Therapeutics II: Exam 1 - Drug Induced Diseases RW
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
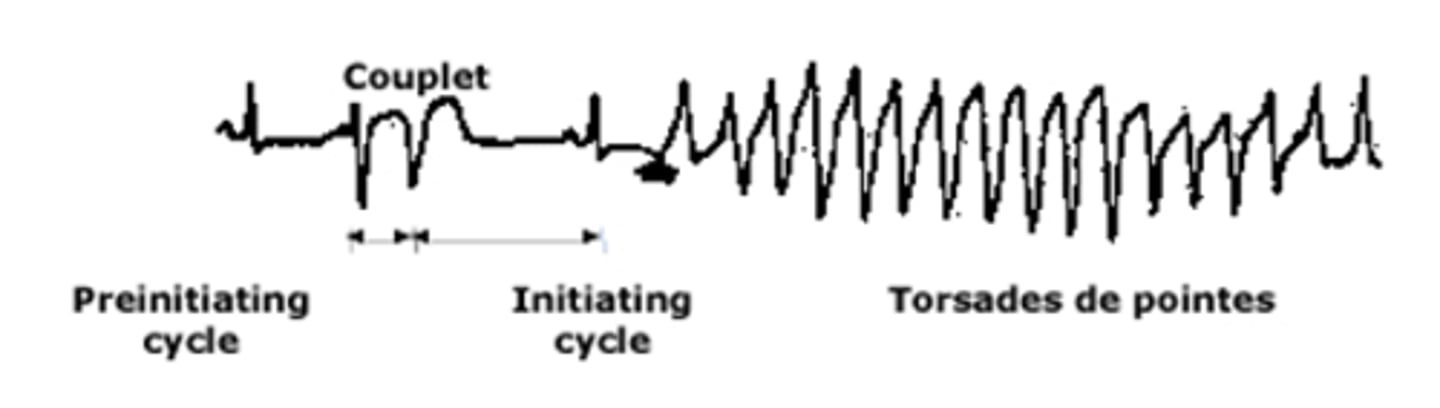
What is torsades de pointes (TdP)
Polymorphic ventricular tachycardia
Atypical, rapid and bizzare
Associated with QT prolongation
How is TdP characterized on an EKG?
Characterized by continuously changing axis of polymorphic QRS morphologies
A short, preinitiating RR interval, due to a ventricular couplet
Followed by a long, initiating cycle, due to compensatory pause after the couplet
What QTc interval is considered a concern for TdP?
QTc’s >500 msec are a concern for TdP
What QTc interval is considered prolonged in men?
>450 msec
What QTc interval is considered prolonged in women?
>470 msec
What factors should be considered when assessing risk of TdP?
Patient and drug risk factors
Rarely occurs without multiple risk factors
What conditions predispose patients to TdP?
Age >65
HF
Electrolyte Abnormalities - Hypokalemia or Hypomagnesemia
Female Gender
What drug regimens are a risk factor for TdP?
Drugs that inc. QTc 60 msec from baseline
Drugs that prolong QTc administered IV with a rapid infusion rate
High drug doses/conc.'s (except Quinidine)
Chronic hepatic or renal insufficiency
Combined use of drugs that prolong QT or slow metabolism
Which drug classes are high risk for QT prolongation and TdP?
Cardiac drugs
Antidepressants
Antipsychotics
Antihistamines
Antimicrobials
Which cardiac drugs are associated with QT prolongation?
Amiodarone
Sotalol
Disopyramide
Dofetilide
Procainamide
Quinidine
Which antidepressants are associated with QT prolongation?
SSRIs (citalopram, escitalopram, fluoxetine)
Moclobemide
TCAs
Lithium
Which antipsychotics are associated with QT prolongation?
Amisulpride
Chlorpromazine
Haloperidol
Ziprasidone
Thioridazine
Which antihistamines are associated with QT prolongation?
Loratadine
Astemizole
Diphenhydramine
Which antimicrobials are associated with QT prolongation?
Ciprofloxacin, moxifloxacin, sparfloxacin
Clarithromycin, erythromycin
Fluconazole, voriconazole
Pentamidine
How should risk of TdP be managed in the outpatient setting?
Avoid use of >2 known/possible drugs in pt.'s with hx. of TdP or long QT syndrome
In pt.'s with other risk factors avoid combo of 2 known (or 1 known and 1 possible) QT prolonging drugs
How should risk of TdP be managed in the inpatient setting?
Same as outpatient but also wath electrolytes closely
Consider EKG - if >500 try to avoid all known/possible
What dangerous complications can TdP lead to?
Ventricular fibrillation
Cardiac arrest
Sudden cardiac death
What are non-pharm management options for TdP?
Temporary pacing (atrial or ventricular)
What are pharmacologic management options for TdP?
Magnesium sulfate (1st line)
Isoproterenol
Sodium bicarbonate (for quinidine-mediated arrhythmias)
What are the benefits of magnesium sulfate for treatment of TdP?
Effective for both treatment and prevention of LQT-related ventricular ectopic beats or TdP
Benefit occurs without QT shortening
Benefit occurs in pt.'s with normal serum Mg at baseline
When should sodium bicarbonate be used to treat TdP?
For quinidine-mediated arrhythmias
What is Heparin-Induced Thrombocytopenia (HIT)?
Immune complication of heparin therapy
Paradoxical thrombocytopenia leading to thrombosis
What is the pathophysiology of HIT?
PF-4 binds to surface of platelet
Complexes of heparin and PF-4 form
IgG binds to the PF-4/Heparin complex
IgG/PF-4/Heparin complex activates via the Fc receptor
Fc stimulation leads to generation of pro-coagulant rich microparticles
Why is HIT difficult to correctly diagnose in hospitalized patients?
Hospitalized patients have multiple possible reasons for developing thrombocytopenia
What is the 4T's score used for?
Identify patients at risk for HIT
What are the 4 patient parameters included in the 4T score?
Magnitude of platelet drop
Timing of thrombocytopenia
Presence of new thrombosis
Other possible reasons for thrombocytopenia
Is the 4T score useful for both ruling in and out a diagnosis of HIT?
High negative predictive value - low value rules out HIT
But, high score not always a strong predictor of HIT
What 4T score indicates low risk of HIT?
≤3 is low risk
What 4T score indicates intermediate risk of HIT?
4-5 is intermediate risk
What 4T score indicates high risk of HIT?
≥6 is high risk
What is the typical onset of HIT?
5-10 days after starting heparin
(unless previously exposed)
When does HIT have a rapid onset (<1 day)?
If recently exposed to heparin
Have residual circulating HIT antibodies
What platelet count nadir is seen in most patients with HIT?
<150,000/uL (85%)
(<20,000 seen in 10%)
What is a common complication of HIT?
New thrombosis (in 50%)
What type of venous thrombosis' can occur with HIT, in order from most to least common?
DVT >
PE >
Warfarin-induced limb gangrene >
Adrenal hemorrhagic necrosis >
Cerebral sinus thrombosis
What type of arterial thrombosis' can occur with HIT, in order from most to least common?
Limb artery thrombosis >
Stroke syndrome >
MI >
Mesenteric artery thrombosis
What symptoms can be see in HIT patients due to acute platelet count fall?
Acute inflammatory or cardiorespiratory s/s
What laboratory testing is performed for HIT?
Heparin-dependent platelet activation
Immunoassay (heparin/PF4 antigen)
How is Quinine-/Sulfa-Induced thrombocytopenia differentiated from HIT, in terms of onset?
≥7 days for Quinine-/Sulfa-Induced
(5-10 for HIT)
How is Quinine-/Sulfa-Induced thrombocytopenia differentiated from HIT, in terms of platelet count?
<20,000 uL for Quinine-/Sulfa-Induced
(20,000-150,000 for HIT)
How is Quinine-/Sulfa-Induced thrombocytopenia differentiated from HIT, in terms of complications?
Bleeding seen with Quinine-/Sulfa-Induced
(thrombosis seen with HIT)
How is Quinine-/Sulfa-Induced thrombocytopenia differentiated from HIT, in terms of lab testing?
Drug-dependent increase in platelet-associated IgG for Quinine-/Sulfa-Induced
If HIT is suspected, what should be done first?
Calculate 4T score to determine probability
If a patient has intermediate or high risk of HIT, what should be done?
1. D/C Heparin
2. Start non-heparin anticoagulation
3. Perform ELA
If a patient has intermediate or high risk of HIT, and their ELA returns positive, what should be done?
Obtain functional assay
If positive - continue with management
If negative - resume heparin
If a patient has intermediate or high risk of HIT, and their ELA returns negative, what should be done?
Resume heparin
If a patient has low risk of HIT, what should be done?
Continue heparin
What should always be done before antibody testing in suspected HIT?
4T score
(Ab test has a 20% false positive rate - leads to overdiagnosis)
What is the use of the SRA test in HIT managment?
Will confirm diagnosis
But, takes several days to do
If a patient has a 4T score of 1-4 what should be done?
Continue heparin and monitor platelets
If a patient has a 4T score of 4-5 what should be done?
Stop or change anticoags, and check Ab
If a patient has a 4T score of 7-8 what should be done?
Change to Argatroban/fondaparinux and check HIT Ab
Once a patient has HIT with thrombosis, how long should they be anticoagulated for?
3 months
With Warfarin or DOAC (preferred)
What are alternative anticoagulant options for patients with HIT?
Danaparoid
Argatroban
Bivalirudin
Fondaparinux
What is the interstitium?
Fabric of connective tissue that supports its many structures
Expands and contracts with ventilation
Surrounds the air spaces, brings blood in close proximity to air with separation but minimal impedance to diffusion
Serves as a conduit and fluid channel for lymphatic drainage and the migration of immune cells
Collects and sequesters a fraction of insoluble particles that deposit in the lung
What are the main functions of the interstitium?
Allows for efficient gas exchange
Allows for lymphatic drainage
What are the 2 categories of interstitial disease?
Acute
Chronic
What is acute interstitial disease?
Edema
Infection
Inflammation
(pulmonary edema and exacerbated HF)
What is chronic interstitial disease?
Fibrosis, end stage of inflammation
Often involves bronchiolitis
(inflammation of bronchioles, inc. risk of infection)
What are the operational classifications of interstitial disease?
Pneumoconiosis
Granulomatous disease
Hypersensitivity pneumonitis
Diffuse interstitial fibrosis
What are types of Diffuse interstitial fibrosis?
Idiopathic pulmonary fibrosis (= "usual interstitial pneumonia")
Giant cell interstitial pneumonia ("GIP")
Other interstitial pneumonias
What type of interstitial disease is most commonly caused by drugs?
Hypersensitivity pneumonitis
A type of allergic reaction that causes swelling of Interstitium or parenchyma
If not treated becomes diffuse interstitial fibrosis (commonly idiopathic)
What are methods of diagnosis of interstitial disease?
CT scan
Pulmonary function tests (PFTs)
Biopsy
Look for eosinophils in blood (and in biopsy)
What test is most commonly used for diagnosis of interstitial disease?
Chest film
Why is are eosinophils in blood used for diagnosis of interstitial disease?
Eosinophilia seen commonly with drug induced ILD
Eosinophils are the immune cells primarily responsible for drug allergy
If pt has symptoms and eosinophils in blood - lean towards hypersensitivity pneumonitis
What groups are at a high risk for interstitial disease?
Demographics, family history (some IPF)
Occupational history
Drugs notorious for causing ILD
(Exceptions: sarcoid, IPF)
What is a characteristic of pulmonary function tests in interstitial disease?
Restrictive pattern on PFTs
Reduced FVC, preserved FEV1, decreased RV
Only occurs late in course of disease
What symptoms are seen with interstitial disease?
All non-specific
Dyspnea on exertion
Cough
Fatigue
What are the two types of interstitial disease drugs cause?
Interstitial pneumonia or fibrosis (IPF)
Pulmonary infiltrate with eosinophilia
What drugs cause interstitial pneumonia or fibrosis (IPF)?
Bleomycin (causes both types)
Cocaine
Methotrexate
What drugs cause pulmonary infiltrate with eosinophilia?
Amiodarone
Bleomycin (causes both types)
Nitrofurantoin
What increases the risk of interstitial disease with Nitrofurantoin?
Use for long-term suppressive therapy
What is the onset of Type 1 Amiodarone-induced interstitial disease?
Rapid - 1-3 months after initiation
What are characteristics of Type 1 Amiodarone-induced interstitial disease?
Mild pneumonitis
Resolve on it's own!
What is the onset of Type 2 Amiodarone-induced interstitial disease?
Slow - occurs after years
What are characteristics of Type 2 Amiodarone-induced interstitial disease?
Risk based on total dose given
High mortality rate
Symptoms don't resolve
Periodic CXR considered in pt.'s on long-term amiodarone
How is interstitial disease treated?
Stop offending agent if possible
Steroids - often at high doses for long periods
Steroid sparing agents - little/no data
(Mycophenolate, AZA, NAC)