NS 1150: Prelim 01 Review
1/174
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
175 Terms
What is nutrition?
The sum total of processes involved in the intake and utilization of food substances by living organisms, including ingestion, digestion, absorption, transport, and metabolism of nutrients in food
What does environment influence?
Choice and decisions of food
True or False: Life without the nourishment of food is not possible
True
What is metabolism?
It encompasses all chemical processes that occur within a living organism (a cell) to maintain life
Glycolysis is at the center of metabolism
Why do we care about nutrition?
Food is medicine: food can help prevent disease
The type of food we eat influences health: development, management, and progression of chronic disease
What is a nutrient?
A substance found in foods that performs one or more physiological or biochemical functions in the body
True or false: All nutrients are the same
False: NOT all nutrients are the same
What are the major functions of nutrients?
Energy: all three macronutrients provide energy, but the body relies primarily on carbohydrates and fat
Structure: promote tissue growth and development, mostly proteins
Regulation: all nutrients
Note: the body makes changes and adapts to preserve protein
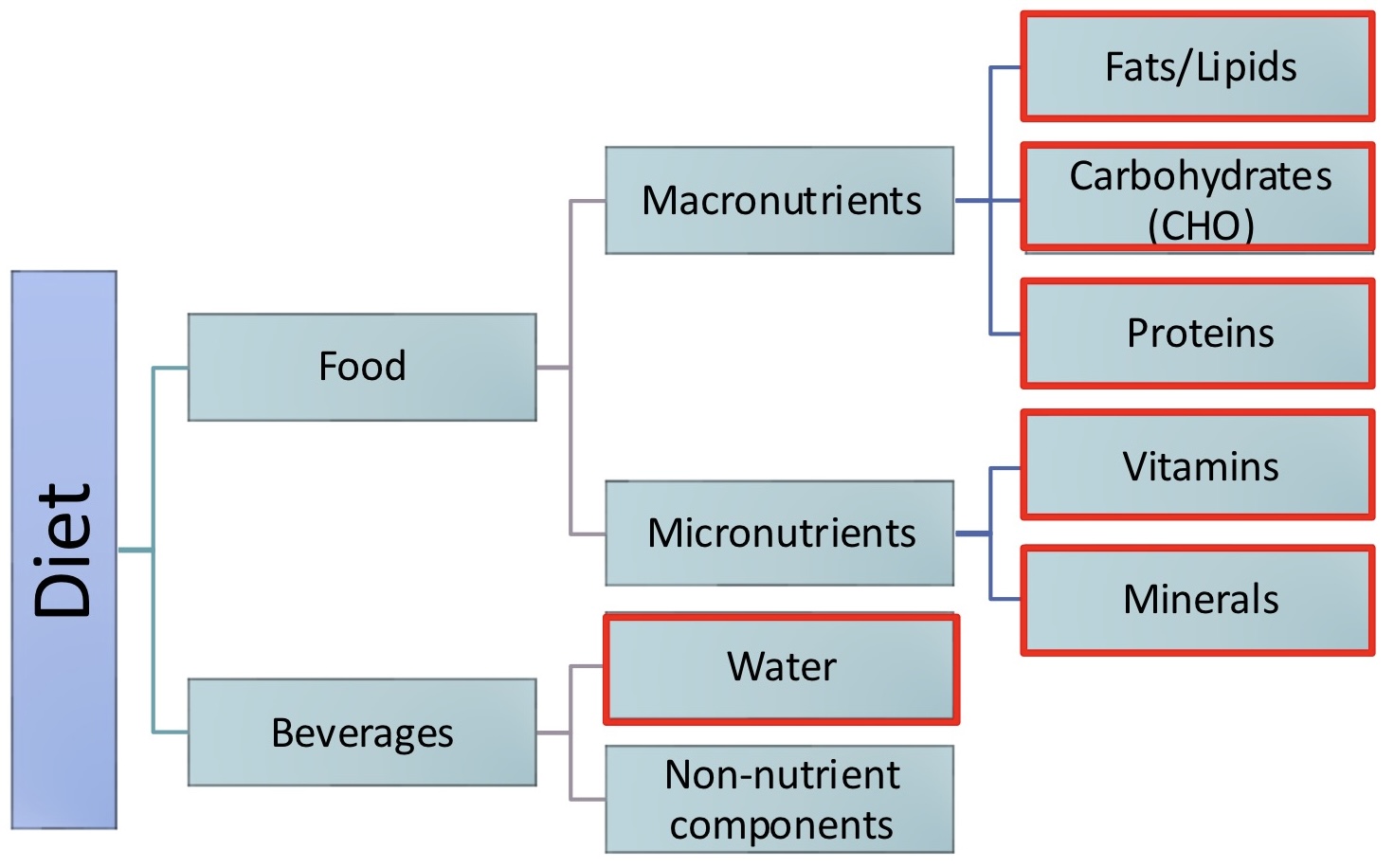
What are the classifications of nutrients?
Organic/Inorganic
Essential/Non-essential or Conditionally essential
Energy-yielding/Non-energy-yielding
Macronutrients/Micronutrients
What does organic and inorganic refer to? What are some examples?
Organic: molecules with carbon atoms
Carbohydrates
Fats/lipids
Protein
Alcohol
Vitamins
Inorganic: molecules without carbon atoms
Water
Minerals
Does certified organic and organic refer to the same thing?
No: certified organic means that there are no pesticides used while organic refers to molecules with carbon atoms
What are essential nutrients?
A substance that must be obtained from the diet, because the body needs it and cannot make it in the required amounts
Why do we need essential nutrients?
Energy production
Growth and development
Regulating body processes
Preventing diseases
What are nonessential nutrients? What are some examples?
A substance found in the body and used by the body to promote health but not required to be consumed on the diet (we have the enzymes to make them)
Cholesterol
Carnitine
Creatine
Some amino acids
What are conditionally essential nutrients?
Normally nonessential nutrient, but under certain circumstances (like growth or disease) it becomes essential
Obtained from diet
Creatine and chronic kidney disease
What are macronutrients and micronutrients?
Macronutrients: to preserve normal body functions, the human body needs these nutrients in large quantities
Micronutrients: the human body needs these nutrients in smaller quantities
What are energy yielding nutrients?
Participate in pathways that make ATP
What are some energy yielding nutrients?
Lipids/Fats: 9kcal/gram
Carbohydrates: 4kcal/gram
Proteins: 4kcal/gram
Alcohol: 7kcal/gram
Note: Alcohol is not a nutrient
What type of nutrients are vitamins and minerals?
Essential, but not energy-yielding nutrients
How many liters of water do we need everyday? How can we obtain water? Why do we need water?
About 2.4 L/day
From liquid or solid/semisolid food intake, and oxidation of food
We need water for:
Transport of nutrients, gases, and waste products
Medium for chemical reactions
Body temperature regulation
What are the two categories of non-nutrient components?
Naturally occurring
Added (intentionally or unintentionally)
What are three different non-nutrient components?
Phytochemicals: health-promoting compounds found in plants
Compounds in tomatoes and garlic
Antioxidants
Zoonutrients: health-promoting compounds found in animals
Nonessential lipids in fish
Functional Foods: foods that are fortified or enhanced to promote health
Phytochemicals, zoonutrients, probiotics
Yogurt
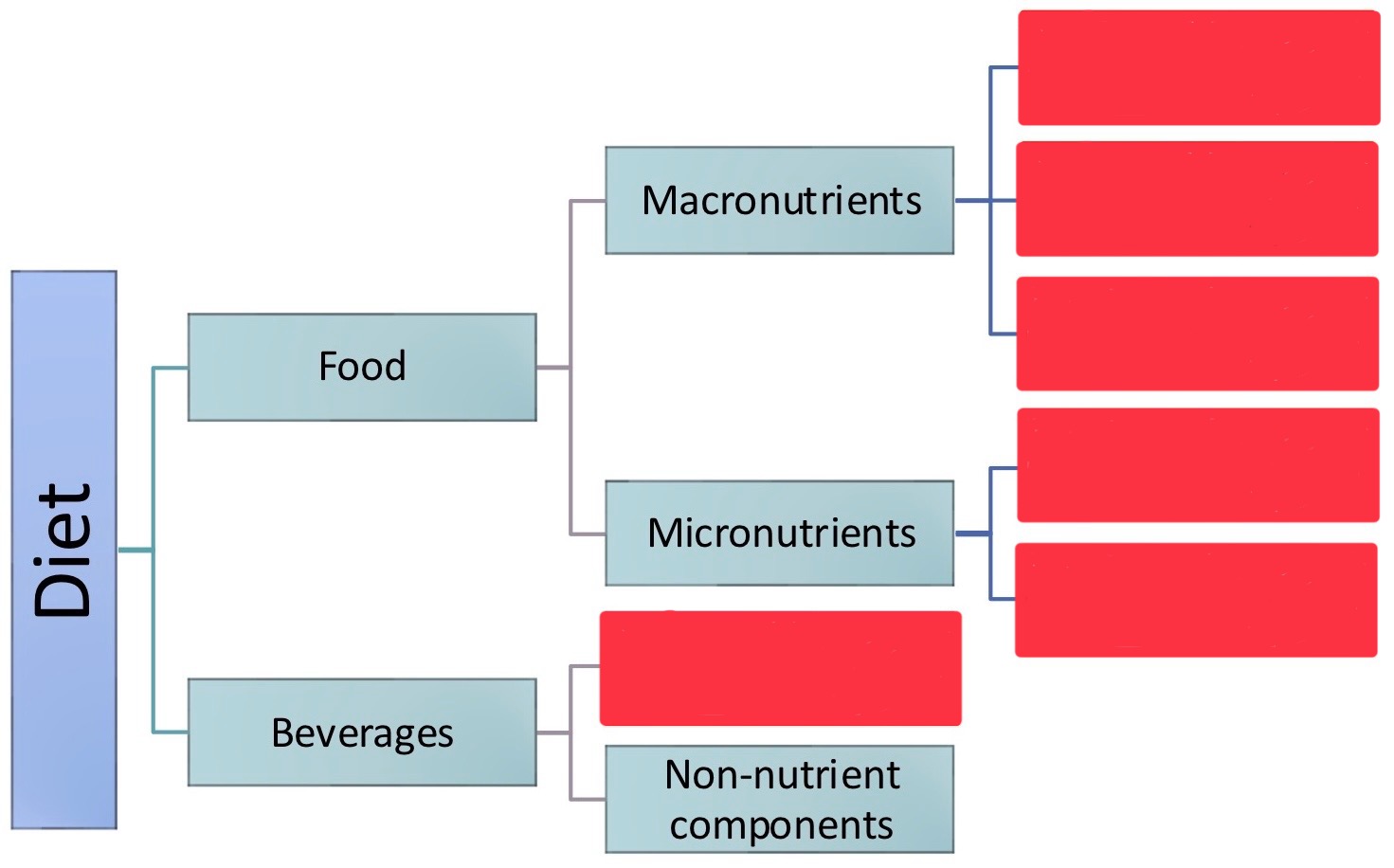
Fill in the essential nutrients
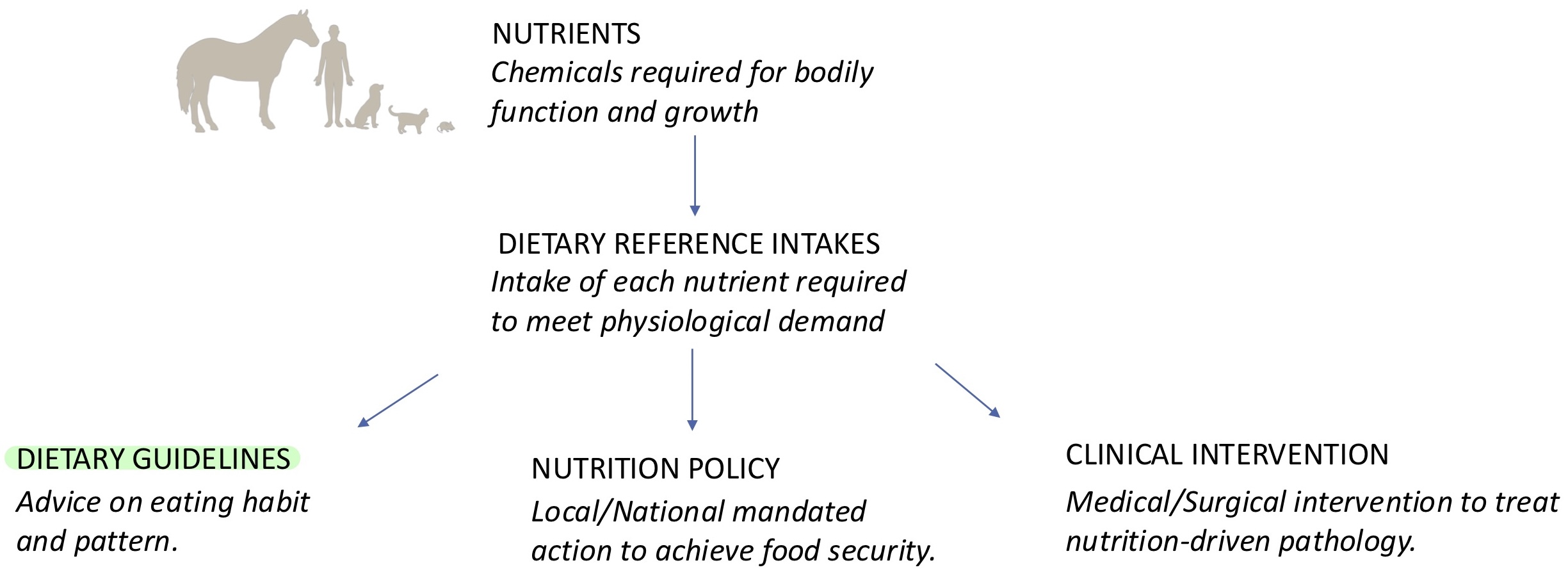
What is dietary reference intakes (DRI)?
A set of dietary reference values to aid individuals in optimizing their health, preventing disease, and avoiding nutrient overconsumption
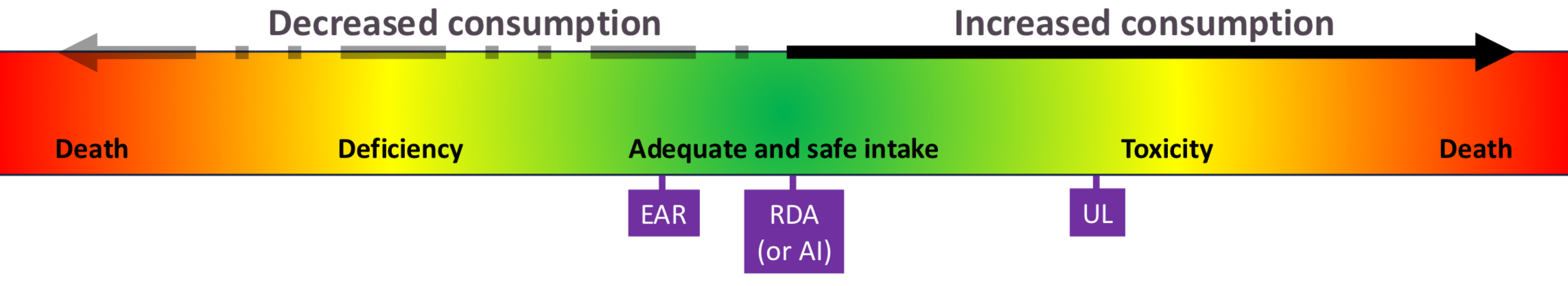
What are the categories for dietary reference intakes?
Estimated average requirement (EAR)
Recommended dietary allowance (RDA)
Adequate intake (AI)
Tolerable upper intake level (UL)
Estimated energy requirements and acceptable macronutrient distribution range
Chronic disease risk reduction intake
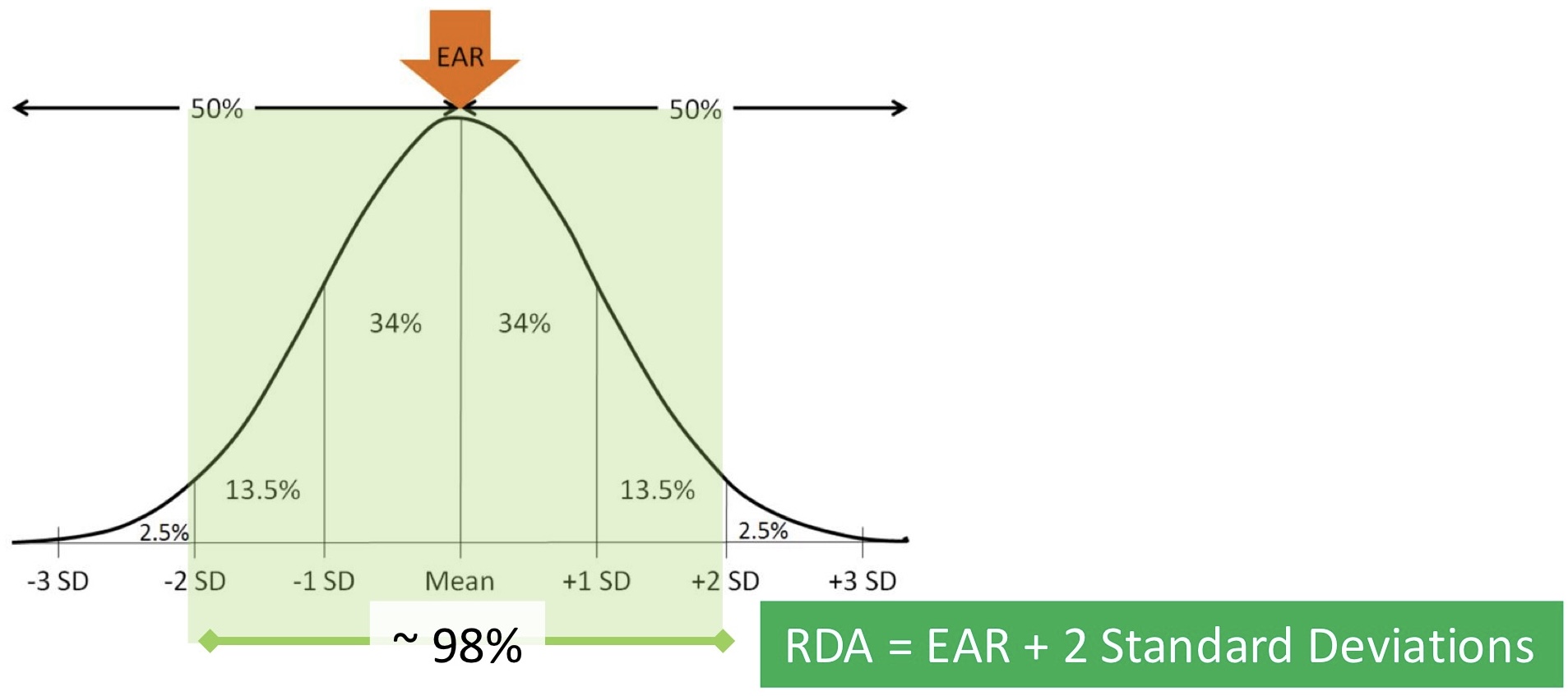
What is estimated average requirement (EAR)?
The nutrient value estimated to meet the requirement of 50% of healthy individuals
Average daily level of intake estimated based on scientific data to meet the requirements of 50% of healthy individuals. EAR is required to calculated RDA
What is recommended dietary allowance (RDA)?
Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals
What is adequate intake (AI)?
It is established when scientific evidence is not sufficient to determine an RDA. As an intake is not a requirement, is likely to exceed the actual requirements of almost all individuals in a life-stage group
Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an RDA
What is tolerable upper intake/upper level (UL)?
Used as the highest level of daily nutrient intake that poses no risks of adverse health effects to most individuals in the general population
Maximum daily intake unlikely to cause adverse health effects. The UL is not intended to be a recommended level of intake, and there is no established benefit to healthy individuals if they consume a nutrient in amounts exceeding the recommended intake (the RDA or AI)
What is estimated energy requirements (EER)?
Used to estimate the calorie needs of the average person within a specific height, weight, gender, age, and physical activity pattern
What is chronic disease risk reduction intake (CDRR)?
Characterizes nutrient intakes that are expected to reduce the risk of developing chronic disease
What is the purpose of Dietary Guidelines for Americans?
Every 5 years
Purpose: inform policymakers, and nutrition and health professionals who develop food, nutrition, and health policy
What does the Dietary Guidelines for Americans explain, discuss, and consider?
Explains data that supports key recommendations
Discusses the health benefits of lifelong healthy dietary choices
Considers nutrition and health across the lifespan
Infants and toddlers
Children and adolescents
Adults
Pregnancy and lactation
Older adults
What are dietary patterns? What is the central aim? What is it not? Is it the same for everyone?
A dietary pattern refers to the combination of various foods, drinks, and nutrients that comprise an individual's total dietary intake over time, including the quantities, proportions, variety, and frequency with which they are consumed (The big picture of what you eat on a regular basis)
The central aim to promote dietary patterns associated with positive health outcomes
Dietary pattern is NOT about simply fulfilling daily recommended allowances
Unique to each individual person across
A healthy dietary pattern limits added sugars to how much?
<10% of calories per day
How many calories do added sugars account for?
Added sugars account on average for almost 270 calories - or >13% of total calories - per day in the U.S. population
Intake of saturated fat should be limited to how much?
<10% of calories per day
What percent of individuals consume amounts of saturated fat consistent with the limit?
23%
What is the old and new advice for dietary cholesterol?
Old advice: Limit intake to <300mg per day
New advice: “individuals should eat as little dietary cholesterol as possible”
Healthy eating patterns limit the adult consumption of sodium to CDRR levels by how much?
≤ 2300 mg/day
What is the average intake of sodium for those ages 1 and older?
About 3393 mg per day
What is a nutritional scientist?
A person who conducts and/or evaluates nutrition-related research
What is a dietitian?
A nutritionist who helps people make healthy dietary choices
What are Dietary Guidelines?
They provide science-based advice on what to eat and drink to promote health, reduce risk of chronic disease, and meet nutrient needs
What aren’t Dietary Guidelines?
Not lawful, no legal basis and not enforced
Not mandatory, but forms the basis of Federal nutrient policy and programs
Not clinical guidelines, not intended for treating diseases
What was common amongst British sailors in the 18th century?
Scurvy
What are the symptoms of scurvy?
Bruising blue/red spots on the skin
Slow to heal wounds
Bleeding from gums
Loosening of teeth
Muscle pain
Joint pain
Fatigue
Fever, convulsions
Death
How many sailors died from scurvy between the 16th and 18th centuries?
Responsible for more than 2 million deaths amongst sailors
How many men did Vasco de Gama and George Anson lose (mainly due to scurvy)?
Vasco da Gama: lost 116 of 170 men on his first voyage to India in 1499
George Anson: lost 1,666 of the 1,854 men following a 4-year circumnavigation trip in 1744
What can nutritional imbalance/inadequacy lead to? What are some modern examples?
Can lead to major detrimental health impact on entire population
Modern examples:
Obesity
Type 2 diabetes
What are some failed treatments for scurvy?
Sulfuric acid
Venesection (blood-letting)
Drinking seawater
What are some effective treatments for scurvy?
Eating rats
“Scurvy grass” (Cochlearia officinalis)
Citrus fruit
Who is James Lind? What is he known for?
Surgeon’s mate in the Royal Navy in late 1730s
Witnessed many cases of scurvy first-hand
1747: carried out the world’s first recorded “randomized controlled trail”
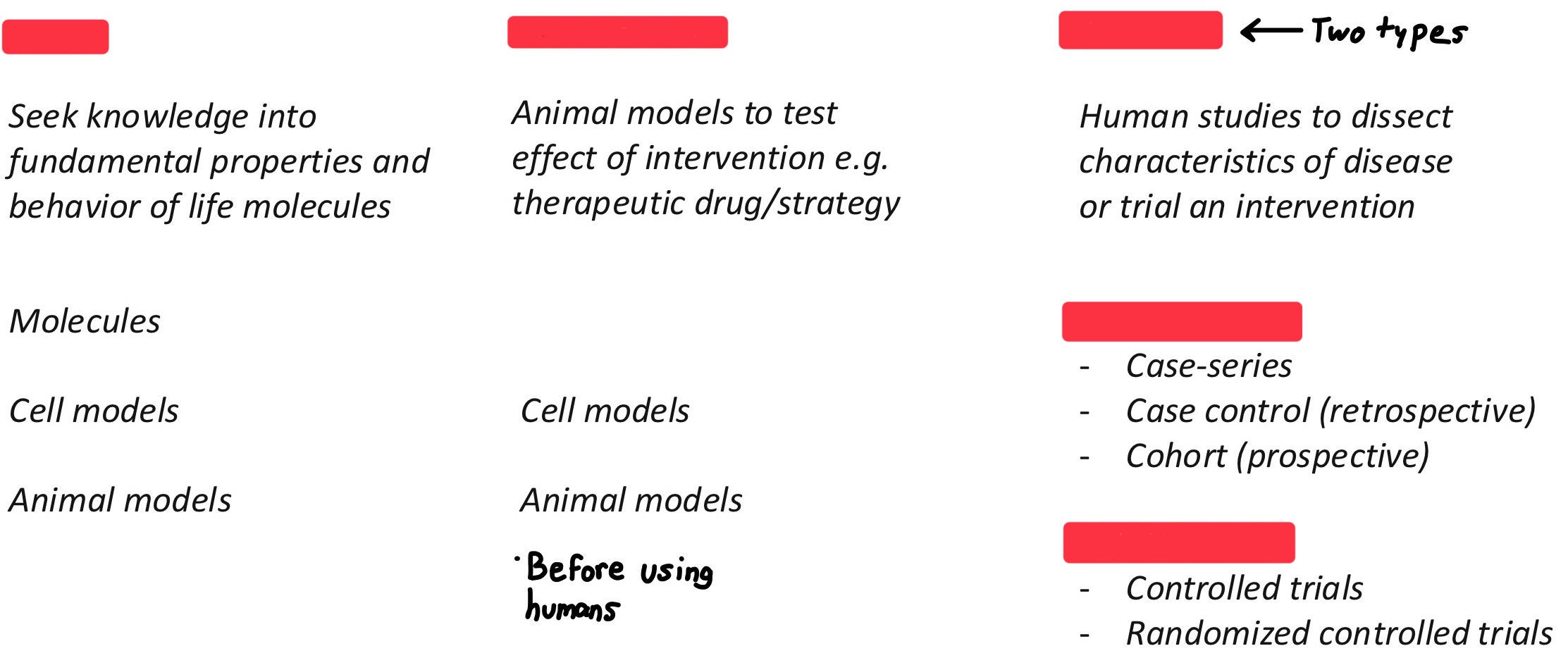
Regarding bio-medical research, fill in the blanks
Describe James Lind’s randomized controlled trial
12 sailors divided into 6 groups of 2 sailors
Each group randomized to receive one of the following treatments:
A quart of cider daily
25 drops of elixir of vitriol, three times a day
Half a pint of sea-water a day
Paste of garlic, mustard seed, horse-radish, balsam of Peru, and gum myrrh three times a day
Two spoonfuls of vinegar, three times a day
Two oranges and one lemon a day
Note: bolded example was the effective one
After James Lind’s randomized controlled trial, was scurvy cured?
No because of the challenges:
Poorly documented study, published in 1753 (experiment done in 1747)
Poor dissemination to Navy/wider public
Lack of influence
Unable to translate result into practical guideline/policy
No one acted on these results
No dietary guideline/policy implemented
Who was Gilbert Blane of Blanefield? What is he known for?
Physician in the Royal Navy
Reproduced James Lind’s study
Used alcohol as a preservative to maintain lemon juice
Blane recommended findings to Admiralty
1795: Royal Navy mandated lemon juice to be consumed daily by every sailor.
How much citrus was needed for the royal navy?
50,000 gallons of citrus juice per year
Regarding the 1800s, what are the benefits of a nutritional policy?
Naval tactical superiority
Protection and expansion of British Empire
Economic productivity
What do food choices impact?
Development of society and economy
What does vitamin C act as for enzymes involved in collagen synthesis?
What enzymes use vitamin C to catalyze the addition of hydroxyl (OH) groups onto proline and lysine residues in the collagen peptide?
What does the addition of these hydroxyl groups allow?
What does a deficiency of vitamin C cause?
Vitamin C (Ascorbic acid) acts as an essential co-factor for enzymes involved in collagen synthesis
Prolyl-hydroxylase and lysyl-hydroxylase enzymes uses vitamin C to catalyze the addition of hydroxyl (OH) groups onto proline and lysine residues in the collagen peptide
Addition of these hydroxyl groups allow the collagen peptide chain to crosslink into a triple-peptide helix structure, thus providing tensile strength
• Deficiency of vitamin C results in ‘weak’ collagen resulting in breakdown to connective tissue in skin, muscle, joints, gumThis leads to the symptoms in scurvy.
What do humans and guinea pigs lack for vitamin C synthesis?
Although rats can synthesize their own vitamin C, what does cooking the meat destroy?
Humans (and guinea pigs) lack a vital enzyme called GULO (L-Gulonolactone oxidase) required for vitamin C synthesis
Other mammals including rats can synthesis their own vitamin C and therefore can survive on long voyages unaffected by scurvy
In fact, eating rats provided a small amount of vitamin C which explains why this offered limited treatment against scurvy
But cooking the meat will destroy its vitamin C content
Who is at risk of vitamin C deficiency?
Intake deficiency:
Socio-economic: social isolation/nutrient insecurity
Behavioral: alcohol/Infant feeding practices
Pathology: allergy/eating disorders
Malabsorption:
Inflammatory bowel disease
Bariatric surgery
Increased consumption:
Smoking
Increased excretion:
Kidney diseases
How can dietary guidelines help?
They can ask questions such as:
How much vitamin C do we require every day?
Is vitamin C requirement the same for everyone?
How do we meet our vitamin C requirement from our diet?
What happens if we over-supplement/are deficient in vitamin C?
How do we educate/inform people about vitamin C?
Do we need a National food fortification policy?
What does the Dietary Reference Intakes (DRI) include?
Documents issued by the Food and Nutrition Board:
Information on basic function of nutrients, food sources, and effects of deficiencies and excessive intakes
Offer quantitative estimates of nutrient intakes to maintain health in US and Canada
Addresses issues of safety, quality, and adequacy of the food supply
What are the life stage groups and years?
Infancy: 0 – 6 months; 7 – 12 months
Toddler: 1 – 3 years
Early Childhood: 4 – 8 years
Puberty/Adolescence: 9 – 13 years, 14 – 18 years
Young Adulthood and Middle Ages: 19 – 30 years, 31 – 50 years
Adulthood and Older Adults: 51 – 70 years, >70 years
Pregnancy and Lactation
What are DRI reference values?
EAR, RDA, UL, AI
What do DRI reference values vary by?
Life stage group and sex
What does DRI help establish?
Dietary guidelines, national policies, and clinical guidelines
How do we meet our vitamin C requirement from our diet?
Recommendations on what to eat and drink to meet nutrient needs, promote health, and prevent disease
Who makes up the DGA advisory committee expert panel
Scientists, policymakers, healthcare providers, nutrition educators, and Federal nutritional program operators
What do DGAs use to assess benefits and risks associated with nutrient intake?
DRIs
What is the DGA framework?
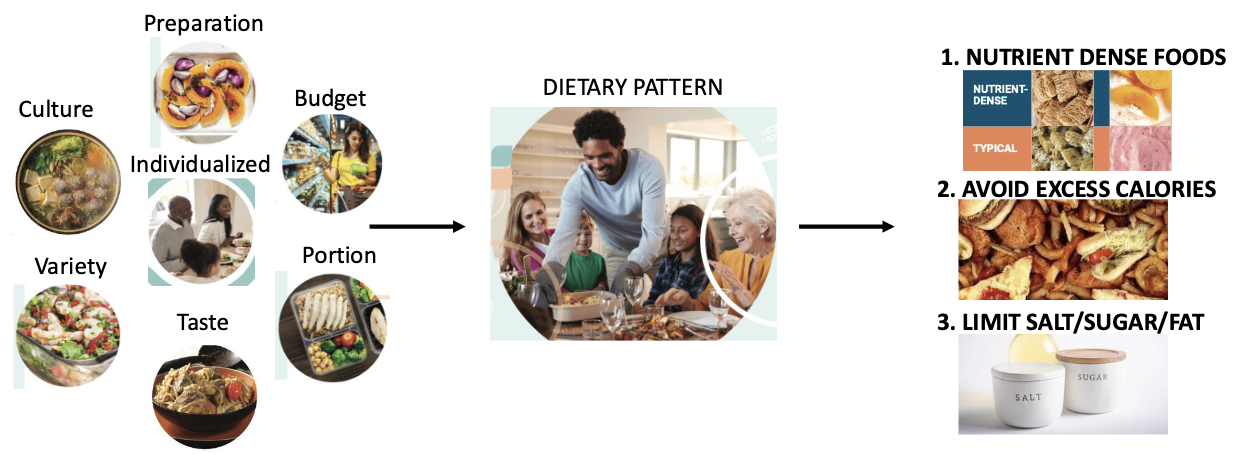
What are nutrient dense foods?
Nutrient dense foods contain higher macro/micronutrient per weight
Lower saturated fat content, sugar and salt
Nutrient dense food contain fewer calories
How can you avoid excess salt/sugar/fat?
Fill in the blanks
What are individualized dietary patterns?
Choice of ingredients and preparation method
Cultural background can have significant impact on food and beverage choice
Must fit a range of budgetary constraints
Variety within different food groups and incorporate fresh, frozen, dried, canned options
Portion size important to meet calorie needs
Lastly must align with individual/family preference
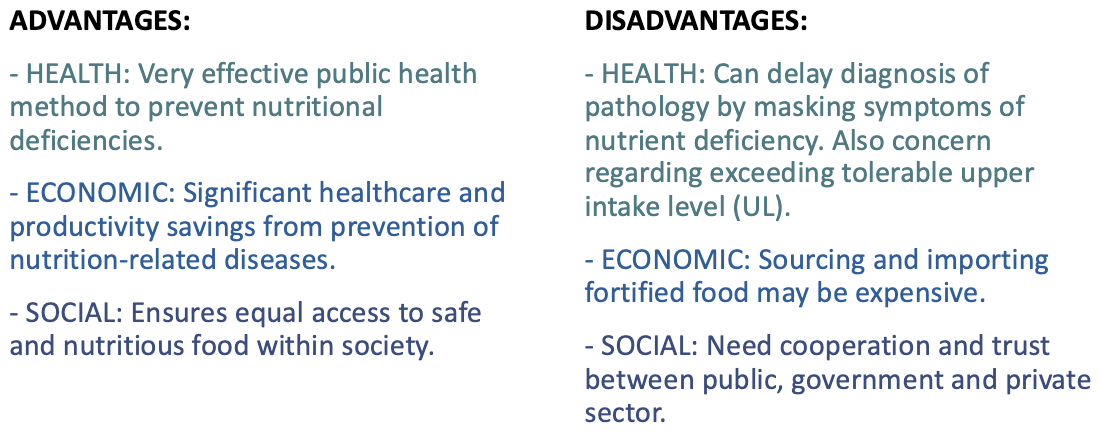
What is the national fortification policy?
Fortification of food is the addition of nutrients that are not typically found in the food
Fortification is a systematic approach to correct identified nutrient deficiencies in the population
Not mandatory in the US, but recommended to food supplier/manufacturer
Contrast with ‘enrichment’ which involves adding back nutrients that were lost during the processing of the food
What are advantages and disadvantages of the national fortification policy?
What happened in the 1920s regarding iodine fortification in salt?
Iodine required by thyroid gland to produce thyroid hormone
Deficiency in iodine triggers enlargement of thyroid (goitre) in attempt to make sufficient thyroid hormone, as well as hypothyroidism which can affect weight, fatigue, neuro-cognitive decline
By 1924, iodine was fortified in table salt. Although not mandatory, this was widely adopted by industry, schools, and endorsed by medical communities
Resulted in significant decline in the incidence of goitre and hypothyroidism
What happened in the 1930s regarding vitamin D fortification in milk?
Vitamin D required for calcium absorption and bone calcification i.e. ‘hardening’ of bones
Chronic deficiency of vitamin D lead to osteomalacia (rickets in children) due to decalcification of bones. Permanent disability if not corrected
Vitamin D synthesized in skin but requires sun light exposure, which can be limited in Northern hemisphere
Food and Drug Administration recommended (not mandated) vitamin D fortification in milk to reduce prevalence of vitamin D deficiency
What happened in the 1990s regarding folic acid?
Folic acid is required for DNA replication, which is especially important in rapidly growing tissues such as the developing fetus
Folic acid deficiency during pregnancy negatively impacts fetal development, such as spina bifida where the spine fails to form an enclosed tube leading to nerve damage
The consequences can lead to lifelong disability, yet folic acid deficiency can be easily corrected with oral supplementation if detected early (or before) pregnancy
In 1998, US government launched folic acid fortification in grain products e.g. bread, cereal, flour
Fortification policy estimated to prevent 1300 babies each year from spina bifida and related defects
What do dietary guidelines for Americans provide a framework on?
A framework on promoting healthy dietary patterns to maintain health and reduce the risk of chronic disease
What do dietary patterns focus on?
Nutrient dense foods, avoid excess calories and limiting intake of salt, sugar and saturated fat
What do dietary patterns need to be?
Need to be individualized based on the culture, lifestyle, age, budget and other life factors
What do national fortification policies supplement?
Supplements additional nutrients to food
What do fortification policies prevent?
Can be very effective to prevent nutritional deficiencies and associated diseases in the population
Fill in the blanks
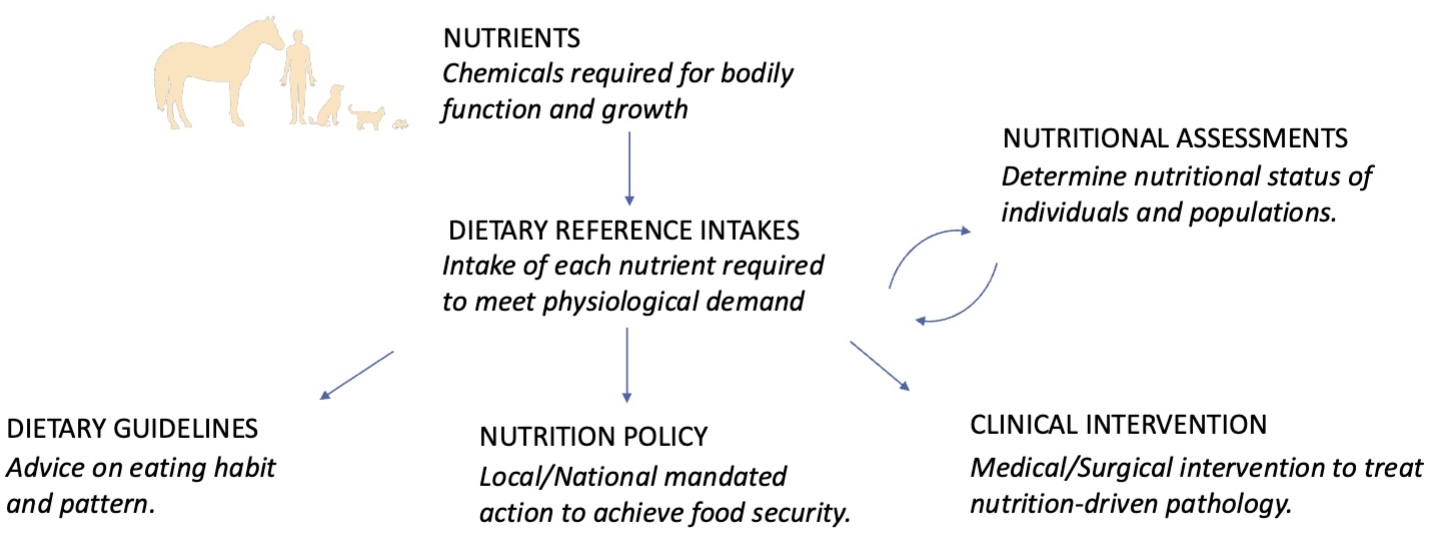
Why is nutrition assessment important?
To identify nutritional status and nutrition-related diseases
To determine appropriate nutrition therapy or programs
To assess response to nutrition/medical therapy or programs
What are the types of nutrition assessments?
Dietary
Clinical
Anthropometric
Biochemical
In terms of dietary assessment, what does retrospective refer to?
Looking back, remember foods consumed
24-hour recall
Food frequency
In terms of dietary assessment, what does prospective refer to?
Tracking intake, making a record of foods as they are consumed
Diet record
24 hour-dietary recall uses data from what?
Food preparation methods
Ingredients used in mixed dishes
Brand name of commercial products
Portion sizes
In a clinical and research setting, who interviews you during a 24 hour-dietary recall?
Clinical: Interview by trained practitioner
Research: Interview or self-administered recall (ASA24: Automated Self-Administered 24-Hour Dietary Assessment Tool)
Takes 30-45 minutes to complete
What are the pro and cons of 24 hour-dietary recall?
Pros
Intake can be quantified
Easy to complete
Cons
Relies on recall (short-term memory)
May require multiple recalls to capture habitual intake
What is a Food Frequency Questionnaire (FFQ)?
Assessing how frequently certain food and beverage items consumed over a specific extended period of time (typically 3 months to 1 year)
Focus on consumption patterns and habitual intake
Can be focused on specific food groups (i.e., vegetable intake) or all foods
What are pros and cons of Food Frequency Questionnaire (FFQ)?
Pros
Capture habitual intake
Easy to collect
Cons
Inaccuracies from incomplete listing of all possible foods
Relies on recall
What do dietary records record? Who analyzes them?
Record all food, beverages, and supplements and amounts consumed over 3-7 consecutive days (weekdays and weekend days)
Trained practitioner analyzes records to determine energy and nutrient intakes