Rad Protection Unit 3- personnel protection
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
NCRP occupational exposure limits
annual effective dose
50 mSv
does not include medical or background radiaiton exposure
cumulative effective dose
age in years x 10 mSv
ALARA
concept
as low as reasonably achievable
collimate
technique
shielding
minimize repeats
methods to reduce exposure
avoid repeat exposure
collimation- increase (make light field smaller)
cumulative timer
highest occupational exposures are: fluoro, portables, and OR
stand 90 degrees from the patient
filtration
non useful low energy photons are removed, less scatter
distance from patient…
patient is a source of scatter radiation
3 feet from the patient (1 meter), the scatter radiation is approximately 1/1000 the intensity
example: if patient exposure is 20 mGy, technologist standing 1 meter at 90 degrees would be exposed to 0.02 mGy
methods to reduce your exposure
protective apparel
lead aprons and protective barries
proper exposure factors
controls scatter (lower kVp, less scatter produced)
correct image acquisition
reduces repeats
high speed image receptors
high speed systems use smaller exposures which causes less scatter
beam limiting devices
reduces scatter
protection of pregnant personnel
should be able to continue duties without interruption of employment
voluntary declaring vs. not declaring
couseling
second “baby badge” is issued worn at waist level
to reduce risk of leukemia or other malignancies
0.5 mSv in one month
5 mSv for the entire pregnancy
must read and sign a form acknowledging counseling
if wearing a lead apron, the 2nd badge is worn inside the apron at waist level
baby badge has a separate reading on the dose report
maternal tissue decreases fetus dose by 30%
work schedule rotation
does not necessarily have to be done
types of radiation
primary radiation
scatter radiation
leakage radiation
primary radiation
useful beam
emerges directly from the tube collimator
scatter radiation
highest does to technologist
primary beam passes through matter and goes in various directions
leakage radiation
escapes the tube housing
protective structural shielding
usually lead or concrete
barriers
primary protective barrier
secondary protective barrier
primary protective barrier
located perpedicular to the primary beam travel (undeflected line of travel)
prevents direct or unscattered radiation from reaching personnel and general public
for 130 kVp of peak energy a 1/16 (~1.6mm)inch of lead or lead equivalent and extends 7 feet (2.1m) upward from the floor if the tube is 5-7 from the wall (1.5-2.1m)
secondary protective barrier
any wall or barrier that is never hit by the primary beam
protects agaist scatter and leakage radiation
1/32 inch of lead or lead equivalent (~0.8 mm)
overlaps the primary barries by ½ inch (~1.3 mm) and extends to the ceiling
protective device requirements
lead apron
0.5 mm lead (Pb) for fluroscopy, AIR, or operating systems aboe 100 kVp (NCRP #102)
protects from 95-99% of scattered radiation
gloves
minimum of 0.25 mm lead (Pb)
neck and thyroid
must be at least 0.5 mm lead (Pb)
protective eyeglasses
0.35 mm lead (Pb) to protect the eyes
protective tube housing
lead lined metal that protects personnel and patients from leakage and off focus radiation
cannot exceed 1 mGy per hour at 1 m away from housing
no one should be touching the xray tube housing during an exposure
protection during fluoroscopy
proper position to be standing
avoid high scatter areas
try to stand behind the physician/ radiologist or RA
90 degrees from the patient, away from the source
wrap around lead
need to move around the room to obtain supplies
should be thyroid shield
unprotected areas are getting 10-20x more exposure
collimation
filtration
technical factors
high speed image receptors
correct image acquisition
appropriate skin to source distance
cumulative timer
rotational scheduling of personnel
personnel must wear the badge on the outside of the lead apron at collar level
remote control fluoro units
can perform the study from the control booth and enter room only when necessary
scatter protection barrier in fluoro
protective curtain
0.25 mm lead equivalent
gonadal protection
bucky slot cover
0.25 mm lead equivalent
protection in mobile radiogrpahy
cord length should be long enough to stand 6 feet (2m) from the patient
stand 90 degrees from the patient
use distance as a means of protection
wear protective shield
yell “x-ray” before taking exposure
do not hold the image receptor
use cassette holders, pillows, sponges, or even a box of gloves
protection in C-arm fluoroscopy
proper position to be standing
in a lateral view, on the side of the patient away from the x-ray tube
protective shields and radiation monitros for all personnel
properly orient the c-arm with the image intensifier on top
minimise beam on time
position the image intensifier as close to the patient as possible to lower the beam intensity needed
advanced interventional radiology (AIR) protection
low dose fluoroscopy mode/ pulse fluoro
collimation
last image hold
shortening duration of studies
extremity monitors
rings- NCRP annual limits to 500 mSv
imaging personnel protection guidelines
technologist should never stand in the path of the primary beam
if holding is necessary, try to utilize a non-occupationally exposed person or immobilization
pregnant technologist technologist are never to hold a patient for an exposure
exposures should never be made witht the doors to room open
cardinal principles of radiation protection
Time- amount of exposure is directly proportional to duration of the exposure
Distance- most effective means of protection, it is indirectly proportional
Shielding- absorbs most of the energy of scatter radiation
~ 85% effectiveness
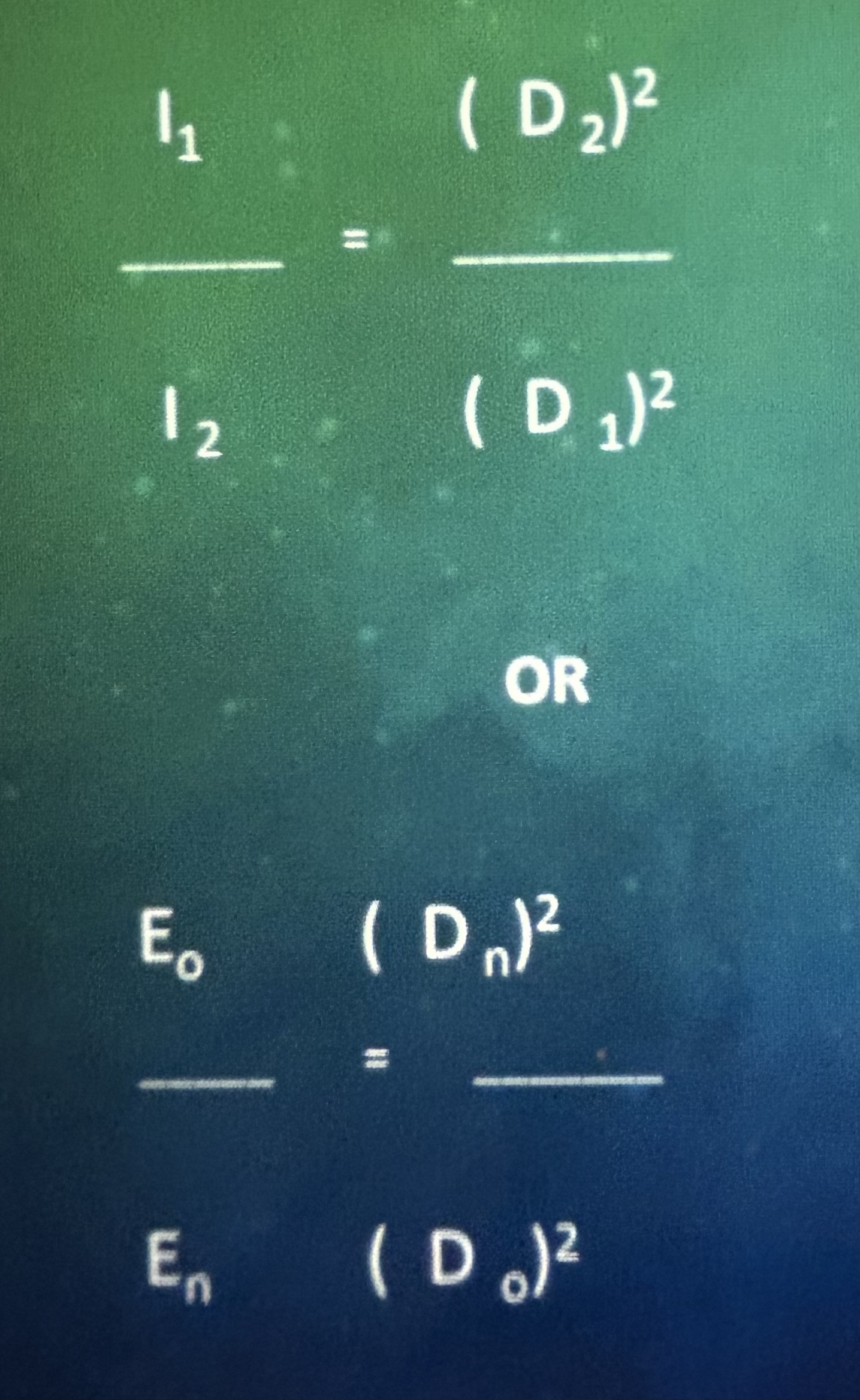
Inverse square law (ISL) equation
diagnostic protection design
workload (W)
radiation on time during a week
mAs/week or mA- minute/week
Use (U)
amount of time the bean is directed at the structure'
takes into account primary or secondary radiation
occupancy (T)
time that the area is occupied behind a barrier
waiting room
empty courtyard
distance (D)
distance from the source to the structure
calculating barrier requirements
W x U x T
needs to be calculated for every barrier in an x-ray room
areas of the department
controlled- occupied by workers who are trained and wearing monitoring devices; maximum permitted equivalent dose is 100 mrem per week
uncontrolled- occupied by the general public; maximum permitted equivalent dose is 2 mrem per week
waiting rooms
hallways
bathrooms
stairways
radiation area sign posting
radiation symbol that is magenta, purple or black on a yellow background
radiaiton hazard (rad Onc and NM)
high radiaiton area
very high radiaiton area
Airborne radioactivity
radioactive materials
warning signs
signs that indicate the room is in use