Principles of prescribing in renal disease
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
What is the role of the kidney? (3)
1) Filter blood to remove waste products of metabolism
2) Keep electrolytes (Na+ and K+) and water content of the body constant (regulates blood volume and plasma osmolarity)
3) Secrete several essential hormones
What is the difference between efferent and afferent?
Afferent: enters
Efferent : leaves
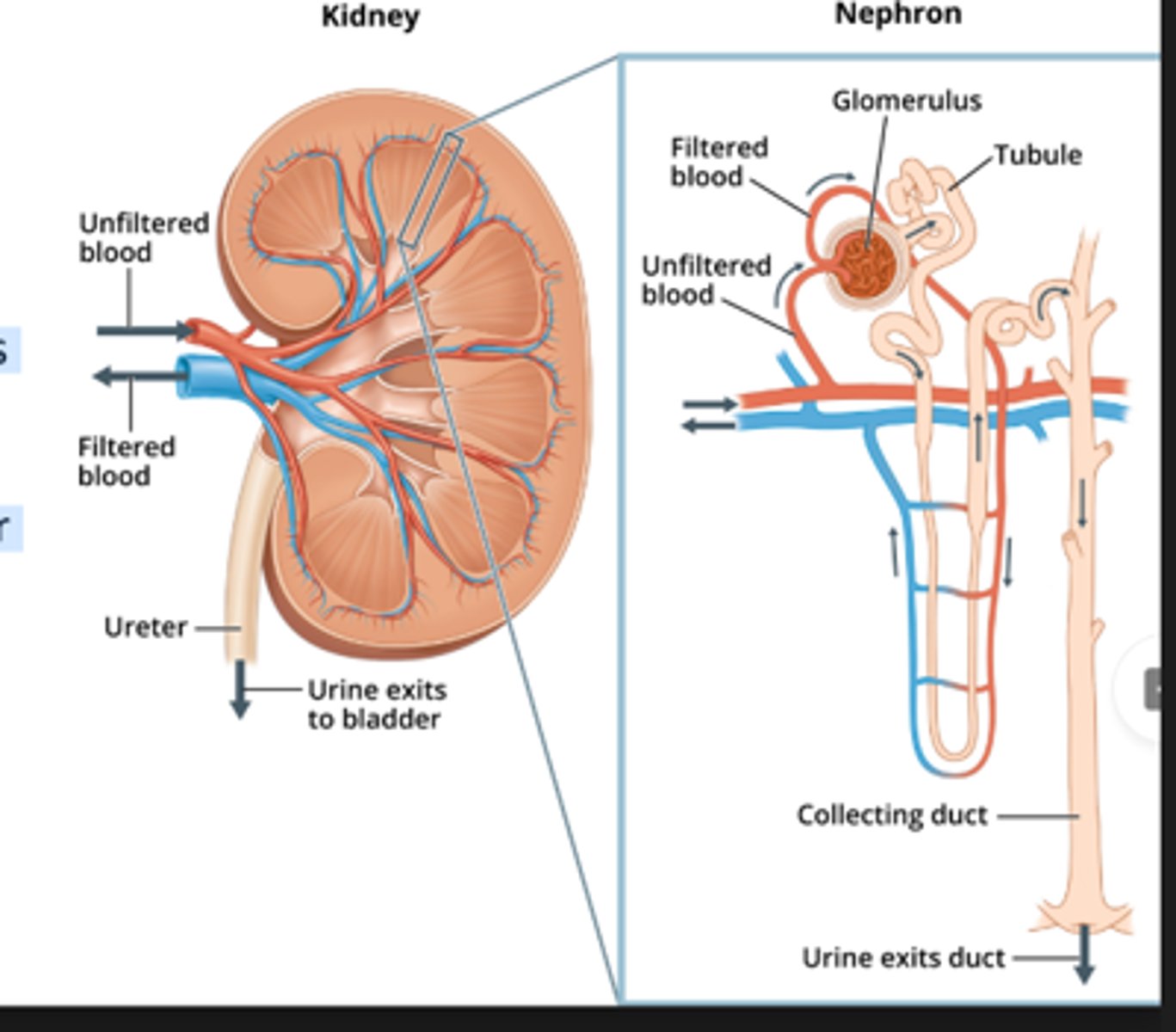
Draw the kidney and the nephron
What is chronic kidney disease?
Reduction in kidney function or structural damage present for greater than 3 months.
This will lead to a build-up of waste and fluid in the body.
Classically a permanent and progressive disease.
Usually ASYMPTOMATIC and diagnosed via routine check-ups
Symptoms are often associated with complications
What are the causes of chronic kidney disease? (8)
Diabetes-->Nephropathy (high impact of sugar)
HTN
Glomerulonephritis
AKI
Medications- usually due to sustained damage
Obesity- increases the workload of the kidney
Obstructive uropathy
CVD
How can an AKI lead to CKD?
Lead to ischaemic changes that the kidney can sometimes not rebound from. A significant AKI
What is Glomerulonephritis and how can it cause CKD?
Glomerulonephritis is a condition where the glomeruli, the tiny filters in the kidneys that remove waste and excess fluid from the blood, become inflamed and damaged.
This inflammation can be caused by various factors, including infections, autoimmune disorders, or other underlying conditions.
Progressive Damage:
If glomerulonephritis is not treated or progresses, the damage to the glomeruli can become severe and lead to chronic kidney disease (CKD).
What is obstructive uropathy and how does it lead to CKD?
Obstructive uropathy, a blockage in the urinary tract
When urine cannot drain properly, it backs up into the kidneys, causing them to swell (a condition called hydronephrosis).
Prolonged hydronephrosis can lead to kidney damage.
Chronic obstruction can cause renal fibrosis which further impairs their function.
How does CVD lead to CKD?
CVD and CKD share common risk factors, including high blood pressure, diabetes, and a family history of kidney or heart disease.
High Blood Pressure:
High blood pressure can damage the small blood vessels in the kidneys, impairing their ability to filter blood effectively, leading to CKD.
Diabetes:
Diabetes can damage the blood vessels and nephrons in the kidneys, reducing their ability to filter waste and excess fluid, which can lead to CKD.
Heart Failure:
When the heart isn't pumping efficiently, blood can back up in the veins leading to the kidneys, causing fluid buildup and reducing blood flow to the kidneys, which can damage them and lead to CKD.
Kidney Damage and Blood Pressure:
Damaged kidneys may not be able to effectively filter excess water and salt from the body, leading to high blood pressure, which in turn can worsen kidney disease.
What is the presentation of CKD? (8)
Pruritus (itching)
Due to urea
Loss of appetite
Nausea
Oedema
Muscle cramps
Peripheral neuropathy
Pallor
Hypertension
What are the complications associated with CKD (5)?
Anaemia
Renal bone disease (RBD)
Cardiovascular disease
Stroke, MI, Backload of fluid, heart works harder
Peripheral neuropathy
Imbalance of electrolytes, leading to Pins and needles
Dialysis related problems
What are the main problems associated with dialysis? (5)
Anaemia
Mineral and bone disorders
Fluid overload
Acidosis
Hyperkalaemia
How does CKD lead to anaemia?
Reduced Erythropoietin (EPO) Production:
Healthy kidneys produce EPO, which stimulates the bone marrow to produce red blood cells.
In CKD, the kidneys are damaged and cannot produce enough EPO, leading to a shortage of red blood cells.
This results in fewer red blood cells to carry oxygen throughout the body, causing anemia.
Iron deficiency
Kidneys play a role in regulating iron levels in the body.
In CKD, the kidneys may not function properly, leading to iron deficiency.
How does CKD lead to renal bone disease?
Impaired Mineral and Hormone Regulation:
When kidneys are damaged, they can't effectively filter blood and regulate the levels of key minerals and hormones, leading to imbalances.
Impacts Vit D and Ca2+ and parathyroid levels disrupted so bone turnover is altered
How is CKD managed?
Monitor renal function
Suspend nephrotoxic medication if at risk of AKI (acutely)
FBC - rule out anaemia
Bone profile - rule out RBD
What are the key methods renal function is monitored?
No compelling evidence to support one calculation over another. eGFR and CrCl often are similar
eGFR (ml/min/1.73m2)
Estimated glomerular filtration rate
True GFR can be accessed via IV radioisotope
Can use EPI/MDRD EPI=newer and more accurate
CrCL
Creatinine Clearance Creatinine is a waste product from the normal wear and tear of muscles
ACR
Albumin:Creatinine ratio
Test to measure amount of albumin (protein) in the urine
What are the drawbacks for using eGFR?
Reports using standardised body surface area (BSA) of 1.73m2
Overestimates renal function in smaller patients
Underestimates renal function in larger patients
DO NOT USE IN - drug dose titrations, elderly patients or extremes of muscle mass
Compare CrCL and eGFR and ACR
eGFR
Estimates glomerular filtration, how much blood is filtered through both glomerular in the body per minute
Need to identify a kidney issue quickly and solve it. Why we use estimates
CrCL
Good for calculating how well we think the kidneys are working
Specific for individual body weight and easy to work out
Good for med dose changes
ACR
Good for assessing CKD
What is important to remember about serum creatnine and CrCL
Estimate of a patients kidney function • Not based off BSA, less likely to over/under estimate function • Provides a 'snapshot' • NB - if a patient is on renal replacement therapy creatine provides no useful information
What is the formula for CrCl
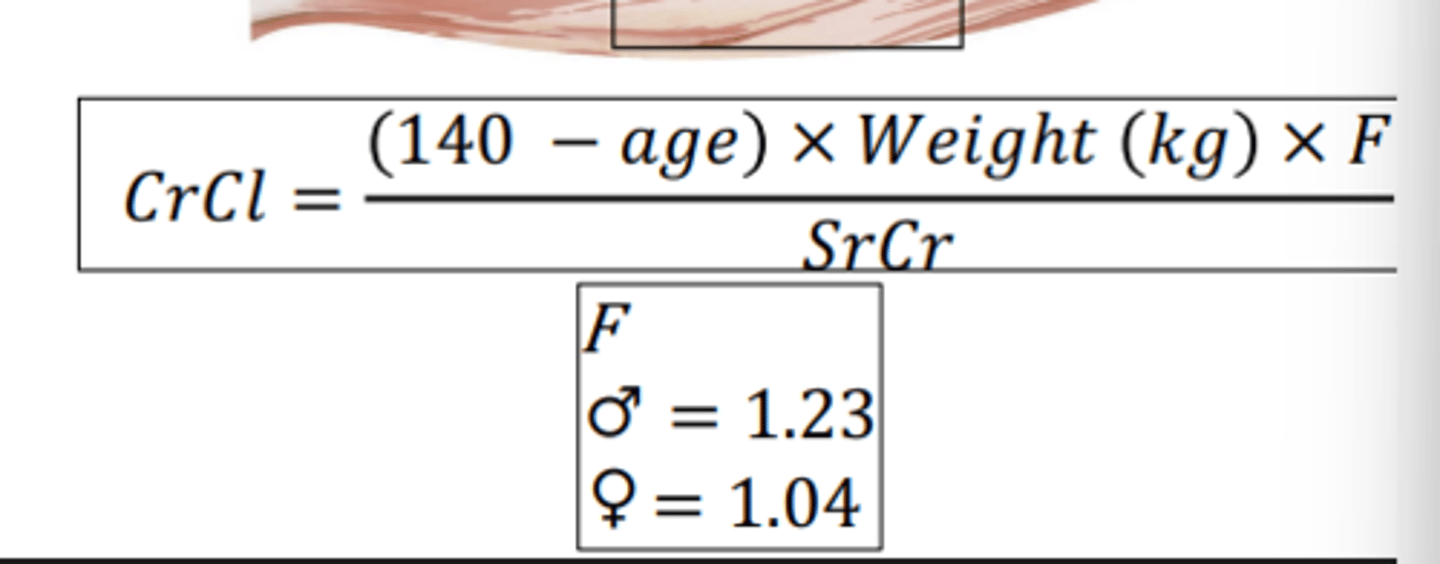
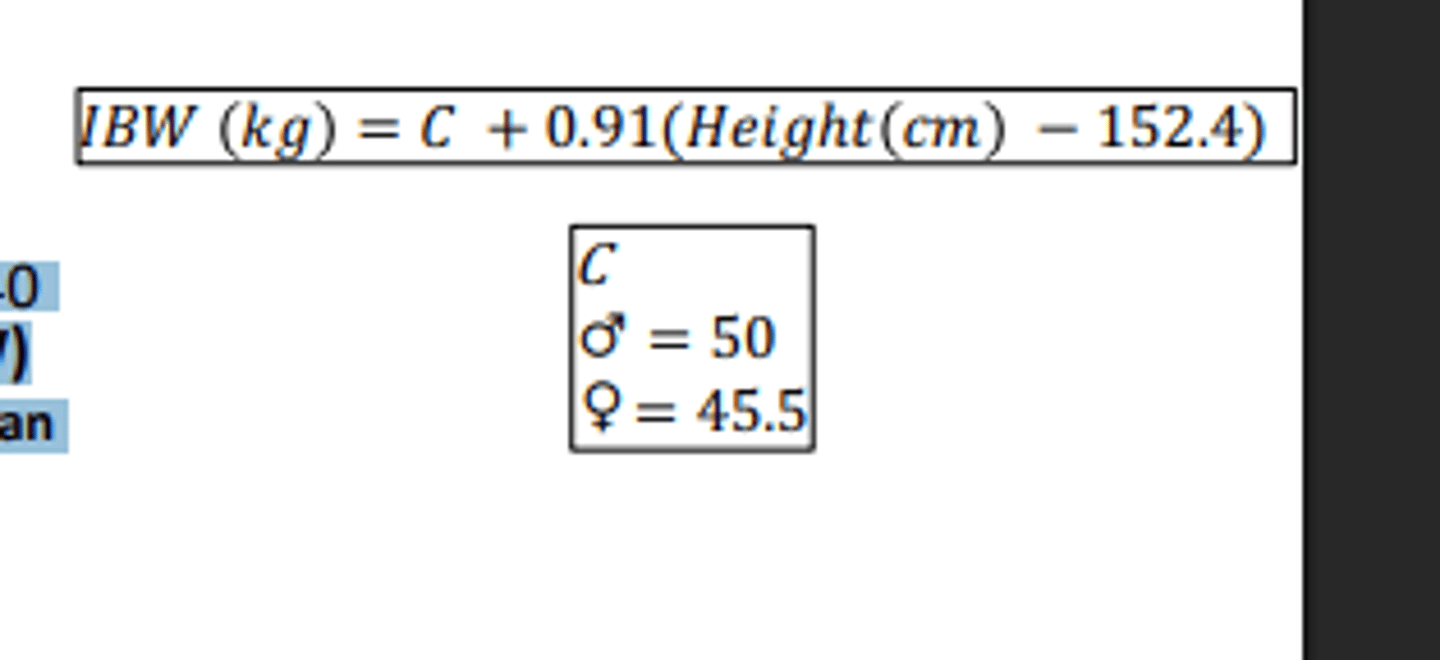
What are the limitations for CrCl ?
Caution in elderly, body builders, amputees, muscle wasting disorders and vegans
Patients with BMI <18 kg/m2 or >40 kg/m2 use ideal body weight (IBW) • Unless actual body weight is less than ideal Not accurate in periods of rapidly changing renal function (e.g. AKI)
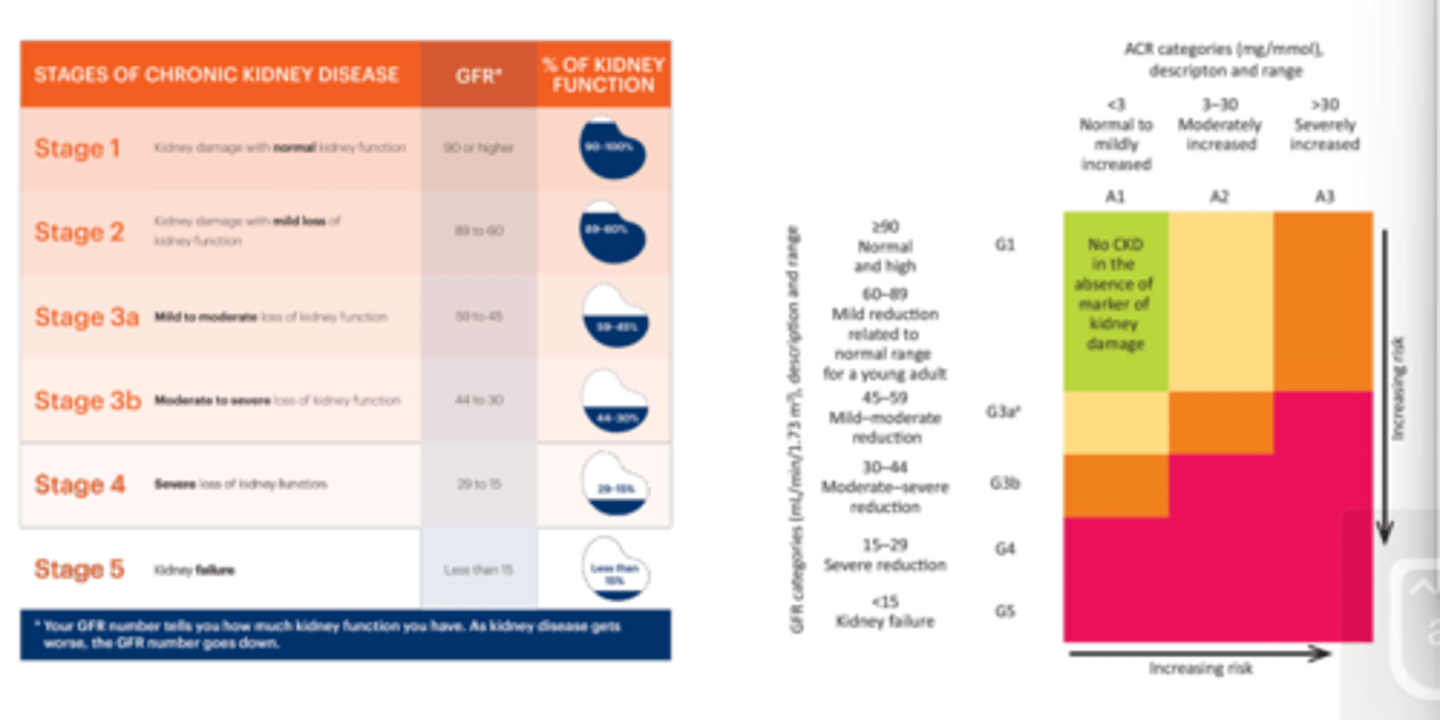
What are the stages of kidney disease|?
Stage 1
Kidney damage with normal kidney function
90 or higher eGFR
90-100% pf kidney function
Stage 2
Kidney damage with mild loss of kidney function
89 to 60 eGFR
59-50%
Stage 3a
Mild to moderate loss of kidney function
59 to 45 eGFR
59-45%
Stage 3b
Moderate to severe loss of kidney function
44 to 30
44-10%
Stage 4
Severe loss of kidney Function
29 to 15
29-15%
Stage 5
* Your GFR number tells you how much kidney function you have. As kidney disease gets
worse, the GFR number goes down.
Kidney failure
Less than 15
Less than
15
Can also categorise using ACR
What are the principles of management for CKD?
Identify underlying cause and manage to slow progression of disease
Control DM
Control HTN
Treat glomerulonephritis
Treat complications
Metabolic acidosis – give Sodium bicarbonate which acts as a buffer
Anaemia – Erythropoietin (α, β, θ) + Iron replacement • RBD – Vitamin D • Dialysis? Renal transplant?
Why do we give Erythropoietin (α, β, θ)?
Give synthetic hormone (glycoprotein that mimics the job and causes bone marrow to produce RBC's)
What is the pharmacological management of CKD, and why is each one used (4)?
ACEi
In the long term they are renal protective
By inhibiting RAAS, you can prevent damage from this
Is nephrotoxic
Anti platelet
Prevent cardiovascular events. CKD can lead to changes in blood clotting factors and platelet function, increasing the risk of blood clots (thrombosis).
Statin- manage CVD risk
SGLT-2
Dapagliflozin/empagliflozin
Used in HF, DM and CKD
Mild diuretic effects, reduces pressure of kidneys
Reduces free circulating glucose
What is an AKI?
Acute Kidney injury
Kidney can recover, the damage isn't permanent, should rebound back to what it was
Underlying causes are not always clear
Especially prevalent in hospital
CKD and AKI are not mutually exclusive
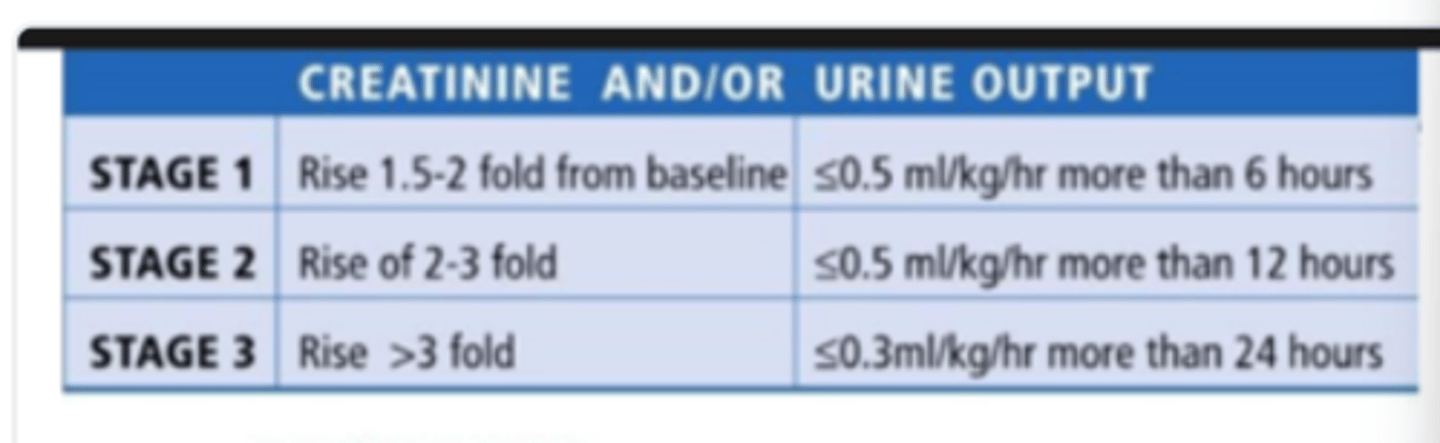
What are the NICE guideline criteria for an AKI?
SrCr ↑ of ≥ 26 micromol/L in 48 hours
SrCr ↑ of ≥ 50% in 7 days
Urine output <0.5ml/kg/hour for >6 hours (only applicable where output can be measured, e.g. catheter)
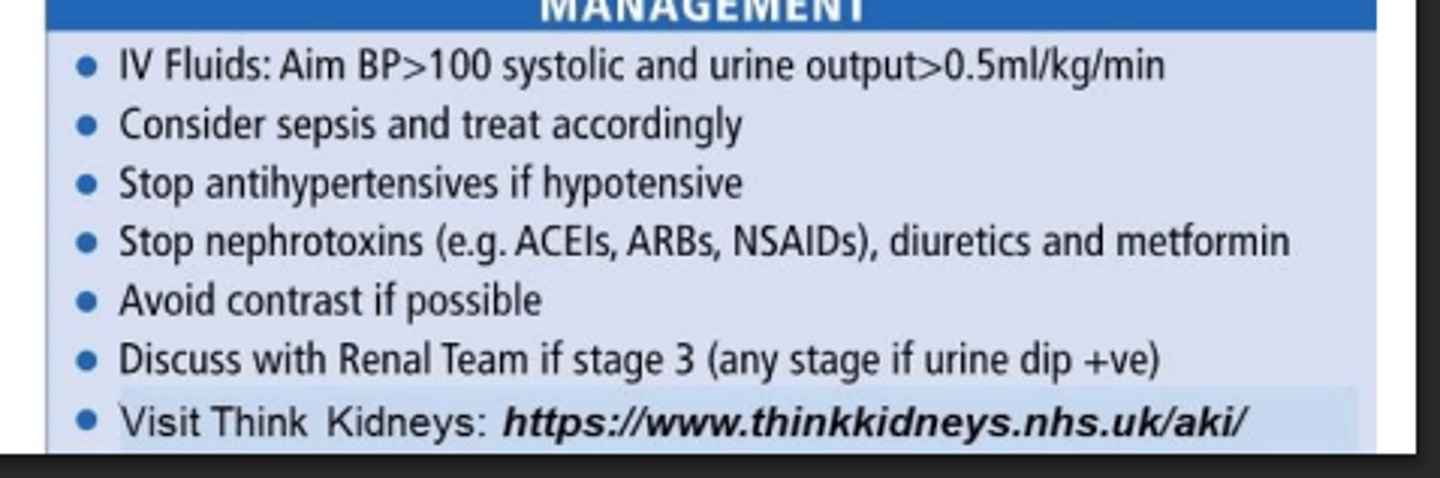
What medications need to be on HOLD stopped with an AKI?
Stop any medications that will make AKI worse
DAMN
Diuretics
ACEi/ARB
Metformin
NSAIDs
What type of CT scan should be avoided in patients with an AKI?
CT scan with contrast media/ contrast CT
Contrast media makes blood shine a bright white
It is very nephrotoxic
What are the risk factors for an AKI?
Aged 65 and over
History of AKI
CKD (eGFR <60 mL/min/1.73 m2
Urological obstruction
Chronic conditions like HF, DM, proteinuria, liver disease
neurological/cognitive impairment where need to rely on others for fluid intake leading to it being reduced
Sepsis
Hypovolemia, hypotension, dehydration, reduced fluid intake
Oliguria
Who have used specific medication within the last week (especially if hypovolaemic), NSAIDS, ACEi, ARB's, diuretics, MRA's, antibiotics (aminoglycosides)
Exposure to Iodine based contrast agents
Cancer and cancer treatment
Immunocomprimised
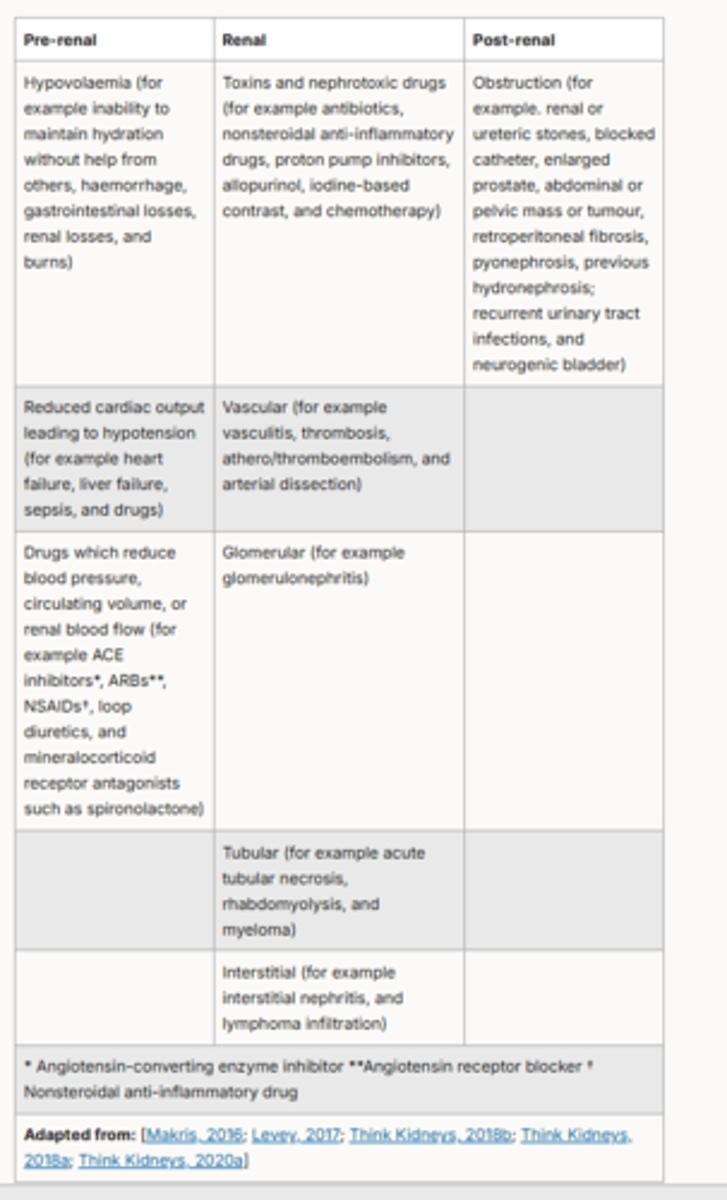
What are the causes of an AKI?
Pre-renal (most common) — due to reduced perfusion of the kidneys and/or hypotension leading to a decreased glomerular filtration rate (GFR). It is usually reversible with appropriate early treatment
Intra-renal — a consequence of structural damage to the kidney, for example, tubules, glomeruli, interstitium, and intrarenal blood vessels. It may result from persistent pre-renal or post-renal causes damaging renal cells
Post-renal (least common, accounting for around 10% of AKI) — due to acute obstruction of urine flow within the renal tract resulting in increased intratubular pressure and decreased GFR
What is an mnemonic/acronym to remember the causes of an AKI?
SHTOP
Sepsis
Hypovolaemia
Toxicity
Obstruction
Parenchymal disease
What are the stages of an AKI?
Worked out automatically from blood test, will not have to interprets this yourself
What are the investigations for an AKI?
Assess:
Fluid balance, BP, urine output, examine chest and bladder
Routine blood test, ABG, VBG
Urine dip
Arrange US is suspected obstruction or not responding to fluids
What is the management for an AKI?
Correct underlying cause
Pre-renal cause
Provide IVT resuscitation
Post-renal cause
Relieve obstruction - insert catheter?
Hold nephrotoxic
What are the two types of IV fluid, and which one is used in an AKI?
Crystalloids
Water with electrolytes
This one is used in AKI
Colloids
Large proteins suspended in fluid
Designed to draw water out of the organs
Not used in AKI
With the complication hyperkalaemia what needs to be remembered?
Normal range --> 3.6 - 5.2 mmol/L
Results in potentially fatal cardiac arrhythmias (ventricular fibrillation)
Perform ECG
Remember medications can cause HYPERkalaemia along side AKI
What is the treatment for hyperkalaemia, and why do we give each one? (6)
Nebulised salbutamol
Shifts K+ into the cell
IV fluids
PO calcium resonium
Kat ion exchange resin
Swaps potassium for calcium
IV calcium gluconate
protect the heart, stabilise the membrane to prevent arrythmia
IV insulin
Shift the K+ out of the heart
IV glucose
Give glucose to prevent hypoglycemia
What are the complications of an AKI? (5)
Hyperkalaemia
Metabolic acidosis
Fluid overload
Uraemia
CKD
What can effect the pharmacokinetics of ADME?
ABSORPTION
Impaired gut wall function
Malabsorption
DISTRIBUTION
Reduced fat tissue and lean body mass
Hypoalbuminemia and
increased concentration of alpha-1-acid glycoprotein
METABOLISM
Changed expression of
metabolizing enzymes and drug transporters
EXCRETION
Impaired renal function
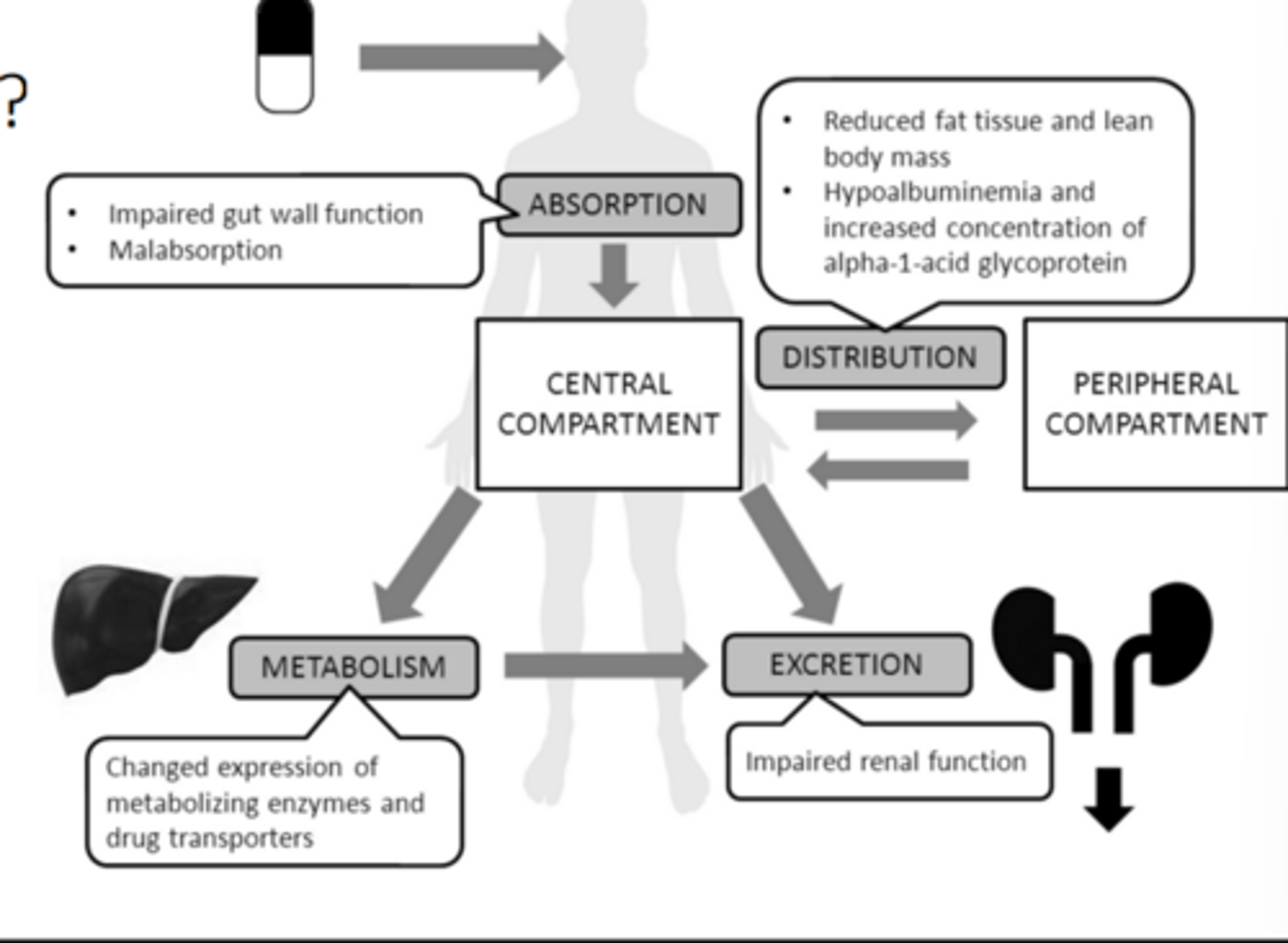
How does renal impairment change pharmacokinetics
Absorption
May be reduced due to uraemia causing nausea, vomiting, diarrhoea
Patient may be taking phosphate binders
May be affected by the increase in gastric pH
Distribution
Drug-Plasma protein binding reduced -
increased free (active) drug
Uraemia increases permeability of
BBB
Volume of distribution may be altered by changes in hydration state of patient
(e.g. increased Vd in oedema so need higher doses)
Metabolism
slower in CKD leading to increased ADRs
Vitamin D - need to use calcitriol or
alfacalcidol
Elimination
Glomerular filtration, renal tubular
secretion and resorption all reduced
Accumulation of drug/active
metabolites highly likely
Why is there special care needed with morphine in renal impairment, what would we give instead?
Used in pain (not chronic)
Metabolised in 2 different metebolism
both are renally excreted and are active
If have kidney issue, active metabolites need to be excreted by the kidney so don't leave carry on binding, risk toxicity
Oxycodone metabolised once is active, then again to be inactive, so when it accumulates, no effect
So this is the opioid given in patients with kidney damage
In cases of renal impairment what do we need to check? (2)
Both the medication and metabolites
Ensure neither toxically accumulate
What do we need to know before drug administration in renal impairment ?
• Many drugs are renally excreted
• Risk of accumulation
• Increased drug T1⁄2
• Drugs may have reduced efficacy
In renal impairment, if a patient is vit D deficient what do we need to give?
Vitamin D requires hydroxylation by the kidney to its active form; alfacalcidol and calcitriol are active metabolites of vitamin D which do not require hydroxylation by the kidney. Considerations related to the individuals renal impairment will need to be made when choosing a vitamin D product.
What are the prescribing approaches for renal impairment?
• Increase dosing interval • Decrease dose •Combination of dose reduction and increased interval
• Review drug choice
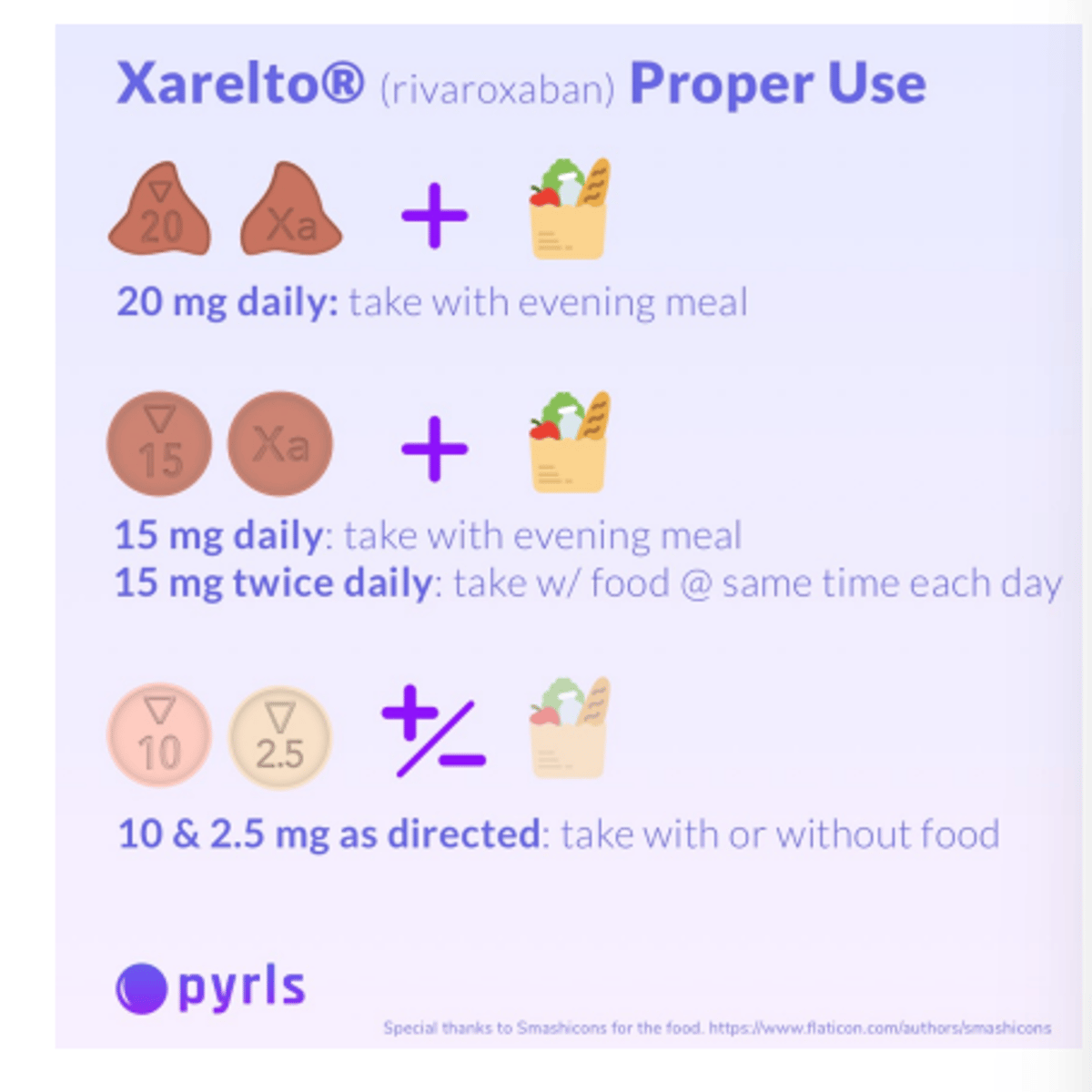
What are the rules around using DOAC's in renal disease?
CrCl should be used as an estimate of renal function for direct-acting oral anticoagulants (DOACs), and drugs with a narrow therapeutic index that are mainly renally excreted.
Has many indications - ensure you know the indication you are treating
Look at the individual rules for each medicine
E.g. Apixaban prophylaxis of stroke in AF
5mg BD
UNLESS 2 of the following 3 criteria are met:
>80 years old
<60kg or SrCr
<133micromol/L
This rule does NOT apply in treatment on DVT/PE
Should NSAIDS be used in renal impairment? Explain your answer?
Avoid if possible
inhibition of prostaglandin-induced vasodilation and can result in reduced renal blood flow and perfusion, especially those with renal disease
Why should ACEi/ ARBs be used on renal disease?
Block the effects of the renin-angiotensin-aldosterone system (RAAS), a system that regulates blood pressure and fluid balance.
They work by reducing glomerular pressure, which helps to protect the kidneys' filtering units (glomeruli).
CE inhibitors and ARBs can sometimes cause a temporary decline in kidney function, especially when first started or in patients with advanced kidney disease.
Hyperkalemia: They can also increase potassium levels in the blood (hyperkalemia), which can be dangerous.
May need to reduce dose in late stage CKD
Mr AK, 67 y/o, ♂
P/C - Fever, Cough, Mild chest pain
PMH - HTN
DHx - • Ramipril 5mg OM • Ibuprofen 400mg TDS PRN (for knee pain)
SHx - 86Kg
Investigations - Na 159mmol/L, Urea 8.9mmol/L, SrCr 397µmol/L, eGFR 20mL/min/1.73m2, WCC 8.0/mm3 , CRP 56mg/L
Ward Round • Diagnosed as LRTI - requires antibiotics • Start IV Co-amoxiclav 1.2g TDS • Start IVT • Monitor temp, FBC (infection markers)
NB - eGFR 20mL/min/1.73m2
Creatinine results - 2021 98µmol/L, 2022 91µmol/L, Today 397µmol/L
What would be the interventions?
What would you recommend on discharge?
Interventions -
Suspend nephrotoxics (ACEi and NSAID)
Amend co-amoxiclav dose interval
Monitor renal function and K+
Discharge - • Recommend swap ACEi to CCB
Recommend use of paracetamo'
Mrs CK, 85 y/o, ♀
P/C - SOB, palpitations
PMH - Hyperthyroidism
DHx - • Levothyroxine 125mcg OM • Amlodipine 10mg OM • Bendroflumethiazide 2.5mg OM
SHx - 65kg • Investigations - SrCr 149µmol/L
Ward Round •
ECG performed - AF
CHA2DS2VASC: 4
ORBIT: 2 low
Start anticoagulation
Patients preference to have ONCE DAILY preparation - Rivaroxaban 20mg OM prescribed
• CrCl = 25ml/min
What are the pharmacist intervention?
Dose reduce anticoagulant
Recommend starting β-blocker
Monitor U&Es, HR, BP
What is the difference between efferent and afferent?
Afferent: enters
Efferent : leaves