Neuromuscular Blocking Agents (Week 3, Mod 7)
1/16
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
What are 4 situations where we would use muscle relaxants clinically?
1) To offset muscle hypertonicity with ketamine
BZPs (benzodiazepines)
Alpha-2 agonists
2) To relieve muscle spasms
BZPs
3) To facilitate smooth induction of anesthesia in large animals
4) To improve surgical conditions
Deep general anesthesia
Local anesthesia
Centrally acting muscle relaxants
Neuromuscular blocking drugs (muscle relaxants or NMBs)
What kind of muscle do NMBs target? Smooth, skeletal, or cardiac?
SKELETAL muscle ONLY… targets the somatic (voluntary) nervous system
What do NMBs target SPECIFICALLY?
Target nicotinic acetylcholine receptors at the synaptic cleft in a muscle cell
Are nicotinic receptor ANTAGONISTS
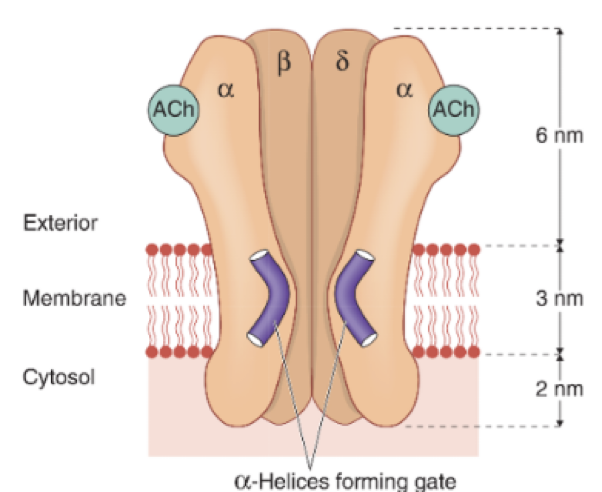
Describe the structure of the nicotinic ACh receptor… how does its conformation change in response to ACh exposure?
Has 5 subunits, each has an alpha helices in the middle
Helices act as a gate, undergo a conformational change when receiving acetylcholine at the two alpha subunits (open)
Allows influx of sodium into the cell to generate an action potential
Describe the general structure of a neuromuscular blocking drug. How does its structure affect its mechanism of action?
NMBs are rigid, bulky molecules with quaternary N (nitrogen with 4 side chains → positively charged)
Can’t diffuse through cell membranes, so has to inhibit receptor extracellularly
Need to block at least 80% of receptors present… only need about 1% of receptors to activate to generate a muscle contraction
What are the effects of NMBs? What kinds of muscles are more susceptible to these effects, and which are less susceptible?
Causes flaccid motor paralysis ONLY of the skeletal muscle; has no analgesic or anesthetic effects
UNETHICAL to perform surgery with only NMBs… patient would be conscious while paralyzed
Muscles that are capable of fast, short contractions will be the first to go (eye muscles, swallowing)
RESPIRATORY muscles are the last to be effected and the first to recover
What are 2 main unwanted side effects of using NMBs? Describe why these happen in detail.
1) Fall in blood pressure - due to GANGLION BLOCK and HISTAMINE RELEASE
Ganglions are highly dependent on nicotinic receptors to receive information, and are found all throughout the body; so could see a decrease in the input to the adrenal medulla, who’s products help to regulate blood pressure
Histamine release can also cause a drop in blood pressure
2) Tachycardia
Tachycardia is a result of the drop in blood pressure; pumps faster in response
PNS is also somewhat blocked by neuromuscular blockers (PNS has MUSCARINIC receptors, which are very similar to nicotinic); PNS acts to slow the heart down, and if this action is blocked, can lead to tachycardia
Describe the pharmacokinetics of NMBs… how does it need to be administered due to its chemical conformation? Describe the rate of onset and duration, as well as how its excreted (very general)
NMBs are a quaternary ammonium compound… means it has a positive charge, so can’t diffuse like normal
As a result of this, MUST be administered IV
Equilibriates with extracellular fluid, allowing the drug to move between cells to target the nicotinic receptors of skeletal muscle cells
Rate of onset and duration vary
Generally metabolised by the liver or excreted uncharged by the kidney
Small Volume of Distribution
Do not cross into “protected” organs eg CNS or placenta
How are muscle relaxants used practically? What are some things you need to consider while using them?
Are only administered IV
Will induce apnoea, so patient must be mechanically ventilated
are only administered to anaesthetised patients
have no anaesthetic or analgesic effects
can be ‘topped up’ or given by IV infusion for as long as required
What in particular do you need to consider while recovering a patient from surgery? Think of what muscles are the first to recover as the NMBs wear off…
Though respiratory muscles are the first to recover after surgery, the muscles that control the airway are actually very sensitive to NMBs
Therefore, though the patient is capable of breathing independently, they are unable to maintain a patent airway
This is why you keep a patient intubated until they start swallowing
What 4 practical procedures would require a neuromuscular blocking drug?
to facilitate endotracheal intubation
to relax skeletal muscle for easier surgical access
to control ventilation during anaesthesia
ophthalmic surgery
Describe the recovery process from NMBs… whats one way we can speed up this process?
Will occur SPONTANEOUSLY
As plasma concentration of relaxant declines, drug will move down its concentration gradient from the neuromuscular junction (NMJ) into plasma
Eventually, sufficient relaxant will have left to restore NM transmission
However, muscle relaxants are competitive antagonists
ACh is broken down by acetylcholinesterase, so if this enzyme is inhibited, ACh levels will increase
If ACh concentrations increase to a sufficient level at the NMJ, transmission will be restored
Therefore, can quicken the process of recovery with ANTICHOLINESTERASES
Inhibits acetylcholinesterase enzyme, keeping it from breaking down ACh as the patient recovers
What effects are commonly seen after using an anti cholinesterase drug? Which nervous system are these symptoms from, and what receptor is responsible?
Can cause:
Bradycardia
Salivation
Bronchoconstricton
Urination and defecation
All stimulated by the PNS… Though antichollinesterases help to increase ACh concentrations at neuromuscular junctions, they also work on EVERY acetylcholinesterase at every synapse in the body… even if its not needed.
Happens at MUSCARINIC receptors
Because of the side effects anticholinesterases cause, what kind of drug is used in conjunction with them? What is this combination usually called?
An antiMUSCARINIC drug
This combo is called anticholinergic drugs… IMPORTANT to know the differences between anticholinergic and anticholinesterases
What is Sugammadex?
An NMB CHEMICAL ANTAGONIST
Interacts chemically with the NMB itself, rendering it inactive
No antimuscarinic needed
Is very expensive, so not commonly used
What are two main factors that could affect the effectiveness of NMBs? Give examples for each.
1) Other drugs
General anesthetics
Antibiotics
Anticholinesterases
2) Pathophysiological conditions
hepatic / renal impairment
age
temperature
acid base balance
electrolyte disturbances
myasthenia gravis - autoimmune disease; destroys nicotinic receptors
What are the two main centrally-acting muscle relaxants??
Benzodiazepines
diazepam; midazolam
Guaifenesin (glycerol gualacolate, “Gee-Gee”)
blocks impulse transmission at internuncial neurones within spinal cord and brain-stem
relaxes limb > respiratory muscle
mild sedation, no analgesia