06: Airway Mechanics Resistance
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
Default status of the airway radius
As wide and relaxed as can be to ensure low resistance and low energy
At a resting state, can you relax/dilate the lower airways
Not to any appreciable degree
How can administering a bronchodilator be a useful diagnostic test
If you administer it and breathing gets easier, then it means that those airways were constricted, and something isn’t normal
What parts of the airway are NOT normally relaxed, and can be actively dilated
Nares
Pharynx
Larynx
Conditions where the upper airway may be actively dilated
Something is wrong
Increased exercise (increased minute ventilation need)
When can you evaluate dilation issues in the upper airway
When an animal is exercising
How is ventilation (breathing) driven
By generating and releasing negative thoracic/pleural pressure in cycles
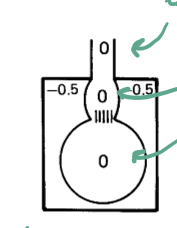
Pressure in the thorax, alveoli, intrathoracic RT, and extrathoracic RT at the end of exhalation
Thorax: small negative
Alveoli: 0
Intra: 0
Extra: 0
Negative all the way through means no air movement, slight negative to keep the elastic components of the RT dilated
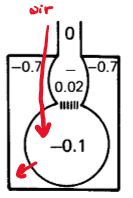
Pressure in the thorax, alveoli, intrathoracic RT, and extrathoracic RT during inhalation
Thorax: slightly larger negative
Alveoli: medium negative
Intra: small negative
Extra: 0
Negative pressure gradient from out (0) → in (-0.7)
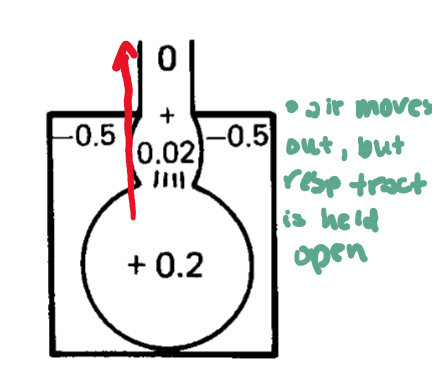
Pressure in the thorax, alveoli, intrathoracic RT, and extrathoracic RT during normal exhalation
Thorax: small negative
Alveoli: medium positive
Intra: small positive
Extra: 0
Muscles relax and generate a positive pressure gradient from in (0.2) → out (0) so the air moves out but the slight negative in the thorax hold the RT open
Pressure in the thorax, alveoli, intrathoracic RT, and extrathoracic RT during forced exhalation
Thorax: positive
Alveoli: large positive
Intra: medium positive
Extra: 0
Muscles force a greater positive gradient by making the thoracic pressure positive while generating a positive gradient from in (8.7) → out (0)
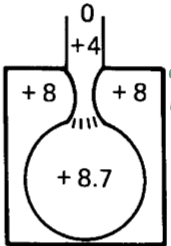
What happens if you forcefully exhale too hard
You can collapse parts of the RT by making the thoracic positive pressure greater than the positive pressure in the RT → reduced exhalation volume despite breathing harder
What determines if the RT collapses when you exhale to hard
Where the pressure pushes in and whether that part of the RT has cartilage or not
What test can be done in humans (and has been done in humans) to diagnose asthma by looking at lower airway mechanics
FEV1
How can dogs increase minute ventilation with a pretty low E input
The are equipped with a better capacity to increase minute ventilation by taking lots of shallow breaths
Why does any RT issue in horses become clinically significant
They increase their work of breathing SO fast (basically a vertical curve) and they really can’t increase minute ventilation with any efficiency
What limits the increase in minute ventilation in humans
Our airways collapse pretty quickly
What is the primary cause of increased resistance in the lower RT
Smooth muscle contraction
What does smooth muscle contraction do to airway mechanics if it happens in the bronchioles
Increases resistance AND decreases lung compliance
Effect of edema in the upper RT
Narrows the space significantly because bone doesn’t dilate, so the fluid has no choice but to distend the mucosa into the lumen (shrinks functional cross section), increasing resistance by a lot
Effect of edema in the lower RT
Narrow the space to a lesser degree because there is no bone and the fluid can distend the mucosa on either side of the lumen, still increases resistance
Increasing resistance increases the energy needed for what parts of breathing
Inhalation, exhalation, or both
If there is increased resistance in the lower RT (intrathoracic), what part of breathing will we see problems in first
Exhalation
If there is increased resistance in the upper RT (extrathoracic), what part of breathing will we see problems in first
Inhalation
When will we see issues if there is a nasal mass or tracheal collapse
Inhalation
When will we see issues if the soft palate is displaced
Exhalation (snoring!!)
When will we see issues if there is laryngeal paresis
Inhalation
Common smooth muscle constrictors
Histamine
Ach
Hypertonic saline
Prostaglandins and leukotrienes (inflammatory molecules)
Ozone
Acid vapor → gastric reflux!
Why do some animals have very severe reactions to a normal, subclinical exposure to a bronchoconstrictor
Airway hyperreactivity
Common situation to see chronic hypersensitivity reactions
Chronic respiratory distress
Why does chronic RT disease result in respiratory hyperreactivity
Disease can cause smooth muscle to become more twitchy
How to test for respiratory hyperreactivity
Administer a small, subclinical dose of a bronchoconstrictor and check for a response that shouldn’t be there