IMED1004 - Alcohol (L22)
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
Alcohol and ethanol are interchangable in this lecture
good
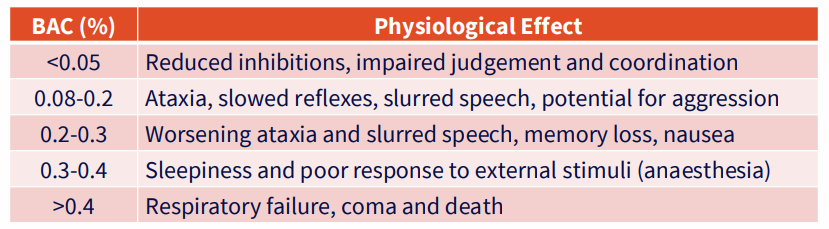
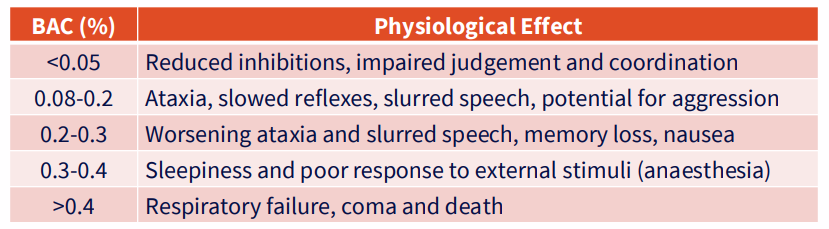
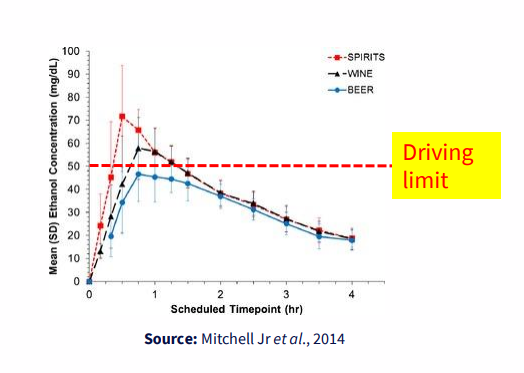
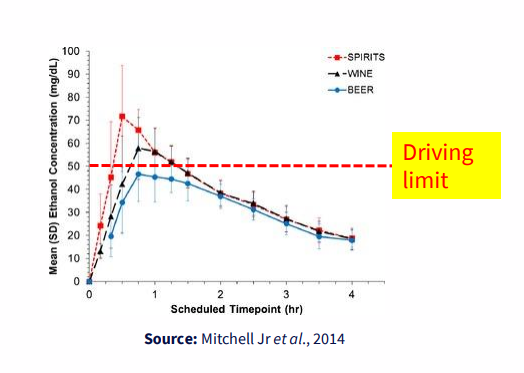
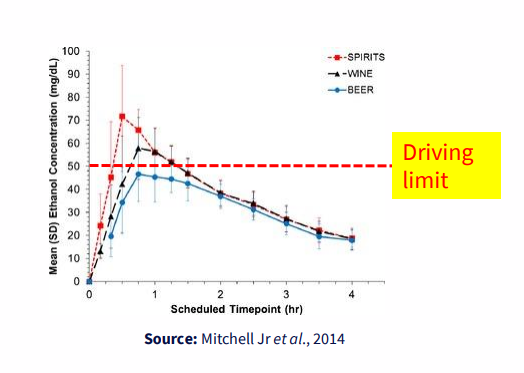
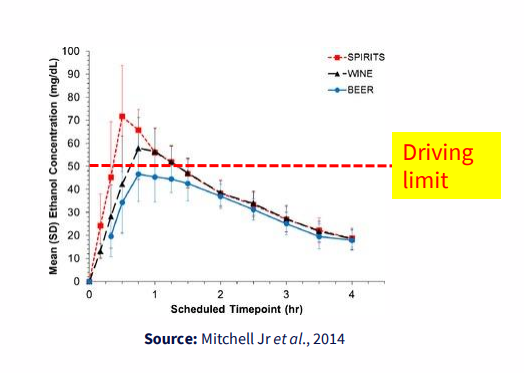
Ethanol Blood Alcohol Concentration
- blood alcohol concentration (BAC) is a measure of the amount of ethanol in the blood
- units: g/100mL or %
- Legal driving limit is <0.05% or 0.05g per 100mL blood
- Alcohol concentration in breath is proportional to its concentration in blood
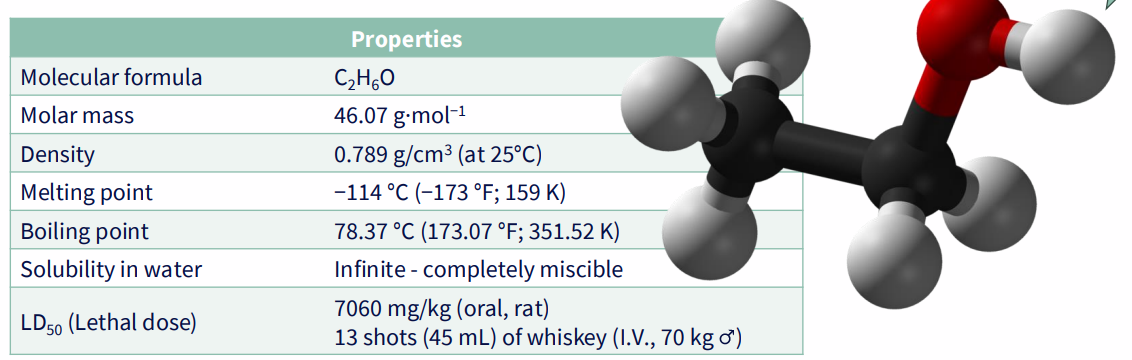
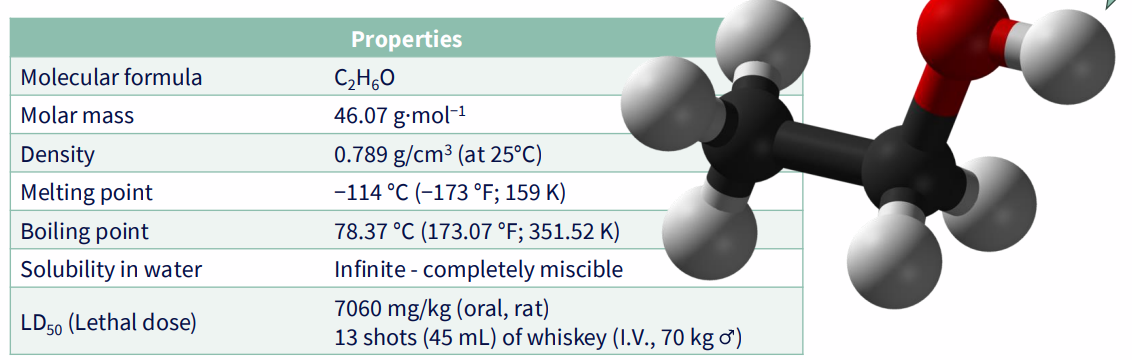
Ethanol: Chemical Properties (NO LEARNING OUTCOME)
- completely miscible in water
- basically it can easily pass lipid membranes becuase it has a hydrophobic and hydrophillic part
Physiology
IN:
- consumption (distributed throughout tissues and fluids)
- production (rare, auto-brewery syndrome, gut fermentation of sugars to alcohol)
.
OUT:
- <10% is directly excreted (breath, sweat, urine, tears)
- >90% is metabolised (liver)
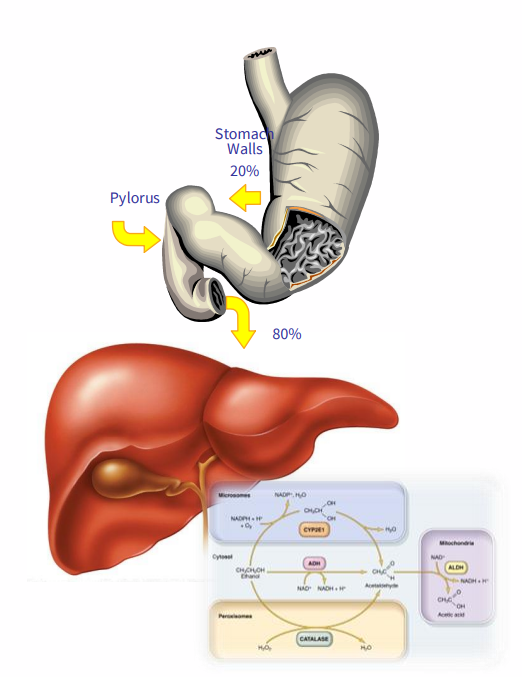
Absorption - Factors affecting diffusion
CONCENTRATION GRADIENT:
- stronger drinks = faster uptake
.
PERMEABILITY:
- water soluble + lipophillic - easily crosses membranes, goes everywhere!
.
SURFACE AREA:
- intestine (200m^2) versus stomach (0.053m^2)
- rate of absorption is greater in the intestine
Never drink on an empty stomach
- food delays gastric emptying to the small intestine
- ethanol remains in the stomach longer
- ethanol is absorbed at a slower rate in the stomach compared with the intestine
- effects on the brain are less acute/significant
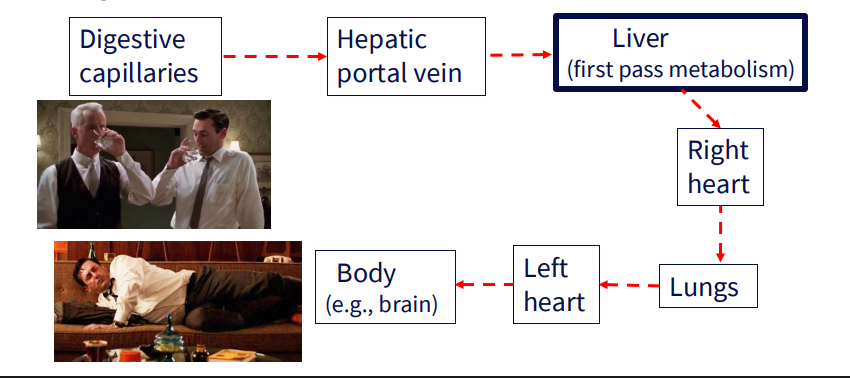
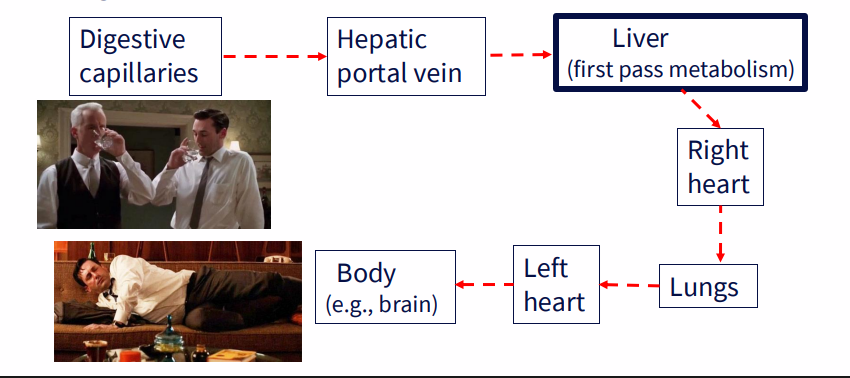
Transport of Alcohol
- transports freely in blood, easily crosses membranes
- EtOH follows water (blood, brain, liver, muscle)
- the average male is 68% water
- the average female is only 55% water
.
- digestive capillaries -> hepatic portal vein -> liver (first pass metabolism) -> right heart -> lungs -> left heart -> body (e.g brain)
Ethanol Excretion (non-metabolic)
- <10% is removed in bodily fluid (urine, breath, sweat)
- concentration of ethanol in the blood is the same as in the urine (as ethanol is excreted in urine, we get less good at excreting ethanol in urine)
- if excretion in urine was the only mechanism of removing ethanol from the bloodstream, it would take several days to clear one standard drink (cannot rely on our kidneys to clear our blood of ethanol, thats why we need to metabolise it)
- alcohol increases urine production through inhibition of anti-diuretic hormone (vasopressin)
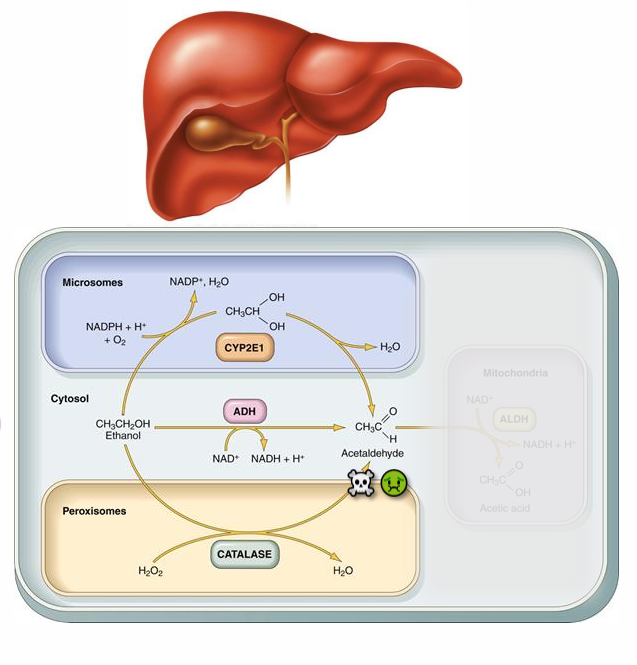
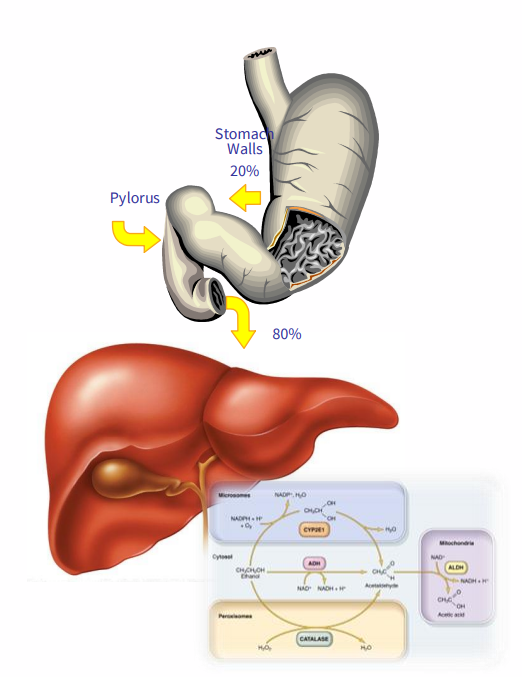
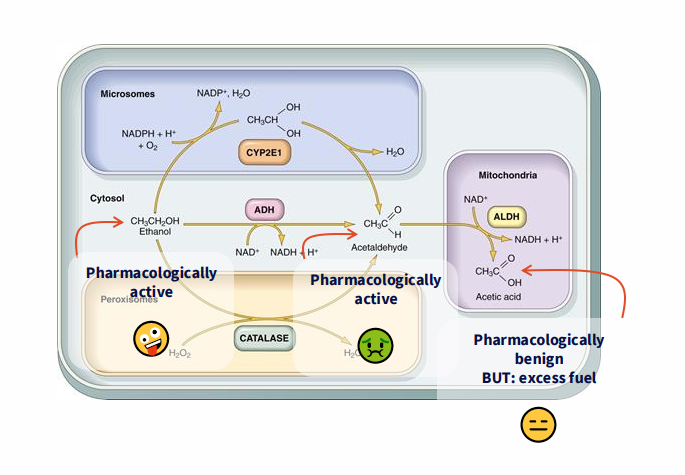
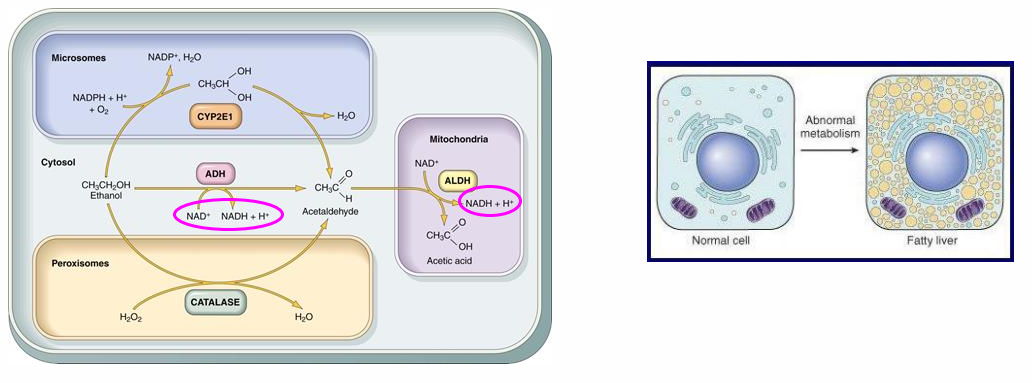
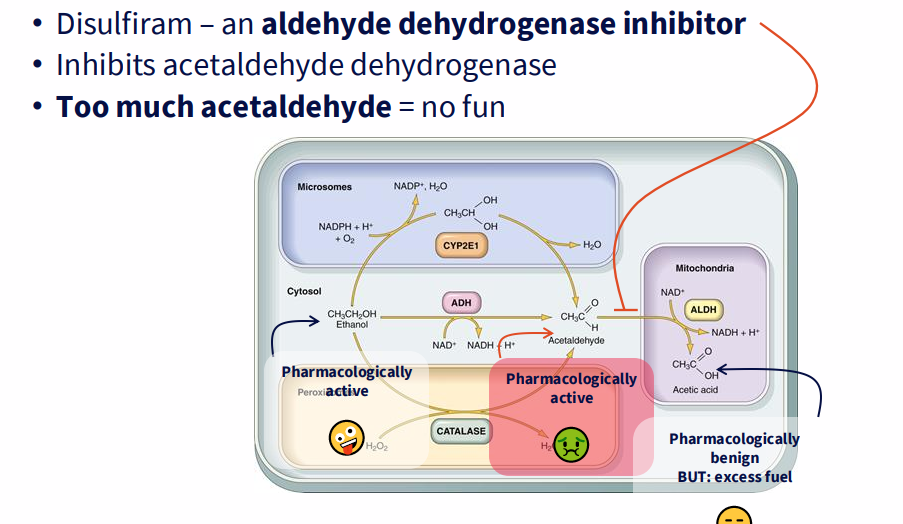
Metabolism (Step 1)
- EtOH -> acetylaldehyde -> acetate (occurs in hepatocytes of the liver)
.
STEP 1: EtOH to acetylaldehyde
- MODERATE: cytochrome P450 (CYP2E1)
- MAJOR (90%) - alcohol dehydrogenase (ADH)
- MINOR - catalase
.
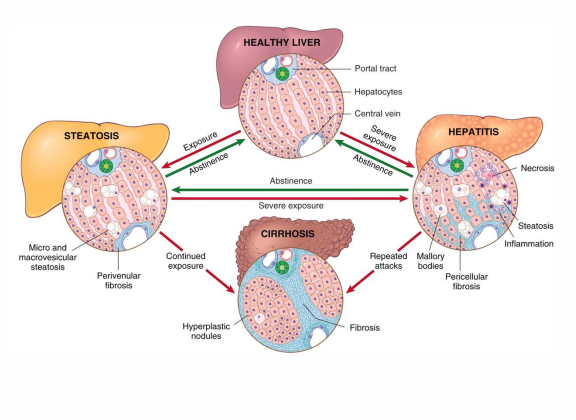
Acetaldehyde is highly toxic, and causes liver damage (cirrhosis)
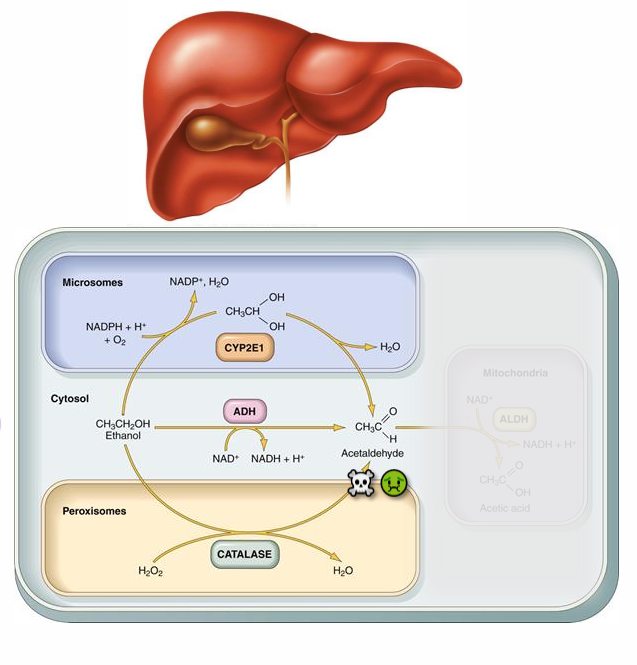
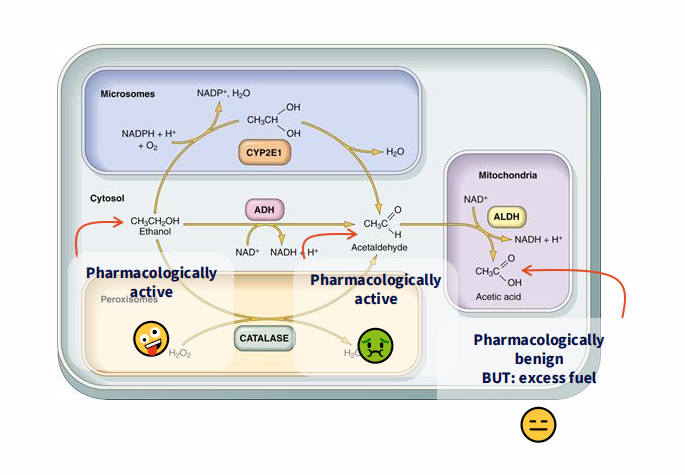
STEP 2 METABOLISM
STEP 2: Acetaldehyde -> acetate
- acetaldehyde dehydrogenase (ALDH)
- aka aldehyde dehydrogenase
.
- ALDH is subject to product (NADH) inhibition
- Acetaldehyde to acetate is rate limiting step in alcohol metabolism
- fixed rate: 7g per hour
- the average persons BAC drops by around 0.015% per hour
.
- dont need to know reaction of the microsome or the peroxazome byt you need to remember the reaction thats happening in the cytosol and mitochondria because that two-step reaction, the metabolism of alcohol, is essential fro understanding
.
- rate limiting step is acetaldehyde to acetate
- you can see whcih one makes you feel drunk and whcih one makes you feel gross based on the diagrams
- if u drink a lot the rate limitng step is saturated which means that acetaldehyde builds up, hence u start to feel sick
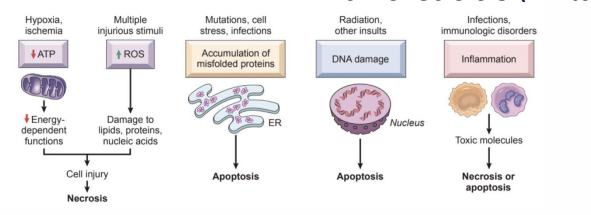
Acute and Chronic Alcohol Injury
ACUTE:
- CNS depressant
- Reversible hepatic and gastric injuries
.
CHRONIC:
- damage to the liver, GI tract, CNS, cardiovascular system, and pancreas
- Carcinogen
- Fetal Alcohol Syndrome
- Malnutrition
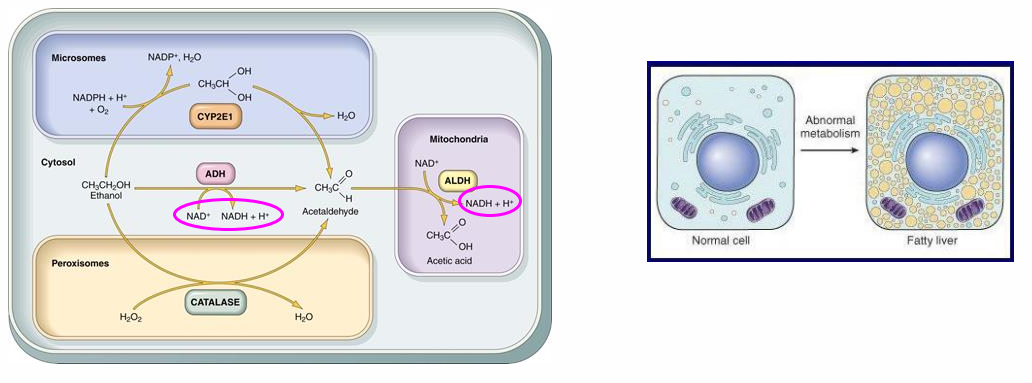
Toxic Effects of Ethanol Metabolism
- all pathways result in an increased NADH/NAD ratio
- decreased fatty acid oxidation -> fatty liver (steatosis) --> hepatitis
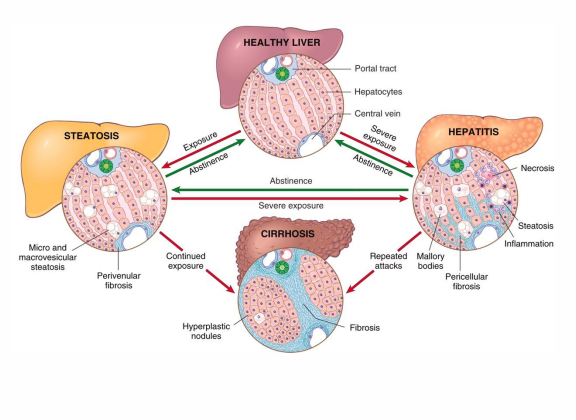
Alcohol-Related Liver Disease
- Excessive ethanol consumption causes more than 60% of cases of chronic liver disease in Western countries and accounts for 40% to 50% of deaths resulting from cirrhosis
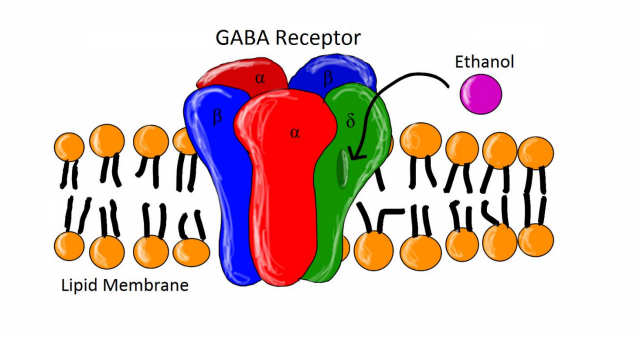
Targets
- primary targets of EtOH are usually membrane-bound receptors (perturbs signalling)
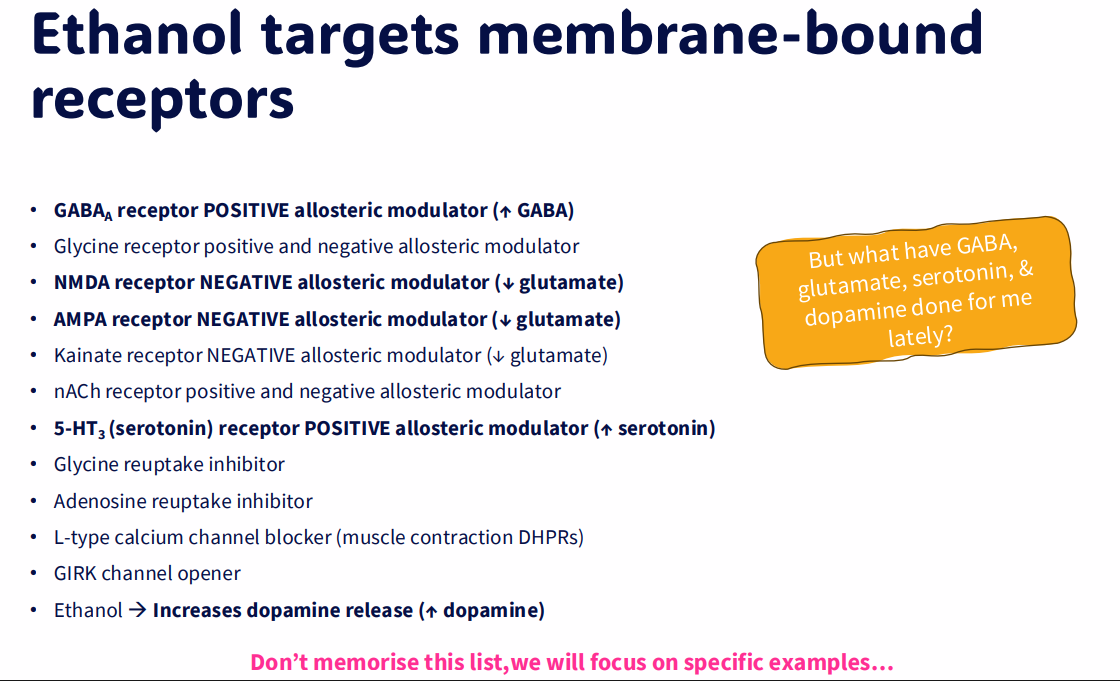
Ethanol targets membrane-bound receptors
- dont need to memoriuse the slide, we will go throiuygh specific examples
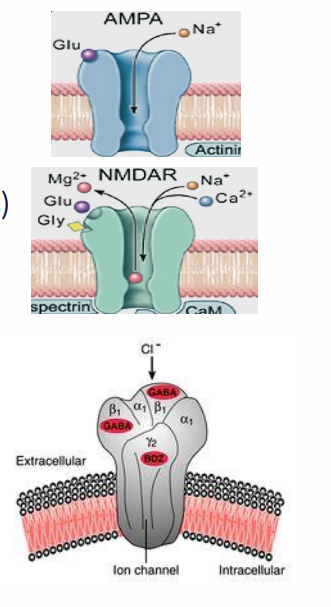
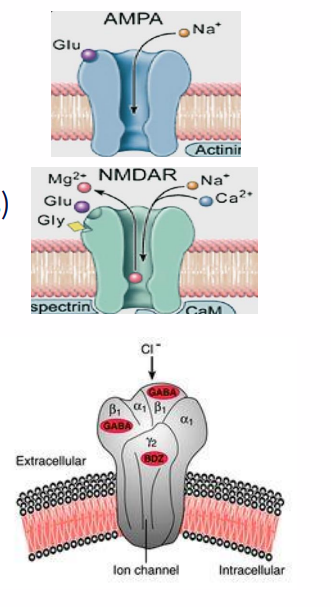
Neurotransmitter functions: GABA and Glutamate
GLUTAMATE:
- the dominant excitatory CNS neurotransmitter
- binds/opens iGluRs (ionotropic glutamate receptors)
- AMPA receptor is an Na+ channel (EPSP)
- NMDA receptor is a Na+ and Ca2+ channel (EPSP)
- Also mGluRs (metabotropic glutamate receptors)
.
GABA (gamma-aminobutyric acid)
- the dominant inhibitory CNS neurotransmitter
- binds/opens GABA(A)Rs: Cl- channels
- Cl- influx causing hyperpolarisation
- Inhibits post-synaptic neuron (IPSP)
- Also GABA(B)Rs (metabotropic)
.
- main role of alcohol is that its a depressant
- affects amount of glutamate and GABA (supposedly)
Your brain relaxes and things slow down
Stimulates GABA, inhibits glutamate
- EtOH activates GABA(A)R -> increased GABA (inhibitory)
- depresses brain activity (relaxation, loss of inhibitions)
- inhibits motor outputs and sensory outputs
.
GABA inhbits glutamate
- 'Normal' thinking depends on the balance of excitatory glutamate and inhibitory GABA
- imbalance -> impaired cognition
It gives you 2 things you really enjoy
DOPAMINE: main focus/desire neurotransmitter
- Responsible for our drive or desire to acquire (food, sex, an achievement, drug)
- it tends to make people more talkative and excitable, and often leaves them wanting more
.
SEROTONIN: main well-being/satisfaction neurotransmitter
- It allows us to be content and happy
- keeps our moods under control by helping with sleep, calming anxiety, and relieving depression
So stimulating serotonin and dopamine is all good, right?
stimulates serotonin and dopamine makes you happy (reward)
- serotonin - happy, safe, relaxed, euphoric
- rising dopamine = reward, pleasure
.
but... they dont stay up forever
- Taking away your reward -> addiction
- falling serotonin = anxious, depressed
- falling dopamine = craving/dependence/seeking behaviour
.
- basically the effects of alcohol are short term. once u take away the reward it goes bad
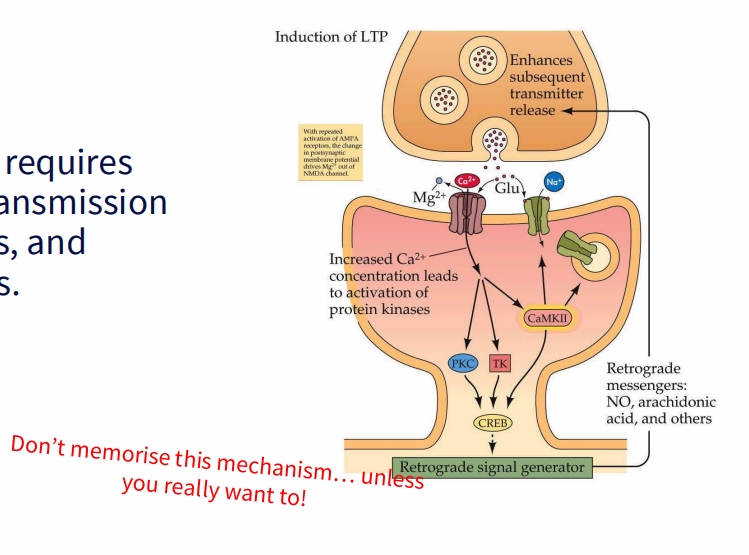
Glutamate Signalling is essential for memory storage
- Memory formation requires glutamate neurotransmission via NMDA receptors and alcohol inhibits this
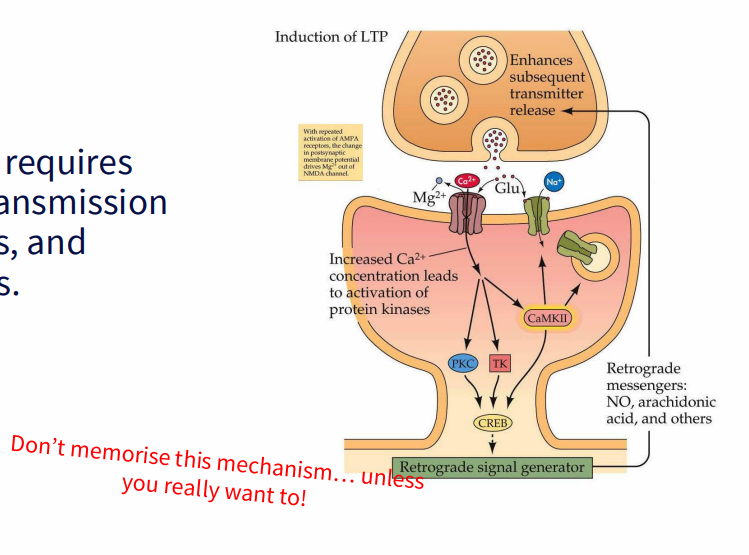
So, guess what happens if you inhibit glutamate signalling via NMDA + AMPA?
INHIBITS MEMORY FORMATION:
- At BAC of 0.2%, LTP is reduced 80%
- increase BAC -> blackouts
.
people black out while drinking because memory formation is inhibited
Long-term neurotoxicity
- brain shrinks (atrophy)
- alcoholic dementia (10% of dementia cases, pre-frontal cortex is particularly susceptible. affect memory, learning, reasoning and other mental functions, as well as personality, mood and social skills
Cancer
ALCOHOL IS CLASSIFIED AS GROUP 1 CARCINOGEN:
- the highest level of certainty, like for tobacco smoke and asbestos
.
STRONG EVIDENCE THAT ALCOHOL CAUSES CANCER OF:
- Pharynx + Larynx
- oesophagus
- liver
- bowel + stomach
- breast
.
- the risk of alcohol-caused cancer at these increases with the amount of alcohol consumed
Pathophysiology: Cancer
Acetaldehyde damages DNA
- for cancers of the mouth, pharnyx, larynx, oesophagus and liver there is strong evidence that the DNA damage is due to acetaldehyde
- alcohol can also cause direct tissue damage
.
- it increases risk of liver cancer by causing cirrhosis
.
- alcohol can influence hormone levels, increasing cancer risk of hormone-dependent cancers (for breast cancer, alcohol interferes with oestrogen and encourages cell division)
Long-term neurotoxicity disease names
WERNICKE'S ENCEPHALOPATHY:
- interferes with vitamin B1 (thiamine) absorption + distribution (+ poor diet), thus energy metabolism in neurons
- causes confusion, personality changes
- Cerebellum susceptible = ataxia
- Eye movement, vision, balance, coordination (staggering)
.
KORSAKOFF'S SYNDROME: (VERY BAD WERNICKE'S)
- inability to form new memories or learn new information
- making up stories to fill gaps in memory (confabulation)
- seeing or hearing things that aren't really there (hallucinations)
- combined with a lack of insight into the condition
Effects of Vasculature
EtOH causes vasodilation:
- increases vasodilator, nitric oxide (NO)
- skin flushing
.
Lowers resting blood pressure:
- your body homeostatically increases your heart rate to compensate
- resting tachycardia
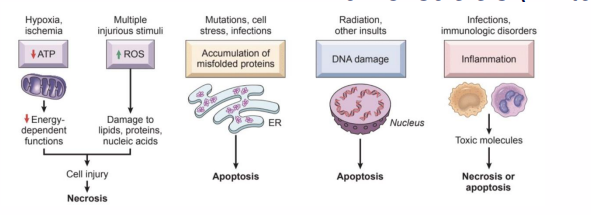
Ethanol is pro-inflammatory
- Oxidative stress -> damage
- Acetaldehyde (stimulates prostaglandin and histamine release - inflammatory response)
- causes cells + tissues to become inflamed + leaky
- reversible
.
- inflammation (direct from ethanol or indirect from prostaglandins and histamine)
- gastritis (inflamed stomach)
- enteritis (inflamed intestines)
- pancreatitis (inflamed pancreas)
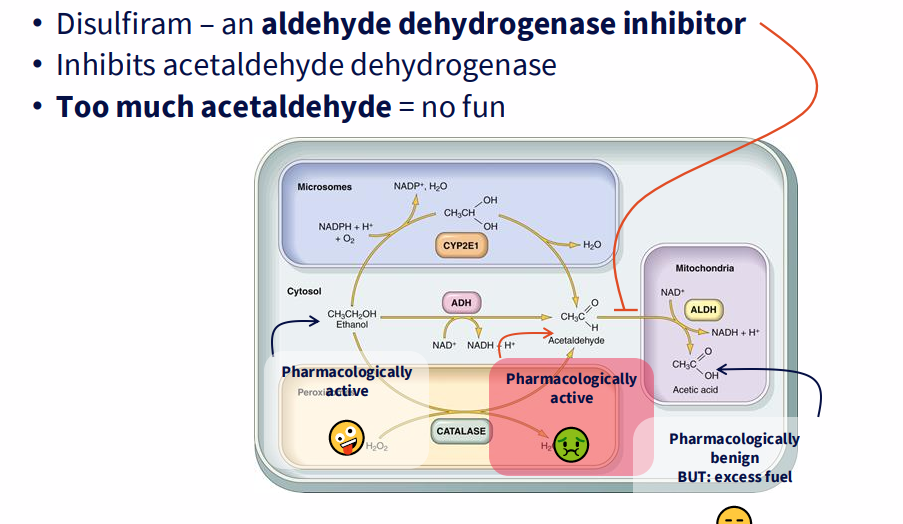
Treating alcohol use disorder - take the fun away
- disulfiram - an aldehyde dehydrogenase inhibitor
- inhibits acetaldehyde dehydrogenase
- too much acetaldehyde = no fun
.
- basically it makes it really not fun to drink alcohol as the final step where acetaldehyde is converted doesnt happen
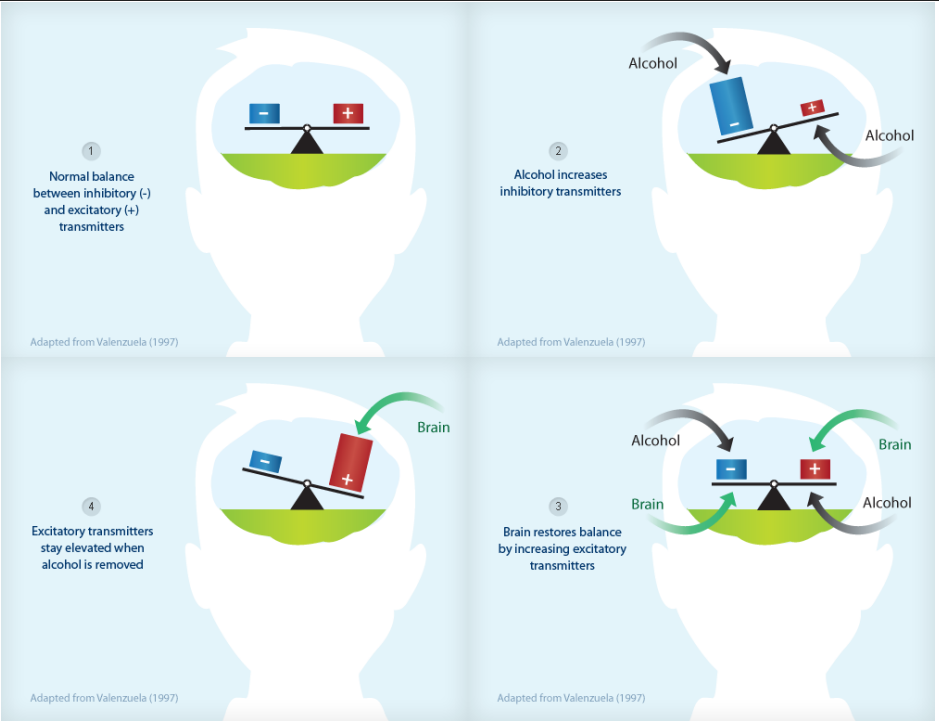
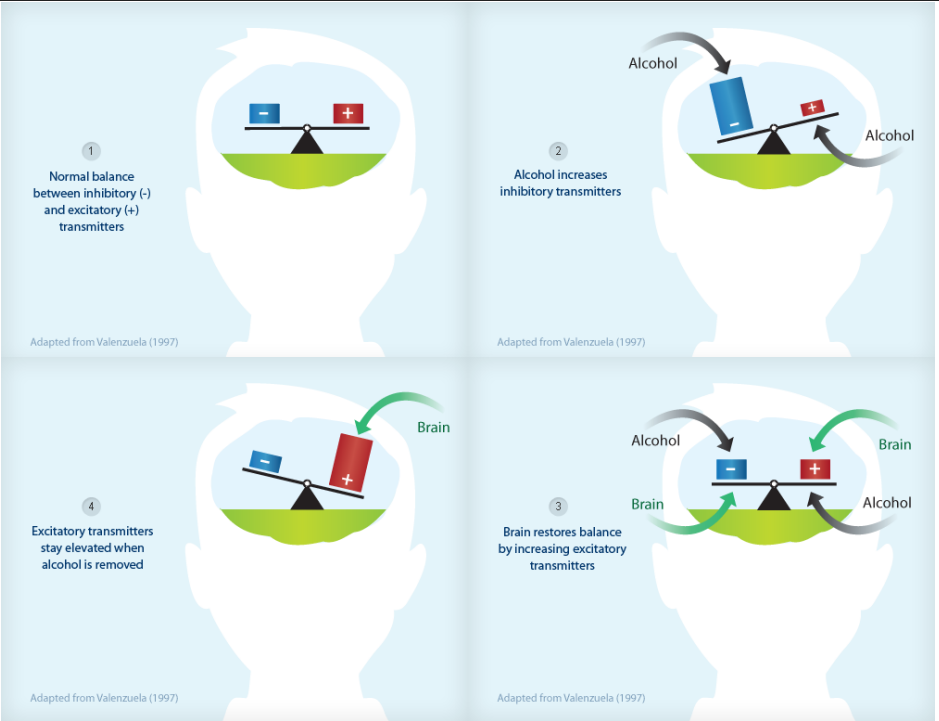
Good representation of alcohol efect on body (addiction and withdrawal)
DIAGRAM ON SLIDE 33
Withdrawal Symptoms
Mild to moderate symptoms:
- 6-48 hours, usually last 1-5 days
- shaking, sweating, tachycardia
- trouble sleeping, feeling anxious or agitated
- feeling sick and vomiting
- headaches, hallucinations
.
VERY SEVERE SYMPTOMS:
SEIZURES (GLUTAMATE +++):
- Usually occur within the first two days, in 2-9% of alcohol dependent people
'DELIRIUM TREMENS':
- usually occur 3-4 days after stopping drinking and typically resolves within 3 days
- occur in about 5% of people admitted to hospital for alcohol problems
- includes: vivid hallucinations, confusion, disorientation, agitation, hyperactivity, insomnia, trembling, resting tachycardia, sweating, fever
Withdrawal Mechanisms
- Too much glutamate (not enough GABA)
- no more happy neurotransmitters...
- taking away your reward -> addiction
- falling serotonin = anxious, depressed
- falling dopamine = craving/dependence/seeking behaviour
Treating alcohol withdrawal
SEIZURES? ANTAGONISE GLUTAMATE:
- GABA will do that
- GABA agonists: diazepam (valium)/acamprosate/baclofen
.
CRAVINGS? MODULATE DOPAMINE/SEROTONIN:
- problem - replacing the reward can jsut change the drug toy are dependent upon
- so reduce the alcohol based reward
- ondansetron (serotonin receptor antagonist) - takes away the alcohol 'reward'
- Naltrexone (opioid receptor antagonist) - takes away the alcohol 'high' = driunking is less rewarding, stopping creates less cravung.