5. Caries
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
106 Terms
Caries
A disease, not a symptom. Caries can cause cavities (a hole)
Cavities
hollow places in teeth caused by decay, can be caused by caries or other things
What is usually the cause for caries?
bacteria
What is a huge issue in treating caries?q
accessibility, especially in low income areas
Prevalence
The number or proportion of cases of a particular disease or condition present in a population at a given time. (who HAS caries within a time frame)
Incidence
The number or rate of new cases of a particular condition during a specific time. ( who DEVELOPS caries in a time frame)
Over the years, caries development in the US has been relatively ____
stable
What are factors that contribute to prelevance
regional factors, health systems, economic factors
What are factors that contributed to caries stability around the world?
Improvement and changes around the world on oral health/treatment
Dental caries experience
people who have experienced or had caries in their whole life. Caries experience cannot decrease, only increase (cumulative experience) and varies among diff ethnicities
Which two minority groups have the largest disparity when it comes to caries?
african-american and hispanic
Dental caries
multifactorial, transmissible, infectious oral disease caused primarily by complex interactions of cariogenic oral flora (biofilm) with fermentable dietary carbs on the tooth surface over time. Can be transferred directly (body fluid) or indirectly (sharing a fork)
Vertical transmission
from parent to child
Horizontal trasmission
person to person (partner to partner, friend to friend)
If you have no teeth, can you have caries?
no
Protective factors
saliva flow and components, proteins, antibacterial, fluoride, calcium, phosphate, protective dietary components, n on-cariogenic sweeteners
Pathologic factors
acidogenic bacteria, frequency of fermentable carbs, ingestion, reduced salivary function
acidgenic vs aciduric bacteria
acidgenic= produce the acids that harm enamel
aciduric= survive and thrive in low pH environment
Caries balance consists of
protective factors and pathologic factors
What are the four factors that contribute to caries
teeth, bacteria, diet, time
Cariogenic challenge process
initiated by exposure of the cariogenic bacteria to fermentable carbs such as monosaccharides glucose and fructose or the disaccharides sucrose and lactose
More factors that can lead to caries
Less saliva, eating too much sugar, bacterial imbalance, lack of access to care, oral health literacy
Direct influences on caries/cavities (bacteria/diet)
Good AND bad bacteria
Antibacterial agents
dental sealants
fluoride
chewing gum
saliva
protein
sugars
Ca2+, PO43-
Plaque pH (microbial species)
External influences
education
behavior
sociodemographic status
income
dental insurance coverage
knowledge
oral health literacy
Cariogenic challenge details
1. Initiated by bad bacteria to form
2. Glucose and fructose are small sugars more likely to impact teeth (small, fermentable sugars)
3. Sucrose and lactose are disaccharides, large sugars
Glycolysis
converts glucose into pyruvic acid (via glycolysis) and then pyruvic acid to lactic acid; acetic acid and propionic acids are side products
Through enzymatic rxn, ______ is transferred until it is pyruvate
glucose
Glucans/fructans function
allow caries to stick to the teeth, act as a glue that allows caries to stay on the teeth
Bacteria uses _____ to make lactic acid and other things
glucose and fructose
Stephan Curve
The relationship between pH at the tooth surface and time following consumption of sugar; enamel demineralize @5.5pH; dentin @ 6pH
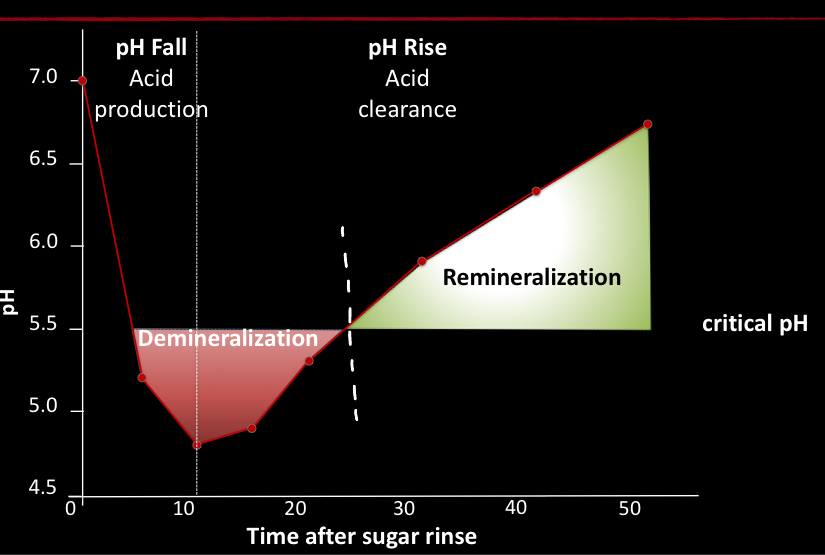
What raises the ph value
bicarbonate (buffer that stabilizes a low pH higher/normal level. neutralizing agent)
Dentin resorbs _____ than enamel because it has less ______
quicker; minerals
What helps raise Ph to promote remineralization?
bicarbonate and saliva
How long does it take for pH to get back to normal? what is a normal pH? what is critical enamel pH?
50 minutes to an hour
7 is normal
5.5 is critical (can result in demineralization)
Cariogenic shifts the caries balance scale towards
pathologic factors
Enamel
outer surface of the tooth. Mostly made of inorganic materials (crystals). Hydrophobic
more minerals in dentin makes it harder to demineralize
Coke contains a lot of ____ that eats away at the teeth
phosphoric acid
Do enamel and dentin behave the same way? why or why not?
no, they are made up of the same materials but in different compositions
Enamel- 88% inorganic, 10% water, 2% organic
Dentin- 50% inorganic, 30% organic, 20% water
Inactive caries
black caries that do not progress, typically visually unappealing
Location of caries bacteria
Determines where caries will form
Occlusal surfaces- pits/fissures/grooves easily attract caries
Incisors- on palatal surfaces may have pits where caries can develop
Interproximal area between teeth- needs flossing, attracts caries
Plaque stagnation areas
around patient brackets
improper restorations
roots and cervical (gumline)
pits/fissures
interproximal area
Pellicle formation
surface accumulation of growth. Glycoproteins from saliva stick to enamel; bacteria need this layer as primer for attachment
Glycoproteins
form on tooth surface in a matter of minutes through electrostatic forces (negative and positive charges areas)
Pellicle
glycoprotein layer a part of saliva that adheres to tooth surface. bacteria with the right receptor adheres to the pellicle
for biofilm formation, in 0-24 hours, bacteria on tooth...
grows overtime by multiplying in colonies (early attachment bacteria colonizers attach first to help form colonies)
Biofilm formation
co-adhesion and growth of attached bacteria to formation of microcolonies
Do micro colonies vary in bacteria type?
yes
Microbial succession (biofilm formation)
increased species diversity with continued co-adhesion and growth of microcolonies (1-7 days)
- colonies grow thicker, varying forms (long, spiral, ovoid)
- climax community: after 4-7 days
Climax community
one week or older. Big mix of a lot of bacteria, some close to the tooth and some far away
- thicker film and less oxygen on the tooth, more oxygen on plaque surface
- bacteria that need oxygen will stay at the surface
Is the incisal edge a plaque stagnation site?
no
Resident oral flora
resident microflora has a diverse composition, consisting of a wide range of gram positive and gram negative bacterial species, as well as yeasts and other types of microorganisms. This is the NORMAL bacteria (symbiotic relationship)
- when good environment changes (normal pH for example) that is when bad bacteria takes over
Types of resident oral flora
streptococcous salivarious
strep mitis
strep oralis
strep sanguinis
strep dentisani
strep(tovella) melaninogenica
prevotella melaninogenica
fusobacterium nucleatum
veilllonella spp
Resident oral flora benefits
- neutral ph, likes o2
- saturation of microbial attachment sites
- more effective competition for essential nutrients
- the creation of conditions unfavorable to the growth of the invading microbes
- production of inhibitory factors (bacteriocins, hydrogen peroxide)
should the mouth ever be 100% sterile?
no
3 hypothesis to resident oral flora
1. specific plaque
2. non-specific plaque
3. ecological plaque
specific plaque hypothesis
only one bacteria causes one disease (certain bacteria can only cause caries). DEBUNKED
Non-specific plaque hypothesis
more than one bacteria/factor can cause caries, multitude of bacteria. How thick. anaerobic and acidic is the biofilm? enough o2?
Ecological Shift
environmental factors contribute to caries (stress, intaking more sugar). shift in environment cause bacteria type shifts from healthy to bad bacteria causes pH shifts causes caries
Factors of the ecological plaque hypothesis
stress (increased sugar intake and acid production)
low Ph (environmental change)
ecological shift (s. mutans, lactobacilli, bifidobacteria, s. sanguinis and s. gordonii)
Disease (health and caries)
Bacteria most common in early lesions
S mutans
Achinomyces gerensceriae, veillonela parvula, veillonela species
Dentinal caries and tubule infection bacteria
deeper the cavity, the more you find the caries that love acid (acetophillic)
- aciduric can withstand acid conditions (lactic bacilli)
- s mutans
-lactobacillus rhamnosus, acidophilus, paracasei, fermentum, plantanum, casei, johanmei)
-actinomyces israeli, adontolyticus, noeslundi
-bifidobacterium detnum, species
- privatella melaningenica
Root caries bacteria
common on root surfaces, receptors are more compatible with glycoproteins on root surface
- scientists still identifying more
- bifidobacterium are the worst bacteria
(s mutans, actinomyces israeli, actinomyces species, bifidobacterium detium, bifidobacterium breve, bifidbacterium species)
Lesion progression, early stage
bacteria at this stage is not deep in the tooth but is on the surface. easily restorable
- caries begin to etch away at the surface. enamel prisms are etched away superficially and cause pores that go deeper into the enamel
incipient lesions
have not invaded the enamel yet, not always a need for treatment
pseudointact surface layer
(incipient lesions) surface is not broken down, no cavity at this point (darker zone). mineral loss is smallest here
Transluscent zone
has majority of demineralization going into the tooth (review pic)
Lesion body
has the most pores it is why the lesion is weak, Loss of minerals is largest here
4 layers of incipient lesion
pseudointact surface layer, lesion body, dark zone, transluscent zone
what causes lesions to look white?
pores
does cavitation have to be treated?
yes
Lesion progression
- subsurface lesion under pseudointact layer
- increased pore volume (30%)
pores are diffusion path for microorganisms and substrate
- light scattering causes white spot
Dentin contains....
lots of tubules and canals filled with nerve endings from pulpal nerve (why we feel cavities). Nerve endings fuel everything and with acids, they begin to seal/crystallize to heal
Secondary dentin
sclerotic dentin
dentin with plugged up tubulues to protect from further acid/caries advancing (not as a result of aggression). Temp change, stress and chewing can also cause the SD to protect the nerve
Advanced white spot
acids reached dentin and remineralized. When dentin is remineralized, only the collagen fibers remain which makes it softer. Pulpal chambers become smaller and smaller with age from remineralization
White/brown spot
pulp builds tertiary dentin by adding more material to it to make it thicker (result of aggression like caries)
Microcavitation
ICDAS stage 4. More demineralization of dentin, more sclerotic dentin, more tertiary dentin
Cavitation
Dentin exposed and begins to get destroyed
Collagen fibers in tact, minerals removed
MMP enzymes in dentin eat away at collagen fibers caused by acids
destroyed dentin must be drilled and restored
Cavitation
softened collagen network. destroyed dentin has to be removed and restored by filling
Lesion progression into dentin (chart)
REVIEW PIC IN NOTES
infected---affected----sound
zone of destruction if the clinically infected dentin/caries. ALWAYS remove
affected= demineralization, dentin softened, partially lost minerals. Stopped caries can result in remineralization which can be left behind
sound=healthy dentin
Infected dentin is ______ in texture
soft and wet, leathery. SOME can be left behind when it is near the pulp, but margins are ALWAYS cleaned out
What type bur is used to clear out dentin
latch type bur (round carbide) WITHOUT water (6-8,000 rpm)
What type flakes does normal dentin have
dry flakes
Breakdown of dentin/enamel to the pulp chamber is....
sometimes not restorable
Order of dentin lesion progression
sclerosis (dark areas), demineralization, tertiary dentin, nerve infection
Once the lesion has passed the _____ progression of the lesion is much quicker
dentoenamel junction
Root surface lesion
plaque stagnation can occur under caries
Calculus
opposite of caries, it is tarter so plaque is remineralizing to become calcified where caries demineralized to become calcified
There are _____ minerals closer to the pulp
LESS> tubules are wider and closer to the pump
You can _____ a lesion when it is not cavitated, you do not always have to _____
arrest; drill
Sugars
arch nemesis of teeth
mono, di and polysaccharideds
monosaccharides
glucose, fructose, galactose
Di-saccharides
glucose+fructose (sucrose), galactose+glucose (lactose), glucose+glucose (maltose)
Polysaccharides
body cannot use these, must be broken down by the amylase enzyme. Once broken, it can be metabolized
starch, amylose, amylopectin
Do you want cariogenic challenge to happen often during the day?
NO
Eating a lot of _______ and _____ can lead to a high cariogenic challenge
snacks/sugars; bad dental habits
xylitol
a sugar alcohol that can be ingested by the bacteria but CANNOT be metabolized or produce acidic properties
Artificial sweetners
NOT cariogenic, but not good for ingestion.
Cariogenic bacteria can _______ glucose
metabolize
commonly metabolized into an acid
cariogenic bacteria can NOT metabolize
calcium, polysaccharides, proteins or water
is bonding hydrophobic or hydrophillic
hydrophobic