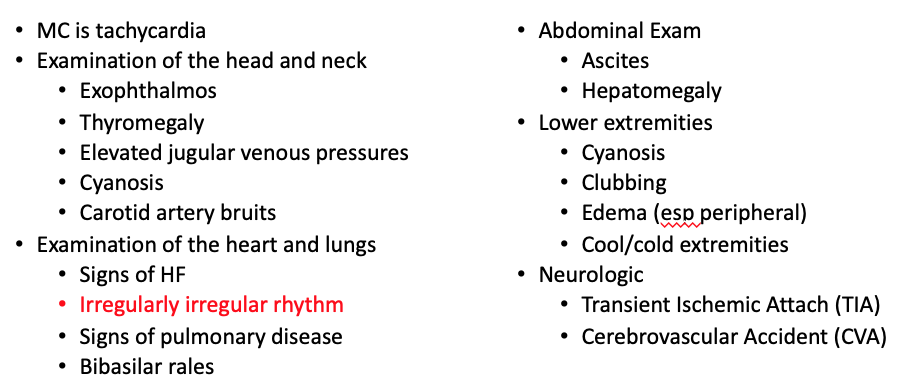
Physical exam of Atrial Fibrillation (A-Fib)
What does this refer to
Atrial flutter
Multifocal atrial tachycardia
Premature atrial contractions
SVT
Wolff-Parkinson-White (WPW)
Differential diagnosis Atrial Fibrillation (A-Fib)
What does this refer to
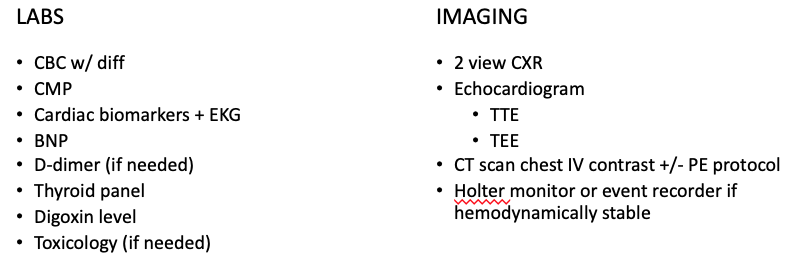
Workup for atrial fibrillation (A-Fib)
What does this refer to
Assess atrial size and ventricular
Function
Thickness
Size
Assess valvular and pericardial disease
Measure peak right ventricular pressure
Transthoracic echo (TTE)
What does this refer to
“More sensitive to detect thrombi in L atrium”
Transesophageal echo (TEE)
What does this refer to
New Onset
Hemodynamically stable
Admit to telemetry bed (Med-Surg Tele)
Cardiology consult
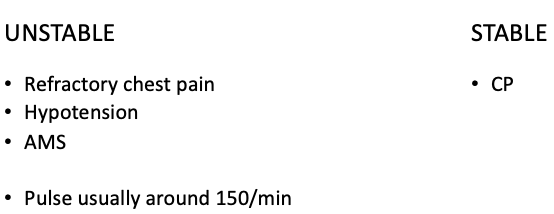
Unstable
ICU
Disposition/management Atrial Fibrillation (A-Fib)
What does this refer to
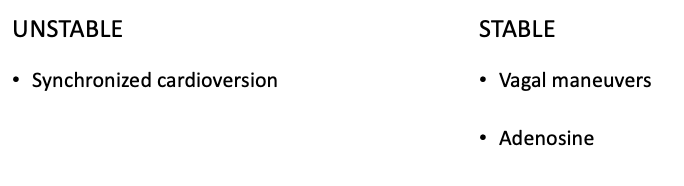
Hemodynamically stable?
Hemodynamically unstable
Synchronized cardioversion
Catheter ablation
Clinical management of Atrial Fibrillation (A-Fib)
What does this refer to
Rate control is # 1
Start here
THEN Rhythm?
Even with rate control
High risk patients should also have rhythm control
Who is high risk?
CAD
HF
Young patients
Everyone gets some type of anticoagulant/blood thinner
ASA +/- Clopidogrel (Plavix) [remember the score] OR
Warfarin (Coumadin)
Dabigatran (Pradaxa)
Rivaroxaban (Xarelto)
Apixaban (Eliquis)
Do we treat rate, rhythm or both? Atrial Fibrillation (A-Fib)
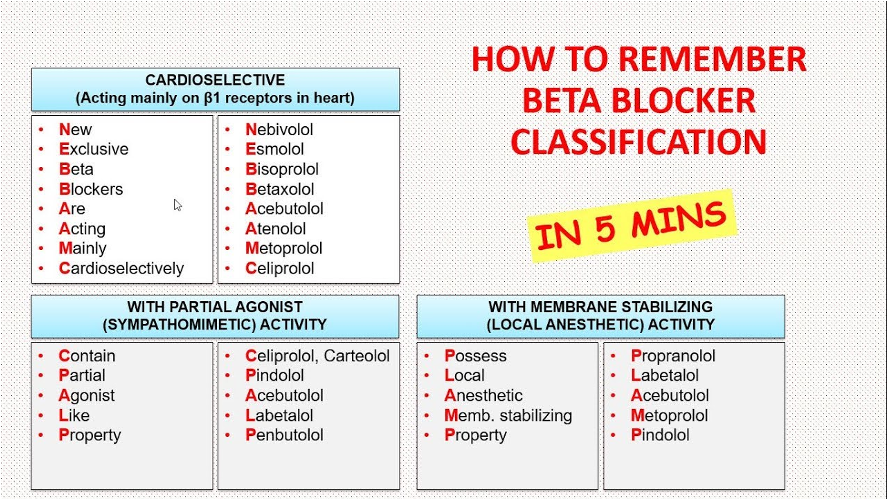
Just know it
What does this refer to
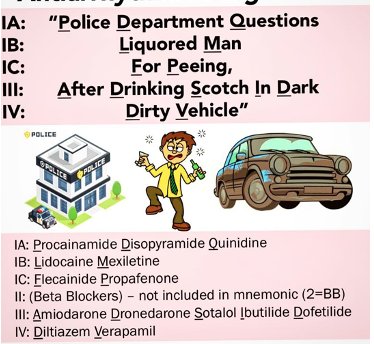
Antiarrhythmics Atrial Fibrillation (A-Fib)
What does this refer to
New onset A-fib and hemodynamically stable
BB or CCB
Long term management (rate)
BB or CCB
BB w. hx CAD
Digoxin w. hx HF w. reduced EF
Long term management (rhythm)
Drug choices based on patient comorbidities
Clinical management Atrial Fibrillation (A-Fib)
What does this refer to
New onset (acute) A-fib
Beta blockers
CCB
A-fib RVR
Diltiazem (Cardizem) or Metoprolol (Lopressor) IV
Anticoagulation
New onset
If cardioversion required – LMWH +/- Warfarin (Coumadin)
Acute Clinical management New Onset – Atrial Fibrillation (A-Fib)
What does this refer to
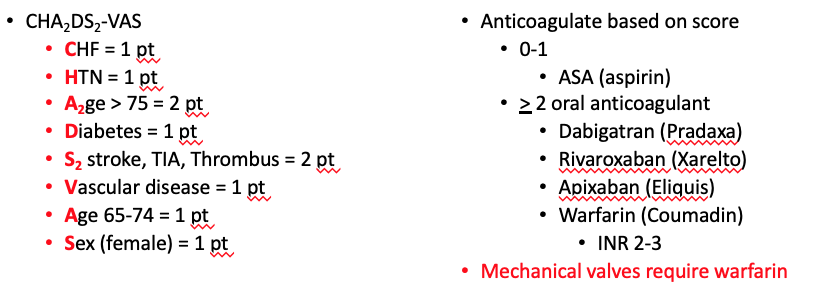
Long term anticoagulation risk Atrial Fibrillation (A-Fib)
What does this refer to
Anticoagulation
Warfarin (Coumadin)
Dabigatran (Pradaxa)
Rivaroxaban (Xarelto)
Apixaban (Eliquis)
Edoxaban (Savaysa)
Rate control (B-blockers)
Metoprolol
Antiarrhythmics (CCB)
Verapamil (Calan)
Diltiazem (Cardizem)
HFrEF —> digoxin preferred therapy
Long term management Atrial Fibrillation (A-Fib)
What does this refer to
1.5 – 2x higher risk of death
Most often due to the strong association between AF and thromboembolic events
Dislodgement or fragmentation of a clot can then lead to embolic phenomena, including stroke
High risk for development of HF
High risk of Renal infarct
Prognosis of Atrial Fibrillation (A-Fib)
What does this refer to
A 64-year-old woman presents to the emergency room for several hours of lightheadedness and palpitations.
Her past medical history includes hypertension, mitral valve regurgitation, and chronic obstructive pulmonary disease.
On physical exam, her pulse is around 150/min.
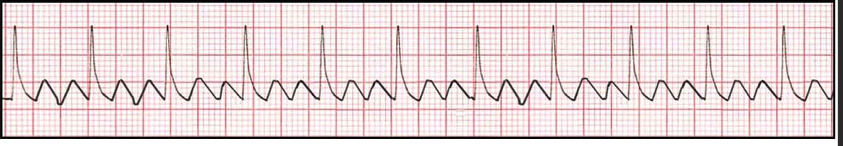
An electrocardiogram is administered, revealing a narrow complex tachycardia and sawtooth-like waves in leads II, III, and aVF.
Atrial flutter
What does this refer to
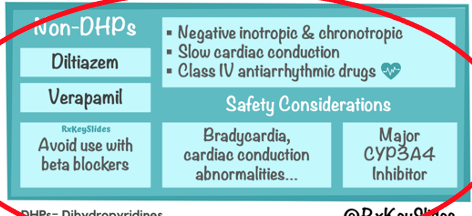
Non-dihydropyridine calcium channel blocker
What does this refer to
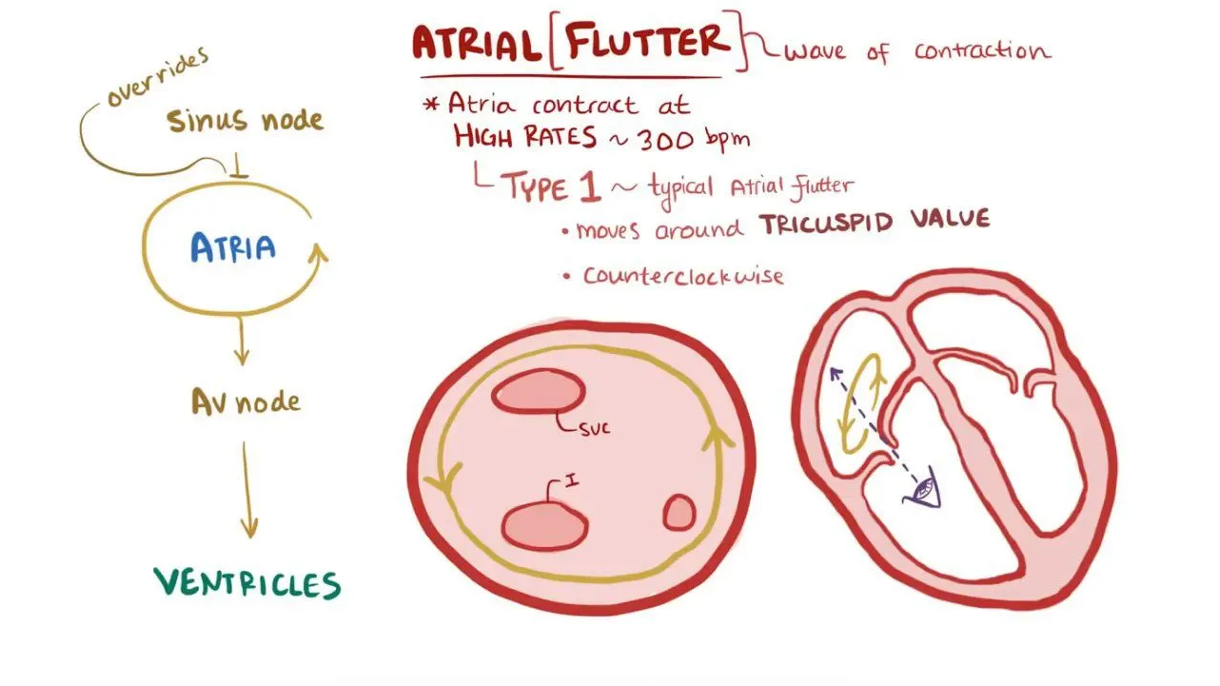
One atrial foci firing at a fast rate
Rate usually > 300 bpm
Atrial Flutter (A-Flutter)
What does this refer to
Risk factors/Associated conditions
Chronic obstructive lung disease
Heart disease
Alcohol use
Diseases of mitral valve
Epidemiology Atrial Flutter (A-Flutter)
What does this refer to
Etiology of Atrial Flutter (A-Flutter)
What does this refer to
Palpitations
Dizziness +/- syncope
Fatigue
Dyspnea/DOE
Chest pain
Clinical history Atrial Flutter (A-Flutter)
What does this refer to
Physical exam Atrial Flutter (A-Flutter)
What does this refer to
Atrial fibrillation
Atrial tachycardia with AV block
Multifocal atrial tachycardia
Differential diagnosis atrial flutter (A-flutter)
What does this refer to
CBC w/ diff
CMP
Cardiac biomarkers + EKG
BNP (HF)
2 view CXR
Echocardiogram
Workup for Atrial Flutter (A-Flutter)
What does this refer to
Clinical intervention Atrial Flutter (A-Flutter)
What does this refer to
Clinical Management of a Stable patient in atrial flutter (A-Flutter)
What does this refer to
“Morbidity and mortality usually related to syncope and HF”
Prognosis of Atrial Flutter (A-Flutter)
What does this refer to
A 17-year-old girl presents to the emergency room with lightheadedness and palpitation.
Her pulse is 250/min and she is hemodynamically stable.
An electrocardiogram shows an antidromic atrioventricular reentrant tachycardia.
She is given procainamide with a resolution of the arrhythmia.
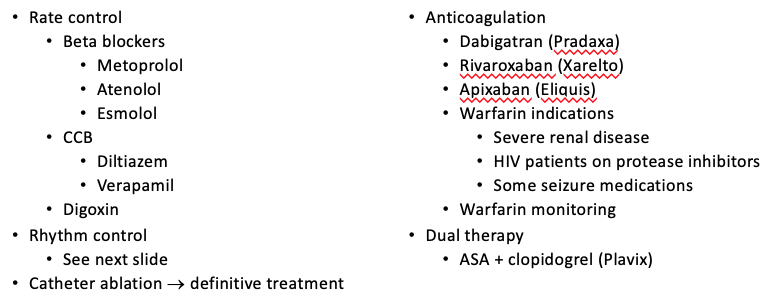
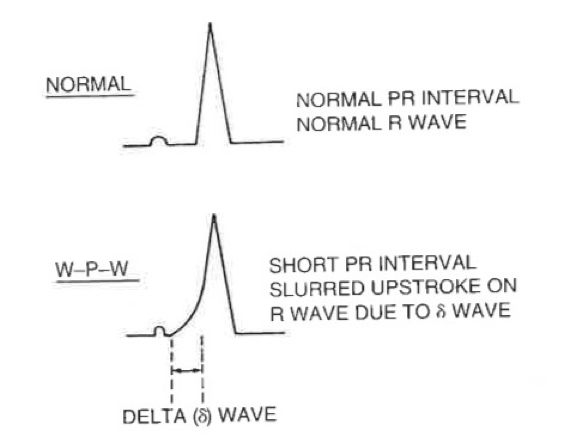
Now in sinus rhythm, she is found to have a widened QRS, delta wave, and shortened PR interval on the electrocardiogram.
Wolff-Parkinson-white (WPW)
What does this refer to
The delta wave
What does this refer to
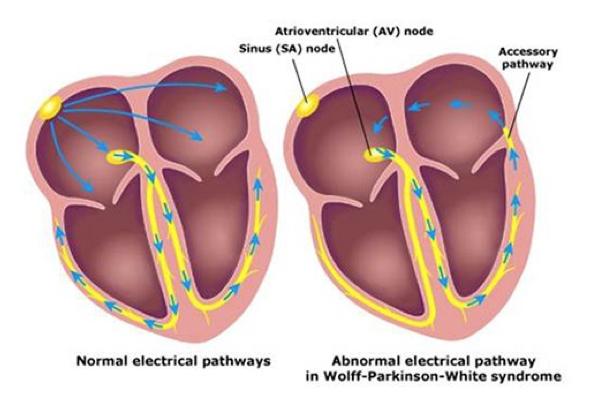
Atria and ventricles are electrically isolated
Conduction of electrical impulses from the atria to the ventricles normally occurring via the atrioventricular node and His-Purkinje system
NOT the case with WPW
Normal AV Conduction
What does this refer to
Pre-excitation manifest on an ECG and symptomatic arrhythmias involving the accessory pathway
Ventricular myocardium is activated early as a result of this bypass pathway, prior to activation via the normal AV node/His-Purkinje pathway
Etiology Wolff-Parkinson-white (WPW)
What does this refer to
Have an additional pathway —> accessory pathway (AP)
Directly connects atria and ventricles, allowing electrical activity to bypass AV node
Tissue in the accessory pathways, congenital in origin
Typically conducts electrical impulses more quickly than the AV node, resulting in shorter PR interval on ECG
Patients with pre-excitation syndrome (Wolff-Parkinson-white (WPW) Syndrome)
What does this refer to
1-3/1000 people affected
Most have no other evidence of heart disease
80% of patients with WPW have reciprocating tachycardia such as A-fib/A-Flutter
Mitral Valve Prolapse (MVP) has an association with WPW
Effects all ages, but bimodal distribution
Infancy
School age children and adolescence
Incidence decreases with age
M > F
No racial predilection
Family history probably greatest risk factor
Epidemiology Wolff-Parkinson-white (WPW)
What does this refer to
Accessory pathway outside of the AV node “preexcites” the ventricles
AV node is bypassed
Pathology
Bypassing AV node causes ventricles to depolarize earlier than normal
Etiology Wolff-Parkinson-white (WPW)
What does this refer to
Tachycardia
What does this refer to
SVT
What does this refer to
Anatomy and physiology of Wolff-Parkinson-White (WPW)
What does this refer to
Symptoms are the result of tachycardia
Palpitations
Lightheadedness and/or dizziness
Syncope or pre-syncope/near syncope
Chest pain
Sudden cardiac death
Clinical history Wolff-Parkinson-white (WPW)
What does this refer to
Usually requires only an electrocardiogram (ECG)
Typically an incidental finding for another clinical indication
Identification of a short PR interval and a delta wave is usually adequate to confirm the diagnosis of WPW pattern*
*Rarely, invasive electrophysiology testing to confirm the diagnosis (competitive athletes)
How’s it diagnosed? Wolff-Parkinson-white (WPW)
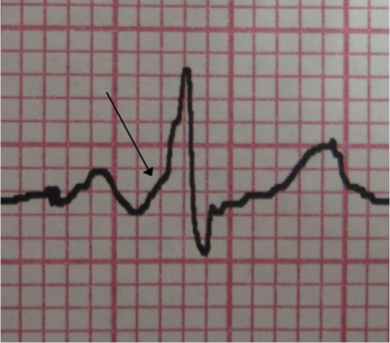
What does this refer to
12-lead showing WPW pattern
W – wave (delta) (arrow on image)
P - PR interval (<0.12 seconds) short
W – wide QRS
Wolff-Parkinson-white (WPW) Syndrome
What does this refer to
Myocardial infarction
PVC
Bundle branch block
Congenital heart defect
Hypertrophic cardiomyopathy
Differential diagnosis Wolff-Parkinson-white (WPW)
What does this refer to (very important)
Complains of 1-2 symptoms
Chest Pain/Short of Breath/Dizzy
Awake
Oriented
Speak in full sentences
Hemodynamically Stable
What does this refer to (Very important)
Symptoms are a result of an abnormal rhythm
Altered Mental Status (AMS)
Loss of Consciousness (LOC)
Shock
Hypotension
Pulmonary Edema
Poor Perfusion
Hemodynamically unstable
What does this refer to
CCB and Digoxin CONTRAINDICATED in (true) _______
Calcium channel blockers or digoxin will worsen a supraventricular tachycardia (SVT) caused by WPW syndrome
Clinical pharmacotherapeutics Wolff-Parkinson-white (WPW)
What does this refer to
Impulse traveling in the opposite direction to what is normal in that nerve fiber
Antidromic Atrioventricular Reciprocating Tachycardia (Wolff-Parkinson-White)
What does this refer
Impulse that is traveling in the normal direction in a nerve fiber
More common
Orthodromic Atrioventricular Reciprocating Tachycardia (Wolff-Parkinson-White)
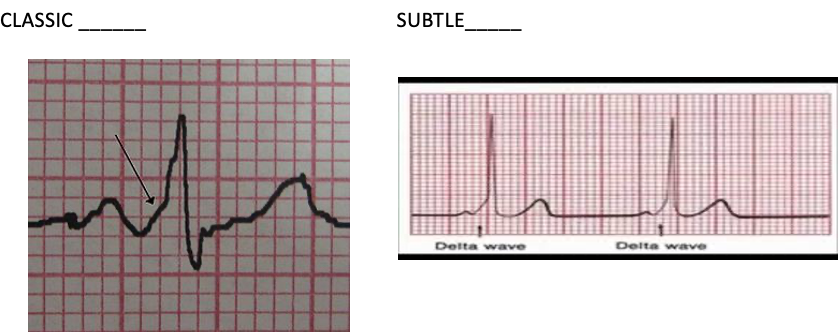
This is the clinical management for what?
Synchronized cardioversion
Unstable Orthodromic narrow QRS complex (Wolff-Parkinson-White)
What is the first line of treatment for a patient with stable orthodromic wide QRS complex (Wolff-Parkinson-White)
Procainamide (Procan)
What is the treatemnt for a patient with orthodromic narrow QRS complex only (Wolff-Parkinson-White)
IV adenosine (6 mg)
What does this refer to
1st Line Treatment for Stable patients
Vagal maneuvers
Carotid sinus massage
Valsalva maneuver
1ST line WIDE QRS COMPLEX
Procainamide (Procan)
2nd line NARROW QRS COMPLEX ONLY
IV adenosine (6mg)
3rd line
IV verapamil OR diltiazem
Clinical management for orthodromic narrow QRS complex for stable (Wolff-Parkinson-White)
What clinical management is this for
Edison before medicine
Synchronized cardioversion
Unstable antidromic wide QRS complex
What clinical management is this for
MEDICINE BEFORE EDISON
1st Line Treatment for Stable patients
Procainamide
Ibutilide
Stable antidromic wide QRS complex
What is this referring
Preferred long-term treatment
Catheter-based radiofrequency ablation is definitive
Clinical management of Wolff-Parkinson-White (WPW)
What does this refer to
Patient placed in a supine or semi-recumbent position
Instructed to exhale forcefully against a closed glottis after a normal inspiratory effort
Signs of adequacy → Are they doing it right?
Neck vein distension, increased tone in abdominal muscles, flushed face
Patient should maintain the strain for 10-15 seconds
Then release and resume normal breathing
Have patient blow into 10 mL syringe just enough to move the plunger around 40 mmHg pressure
Vagal Maneuvers Wolff-Parkinson-white (WPW)
What does this refer to
Placed supine with neck extended (chin away from chest)
Carotid sinus located inferior to angle of mandible at level of thyroid cartilage
Pressure applied to one carotid sinus for 5-10 seconds
Pressure via vigorous circular motion may be more effective, steady pressure recommended (may be more reproducible)
If expected response not obtained
Repeat on other side after a one- to two-minute delay
Contraindications
Avoided if prior TIA/stroke and in patients with carotid bruits
Carotid Sinus Massage Wolff-Parkinson-white (WPW)
What does this refer to
A 28-year-old woman presents to the emergency department for palpitations and lightheadedness.
She reports that her symptoms began approximately 20 minutes ago and it has not subsided.
Medical history is significant for hyperthyroidism.
Vital signs are significant for a blood pressure of 135/95 mmHg and a pulse of 155/min.
An electrocardiogram is performed that shows a narrow QRS-complex tachyarrhythmia.
Carotid sinus massage is performed and her symptoms do not improve.
Vagal maneuvers do not improve her symptoms
Intravenous adenosine is administered and her pulse decreases to 79/min.
Supraventricular tachycardia (SVT)
What does this refer to
Rapid heartbeats that begin in or involve the upper chambers (atria) of the heart
Usually sudden onset
Common forms of ______ —> NARROW COMPLEX
Paroxysmal Supraventricular Tachycardia (PSVT)
Atrial Fibrillation
Atrial Flutter/Atrial Tachycardia
WPW
Supraventricular Tachycardia (SVT)
What does this refer to
Type of “short-circuit” arrhythmia
Age > 50yo
Coronary Artery Disease (CAD)
Previous heart surgery
Epidemiology Supraventricular Tachycardia (SVT)
What does this refer to
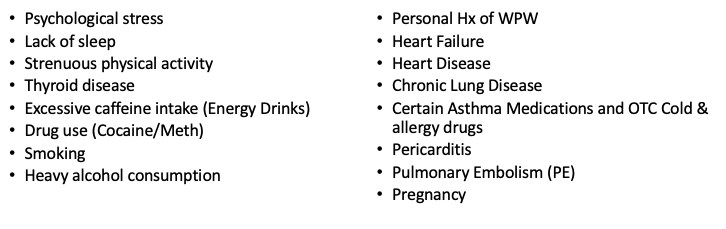
Etiology Supraventricular Tachycardia (SVT)
What does this refer to
Fluttering sensation in the chest
Rapid heartbeat (palpitations)
Shortness of breath
Lightheadedness or dizziness
Sweating
Pounding sensation in the neck
Syncope/Near Syncope
Clinical history Supraventricular Tachycardia (SVT)
What does this refer to
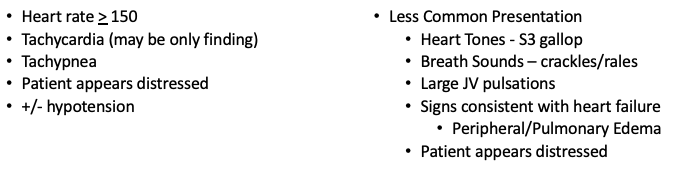
Physical exam supraventricular tachycardia (SVT)
What does this refer to
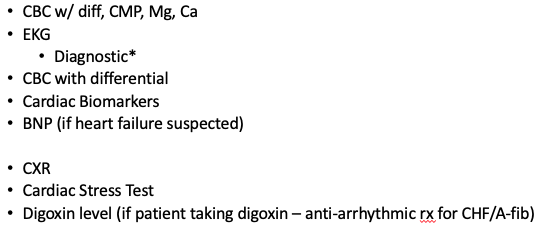
Workup for supraventricular tachycardia
What does this refer to
Time of onset
Very sudden/abrupt
Identified trigger
Previous episodes/treatment
EKG findings [per the 2015 ACLS guidelines]
Narrow complex tachycardia
Rate > 150
Absent or “buried P waves”
Diagnosis of Supraventricular Tachycardia (SVT)
What does this refer to
Atrial Fib
Atrial Flutter
Ventricular Tachycardia
Differential diagnosis of supraventricular tachycardia (SVT)
What does this refer to
In stable patients, perform vagal maneuvers
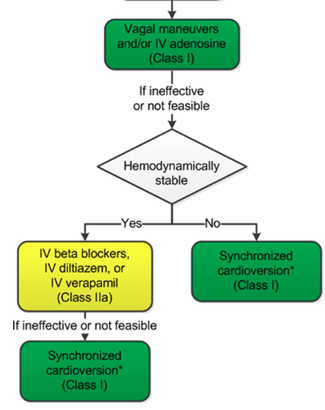
Clinical intervention for regular supraventricular tachycardia (SVT)
What is the first line of treatment for supraventricular tachycardia (SVT)
adenosine
What does this refer to

Clinical management for stable supraventricular tachycardia (SVT)

What does this refer to
Synchronized cardioversion
Clinical management of unstable supraventricular tachycardia
What does this refer to
Symptomatic Wolff-Parkinson-White Syndrome (WPW) syndrome
Small risk of sudden death.
Prognosis in paroxysmal SVT is dependent on any underlying structural heart disease
Patients with a structurally normal heart have an excellent prognosis
May result in heart failure/pulmonary edema/myocardial ischemia/ myocardial infarct
Prognosis of supraventricular tachycardia (SVT)
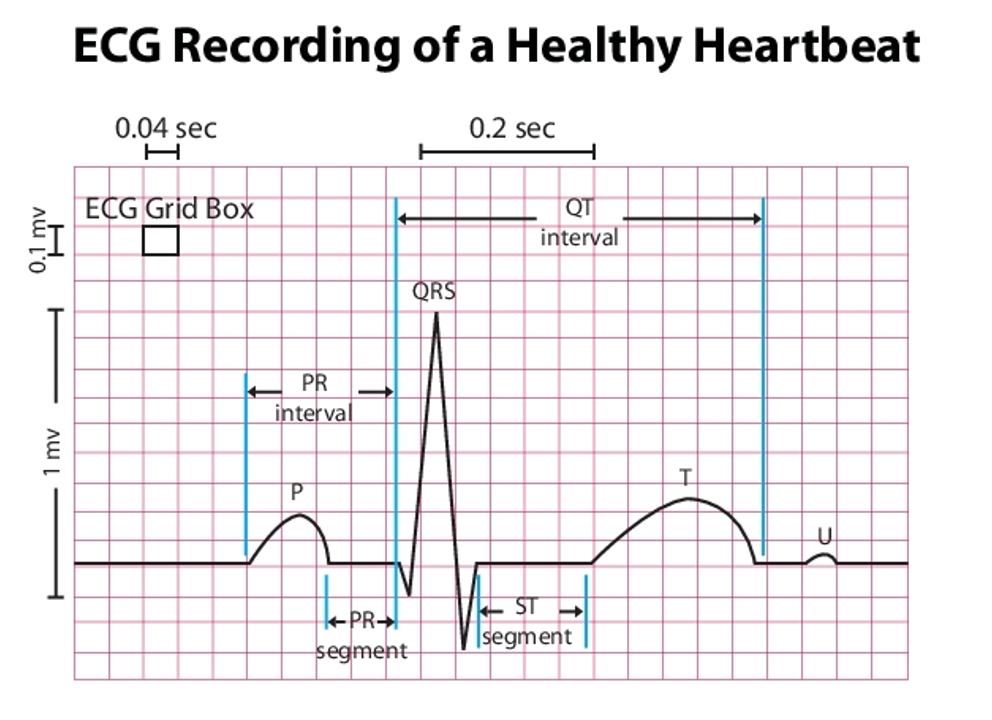
How many boxes should your PR interval be in a normal healthy heartbeat? (beginning of P to end of R)
4 boxes
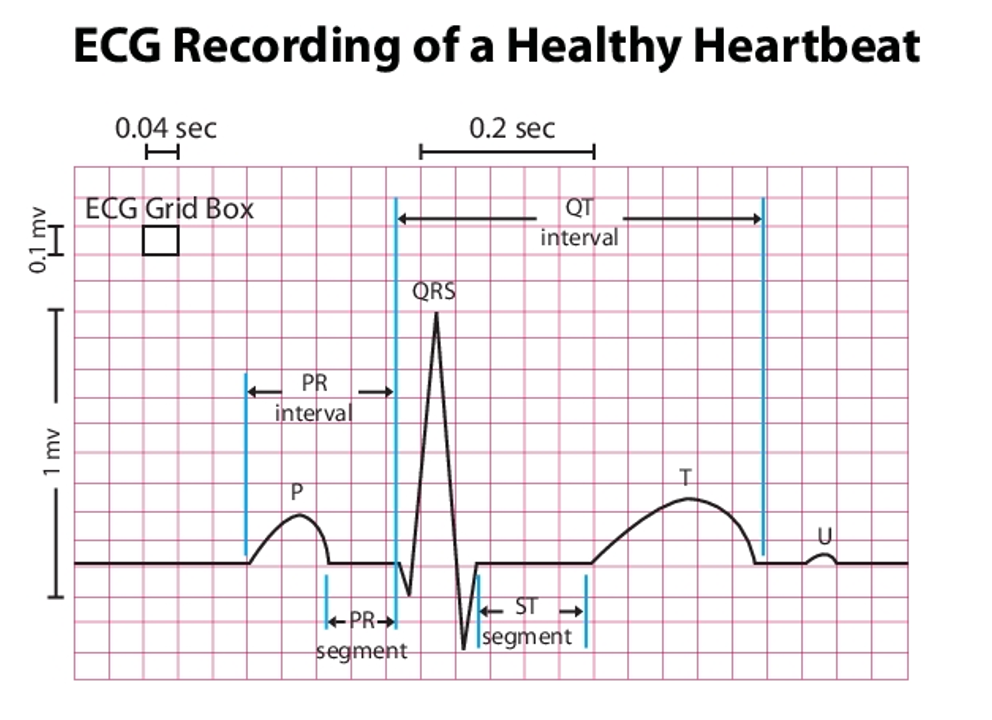
How many boxes should your PR segment be in a normal healthy heartbeat? (end of P to beginning of R)
2 boxes
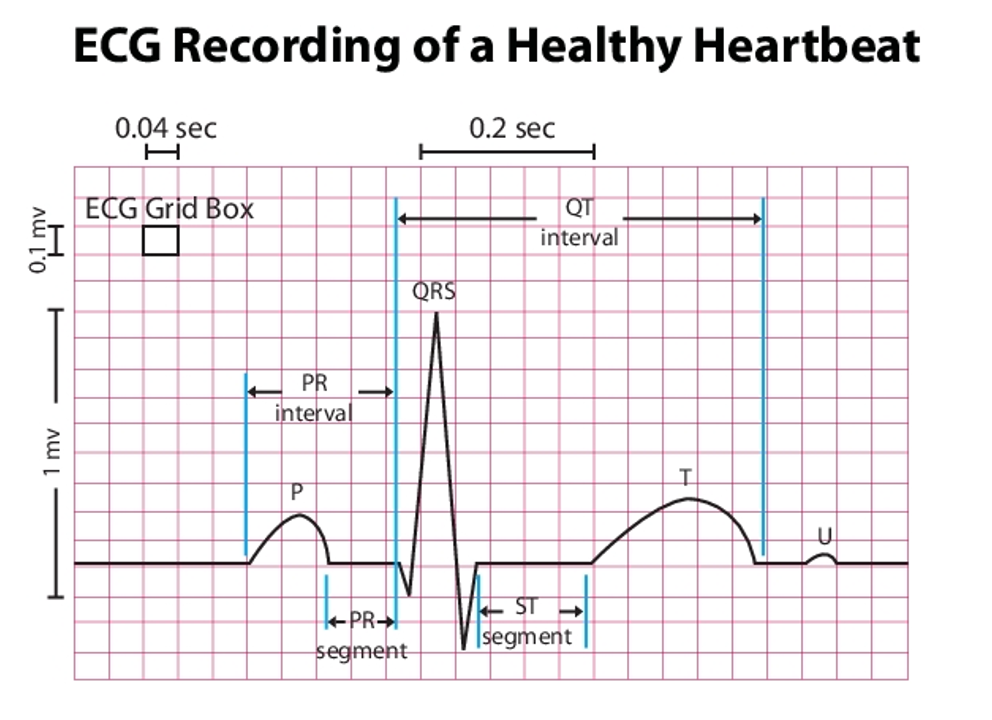
How many boxes should your QT interval be in a normal healthy heartbeat? (beginning of Q to end of T)
11 boxes
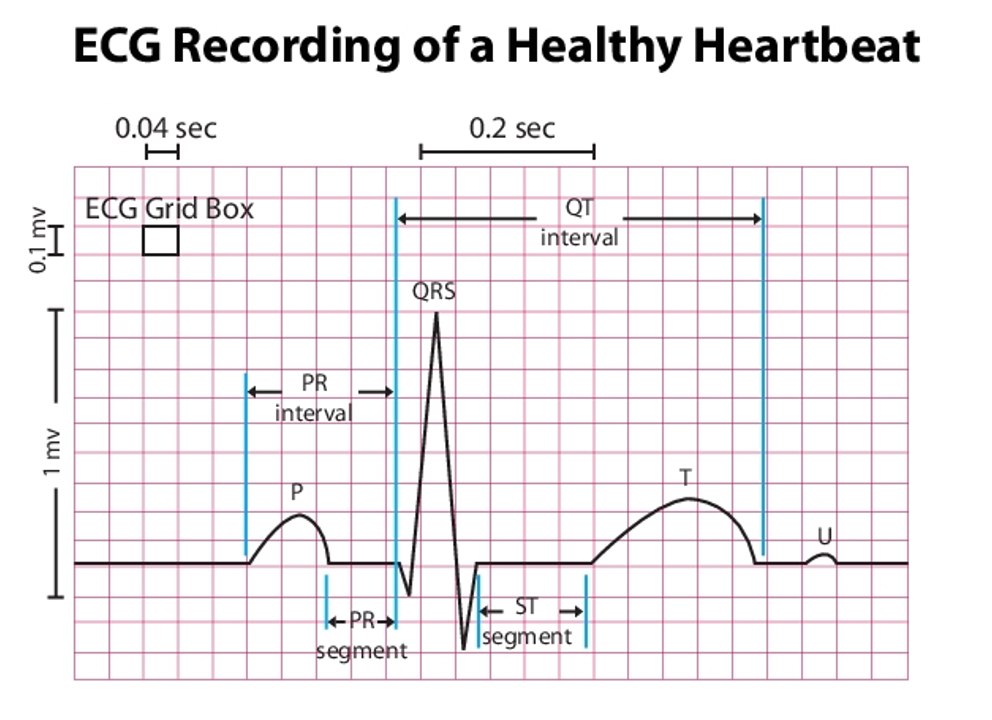
How many boxes should your ST segment be in a normal healthy heartbeat? (beginning of S to beginning of T)
4 boxes
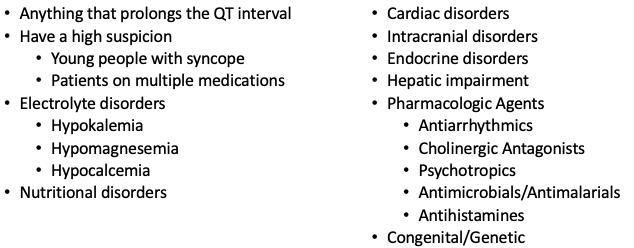
What does this refer to
A disorder of myocardial repolarization
Characterized by a prolonged QT interval
Qtc >0.44 in men considered prolonged (normal < or = 0.44)
Qtc >0.47 in women considered prolonged (normal 0.45-0.47)
Long QT syndrome
What does this refer to
Incidence difficult to determine accurately
Congenital LQTS estimated at 1 in 3000 in general population
Epidemiology of Long QT syndrome
What does this refer to
May be either congenital or acquired
Congenital
Jervell and Lange-Nielsen Syndrome
Autosomal recessive
Associated with congenital sensorineural deafness
Romano-Ward Syndrome
Autosomal dominant
No sensorineural deafness
Acquired _______
Drug therapy
Electrolyte imbalance
Etiology of Long QT syndrome
What does this refer to
Major classes of drugs that prolong the QT interval
Antiarrhythmic drugs (Quinidine)
Certain non-sedating antihistamines (terfenadine)
Macrolide antibiotics (Azithromycin)
Certain psychotropic medications (Haloperidol)
Certain gastric motility agents (cisapride)
A COMMON “EVERY DAY USE” DRUG? ONDANSETRON (ZOFRAN)
Lists of drugs that prolong QT interval @ www.crediblemeds.org/
Drug classes Long QT Syndrome
Which congenital Long QT syndrome is the below
Autosomal recessive
Associated with congenital sensorineural deafness
Jervell and Lange-Nielsen Syndrome
What does this refer to
Autosomal dominant
No sensorineural deafness
Romano-Ward Syndrome
What does this refer to
class IA Antiarrhythmics (quinidine, procainamide, and disopyramide)
class III Antiarrhythmics (sotalol and ibutilide)
antiBiotics
antipsyChotics
antiDepressants
antiEmetics
diuertics (e.g., furosemide)
Etiology Drugs (ABCDEF) Long QT Syndrome
What does this refer to
Clinical manifestations of congenital LQTS highly variable
Many have no symptoms
ASYMPTOMATIC
Symptoms (generally from an arrhythmia)
Palpitations/tachycardia
Pallor
Syncope
Seizures
Cardiac arrest
Clinical history/physical exam Long QT Syndrome
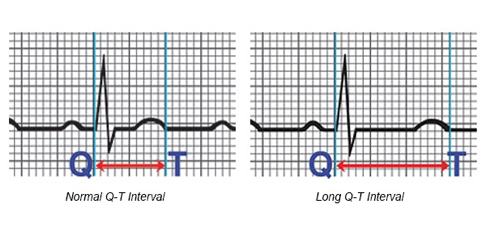
What does this refer to
QTi often measured in Lead II of a 12 Lead
Measured from onset of Q to end of T wave
QT varies inversely with heart rate, therefore a corrected QT (QTc) is obtained
Qtc > 0.44 in men considered prolonged
Qtc > 0.47 in women considered prolonged (normal 0.45-0.47)
> 0.50 considered highly abnormal (increasing danger)
Diagnosis Long QT Syndrome
What does this refer to
Patients with a possible overdose of a QT-prolonging drug should be evaluated for risk of Torsades de Pointes (TdP)
Cornerstone of management of acquired LQTS?
Identify and stop any precipitating drug
A permanent pacemaker may be required in the occasional patient with a chronic bradyarrhythmia
Mild QT prolongation
Without TdP or syncope may be tolerated and monitored as an outpatient
Clinical intervention Long QT Syndrome
What does this refer to
CBC w. diff
CMP
EKG/cardiac biomarkers
CXR
Workup Long QT Syndrome
What does this refer to
LQTS associated with an increased risk of a characteristic life-threatening cardiac arrhythmia
Torsades de pointes (tōr-sad' dĕ pwant'), (TdP)
An atypical, rapid, and bizarre form of ventricular tachycardia
Long QT Syndrome (Gone Wrong)
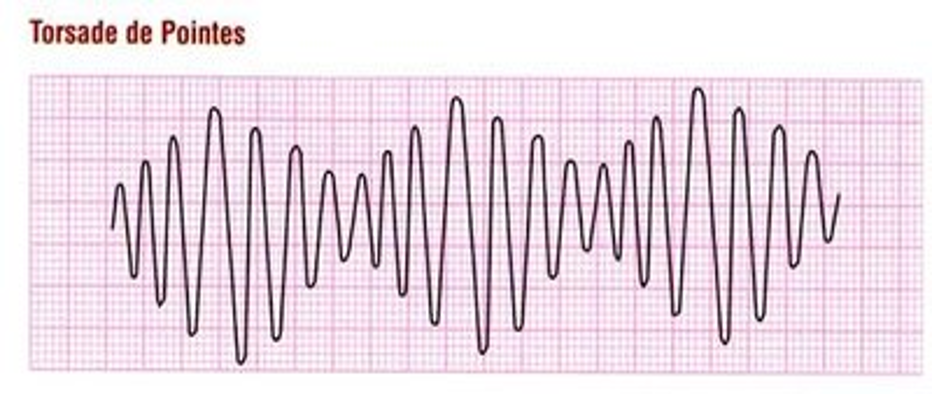
What does this refer to
___________is an uncommon and distinctive form of polymorphic ventricular tachycardia (VT) characterized by a gradual change in the amplitude and twisting of the QRS complexes around the isoelectric line
Typical HR 150-250 bpm
Associated with prolonged QT syndrome
Acquired
Congenital
Torsades de Pointes
What does this refer to
Total incidence and prevalence of TdP is unknown
Often manifests as syncope or sudden cardiac death (SCD)
Women (longer QT) > Men
Wide age range, most frequently in 35-50 yo
Epidemiology Torsades de Pointes
What does this refer to
Many cases present as sudden cardiac death
Recurrent palpitations, syncope, dizziness
Nonspecific symptoms
Nausea
Chest pain
Dyspnea
Diaphoresis
Obtaining a good drug history is essential and includes*
Prescription drugs
OTC drugs
Illicit drugs
Herbal medications
Clinical history of Torsades de Pointes
What does this refer to
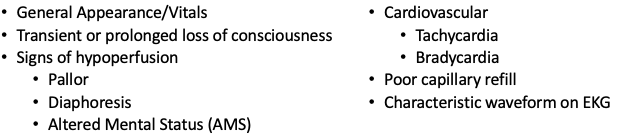
Physical exam for Torsades de Pointes
What does this refer to
Etiology of Torsades de Pointes
What does this refer to
Many cases present as sudden cardiac death
Recurrent palpitations, syncope, dizziness
Nonspecific symptoms
Nausea
Chest pain
Dyspnea
Diaphoresis
Obtaining a good drug history is essential and includes*
Prescription drugs
OTC drugs
Illicit drugs
Herbal medications
Clinical History of Torsades de Pointes