NS 4410 Liver B
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
126 Terms
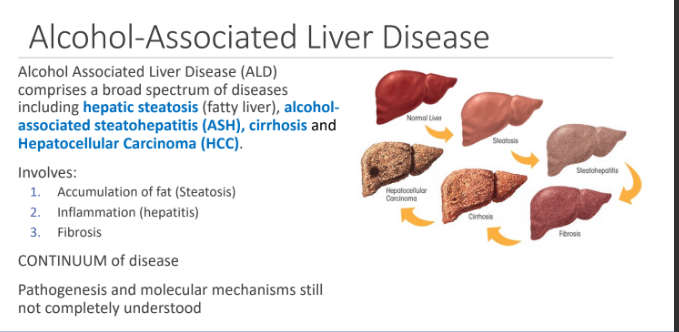
Alcohol Associated Liver Disease (ALD) comprises a broad spectrum of diseases including what 4 conditions?
hepatic steatosis (fatty liver),
alcohol- associated steatohepatitis (ASH)
cirrhosis
hepatocellular Carcinoma (HCC).
Alcohol Associated Liver Disease involves what 3 things?
1. Accumulation of fat (Steatosis)
2. Inflammation (hepatitis)
3. Fibrosis
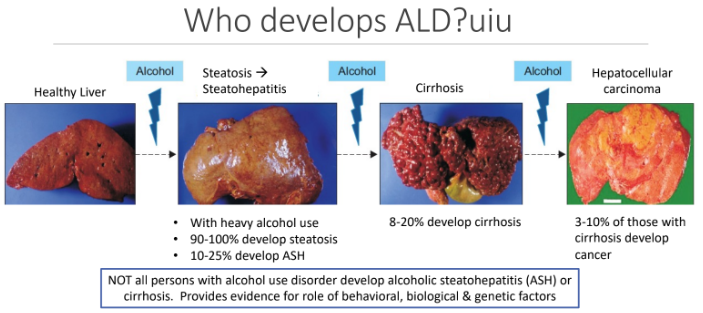
Who develops ALD?
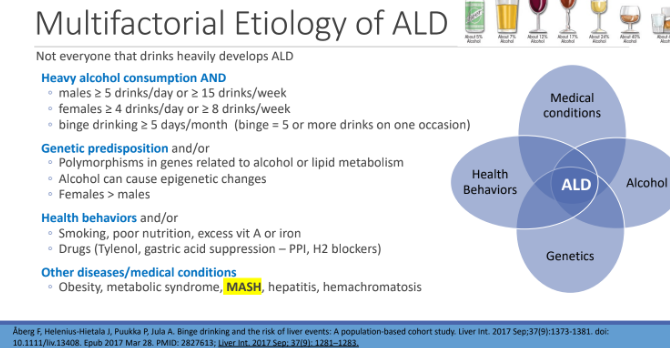
Multifactorial Etiology of ALD Not everyone that drinks heavily develops ALD. What are 4 etiologies?
Heavy alcohol consumption AND
Genetic predisposition and/or
Health behaviors and/or
Other diseases/medical conditions
Etiology: Heavy Alcohol Consumption: Direct relationship between amount of alcohol consumed and probability of developing ___
ALD
Almost all persons consuming > 40g/day regularly (about 3 drinks/day) for 2 weeks or more have
Steatosis
About 10-20% of persons consuming ≥ 400 g/week (4 drinks/day or more) for 10 or more years; i.e. “heavy chronic drinkers”, develop
Cirrhosis
What does Heavy alcohol use mean for men and women?
males ≥ 5 drinks/day or ≥ 15 drinks/week
females ≥ 4 drinks/day or ≥ 8 drinks/week
binge drinking ≥ 5 days/month
Etiology: Binge Drinking: Increased risk of ALD if drink outside of?
meal-times
What is binge drinking?
5 or more drinks, on one occasion, in past month
Binge Drinking may be an independent risk factor for liver disease. Independent of average ___ intake & ____; Higher risk with more frequent ____
alcohol; age; binge drinking
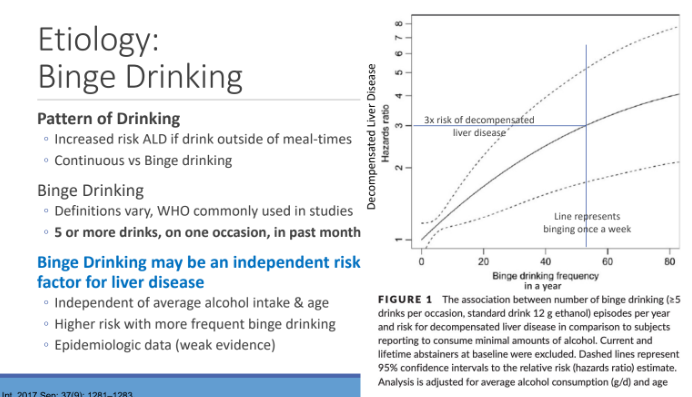
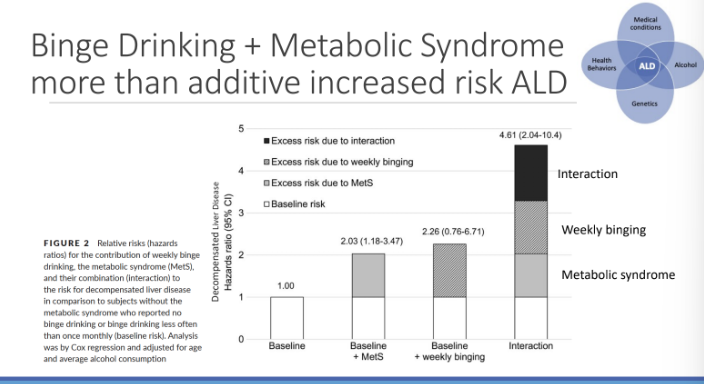
Binge Drinking + metabolic syndrome more than additive increased risk
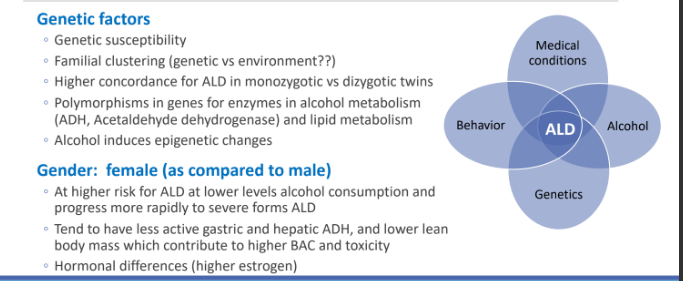
Genetic and Sex Risk factors for ALD: Genetic factors: Alcohol induces what type of changes?
epigenetic changes
Genetic and Sex Risk factors for ALD: Genetic factors: Polymorphisms in genes for enzymes in ____ metabolism and ____ metabolism
alcohol (ADH, Acetaldehyde dehydrogenase); lipid
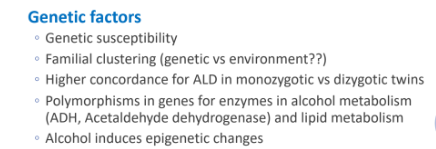
Genetic and Sex Risk factors for ALD: Female, at higher risk for ALD at lower levels of ______ and progress more rapidly to severe forms ALD
alcohol consumption
Genetic and Sex Risk factors for ALD: Females tend to have less active ____ and _______, and lower lean body mass which contribute to higher ____ and toxicity
gastric; hepatic ADH; BAC
Genetic and Sex Risk factors for ALD: There are hormonal differences in gender, what do females have that men don’t
higher estrogen
Behavioral & Medical Risk Factors for ALD: What are 4 behavioral risk factors for ALD?
Smoking: exacerbates effects of alcohol, 3x increase risk
Poor nutrition
Drugs: Acetaminophen (Tylenol), gastric acid suppressors
Nutrients: Vitamin A, iron (toxic to the liver)
Behavioral & Medical Risk Factors for ALD: What are 5 co-occurring medical conditions?
Obesity,
metabolic syndrome
MASH*
Chronic viral hepatitis (Hep B or Hep C)
Iron accumulation in the liver (hemochromatosis)
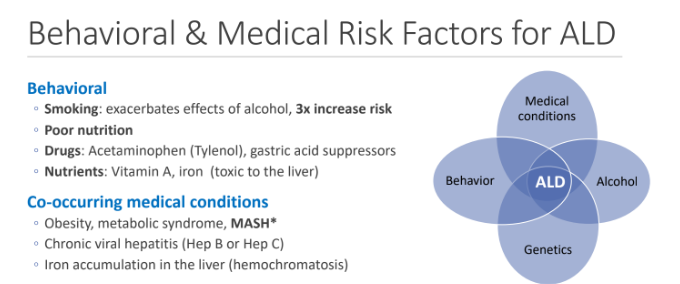
Persons with MASH should refrain from?
ANY alcohol use
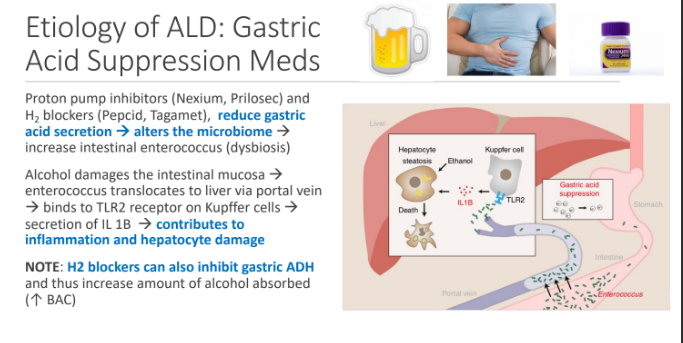
Etiology of ALD: Gastric Acid Suppression Meds: Proton pump inhibitors (Nexium, Prilosec) and H2 blockers (Pepcid, Tagamet), reduce ____ secretion which alters the microbiome which increase intestinal ____
gastric acid; enterococcus (dysbiosis)
Alcohol damages the_____ mucosa which leads to enterococcus translocate to liver via portal vein binds to TLR2 receptor on ____ cells this leads to secretion of ___ → contributes to inflammation and ____ damage
intestinal; Kupffer; IL 1B; hepatocyte
H2 blockers can also inhibit ___ and thus increase amount of alcohol absorbed(↑ BAC)
gastric ADH
Which of the following persons should be advised to reduce consumption of alcohol to reduce their risk of liver disease? More than one answer can be selected.
A. 35-year-old male with MASH, has a few drinks on “special occasions”
several times a year (holidays, family gatherings, birthday celebrations)
B. 26-year-old female with BMI of 35 kg/m2 that drinks “socially” on
weekends and takes Tylenol, Prilosec, and DripDrop (ORS) for her
hangovers
C. 33-year-old female with BMI 22 and HTN that drinks 1-2 glasses of wine on
Friday and Saturday evenings.
D. 46-year-old male with BMI of 27 and T2DM that has 4-5 beers most nights
A, B, D
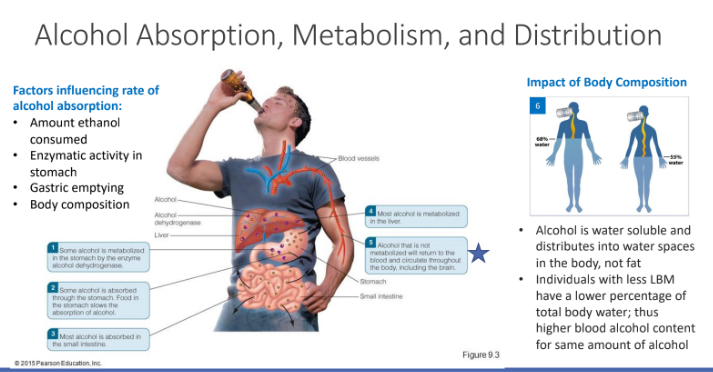
Alcohol primarily absorbed in the___ and ____
stomach (22%); small intestine (~75%)
After absorption alcohol enters the ______, which enters ______ and then metabolized
portal vein; liver
If alcohol consumed exceeds the liver’s capacity to metabolize on “first pass,” alcohol enters _____ and goes to all ____
peripheral circulation; tissues
Minimal amounts of alcohol are excreted what 3 ways?
Feces
Urine
Exhaled by the lungs
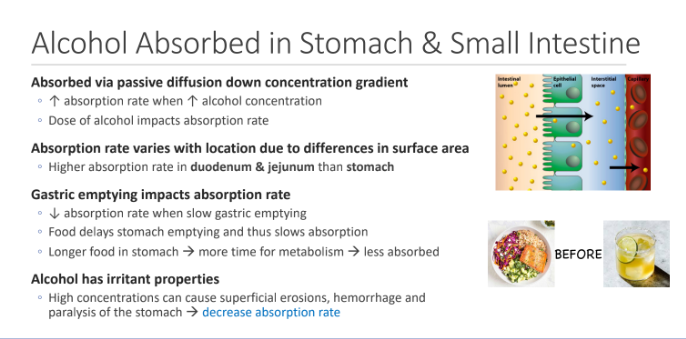
Alcohol Absorbed in Stomach & Small Intestine: Absorbed via ____ diffusion down _____ gradient; There is an increase absorption rate when? What affects absorption rate?
passive; concentration; ↑ alcohol concentration; Dose of alcohol impacts
Absorption rate varies with location due to differences in surface area. There are higher absorption rate in ___ & ____ than stomach
duodenum; jejunum
Gastric emptying impacts absorption rate; ___ absorption rate when slow gastric emptying; ____ delays stomach emptying and thus slows absorption; Longer food in stomach → more time for ____ → less absorbed
decrease; Food; metabolism
Alcohol has irritant properties. High concentrations can cause what 3 things to decrease absorption rate?
Superficial erosions
hemorrhage
paralysis of the stomach
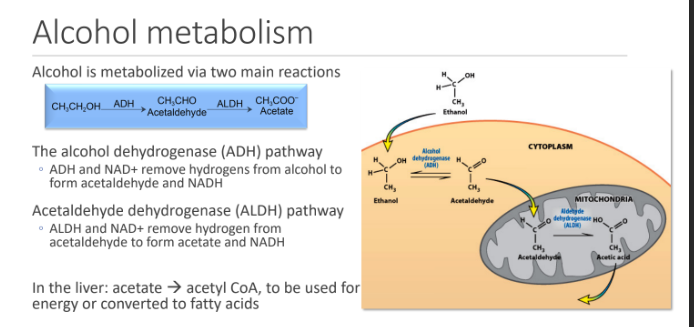
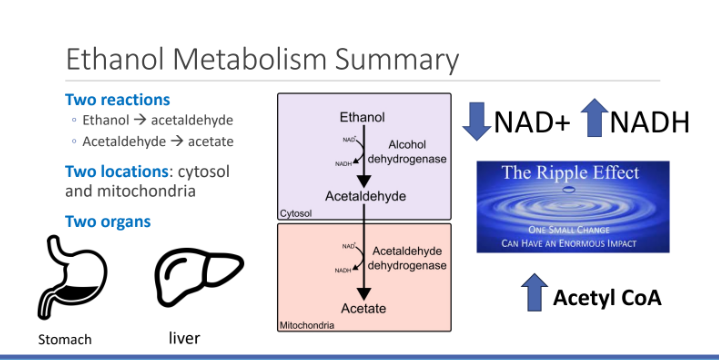
Alcohol is metabolized via two main reactions. What are the two?
The alcohol dehydrogenase (ADH) pathway → ADH and NAD+ remove hydrogens from alcohol to form acetaldehyde and NADH
Acetaldehyde dehydrogenase (ALDH) pathway → ALDH and NAD+ remove hydrogen from acetaldehyde to form acetate and NADH
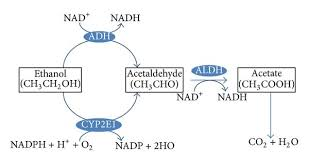
In the liver: acetate → ____, to be used for energy or converted to fatty acids
acetyl CoA
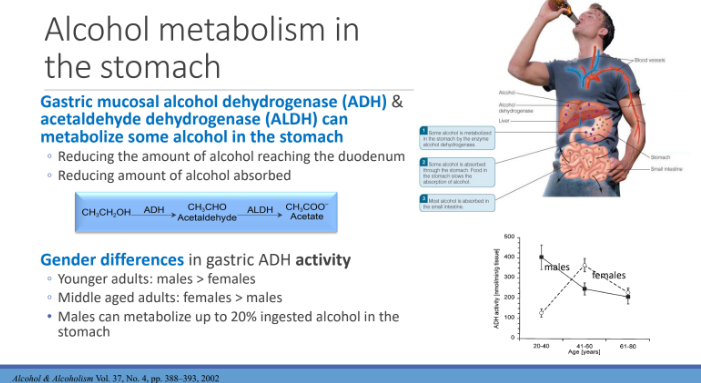
Gastric mucosal alcohol dehydrogenase (ADH) & acetaldehyde dehydrogenase (ALDH) can metabolize some alcohol in the stomach. This reduces what 2 amounts?
Reducing the amount of alcohol reaching the duodenum
Reducing amount of alcohol absorbed
Gender differences in gastric ADH activity
Younger adults: males > females
Middle aged adults: females > males
Males can metabolize up to 20% ingested alcohol in the stomach
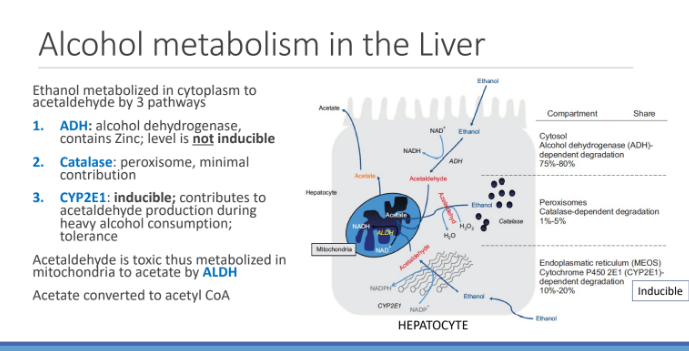
Ethanol metabolized in cytoplasm to acetaldehyde by 3 pathways. What are the 3 ways?
1. ADH: alcohol dehydrogenase, contains Zinc; level is not inducible
2.Catalase: peroxisome, minimal contribution
3 CYP2E1: inducible; contributes to acetaldehyde production during heavy alcohol consumption; tolerance
Acetaldehyde is ____ thus metabolized in mitochondria to acetate by ____ ; Acetate converted to acetyl CoA
toxic; ALDH
What are 4 Factors influencing rate of alcohol absorption:?
Amount ethanol consumed
Enzymatic activity in stomach
Gastric emptying
Body composition
Impact of Body Composition: Alcohol is water soluble and distributes into water spaces in the body, not fat. Individuals with less LBM have a lower percentage of total body water; thus higher?
blood alcohol content for same amount of alcohol
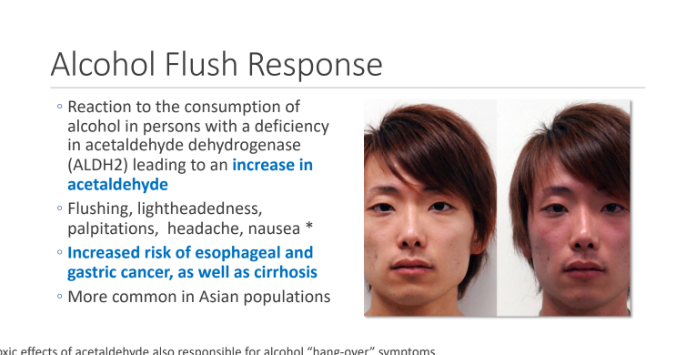
Alcohol Flush Response; Reaction to the consumption of alcohol in persons with a deficiency in _____ leading to an increase in ____
acetaldehyde dehydrogenase (ALDH2); acetaldehyde
What are 5 symptoms of alcohol flush?
Flushing
lightheadedness,
palpitations
headache
nausea
Alcohol Flush Response increased the risk of what 2 things?
esophageal and gastric cancer,
cirrhosis
Blood alcohol concentration is determined by all the following EXCEPT:
A. How many and how rapidly the alcoholic drinks are consumed.
B. How recently the person ate.
C. Amount of caffeine consumed at same time as alcohol.
D. Presence of gastroparesis.
E. Rate of alcohol oxidation in the liver.
c
Alcohol is a DRUG and an ENERGY source. Alcohol is a drug that is detoxified via oxidation to ____ and then to ____ , primarily in the liver
acetaldehyde; acetate
Alcohol is a DRUG and an ENERGY source. the Acetyl CoA generated from acetate is an energy source; caloric value of alcohol is?
7 calories/gram
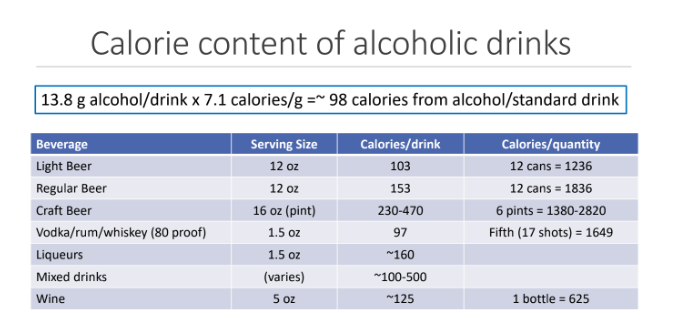
Calorie content of alcoholic drinks
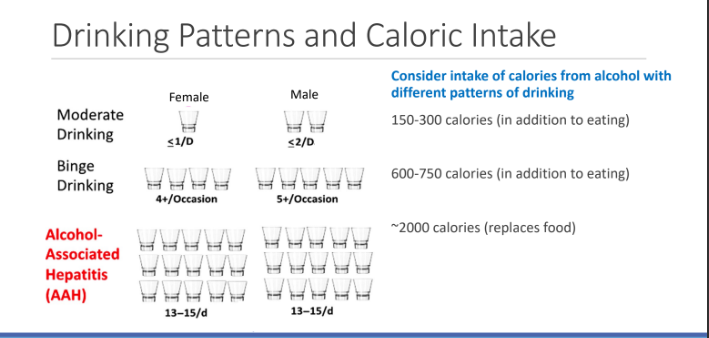
Drinking Patterns and Caloric Intake
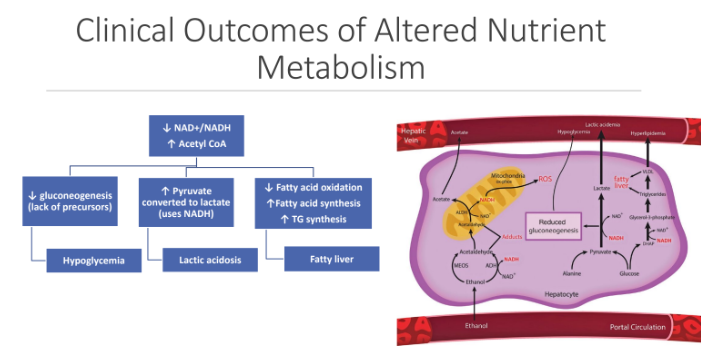
Alcohol metabolism results in What 3 things?
↓NAD+
↑NADH
↑Acetyl CoA
Alcohol metabolism inhibits what 4 processes?
Glycolysis
TCA/Krebs cycle
Fatty acid oxidation
Gluconeogenesis
Alcohol metabolism favors what 3 things?
Lactate formation
Ketone synthesis
Lipogenesis
Clinical Outcomes of Altered Nutrient Metabolism
Ethanol Metabolism Summary: What two locations is ethanol metabolism?
Cytosol
Mitochondria
A 50-year-old female presents to the emergency department with confusion and
jaundice. She has a history of chronic alcohol use, consuming approximately 10 drinks
per day for the past 20 years. Laboratory tests show elevated liver enzymes, with an
AST/ALT ratio of 3:1. Which of the following statements best describes the metabolic
effects of her alcohol consumption?
A. Increases NADH levels which enhances gluconeogenesis leading to increased risk of
hypoglycemia.
B. Increases NAD+ levels resulting in lactic acidosis and ketogenesis.
C. Decreases NAD+ which Inhibits gluconeogenesis and increases acetyl CoA to
promote fatty acid synthesis.
D. Decreases NAD+ and acetyl CoA which increases gluconeogenesis and promotes the
synthesis of triglycerides.
E. Decreases NADH levels which inhibits gluconeogenesis and reduces TCA cycle
activity.
c
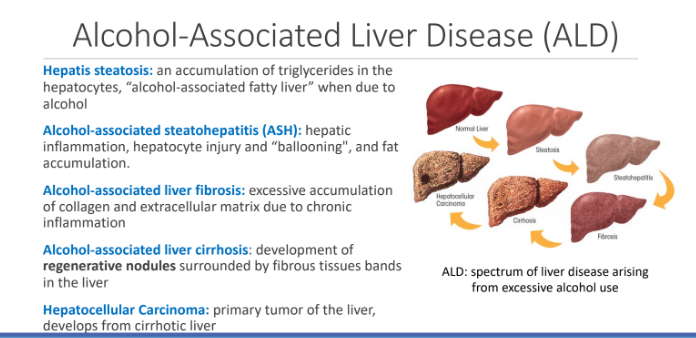
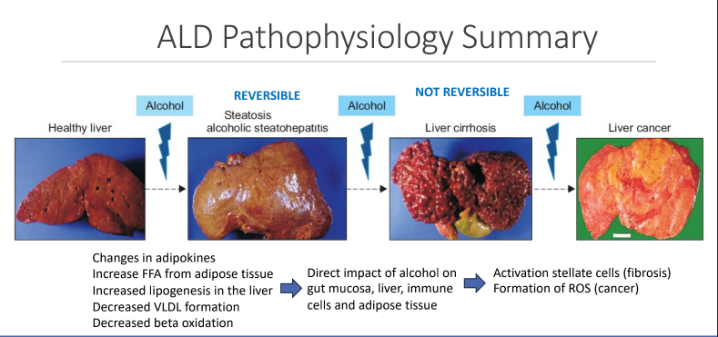
Alcohol-Associated Liver Disease (ALD): What is Hepatis steatosis?
an accumulation of triglycerides in the hepatocytes, “alcohol-associated fatty liver” when due to alcohol
What is Alcohol-associated steatohepatitis (ASH):?
hepatic inflammation, hepatocyte injury and “ballooning", and fat accumulation.
What is Alcohol-associated liver fibrosis?
excessive accumulation of collagen and extracellular matrix due to chronic inflammation
What is Alcohol-associated liver cirrhosis?
development of regenerative nodules surrounded by fibrous tissues bands in the liver
What is Hepatocellular Carcinoma?
primary tumor of the liver, develops from cirrhotic liver
ALD Pathogenesis
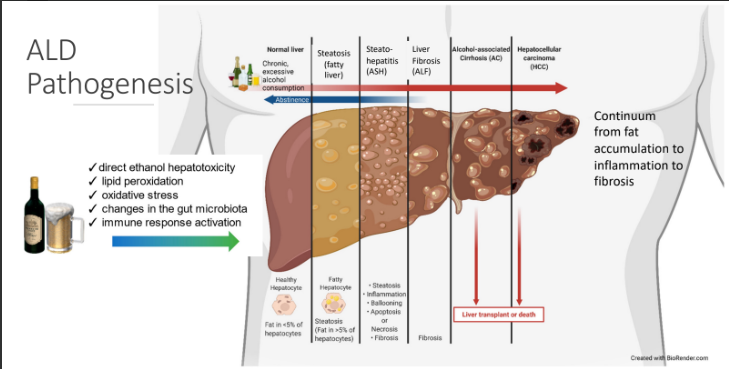
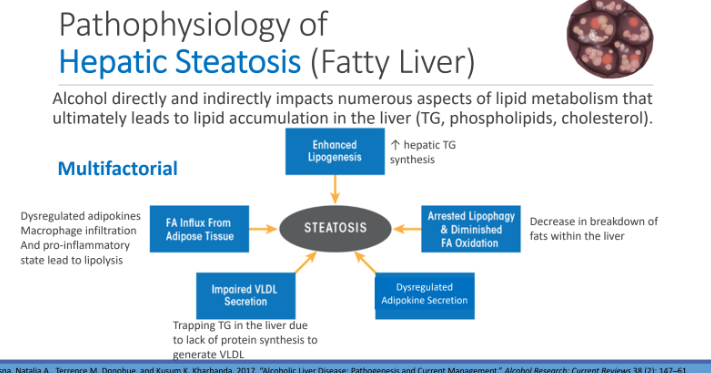
Pathophysiology of Hepatic Steatosis (Fatty Liver): Alcohol directly and indirectly impacts numerous aspects of lipid metabolism that ultimately leads to lipid accumulation in the liver (TG, phospholipids, cholesterol). What are 5 reasons?
Enhanced lipogenesis
FA influx from adipose tissue
Impaired VLDL secretion
Dysregulated adipokine secretion
Arrested lipophagy and diminished FA ox
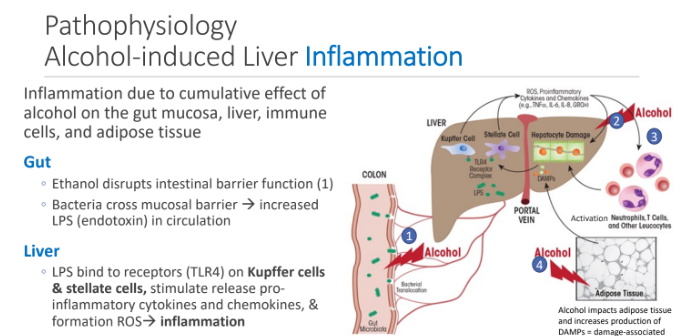
Inflammation due to cumulative effect of alcohol on the what 4 areas?
gut mucosa
liver
immune cells,
Adipose tissue
In the Gut: Ethanol disrupts ____ function; ____ cross mucosal barrier → increased____ in circulation
intestinal barrier; Bacteria; LPS (endotoxin)
Liver: LPS bind to receptors (TLR4) on Kupffer cells & stellate cells, stimulate what 2 things which lead to inflammation?
pro- inflammatory cytokines and chemokines,
formation ROS
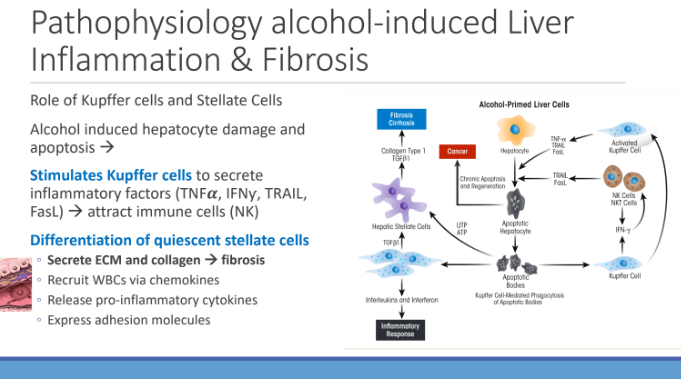
Alcohol induced hepatocyte damage and ____ which stimulates kupffer cells to secrete? to attract?
apoptosis ; inflammatory factors (TNFα, IFNƴ, TRAIL, FasL); immune cells (NK)
Alcohol induced hepatocyte damage and apoptosis leads to differentiation of?
quiescent stellate cells
Differentiation of quiescent stellate cells leads to what 4 things?
Secrete ECM and collagen → fibrosis
Recruit WBCs via chemokines
Release pro-inflammatory cytokines
Express adhesion molecules
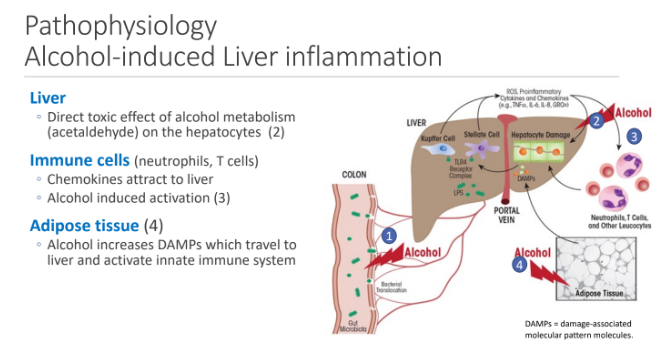
In the liver, there is a direct toxic effect of alcohol metabolism (acetaldehyde) on?
hepatocytes
How does alcohol contribute to liver inflammation through immune cells (neutrophils and, tcell)
Alcohol induced activation
Chemokines attract to liver
Adipose tissue: alcohol increases _____ which travel to liver and activate innate immune system
DAMPs
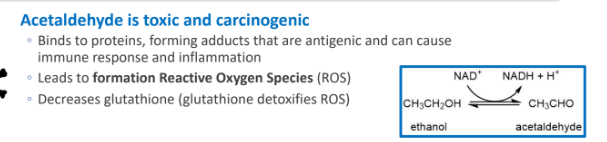
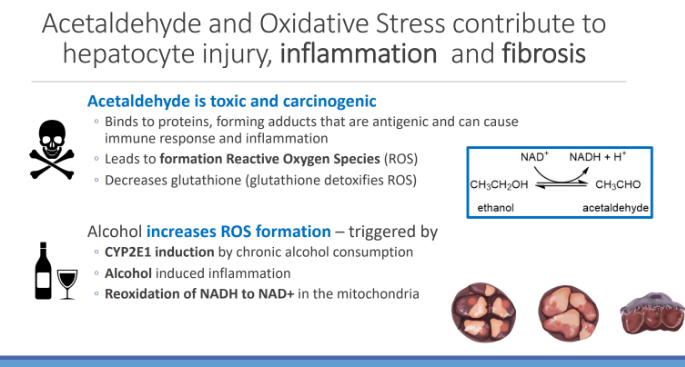
Acetaldehyde and Oxidative Stress contribute to hepatocyte injury, inflammation and fibrosis: Acetaldehyde is toxic and carcinogenic, it binds to ____ , forming adducts that are _____ and can cause immune response and inflammation; This leads to formation of ______; and decreases ____
proteins; antigenic; ROS; glutathione (which detoxifies ROS)
Alcohol increases ROS formation – triggered by what 3 things?
CYP2E1 induction by chronic alcohol consumption
Alcohol induced inflammation
Reoxidation of NADH to NAD+ in the mitochondria
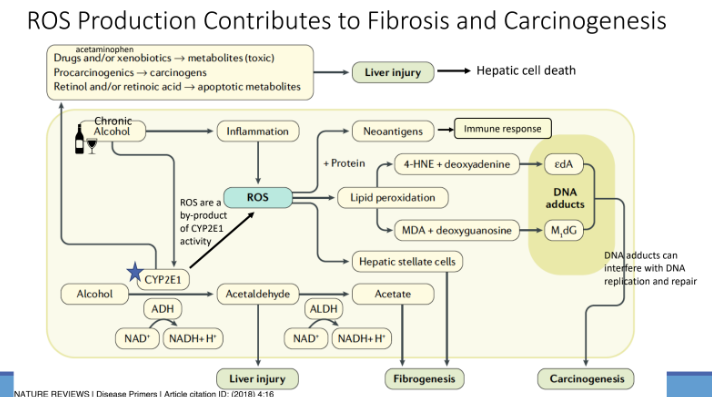
ROS Production Contributes to Fibrosis and Carcinogenesis
ALD Pathophysiology Summary
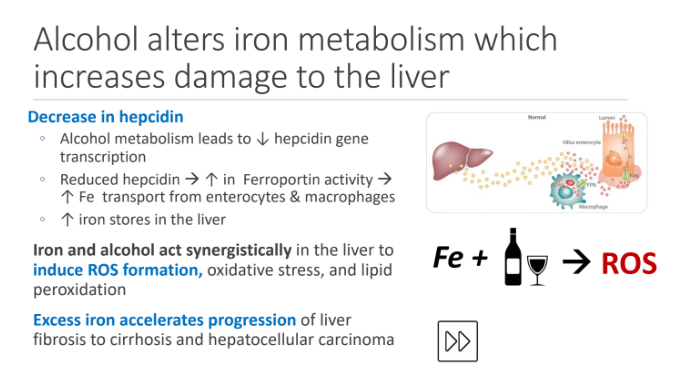
Alcohol alters iron metabolism which increases damage to the liver: Alcohol metabolism leads to ↓?
hepcidin gene transcription
Reduced hepcidin leads to an increase in?
This increases ____ transport from enterocytes & macrophages Which increases?
Ferroportin activity
Fe
iron stores in the liver
Iron and alcohol act synergistically in the liver to
induce what three things?
ROS formation
oxidative stress
lipid peroxidation
Excess iron accelerates progression of?
liver fibrosis to cirrhosis and hepatocellular carcinoma
Alcoholic steatosis (Fatty Liver) Can develop clinical symptoms/signs within ____ of heavy regular alcohol consumption (____ drinks per day for men and___ drinks per for women)
2 weeks; ≥ 5; ≥ 4
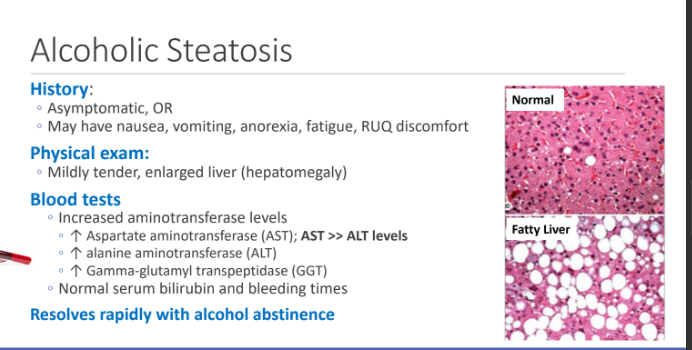
What are 4 ways to assess Alcoholic Steatosis?
History → asymptomatic or nausea, vom, anorexia, fatigue RUQ discomfort
Physical exam → Mildly tender, enlarged liver (hepatomegaly)
Blood Tests
Resolution rapidly with alcohol abstinence
What are 3 blood tests things that we look for since Increased aminotransferase levels
↑ Aspartate aminotransferase (AST); AST >> ALT levels
↑ alanine aminotransferase (ALT)
↑ Gamma-glutamyl transpeptidase (GGT)
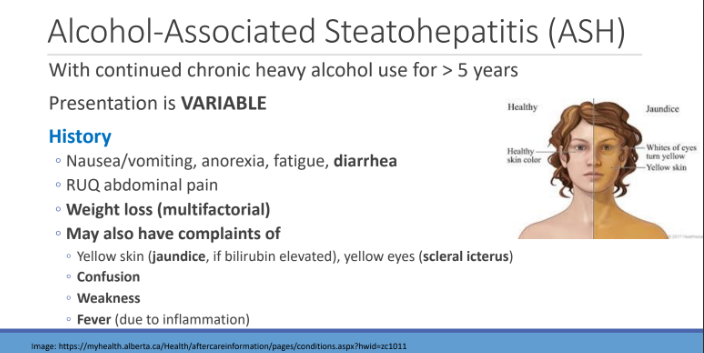
Alcohol-Associated Steatohepatitis (ASH): With continued chronic heavy alcohol use for > 5 years Presentation is VARIABLE. What are 4 things to look out for in history of ASH?
Nausea/vomiting, anorexia, fatigue, diarrhea
RUQ abdominal pain
Weight loss (multifactorial)
May also have complaints of
yellow skin (jaundice, if bilirubin elevated), yellow eyes (scleral icterus)
Confusion
Weakness
Fever (due to inflammation)
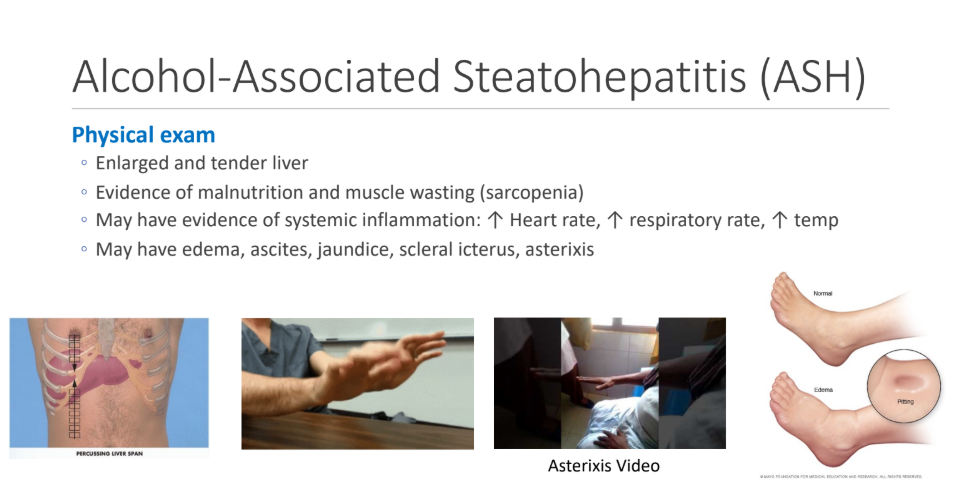
What are 4 things to look out for in Physical exam in Alcohol-Associated Steatohepatitis (ASH)?
Enlarged and tender liver
Evidence of malnutrition and muscle wasting (sarcopenia)
May have evidence of systemic inflammation: ↑ Heart rate, ↑ respiratory rate, ↑ temp
May have edema, ascites, jaundice, scleral icterus, asterixis
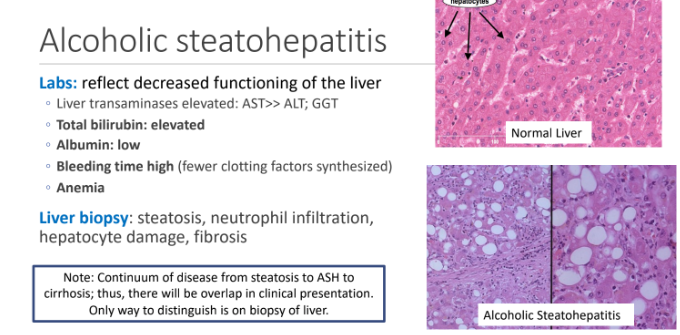
What are 5 labs of ASH (reflects decreased functioning of liver)
Liver transaminases elevated: AST>> ALT; GGT
Total bilirubin: elevated
Albumin: low
Bleeding time high (fewer clotting factors synthesized)
Anemia
What 4 things can a liver biopsy check for?
steatosis,
neutrophil infiltration,
hepatocyte damage,
fibrosis
Cirrhosis Signs and Symptoms: What 3 things can Hepatic Encephalopathy (HE) cause?
Impaired mentation: confusion, agitation, irritability, sleep disturbance, decreased attention
Neuromuscular disturbances: asterixis
Altered consciousness: lethargy, drowsiness, somnolence
What 3 things does a blood test show for Hepatic Encephalopathy (HE)?
↑ AST, ALT, GGT
↑Bilirubin
↓Albumin

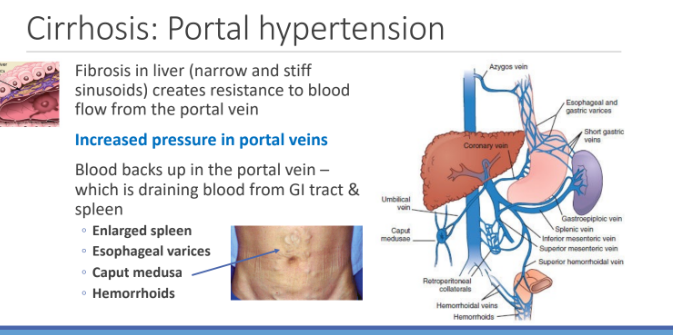
Cirrhosis: Portal hypertension: Fibrosis in liver (narrow and stiff sinusoids) creates ____ to blood flow from the ____; this causes increased ___ in portal veins
resistance; portal vein; pressure
Cirrhosis: Portal Hypertension: Blood backs up in the portal vein – which is draining blood from GI tract & spleen. This causes what 4 things?
Enlarged spleen
Esophageal varices
Caput medusa
Hemorrhoids
What is Cirrhosis: Ascites?
Abnormal accumulation of fluid in the peritoneal cavity
Portal hypertension causes an increase in hydrostatic pressure in portal veins, this decrease in oncotic pressure in vasculature due to decreased synthesis of albumin. Fluid moves from____ and liver into the _____ ; Ascites can become infected and cause_____ (fatal without treatment)
vasculature; peritoneal cavity; spontaneous bacterial peritonitis
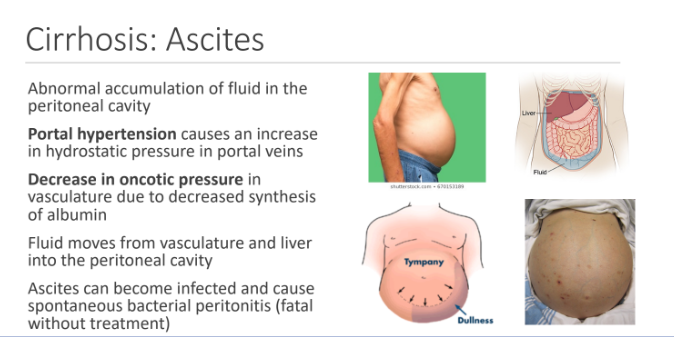
What are 3 Ascites management ways?
1. Low sodium diet
Diuretics: to increase excretion of sodium and water by the kidney
Paracentesis: procedure to withdraw fluid from the peritoneal cavity
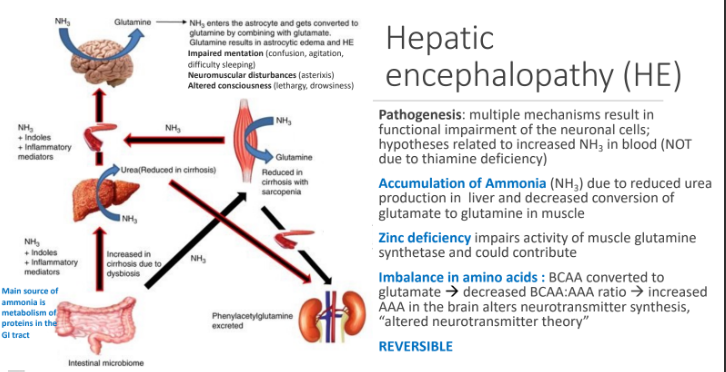
Hepatic encephalopathy (HE) Pathogenesis: multiple mechanisms result in functional impairment of the neuronal cells; hypotheses related to increased NH3 in blood (NOT due to thiamine deficiency). What are 3 contributors to HE?
Accumulation of Ammonia (NH3) → reduced urea production in liver and decreased conversion of glutamate to glutamine in muscle
Zinc deficiency → impairs activity of muscle glutamine synthetase and could contribute
Imbalance in amino acids → : BCAA converted to glutamate → decreased BCAA:AAA ratio → increased AAA in the brain alters neurotransmitter synthesis, “altered neurotransmitter theory”
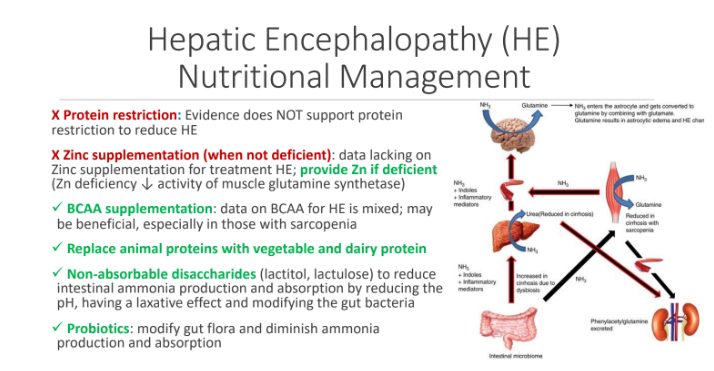
Hepatic Encephalopathy (HE) Nutritional Management: What 2 things should we NOT do?
X Protein restriction: Evidence does NOT support protein restriction to reduce HE
X Zinc supplementation (when not deficient): data lacking on Zinc supplementation for treatment HE; provide Zn if deficient (Zn deficiency ↓ activity of muscle glutamine synthetase)
Hepatic Encephalopathy (HE) Nutritional Management: What 4 things should we do?
BCAA supplementation: data on BCAA for HE is mixed; may be beneficial, especially in those with sarcopenia
Replace animal proteins with vegetable and dairy protein
Non-absorbable disaccharides (lactitol, lactulose) to reduce intestinal ammonia production and absorption by reducing the pH, having a laxative effect and modifying the gut bacteria
Probiotics: modify gut flora and diminish ammonia
production and absorption
Malnutrition in cirrhosis associated with increased (4 answers)?
Susceptibility to infections
Hepatic encephalopathy
Ascites
And lower survival
Etiology of Malnutrition in ALD
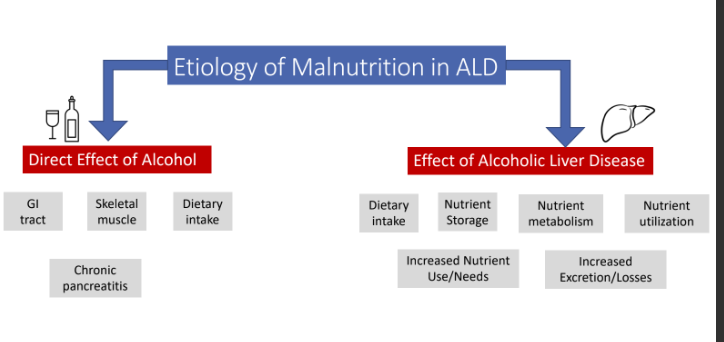
What is the Direct effect of alcohol on GI tract?
◦ Inflammation of mucosa (gastritis)
Direct effect of alcohol on GI tract: Mucosal erosions and fibrous tissue accumulation leads to Reduced?
digestion and absorption
Inflammation of mucosa (gastritis) by alcohol also leads to _____ overgrowth and _____; there is also increase _____ permeability
bacterial;dysbiosis; intestinal