Ruminants
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
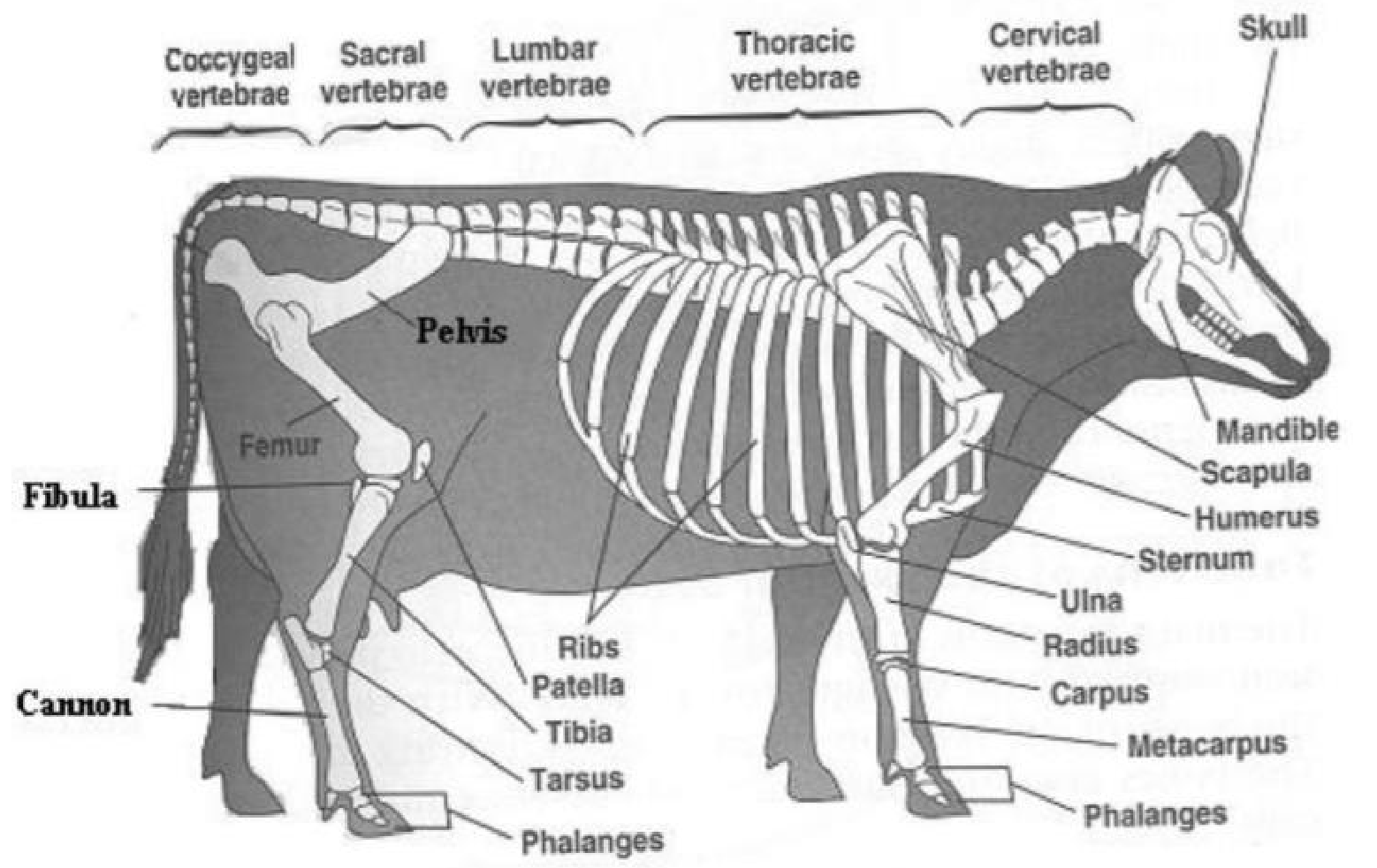
Basic Bovine Anatomy
Procedure of clinical exam of bovine
Biosecurity - x3 copies from the client, the new owner and the truck drive
education via Animal Health Australia or Emergency Animal Disease
DPI Biosecurity manual
Presenting Problem
Signalment
species, breed, age, sex
History (hard on a farm)
immediate, past, herd
Observe environment - farm and surrounding areas
Observe animal at distance
mentation, posture, gait, gross visual abnormalities
BCS = 1-5
Conformation = flat vs curved back
respiratory rate
Detailed observation of animal with restraint
Physical clinical exam of animal ± restraint
tail → head , left → right
tests = temp, pulse (tail), HR and MM + CRT (vulva)
body = contour of abdomen and BCS symmetry
Left side = thorax and abdomen + rumen
Right side = thorax and abdomen + intestines
Front = head, nasal discharge, neck
Internal = rectal exam or PD, kidneys, GIT
Diagnostics = lab, US, radiography, CT
cost vs benefit analysis
time vs benefit analysis
body systems + types of lesions
Key components of rear clinical exam of bovine
Urine collection
Females = stroke below the vulva to stimulate
Bulls = stimulate prepuce or hose with water
mid stream sample
identify colour, clarity and content
can use strips to analyse pH, ketons, cells and protein
Mucous Membranes
Colour - pink and moist
Abnormal = discharge, colour change, odour
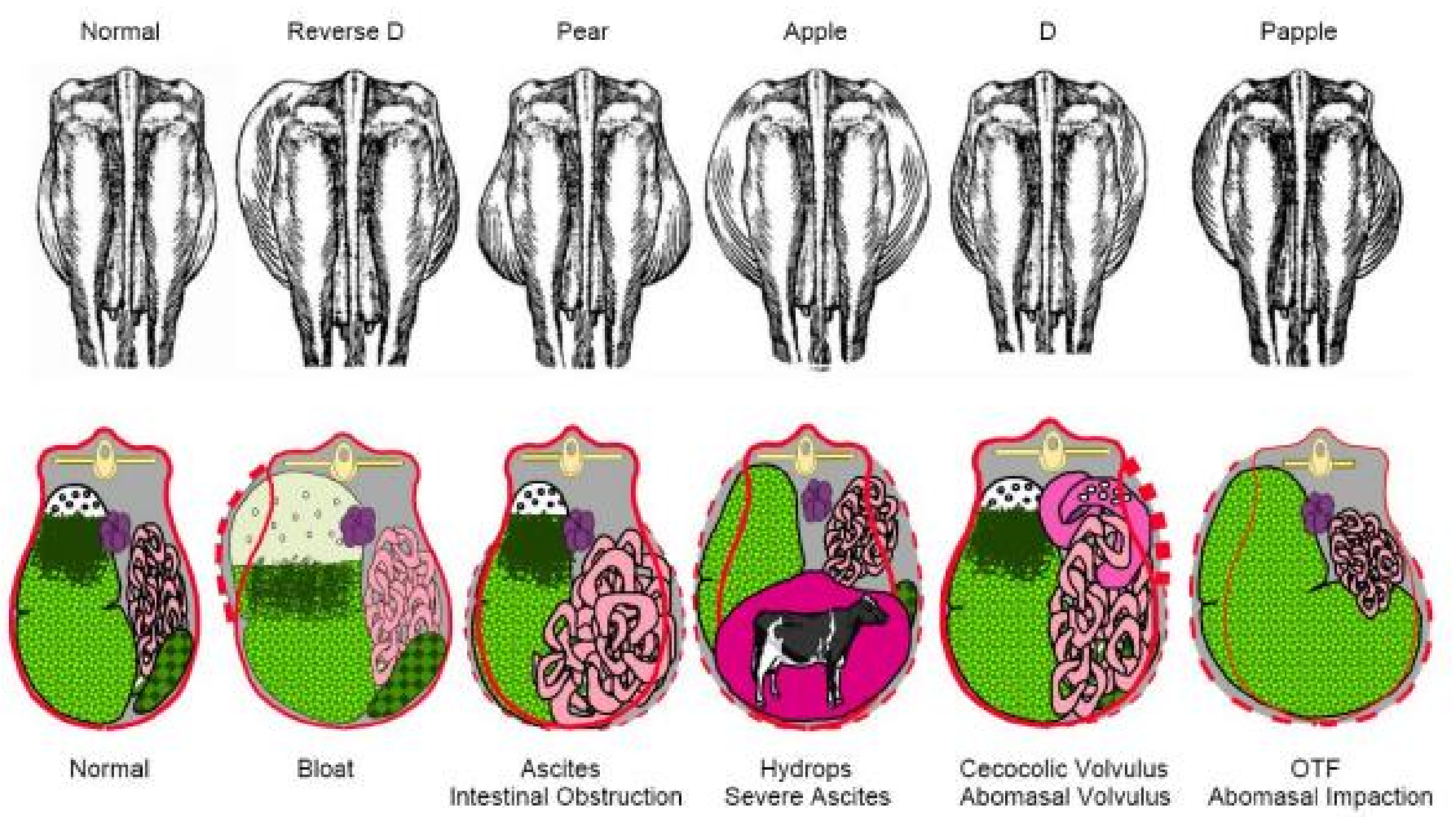
Contour of Abdomen Symmetry
Normal = symmetrical
Left flank (top left) filled = full
Left side = gas filled rumen
Bloated at base = hydrops / obstetrics
Bloated all the way around = intestine issue
Key Parameters of Bovine
Temperature = collect from anus internal wall
38.5 - 39.5 degrees
below 37 is dying
above 40 is high, but be cautious of environment → will alter respiratory rate
Pulse Rate = collect from tail
Beef = 60-80 beats per min
Dairy = 50 beats per min
Respiration
20-30 breaths per min
Rumen Contractions
1-2 per minute
Left vs Right Side of Thorax/Abdomen Exam of Bovine
Left Side
Rumen
normal = contract 1-2 per minute
feel in the paralumbar fossa (triangle dorsal sac of rumen)
measure intensity, duration and frequency of primary (food) and secondary (gas movement) cycle contraction
can be palpated / ballot rumen (sick = won’t feel)
can percuss and auscultate reticulum
gas filled viscera (LDA/RDA) → PING or basketball on concrete
gas filled rumen → PUNG
rumen atony and collapse
ruminal distension
pneumoperitoneum
more fibrous = sound scratchy
gas gap (top third), rumen, fibrous mat (doughy/water bed), fluid (bottom)
Right Side
Caecum
Intestines
possible displaced abomasum
Left + Right
Lymph nodes (pre-femoral and pre-scapular or submandibula)
Thorax → quiet is normal
Respiratory organs (rate and crackles/wheeze) → stethoscope
x2 ribs from the back, then down to elbow
if extended neck = lung issue
Cardiac system (rate, rhythm, murmurs) → stethoscope + palpate
Foot conformation
Parameters + key examination for sheep/goats
Teeth = total divide 2 is roughly age (remember milk teeth)
BCS
Heart Rate / Pulse = femoral artery or heart auscultation → 70-80 bpm
Respiratory Rate = distance → 12-20 bpm
Lymph Nodes = submandibular
MM + CRT = FAMACHA score of 1 or 2 is normal (/5)→ pink and moist
Temperature = 38.5-40 degrees
Rumen contractions = 2 per minute
Fleece + skin
Feet and musculoskeletal
foot rot and lameness is very common
Thorax + Abdomen = loud is normal in sheep
Reproductive
Preventative health
Recent husbandry
Footrot vs Heel Abscess vs Toe Abscess
Footrot | Heel Abscess | Toe Abscess |
|
|
|
Cheesy Gland
Cheesy Gland = casous lymphadenitis or Corynebacterium pseudotuberculosis
abscesses in lymph nodes around body
effects sheep
wide spread post shearing
dipping post shearing increases risk (open wounds)
large loss to meat industry (doen’t really effect wool)
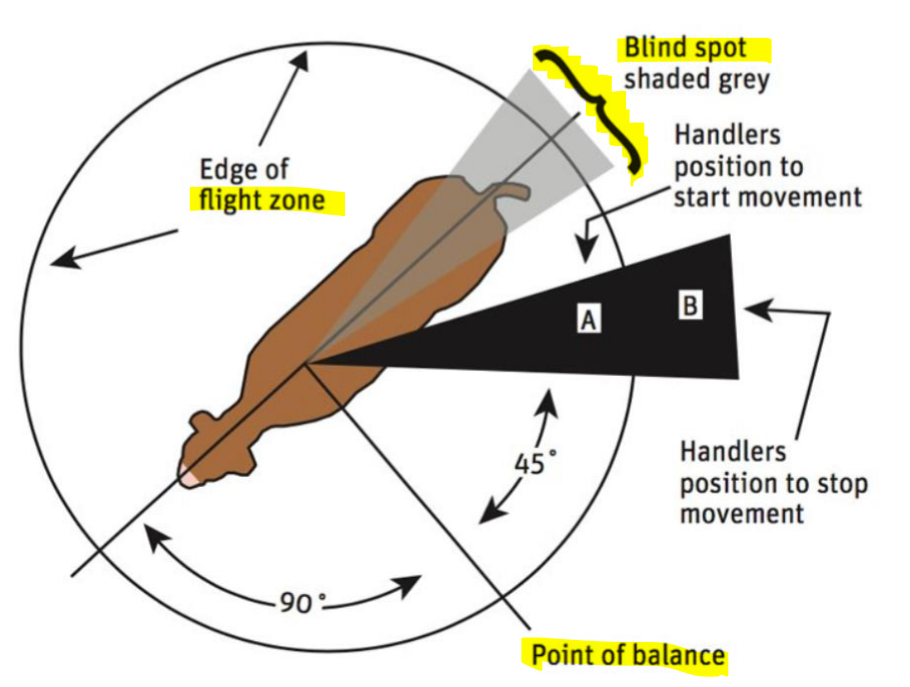
Safe Cattle Handling
People → Animals → Equipment
Use point of balance to move cattle in a low stress stock handling
Cows have 320 degrees of vision
point of balance is at 90 from front
blind spot directly behind
move the front animal first and the others will follow
as handler moves forward, past each post of balance they will all move
Anaesthetic and Analgesia for disbudding, dehorning and castration of cattle + sheep
improve welfare and quicker recover
not legally required in young calves
Meloxicam = injectable, easy, expensive
Bucccalgesia = oral, hard (takes 10-15 mins to work = catch sheep x2)
TriSolfen = spray on after procedure, easy and cheap
local anaesthetic and antiseptic
best oncalves 6-8 weeks
Explain disbudding vs dehorning in both calves and kids
Disbudding | Dehorning |
|
|
improves safety for humans and animals (also their welfare)
improve meat quality and reduce bruising
do not give food 3 hours before procedure
must be in good health prior to surgery
ideally castrate males at the time time
Calves
very common - less than 2 months
polled gene is breeding against horn / reduce growth and need to dehorn
anaesthesia + pain relief (xylazine + lignocaine to cornual nerve)
NSAID = meloxicam
tools
disbudding knife (under 2 months)
scoop dehorners (2-6 months)
cup dehorners (2-6 months)
horn saw (6+ months)
gullotine or tippers (6+ months)
foetotomy wire = last option
keep calves sternal post procedure
Kids
very common - 1-2 weeks old
local anaesthesia and sedation (xylazine) + cornual nerve block
NSAID = meloxicam
tools = surgical, cyrosurgery or heat cautery (heat → risk brain necrosis)
Explain castration
prevent undesired bull calves from breeding - breeding control or improving genetics
behaviour control = easier to handle, less injuries, less property damage
meat quality = more tender, lower glucose and more connective tissue
under 6 months = legal to do with or without GA
over 6 months = illegal to castrate
Surgical | Non-Surgical |
Scalpel + emasculator
Henderson tool
| Elastrator Rings
Burdizzo (not common)
|
Clostridial Diseases
Pulpy Kidney (enterotxaemia)
sudden change in young lambs feeding on fresh pasture or grain
usually young, fast growing animals
bacteria and toxic
sudden death
Tetanus
poor hygiene from from castration or banding
wounds from penetrating things, foot trimming, dog bites, dehorning
stiff leg gait → convulsions → sore horse
treat with antitoxin ($$ low survival change) or prevent
Black leg
gas under skin → crackles → muscle bruising
common in young calves, uncommon in sheep
very depressed, abdominal pain → sudden death
Black disease
liver fluke infection → liver damage = bacteria + toxin
common in rams
very depressed, abdominal pain → sudden death
Malignant Oedema
contaminated wounds post shearing, mulesing, castration
lambing
local swelling + depressed with fever → death
Leptospirosis
zoonotic disease
spirochaete is infected in urine and abortion material
enter via skin abrasion / mucosa → lymphatics → liver → bacteria
sheds and contaminates environment for long time
antibodies can clear the pathogen
in utero → cause abortion, still birth or premature/weak calves
Signs
abortion
fever
kidney and liver damage
decreased milk production
acute or systemic disease
Treatment
often too late
Antibiotics = Oxytetracycline or amoxycillin + fluids or transfusion
Vaccination = ideal prevention
Control environmental disks - zoonotic!
Botulism
due to phosphorus deficiency
pica (eat things that aren’t usually food) → will chew on bones to try and help (also bad)
contaminated or spoiled feed
due to eating animal carcasses, rotting animal material or poor silage
Signs
low growth rate + poor reproduction
hindlimb weakness → paralysis
down but alert so unable to rise = death
Prevent = annual or every 3 year vaccine
Pink Eye
kerato conjunctivitis
effects 80% of herd, in one or two eyes = blindness
pink or cloudy eye
Treatment
sew eyelid shut for a week to allow for healing
prevent with vaccination 3-6 weeks prior to pink eye season
control flies - insecticidal ear tags, remove rotting food, limit dust
Tick Fever
Vector = Bebesia Bovis, Babesia bigemina and Anaplasma marginale + Theileria
egg on grass → larvae + nymph → adults create eggs leave in faeces
one host tick (Bush Tick)
all over Southern Aus coastline
5% mortality but very high morbidity
reduced BCS, growth rate, milk production, fertility
cannot be sold or exported = withholding periods post all treatment
B. bovis | B. bigemina | Anaplasmosis |
|
|
|
|
|
|
Treatment Babesiois = Imidocarb, NSAIDS to reduce fever, supportive care ± transfusion
Treatment Anaplasmosis = Tetracyline or Imidocarb
Prevention for all = single vaccination
Bovine Ephemeral Fever (BEF)
3 day sickness
transmitted by mosquitoes and biting midges
effects bulls, pregnant/lactating cows, well conditioned cattle, during wet season
Signs
high fever → will stand in the dam to cool off
lameness and recumbency → death
muscle twitching
drop in milk production
abortion
Prevention = vaccination 2-4 weeks apart before Spring
Treatment = NSAIDS (meloxicam) and calcium
Restrain in ruminants
Physical restraint
Chemical restraint
Xylazine (most common in bovine, avoid in sheep)
Diazepam (in sheep for short periods)
Blood collection and fluid nursing
Jugular = large volume
Coccygeal (tail) = small volume
Arterial vein = blood gas
Subcutaneous abdominal (milk vein) = rate
Red top = most common → clotting factor = 2, 4, 10ml
Purple top = EDTA = 2, 4, 10ml
Green top = Lith hep = 4ml
Cattle: IV Hypertonic Saline at 4ml/kg → immediately after give oral fluids via frick speculum, pump, tubing or buckets of medications
Small Ruminants: IV fluids via cephalic vein of 0.9% NaCl
Hydration and Azotaemia= 2ml/kg/hr
Hyokalaemia is common = max 10-40 mEg
Neonate maintenance = 4mll/kg/hr
Hypoglycaemia common in neonates = max 50% dextrose
Downer Cow
Main Causes:
Mastitis → open teats + dirty enviro causing infection
Metritis → post birth infected uterus
Major Sepsis → secondary metritis
Metabolic
Musculoskeletal or neurological → lame, infection, dislocated hip
Nursing Care
improve environment = warmth, shelter, soft bedding
posture = sternal recumbency (prevent bloating), lift daily and move
fresh water daily
hand strip milk from udder
Surgery in the field
clippers, surgical prep solutions in buckets
surgical instruments, suture material, flush
post surgical antibiotics and topical treatments
aseptic as possible = clip, water scrub with nail brush, surgical prep
Sedation = lignocaine (ideal) or xylazine (low dose/avoid for standing procedures)
Blocks = L block (flank, paravertebral , epidural, cornual nerve block, ring block)
Urinary Blockage
Obstructions is urethral process, distal sigmoid flexure or bladder
most common in early castrated male goats
Stone types
Phosphatic stones = sandy (due to high grain and pellets diet)
Calcium carbonate = hard (due to high alfalfa and legume diet)
Symptoms = straining, vocalising, sawhorse/wide stance, anuria, anorexia, lethargy, recumbency
Treatment
blood test - check biochemistry, balance electrolytes
anti-inflammatory, analgesics and fluids
urinary acidification + diet change for x2 weeks (dissolve stones
prone to recurrence → surgery
urethral amputation = cheap surgery in field
cystotomy = expensive hospital procedure to drain + stitch
Prevention = prevent infection by castrated at 3 months old
Causes, signs and treatment for an anaemic small ruminant
Causes:
Blood loss = trauma, endoparasites, ectoparasites
Haemolysis = leptospirosis (zoonotic), clostridial infections, chronic copper toxicosis
Decreased Erythrocytes = Johne’s disease (notifiable), Lymphoma, Neoplasia
Clinical Signs:
pale MM → low FAMACHA score and PCV
weakness, lethargy
tachycardia and tachypnoea
Treatment:
Whole RBCs = cheap, easy, replaces all components, good for haemorrhaging
Fresh Frozen Plasma = expensive, great for failure passive transfer, hypoproteinaemia, oncotic support, great in food producing animals
Packed RBC = normovolaemic anaemic patient, avoid in food producing animals
Serum = limited research
Blood collection and transfusion for small ruminants
Collection from the donor:
minimise risk of reaction
minimise risk of transmissible disease
decrease stress (bring a friend)
can donate 20% circulating blood volume = 10-15ml/kg of body weight = 450ml
lignocaine → prime T port and tape in place → take sample → heparinized flush
Administration:
first transfusion is low risk, but ideal to blood type before - go slow
acute haemorrhagic shock = replace 50% of the estimated loss
chronic = (desired PCV% - recipient PCV%)/ donor PCV% x recipient weight x 0.08
delivery
Initial = 1ml/kg/hr
Monitor vitals every 5 mins
Increase to 10-20 ml/kg/hr after 20 mins if no adverse reactions
SE (rare)
| Treatment for SE
|
Reproduction industry and expectations
1 calf per cow per year = goal for beef and dairy
repro performance of dairy cow have been increasing since 2000
reproduction inefficiency is that main reason cows are culled
ideally balance each cows milk production and reproduction to be equally efficient, successful and profitable
Calving → 1st insemination <70 days → conception = >50-60%
Good heifers will calve by 24 months
Lactation = 305 days
Dry Period = 60 days
Abortions are very rare, only <3%
Explain the reproduction/oestrus cycle of bovine
Calving interval = 365 days (x1 calf per cow per year)
Gestation = 285 days or 9 months
Uterine involution (shrinking) = 35-40 days
Ovarian cycle = up to 60 days
development of postpartum disease (dystocia, retained placenta, urinary infection, metabolic disorders) will delay uterine involution and ovarian cyclicity
negative energy balance impacts post partum uterine involution = high milk production despite low feed intake
Oestrus Cycle = 21 days:
Day 1-3 = Met-oestrus
FSH → start follicular wave then subsides
Day 3-14 = Dioestrus (progesterone at highest)
Dominant follicle is LH dependant
CL produces progesterone
PGF (prostaglandin) breaks down CL = called luteolysis as it prepares for next follicular wave
Day 14-16 = Proestrus
increasing in oestrogen to prepare for ovulation
Day 16-18 = Oestrus
peak in oestrogen
peak in LH
Day 18-20 = Met-oestrus
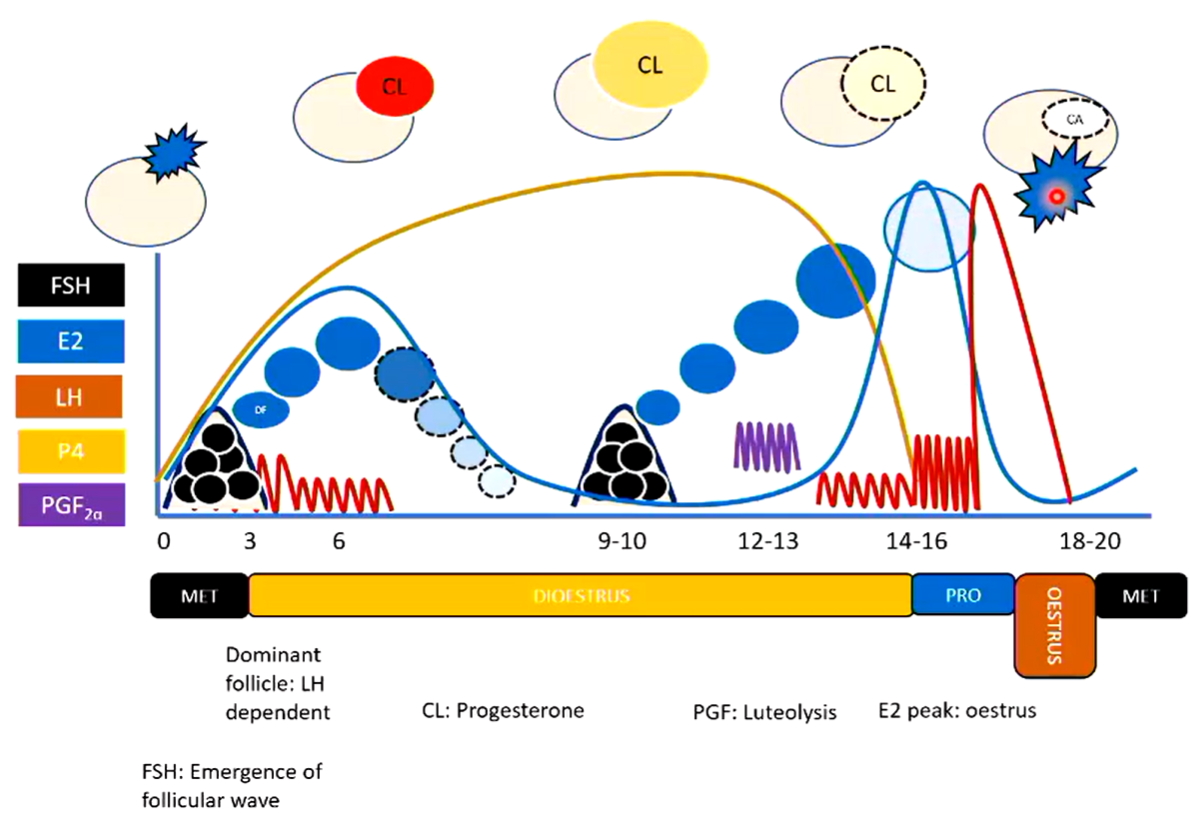
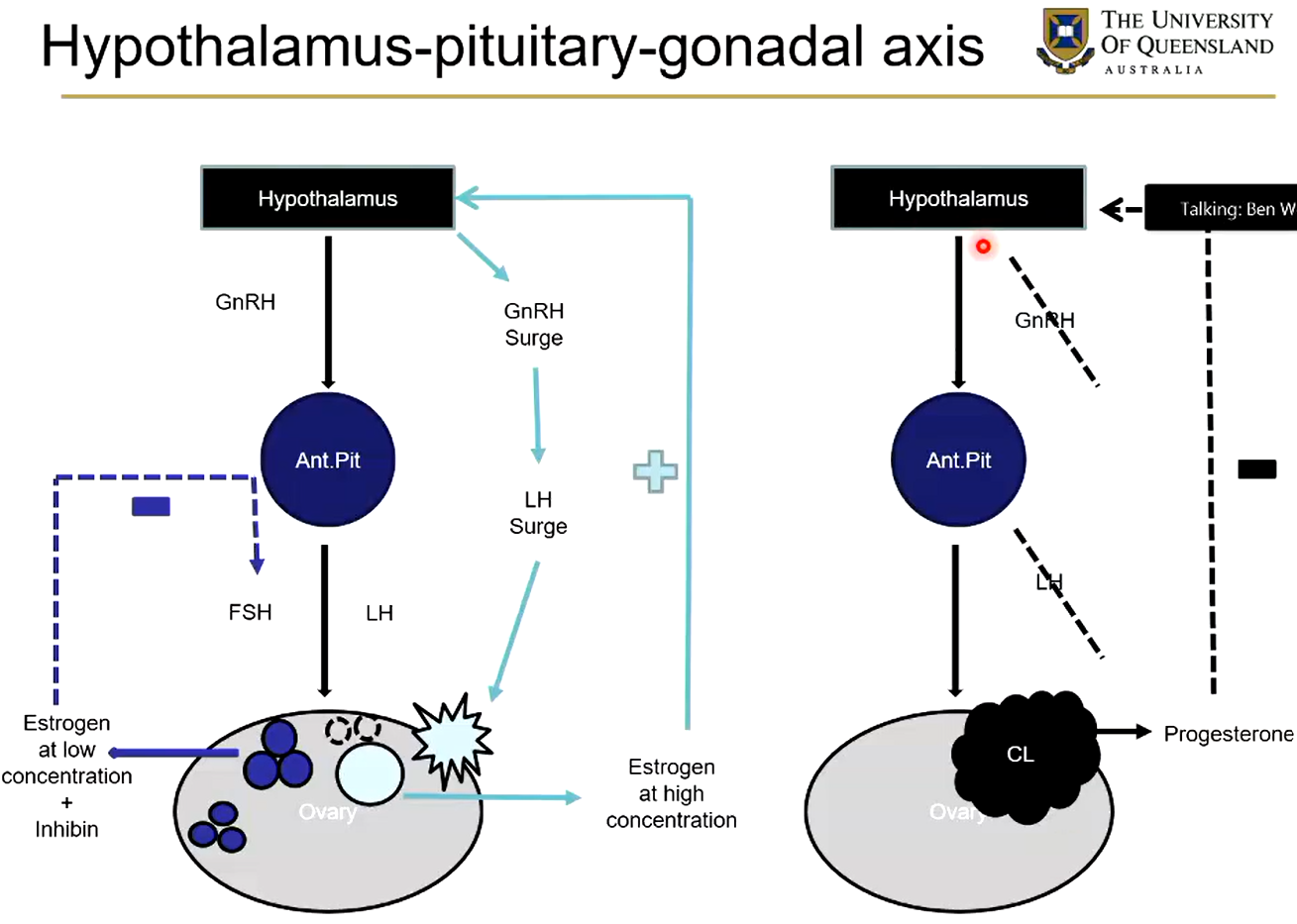
Explain the hypothalamus pituitary gonadal axis
Hypothalamus → GnRH (gonadotropin releasing hormone) to the anterior pituitary
Anterior pituitary releases FSH (follicle stimulating hormone) and LH (luteinising hormone) = effects ovary
follicles continually develop in the ovary which secrete small amounts of oestrogen and inhibin → negative feedback loop on FSH (self regulates)
If a dominant follicle grows → lots of oestrogen = positive feedback loop on Hypothalamus to release lots of GnRH → lots of LH = ovulation
Ovulation produces a CL (corpus luteum)
CL produces progesterone (maintenance hormone for pregnancy → negative feedback loop on hypothalamus to inhibit GnRH production
Therefore: can use prostaglandin (PGF) to cause death in corpus luteum (leutolysis) and hence bring cow back into cycle for next pregnancy
How can you detect oestrus?
Behaviour
cow have wide stand waiting to be mounted
occurs 3 time per day - morning, lunch, night each for 20-30 minutes
AI usually follows traditional timings to
Mount Detectors: small heat patch stuck to cow and will change colour if increase in heat → will occur from mounting other cows
Activity Monitors: pedometer (steps) or a collar (measure rumination → ready to mount)
Ultrasonography:
foetal viability, age, number and gender
early as 28-30 days of gestation
Rectal palpation:
used in dairy and beef cows (not small ruminants)
do during 35-45 days of gestation
traditional method = cheap
Explain oestrus synchronisation vs Timed AI and the advantages/disadvantages
Oestrus Synchronisation: CIDR device used to release hormones into cattle
inseminate during the 2-5 days of oestrus detection (after PGF hormone)
can be used to mimic the luteal phase
Advantages | Disadvantages |
|
|
Timed AI: can be done at the same time as AI to be during the 24-32 hours of ovulation
Doing both Ovisynch and Timed AI
excellent farm management - repro, nutrition and herd health
animal identification → inject right cow at right time
good recording keeping to time hormonal administrations and AI
Advantages | Disadvantages |
|
|
Natural service vs AI, and the advantage/disadvantages
Advantages | Disadvantages | |
Natural Service (mostly bulls) |
|
|
Artificial Insemination (AI) |
|
|
Veneral Diseases (Tritichomonas foetus)
extracellular protozoan parasite found in bovine breeder cows which cause:
abnormal pregnancy diagnosis results
prolonged calving intervals in females = only clinical signs
disease is asymptomatic
disease has not vaccine in Australia
often occurs in very dry and dusty environments
collect semen sample using a Tricamper or a “Pizzle Stick”
can detect parasite in a direct culture or smear
PCR can be used
Bovine Venereal Campylobacteriosis (Vibriosis) can be given to help control veneral bacterium
Bull Breeding Soundness Exam (BBSE)
BBSE = quick and cheap screening test of bulls (NOT a fertility test) that assesses the risk of reproductive failure
serving capacity / ability test
not common
assess libido, mounting behaviour and ability to serve within 20 minutes (0-1 = low, 2-3 = medium, 4 = high)
general physical and clinical exam
BCS, leg/foot confirmation, gait, head, eyes, dentition
scrotal circumference and reproductive tract (external and internal)
scrotal tape = measures puberty cycle
heritable - minimal requirements depending on breed
collect semen and evaluate motility
transrectal massage
artificial vagina
electroejaculation
evaluate volume, colour, motility, live vs dead, morphology
Result of BSSE
Tick (ACV standard approved)
Cross (not ACV standard approved)
Q (qualitified but not completely ACV standard)
NT (not evaluated or meet ACV standard)
Fertile = will impregnate 60% after 3 weeks, and 90% after 9 weeks of health females
Sub-fertile = impregnate females by natural service, but not at the rate of fertile males
Infertile = unable to impregnate females
In-vivo vs In-vitro embryo reproduction
In-Vivo
| In-Vitro
| |
Pro's |
|
|
Reasons for failures =
poor nutrition
heat stress
reproductive disease
poor breeding soundness
poor reproductive management
genetic congenital abnormalities
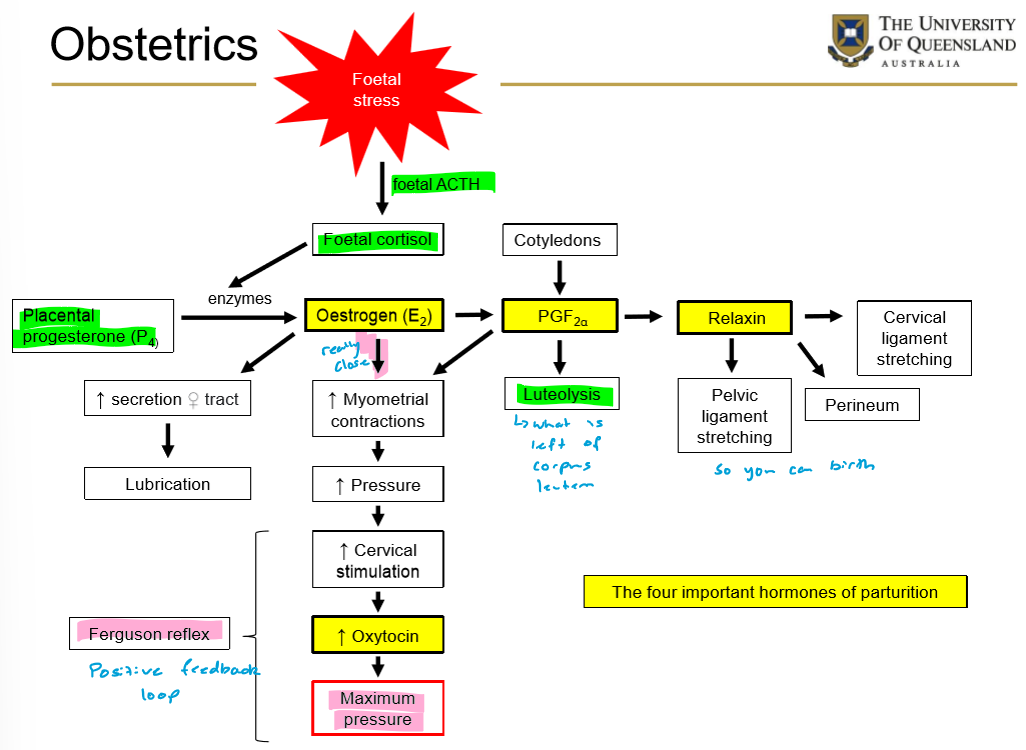
Important Hormones in Bovine Parturition
Prostaglandin (PGF2a) → Endometrium
luteolysis = break down corpus luteum
soften cervix
make myometrium sensible
initiate oxytocin release
Oestrogen → Development of mammary gland
oxytocin receptor increases
release cervical seal
soften cervix
increase secretion of mucous for smooth delivery
Relaxin → Ovary
increase elasticity in pelvis ligaments (rump will drop)
soft the cervix
stimulate mammary gland
decrease tonus in uterus
Oxytocin → posterior pituitary
maximum pressure
myometrial contractions
stimulate mammy gland
can also be used post calving to contract uterus
3 Stages of Bovine Parturition
Stage 1 = 6-12 hours
uterine contractions begin
cervical dilation
will be restless and separate from the herd = increase HR
foetus will be getting into position so cow is very pressure sensitive
water bag / amniotic sac expelled = clear/yellow
Stage 2 = <2 hours
uterine contractions increase
foetus enters birth canal = head + thorax ideal to prevent mum getting hip lock
calf delivery = heifers will take longer than cows
check for tares and spares
Stage 3 = 2-8 hours
afterbirth / placenta delivered → always allow it to come out naturally so you don’t break it → systemic infection
retained foetal membrane (24hrs +) is very smelly
contractions and epithelium weaken
calve suckling → oxytocin release for mum
all in all out systems, good nutrition + hygiene, vaccinations = herd health
Methods to assist birthing
crush with a kick gate OR ropes to cast animal/ and tie to a tree or to get to ground
lubricant and gloves
always need to have head engaged
eponychium = hoof capsule slippers to protect uterus and canal
disinfectant (iodine or chlorhex) in a bucket to soak after
chains on foetus above and below fetlock
calving jack, pulleys or ropes
head snare (lasso to put around head/into mouth) or eye hooks
epidural anaesthesia = 1ml/100kg of lignocaine (1hr
ensure correct position and pulling → push back in and readjust position
rotate the calves hips 90 to get through cow pelvis
pull calf one leg at a time to reduce width of shoulders
anterior = head + front hooves down = 96%
posterior = hind hooves up = 4%
always check presentation = tongue , eye, hoof or rectum reflex
only caesarean if head is not engaging with legs or after 15-20 mins no progress
if calf is dead, can cut it up inside and pull out in pieces
Ewes and Dose
30mins to 2 hours
use ropes not chains
usually twins so need to birth individually
always check for tears and spares
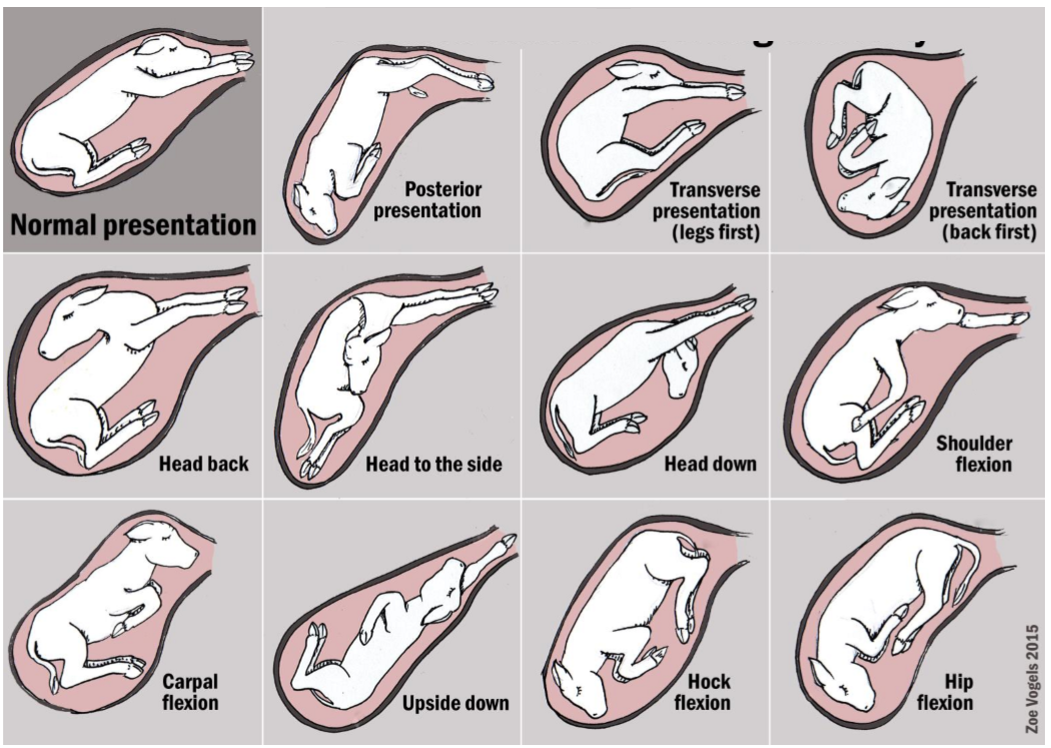
Types of dystocia / incorrect birthing positions
Head down = front hooves first but head is down
Head to side = front hooves first but head to side (easy to decapitate)
Bilateral Flexion
Breech = hip and hock flexion (ball with back end facing out)
bring hind legs up but keep hand over hooves to protect uterus
push hind legs forward then bend stifle and hock
Carpal or shoulder flexion = head first but front legs flexed
put hand down and bend legs up, keep hands over hooves to protect uterus
Unilateral Flexion
push back in and reach for second leg
ensure head is still engaged
Twins = focus on what anatomy can be felt and the way legs are bending
Front leg fetlock + knee bend in same direction
Back leg fetlock and hock bend in opposite directions
Complications in Birthing
Uterine prolapse
20 mins post calving → if not fixed can pull bladder out = infection
the longer the uterus is out, the more blood it fills with = harder to get in
use hip lifters or put them in frog leg to push rumen forward/ allow space
may require an arm extender (wine bottle) to push back in
use saline or iodine to wash + biohazard bag to lift up uterus, use gravity
can put sugar on uterus to withdraw moisture + size
epidural
can give oxytocin to induce contractions + pull back in
may need antibiotics and/or NSAIDS
usually associated with hypocalcaemia and difficult calving
always give 4 in 1 vaccine post
Vaginal Prolapse
must cull cow after birth as not viable to birth again
epidural → clean and debride → lubricate and replace → Buhner suture
Buhner Suture → subcut tie ventral to vulva used to hold uterus in post prolapse
Foetus Fractures → if too much forced used or difficult calving
Haemorrhage → torn artery during birth, good prognosis
Pelvic Fat Rupture → only if high BCS, clean and check
Calving Paralysis → assist lifting and standing / physio post birth so not recumbent
Calf parameters + resuscitation
Heart Rate
Normal = 100-200 bpm
If <80 bpm = stress, hypoxia, acidosis
if <50 bpm = adrenaline, intubate and ventilate
Respiratory Rate
Normal = 20-40 per minute/ <30 seconds, active and spontaneous
if irregular or <10 bpm = doxapram
if not spontaneous = intubate and dexamethasone
Position
Normal = sternal recumbency by 5-10 mins, responds to stimulation
if unable to remain sternal within 10mins = CNC hypoxia or oedema
Resuscitation
vigorous stimulation of body with a towel
nasopharyngeal stimulation
suction nasal passage and oropharynx
intubate with a 6-8mm ET tube
Oxygen
Colostrum/ Colostrum Banking and Failure of Passive Transfer
Colostrum = first milk post calving, contains immunoglobins, total solids, very high in vitamins (A, D, E), high in iron, Calcium , Phosphorus, Magnesium
within 24 hrs = 10% of bodyweight in colostrum in first 6 hours of life, over x2 doses
there is no placental transfer of Ig during gestation → must all be after
no proteolytic enzymes = prevent clotting
high pH in small intestine
Quality measured using
Brix refractometer = >30%
Specific Gravity = 1.050 +
Colostrum metre = IgG conc >80g/L
Bacterial contamination = TPP <100,000 and TCC <10,000
Risk factors of low quality/failure
mum is too quick to return to milking
leaking of Ig prior to parturition
breed dependant
systemic illness
adverse weather
Failure of Passive Transfer (FPT)
serum of IgG is below 10 mg/ml (need 3-5 L total)
very common
directly measure = radial immunodiffusion or ELISA
indirect measure
total serum tolids / tootal protein = sample 8-12 calves, 1-7 days old
GGT ($$) = high levels of colostrum for parallel transfer, up to 10 days old
Colostrum Banking
wash and dry udder
feed to calf instantly or refrigerate
Short term = fridge IgG for 2 days or if adding potassium up to 7 days
Long term = freeze for 6-12 months, defrosted in warm water bath at 49 degrees
Calf Digestion Tract + Feeding
0-3 weeks = Born monogastric
abomasum is 70-80% of the volume (1.5 L)
unable to digest cellulose
3 weeks - weaning = Transition
rumen pH rises slowly → pH = 6 by 10 weeks
protozoal collonisation + microbial fermentation of cellulose
Ruminant Phase
rumen expands to 25-30 L by 12 weeks
energy utilisation from rumination increases efficiency
cow will feed x2 per day
lamb will feed x6 per day
Neonatal Diarrhoea + Estimating dehydration
neonatal calf = <1 month
multifactorial and multi pathogen diarrhoea
Nutritional deficiency = lack of osmosis
Hypersecretory = E coli, salmonella, coccidia
Malabsorptive = damage to enterocytes viral + protozoal + inflam
Lack of clostridium
Coronavirus
always assume
hyponatremia (low sodium), hypoglycaemia (low glucose)
hyperkalaemia (high K)
potentially hypochloraemia (low chloride)
most common cause of pre-weaning mortality and morbidity = big economic loss
protect disease spread and ensure adequate nutrition with calf hutches
may need antibiotics = amoxicillin, ampicillin, TMS, ceftiofur, oxytetracycline
Estimating Dehydration
Normal/Mild | Moderate | Severe | |
Hydration | 0-4% | 5-8% | 9+ |
Demeanour | Normal, standing | Depressed, dopey, weak | Depressed, comatose, flat, no response |
MM | Pink, moist | Pale, tacky | Pale, dry, cold |
Eye Recession | None, bright | 2-4mm, slight | 4+ mm, significant |
Skin Tent | 1-4 seconds | 3-5 seconds | 6+ seconds |
Urine pH | >6.5 | 6-6.4 | <6.0 |
Suckle Reflex | Strong | Weak | None |
Action | Oral Fluids | Oral, IV or Sub Cut | IV |
Estimating Dehydration
Maintenance = 100 ml/kg/day
Ongoing losses of 1-4 L through scours will need replacement
replace half of deficit in 6 hours
replace balance over next 12-24 hours
Estimating Base Deficit (loss through scours) = Negative Base x Weight (kg) x 0.5
Pros | Cons | |
Oral
|
|
|
IV
|
|
|
Enzootic Calf Pneumonia = Lower Respiratory Disease
age specific - only calves = 2-10 weeks old, up to 6 months
can hear lungs crackling
infection in bronchopneumonia due to viral, host immunity, enviro or pathogen
high morbidity and viral mortality
dairy calves get it more than beef
more susceptible if housed indoors than outdoors (less fresh air)
Mastitis - what is it, pathogens, transmission and clinical signs
Udder = x4 quarters, x4 teats, risk of suspension (older → stretches → risk of infection)
Teat Defence = skin, canal, keratin plug when not milking, sphincter at end of teat
Udder Defence
lactoferrin - binds bacteria cells to stop repro
Immunoglobulins = in colostrum
cellular response = somatic cell counts (SCC - low is good 150-200)
inflammatory response
Types of Mastitis:
Contagious | Environment |
|
|
|
|
Clinical Signs
Down cow
abnormal milk = watery, clear, serum, bloody, flakes, clots
abnormal udder
acute = sudden onset, systemic illness (fever, high HR/RR), low milk production, may be recumbent and dehydrated. Udder is red, swollen, hard, changed milk colour
subclinical = udder and milk is normal, increased SCC (must culture for diagnosis), decreased milk production and quality
Explain the Dry Period and how that leads to mastitis and hyperkeratosis
Dry Period
Drying off = no milk production, teat canal changes, less frequent observation from farmers, changing immune system
Dry period = low chance of mastitis
Transition Period = protective factors are diluted, teat canal keratin plug breaks down causing leaking
Involution = not milks due to high risk of mastitis
Full Involuted = resistant to mastitis, high WBC and lactoferrin levels
Teat End Hyperkeratosis
score teat end from 1-5
1 = no ring, smooth, normal teat after lactation
2 = slightly rough ring
3 = rough ring
4 = very rough ring
5 = open lesions and scabs
risk factors = pointy teats, older, high production, slow milkers, over milking, high vacuumed cups
Milking Machine = increases exposure to bacteria, but decreases resistance. May change anatomy of teat
Mastitis - risk factors and how to diagnose
Mastitis Risk Factors
Age and parity (number of calves delivered, older = higher chance)
stage of lactation
udder and tear structure (older = stretched = higher chance)
hygiene of milkers and pasture/stalls
stockmanship and low stress environment
Rapid Mastitis Test (RMT or CMT)
2-3 squirts of milk from each quarter into each of the paddles
observe gross changes in milk against blue
tilt paddle 45 degrees, pour off excess milk so equal in each
add equal parts of RMT (reagentto milk) and swirl/rock paddle to mix for 10-15 secs
while swirling watch for change
Negative = normal, so no change in milk
Positive = higher SCC, will form thicker slime or egg white consistency
Bacteria Culture
wearing gloves, brush away dirt from iodine and dip in diluted iodine for 30 secs
dry each teat with a paper towel
individually scrub each teat with 70-80% ethyl alcohol
collect a 3-5 ml sample aseptically
label, fridge and send to lab for culture
Mastitis - treatment, control and prevention
Treatment
Lactating cow therapy
intramammary treatment = more common
parenteral treatment = beef > diary
Dry cow therapy
prevents spread of infection
restore productivity
prevent mastitis and development of disease
reduce recurrence and carriers of disease
avoid long term udder damage
Antibiotic therapy
rapid and high elimination of bacteria
low likelihood of recurrent infections
reduces extent of drop in milk production
fast return of normal SCC
Control + Prevent → Aim = reduce farm level SCC
Obtain individual cow SCC → cull if persistently high or treat all
Improve milking practice → gloves, detect early, disinfectant
Minimise Enviro → clead udders pre milking, check regular, stand for 30mins post milking to allow teat to seal again, clean dry bedding
Ketosis - what is it, risk factors and prevention strategies
increase in vascular ketone bones (acetoacetate, acetone, beta-hydroxy butyrate)
disorder of the energy metabolism in will conditioned cows
nearly all dairy cows have after calving
Clinical Signs
drop in BCS
decreased appetite
drop in milk production
odour of acetone in bread
abnormal behaviour
Diagnosis
Blood test to measure BHB
Urine test to measure acetoacetate
Treatment
restore energy metabolism
oral propylene glycol - 250 ml x2 per day then 300ml once per day for 5 days
rapid IV 50% dextrose solution
Hypocalcaemia - what is it, risk factors and treatment
low blood calcium (normal blood calcium = 8.5-10 mg/dl)
also known as parturient paresis
most susceptible during 3-7th calf - either pre, during or post parturition
due to bone resorption, kidney/gut absorption, issues with NS, muscles → seizure
Signs
prolonged sternal recumbency / downer cow
depressed
lateral kind in neck and head turned to flank
high HR
weak or absent rumen contractions
secondary bloat (increase in fluid but can’t burp)
low temperature
Treatment
4 in 1 vaccine (includes calcium)
increase BCS (will have lost weight whilst down + calving paralysis)
IV or Oral calcium boroguconate + supplements of P, Mg and glucose
assist cow to stand
list to lungs
Prevention
DCAD diets
high in anionic salts (CaCl2 and MgSO4)
lower sodium and potassium in the diet
assist with mild metabolic acidosis
PTH receptors become more sensitive + active so they don’t resorb
Bone = breakdown and release Ca
Kidneys = increase C reabsoption
Intestines = increase Vitamin D and increase absorption of Ca
calcium binders in diet
bind dietary Ca in gut so cow cannot easily absorb C
triggers cows natural calcium regulatory mechanisms
Hypomagnesaemia + Hypokalaemia
most common during transition period = herd is stressed, need increased nutrients, low immunity, 3 weeks pre/post partition
Hypomagneseamia
low magnesium due to cell metabolism and enzymes
common in lactating cows during winter and sprin
if fast growing pasture, low roughage
cold and wet weather
Clinical signs
fat or thin cows
lactating cows held off feed or cows in oestrus
muscular spams or convolutions
imbalance of Ca and P
Hypokalaemia
low potassium intake due to no forage
may lead to LDA due to metabolic acidosis
Clinical signs
unable to stand or lift head off ground + muscle weakness
depression
muscle fasciculations
Diagnosis = need serum biochemical analysis
Treatment = oral potassium and adequate dry matter intake
Lameness - risk factors and treatment
painful + restrict normal behaviour
expensive due to compromising milk yield, reproduction, involuntary culling
Score hooves = locomotion, lameness and mobility
Sprecher Methods = measures locomotion (1-5) due to curved back
Lameness = scores 0-3
Causes
Non-infectious = white line, sole/toe ulcer, haemorrhage, corkscrew claw
Infectious = digital or interdigital dermitite, heel erosion, foot rot
Tools to test
hook knives, hoof tester, hoof trimmer, file
straps, pulleys or tilt crush to hold feet
antiseptic spray
Treatment
Claw = therapeutic trimming, remove loos hoof horn, apply block, NSAIDS + antibiotics
Skin = antibiotic or footbaths
Risk factors = age, milk yield, parity, heifers, weight, nutrition, environmental
Prevention = routine trimming, genetics, attend to lame cows quickly, concrete
Emergency Triage
Immediate care
Imminently life-threatening cases
Potentially life-threatening
Potentially serious
Less urgent
Considerations
general exam and vital signs
brief pertinent history of presenting problem
patients name, age, main concerns, any events leading till emergency
nature of traumatic event, witnesses, any deterioration, timing or dose of toxin
concurrent disease and medications
in depth medical history is for later
Cattle emergency = bloat
Primary or frothy bloat = acute/fast increased tension in rumen above the fibromat so can’t expel the built up due to diet change, or new paddock (lush legumes, lucerne, white clover)
Secondary or free gas bloat = unable to eructate, flaccid rumen, obstruction, prolonged recumbency, due to prussic acid poisoning or rumen paralysis
Clinical Signs
progressive distension of LEFT paralumbar fossa
colic
herd problem - all change paddock and eating clover/foaming agent
If Moderate = take cattle off feed, oral 250-500 mls of paraffin/vegetable oil/anti bloat OR if desperate 50mls of detergent in 1L water
If Marked = skin tent over paralumbar fossa, treat medically as may lead to aspiration
If Severe = respiratory distress, emergency surgery (stab left paralumbar fossa)
Management and Prevention
slowly wean off pasture/silage/hay before changing to new one
modify gut microbes and digestion
use anti-bloat preparation (monensin) in winter to prefer for high foliage in summer
Bos indicus less risk
Cattle emergency = acidosis
Clinical Signs
acute disease onset
rumen hypomobility or atony/weakness due to dead rumen with no bacteria
Rumen pH will be <5.5
confirm history excess of grain in diet, and grain in faeces
acidaemia and diarrhoea
dehydrated, depressed, uncoordinated collapse → death
Treatment
1g/kg of sodium bicarbonate in 10L of water via stomach tube
0.5 g/kg of magnesium hydroxide in 5 L of water via stomach tube
0.5g/kg of sodium bicarbonate in 5L of water via stomach tube every 6hr x2
1mg/kg of flunixin meglumine via IV injection every 8hrs x3
10mg/kg of thiamine via IM injection every 24hrs x3
12 mg/kg of procaine penicillin G via IM x2 day for x3 days
1ml/50kg of chlorpheniramine maleate via IM injection every 8hrs x4
250 mL of calcium borogluconate
monitor and reintroduce food
Small ruminant emergency = pregnancy toxaemia / ketosis
last 2-4 weeks of gestation when sheep/goats have multiple young
rapid foetal growth → less abdominal space = large impact on ewe
Clinical Signs
anorexia → weak and recumbent
depressed + separate from herd
progress to neurological signs - tremors, star gazing, uncoordinated,
Treatment
propylene glycol (60ml PO every 12hrs for 3 days OR 100mL/day)
IV glucose or dextrose
Ketosis and Preg Tox Treatment oral or as a drench or mix with feed
Prevention
check ewe BCS
ultrasound
avoid mustering and yarding that prevent ewes from feeding for more than 12 hours
in last 6 weeks prior to lambing
supplementary feeding
avoid procedures involving tipping, crutching, shearing, foot paring
in last 2 weeks prior to lambing = avoid drafting, drenching, or vaccinating
Small ruminant emergency = milk fever
high risk = older eyes, ewes in last few weeks of pregnancy, held off feed
Clinical Signs
unable to walk → lying down on sternum
nervous
dilated pupils
paralysis
death within 1-2 days
Treatment
INJ calcium borogluconate
recovery is rapid in 30mins
treatment can be repeated every 4-6 hours if animals don’t fully recover
Prevention
supplement ewes with calcium - lick blocks and crushed limestone
do not hold ewes off feed for longer than necessary (especially last 60 days of pregnancy
Small ruminant emergency = hypomagnesaemia or grass tetany
sheep do not store magnesium = must ingest each day to ensure needs are met
winter pasture / any scenario where there are = low legumes, calcium, magnesium
changes in diet or quality of feed
pre or post lambing
Clinical Signs
nervous and shaking
stiff legs
staggering or falling over
fast growing lambs
ewes found dead
Treatment
MgCl orally
Magnesium sulphate IV (4 in 1 vaccine)
Small ruminant emergency = poliencephalmalacia
Thiamine deficiency caused by sudden changes in diet leading to neurological disease (demyelination)
reduces energy to the brain → star gazing
Thiamine is normally produced by bacteria in rumen of cattle and sheep if diet is well balanced → produce enzymes which break down and inactive thiamine
Small ruminant emergency = urolithiasis
common in early castrated males due to small urethra
stones
Apatite = calcium carbonate hard beads due to diet of lucerne + legumes
Struvite = phosphatic stones, sandy due to diet high in grain + pellets
Clinical Signs
straining or “constipated”
lethargic
drug reaction
painful → excessive vocalisation and grinding teeth
pulsation of penis
Treatment
diazepam + poke or push penis out
surgery = catheter to flush out or amputation