IMED1004 - Cardiovascular Disease (L25, 26)
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
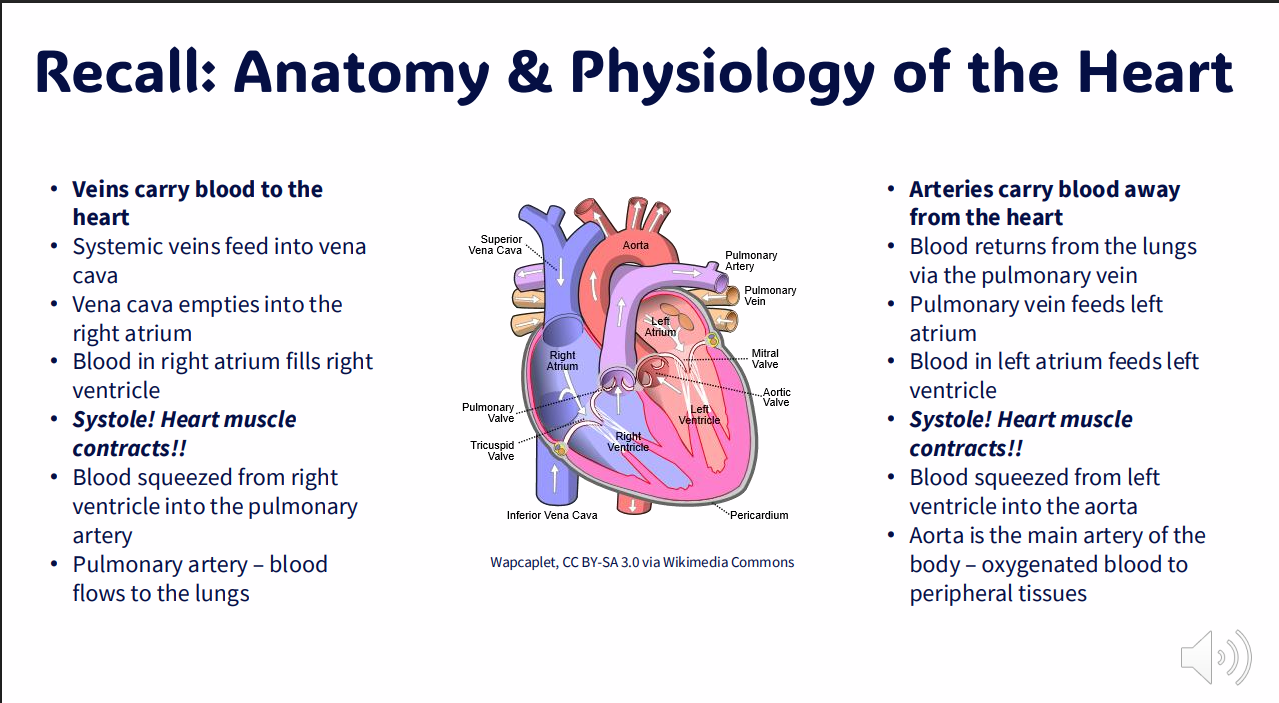
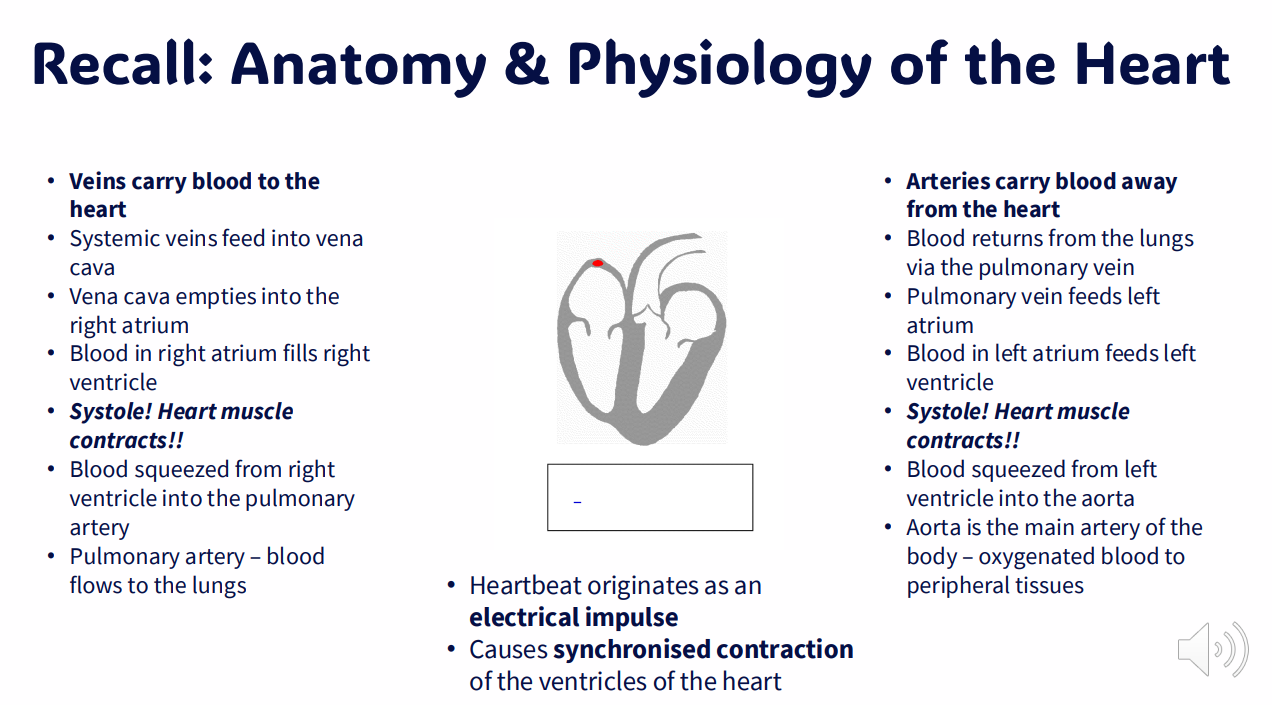
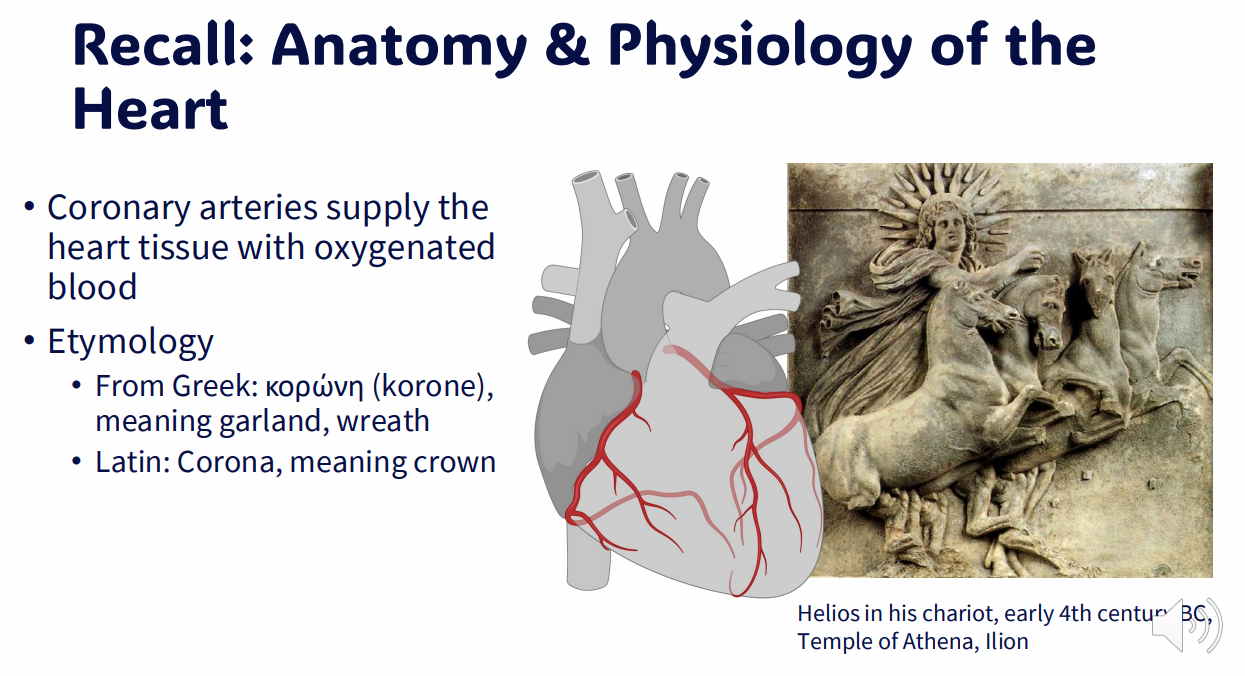
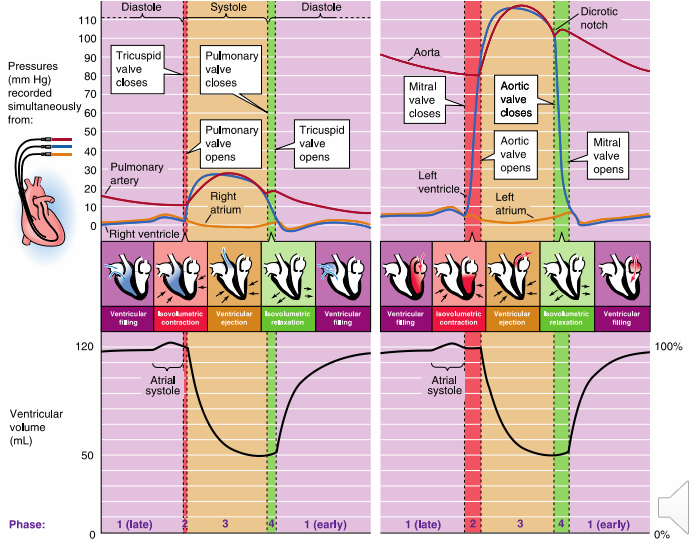
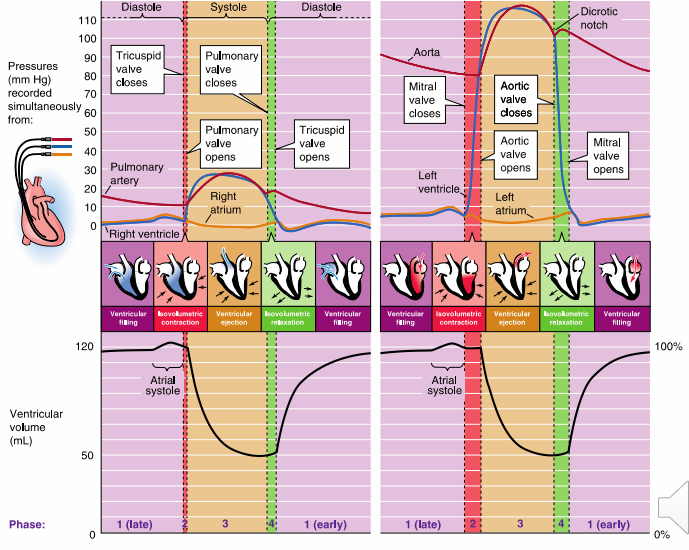
Recall: Anatomy and Phsyiology of the Heart 1
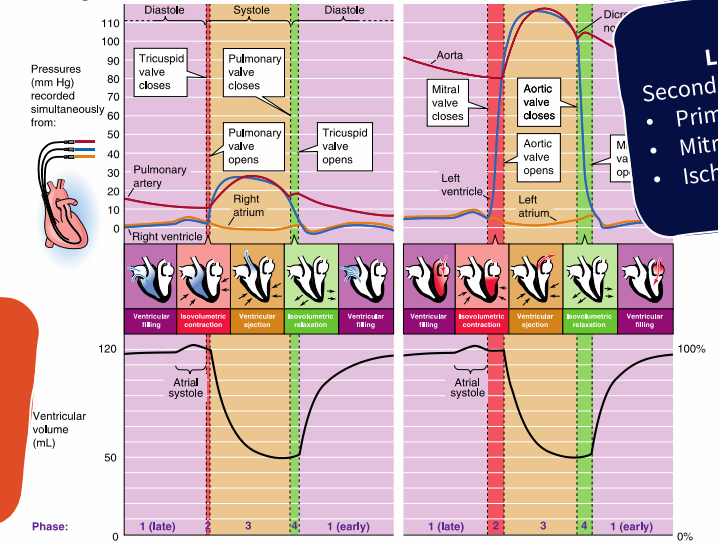
DIAGRAM ON SLIDE 5
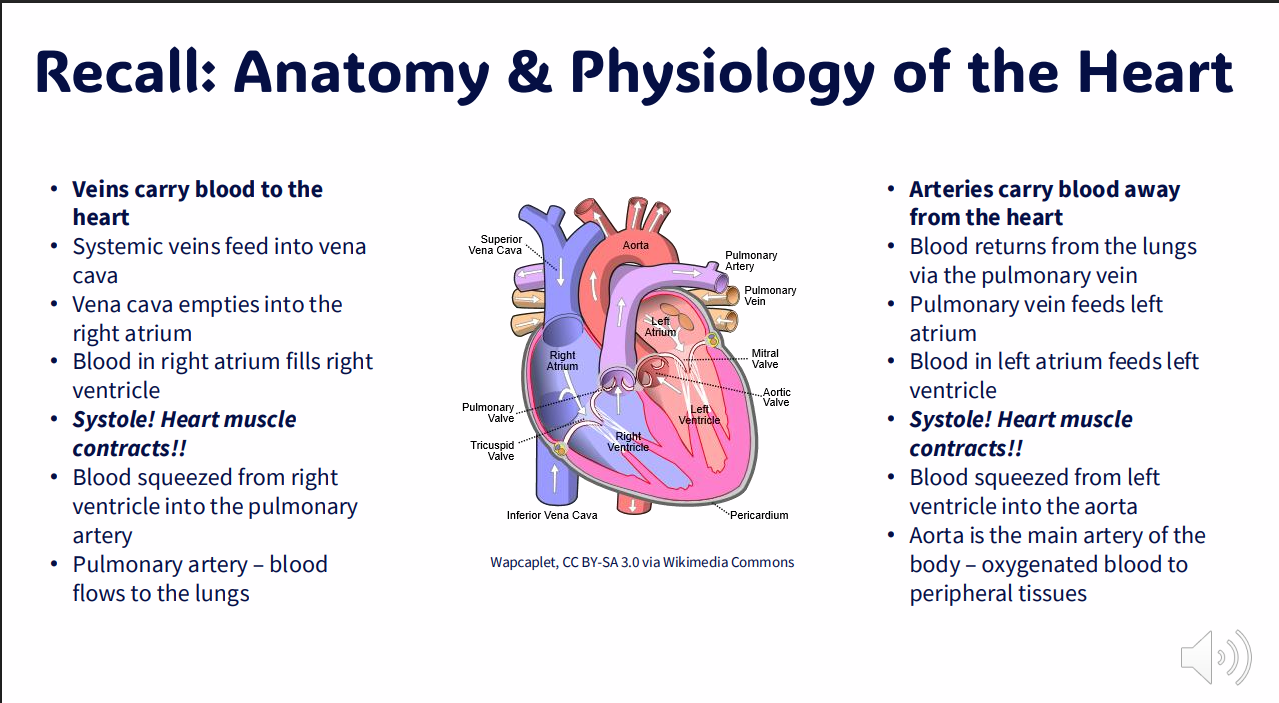
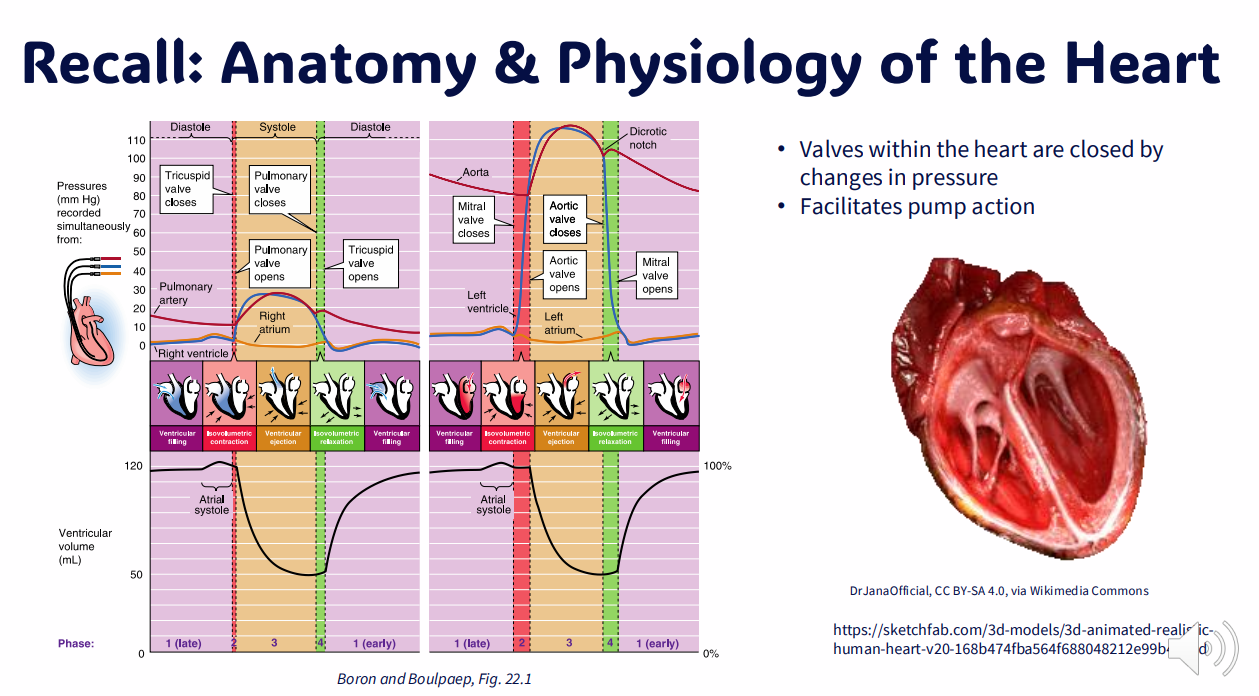
Recall: Anatomy and Physiology of the Heart 2
DIAGRAM ON SLIDE 6
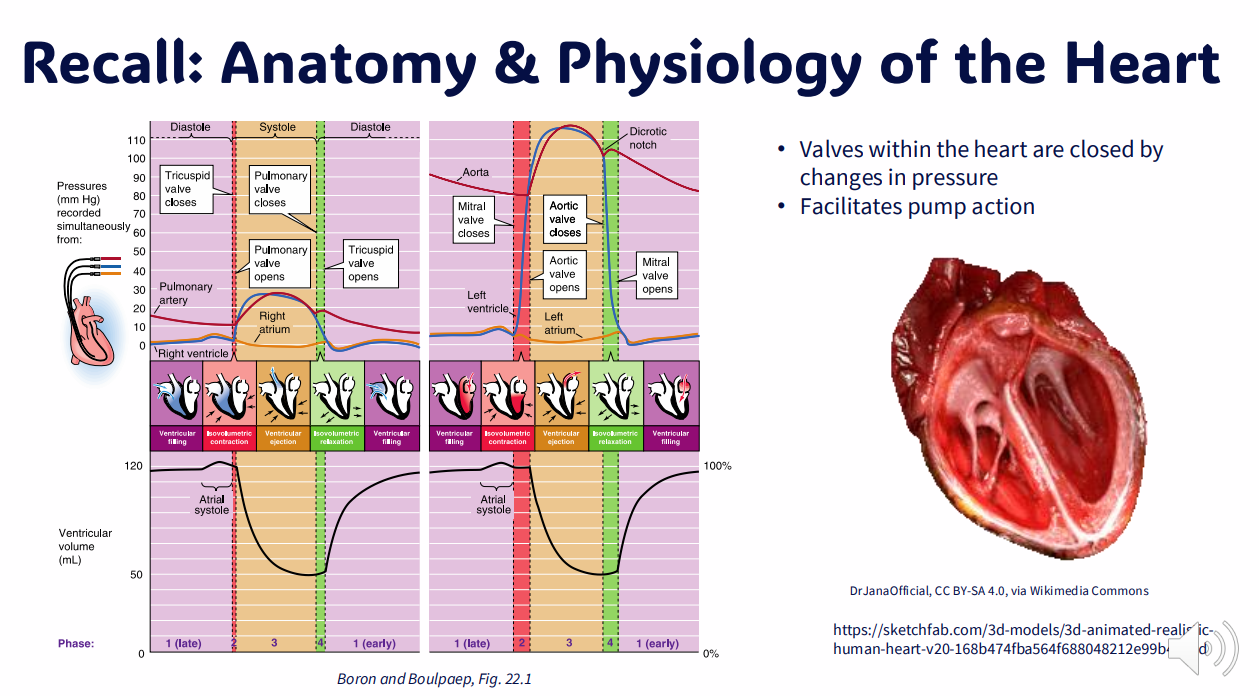
Recall: Anatomy and Physiology Of the Heart 3
DIAGRAM ON SLIDE 7
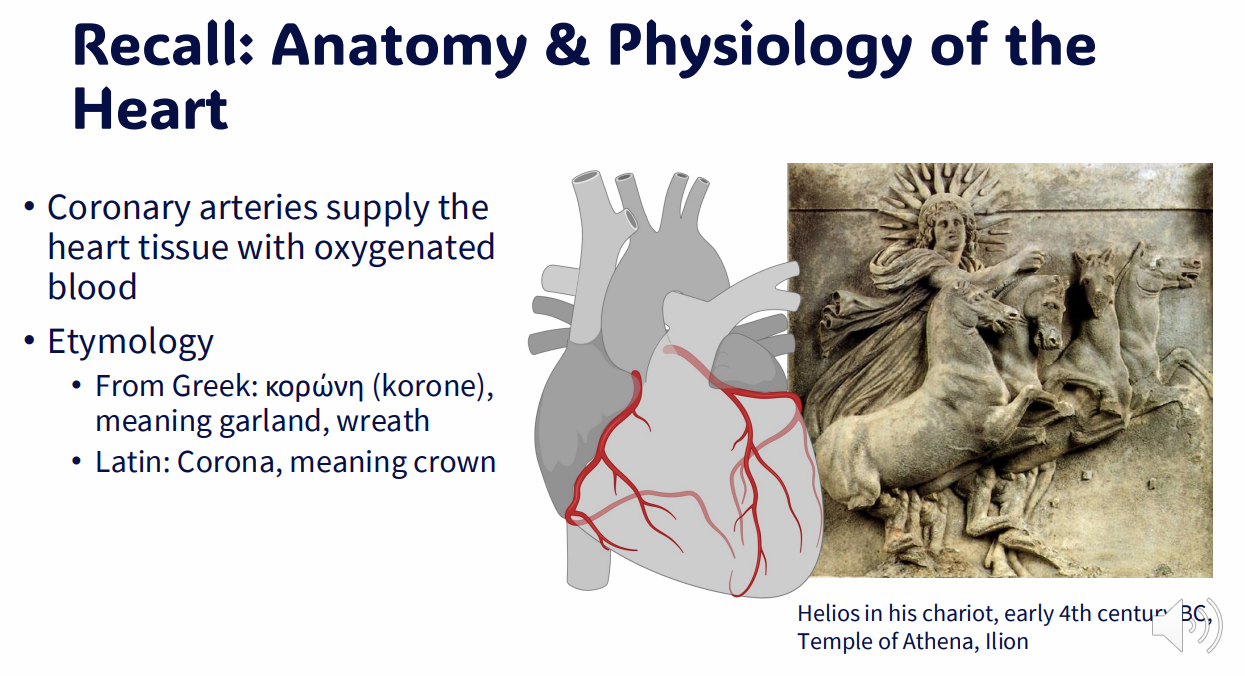
Recall: Anatomy and Phsyiology of the Heart 4
DIAGRAM ON SLIDE 8
"Cardiovascular disease" describes a diverse range of conditions
Clinical Manifestations of Pathology: molecular, functional or morphologic abnormalities
- Failure of the pump
- Obstruction to flow
- Regurgitant flow
- Shunted flow
- Disorders of cardiac contraction
- Rupture of heart or major vessel
.
AETIOLOGIES: Causes of disease
- ischemia
- infection
- maternal disease
- genetics
- nutritional deficiencies
- alcohol, smoking, drug use and other modifiable risk factors
- environment
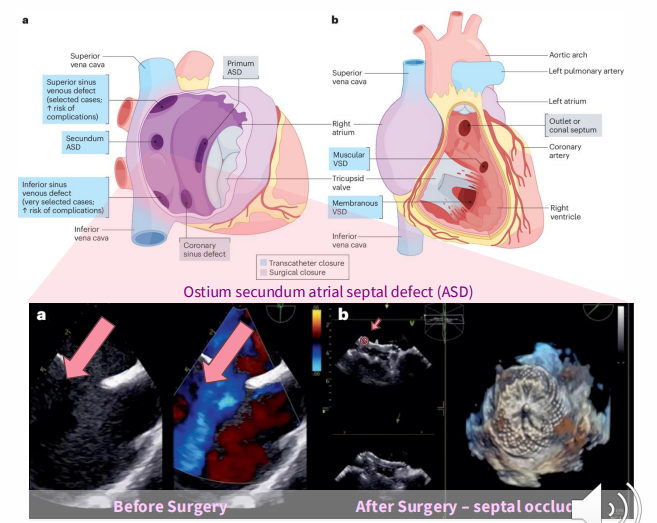
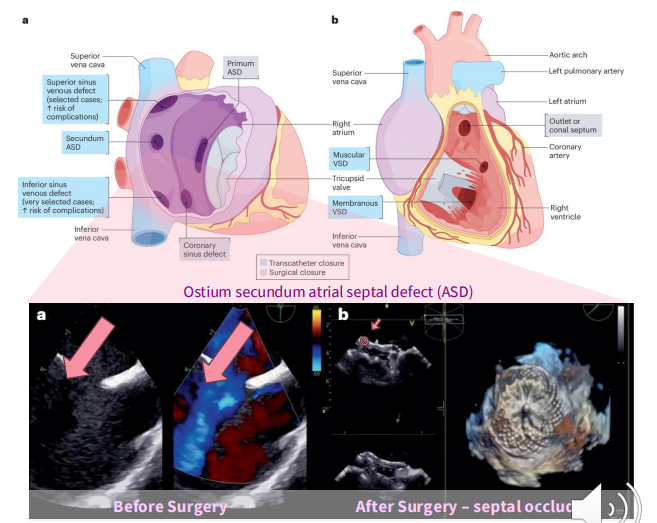
Congenital Heart Disease
- gross structural abnormality of the heart or intrathoracic great vessels
- Colloquially: "hole in the heart"
- shunt permits flow of blood between two sides of heart
- Symptoms, prognosis will vary with the type and severity of the defect
Congenital Heart Disease Causes
- 90% of cases - cause not known
- chromosomal disorders
- genetic (family history)
- prematurity
.
IN UTERO:
- infectious disease; Syphilis, rubella, toxoplasmosis
- diabetes mellitus
- micronutrient deficiencies
- teratogens
- tobacco, alcohol and illicit drug exposure
.
- Incidence: around 1% of live births
- Leading cause of birth defects
- Treatment of neonates improving; newly-diagnosed adults increasing proportion of cases
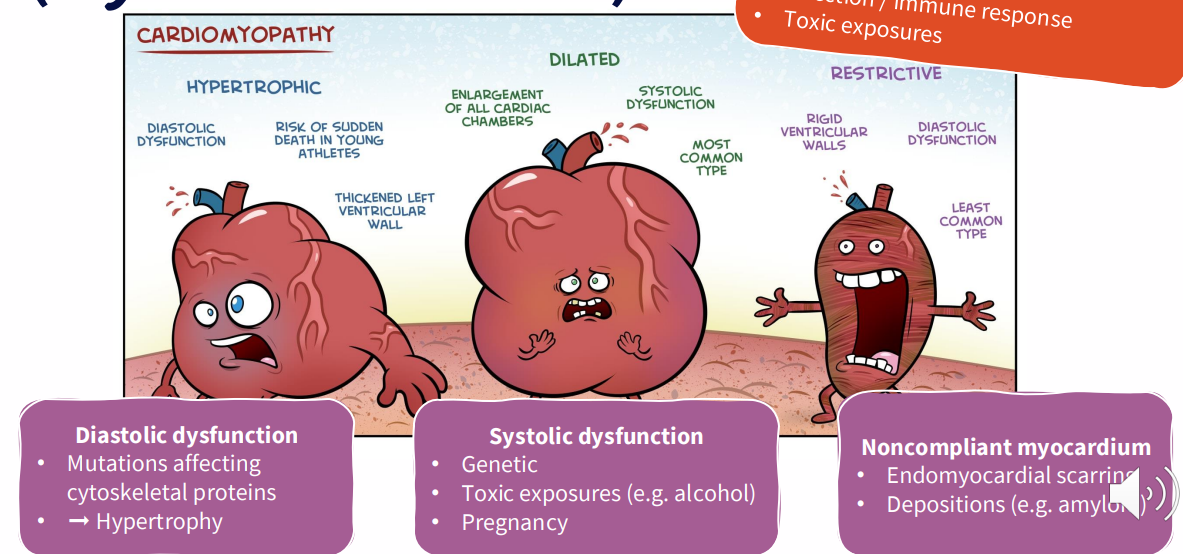
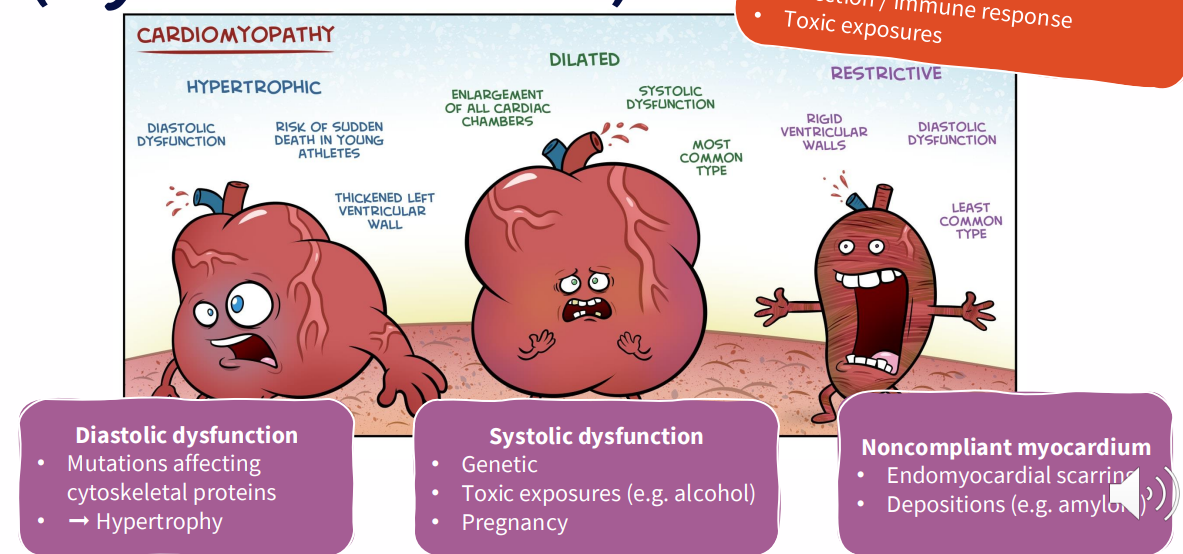
Cardiomyopathies (Myocardial Diseases)
INTRINSIC CARDIOVASCULAR MUSCLE DISEASE:
- Some aetiologies: idiopathic, genetic, infection/immune response, toxic exposures
.
DIASTOLIC DYSFUNCTION:
- mutations affecting cytoskeletal proteins - hypertrophy
.
SYSTOLIC DYSFUNCTION:
- genetic
- toxic exposures (e.g alcohol)
- pregnancy
.
NONCOMPLIANT MYOCARDIUM:
- endomyocardial scarring
- depositions (e.g amyloid)
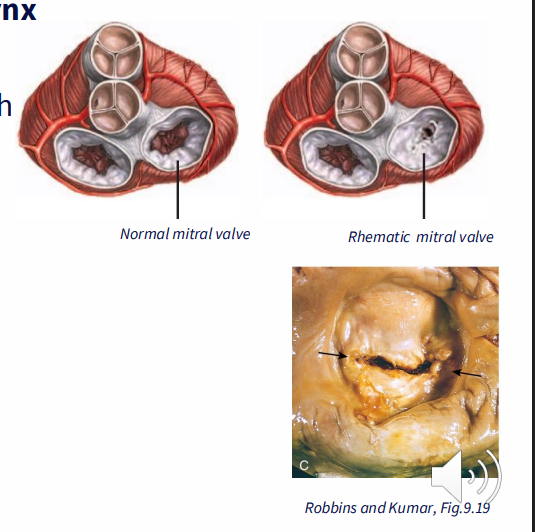
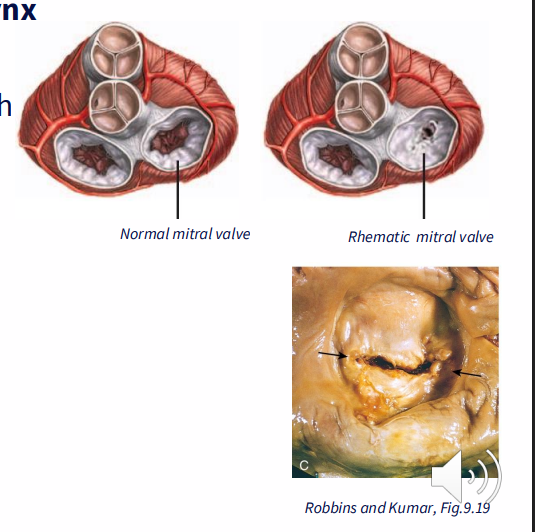
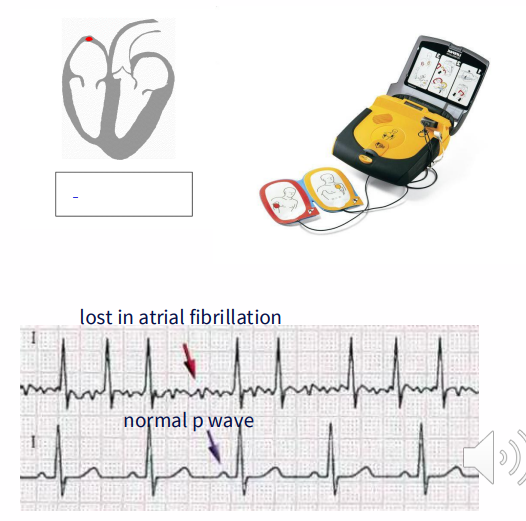
Valvular Heart Disease: Rheumatic Heart Disease (RHD)
CAUSE: Streptococcal infection of tonsils and pharynx
Rheumatic Fever:
- anti-streptococcal antibodies are cross-reactive with cardiac tissue
- Fibrosis, stenosis (narrowing) of mitral valve
- pressure buildup in left atrium
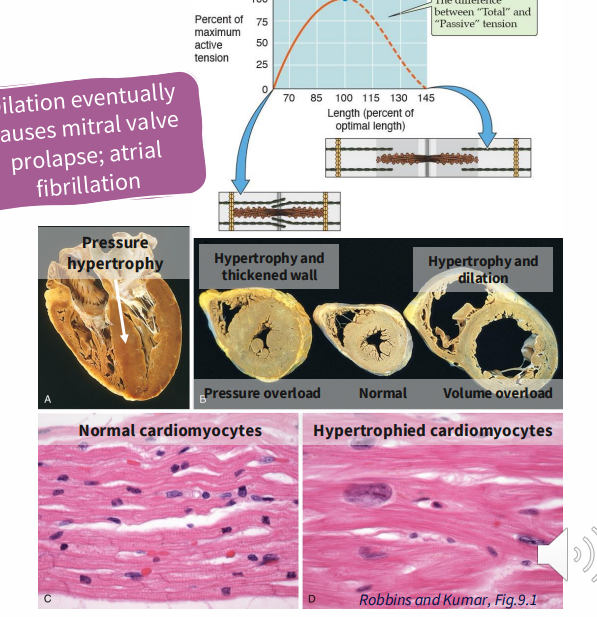
- Dilation of left atrium; hypertrophy
- atrial fibrillation; congestive heart failure
.
- Common in poor socioeconomic conditions
- 15.6 million people
- Poor access to healthcare, nutrition
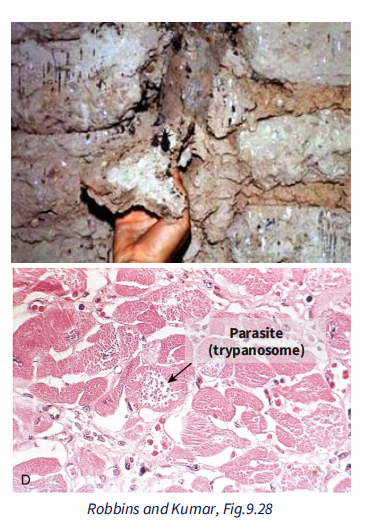
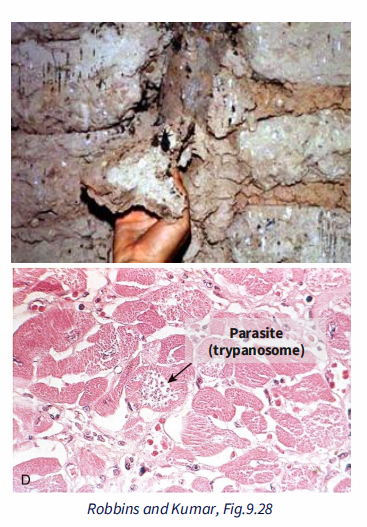
Myocarditis: Chagas disease (American trypanosomiasis)
- Parasitic infection - Trypanosoma cruzi
- Transmitted by insects (triatomine), live in cracks of poorly constructed homes
- 10 million people are infected worldwide
- some control achieved through vector control, screening
- further control could be achieved by improving living conditions
- Causes destruction of heart muscle: inflammatory response; necrosis
- Acute attack: 10% die
- Chronic, immune-mediate: congestive heart failure, arrhythmia
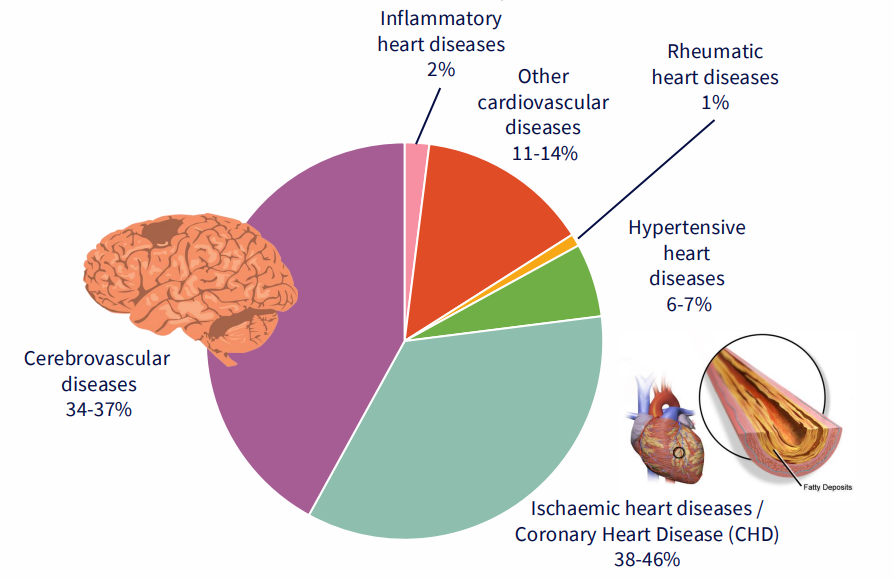
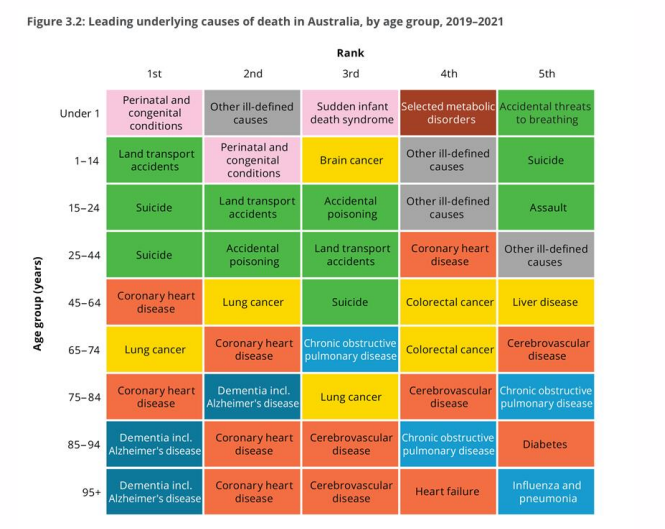
Ischaemic Heart Disease, coronary heart disease and stroke are major causes of death
DIAGRAM ON SLIDE 15
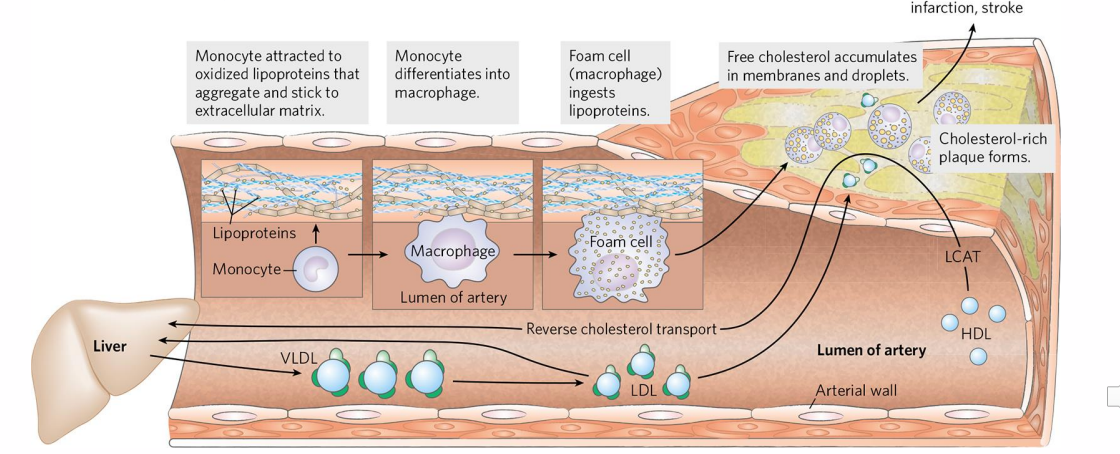
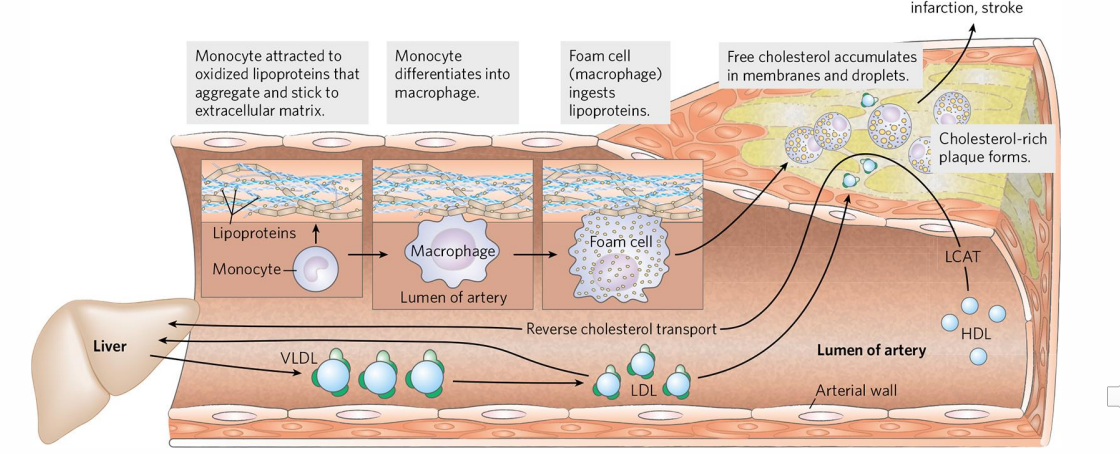
Pathophysiology of Atherosclerosis
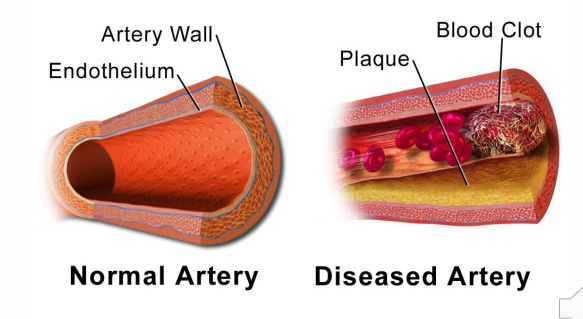
- Atherosclerosis results in narrowing of blood vessels
- this is a major cause of heart attack and stroke
.
- when we have imbalance between the LDL and HDL, HDL cant remove sufficient amounts of these LDL, resulting in increased concentration of these LDL in circulation
- these can stick or aggregate to extracellular matrix and they can oxidise
- this attracts monocytes which differentiate into macrophages and they will ingest these lipoproteins and become foam cells
- endothelium becomes more permeable to the lymphocytes and monocytes and so these cells migrate into the vessel wall
- this will attract more LDL which migrates into the cholesterol wall (which accumulates which we call a plaque)
.
- anothrer serious thing that can happen is that the macrophages at the centre of the plaque can die and we have formation of necrotic core and fibrous cap
- hence this fibrous cap can cause thrombosis
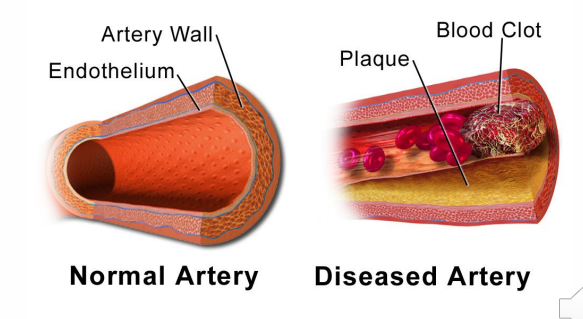
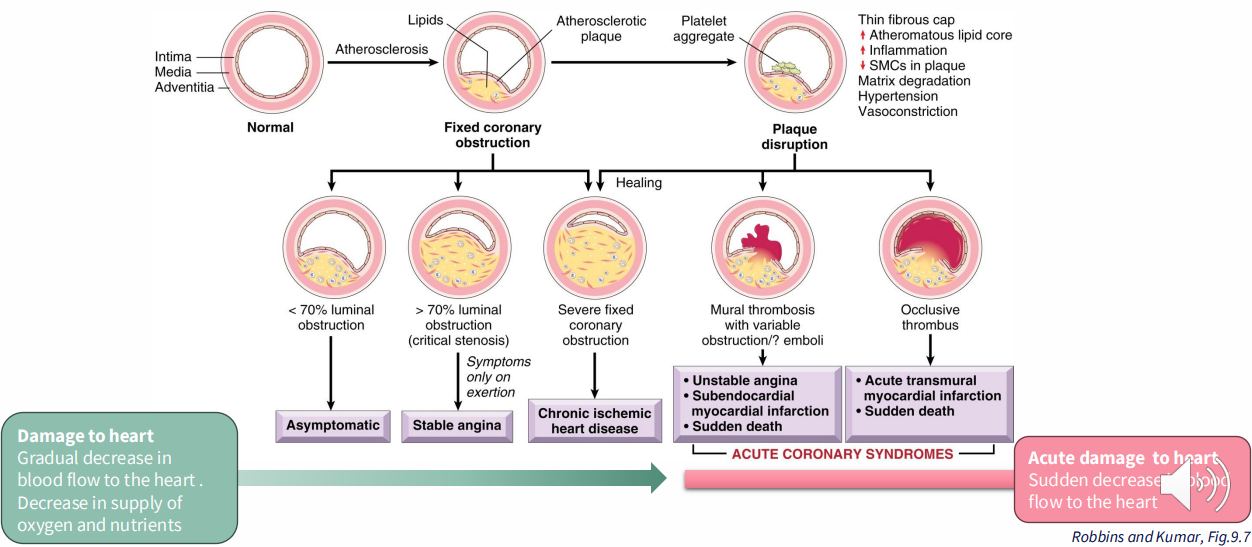
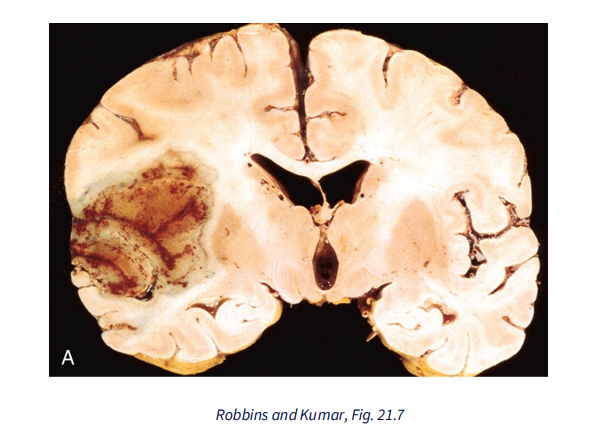
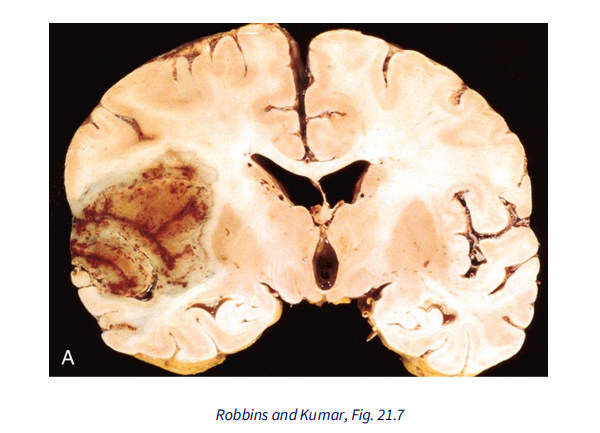
Pathogenesis of myrocardial infarction, stroke
- fibrous cap ruptures -> lipid fragments, cellular debris released into vessel lumen
- thrombogenic agents -> formation of thrombus
- thrombus: accumulation of RBCs, platelets (commonly called a clot)
.
larger thrombus in:
- coronary blood vessel --> heart attack
- cerebral blood vessel --> stroke
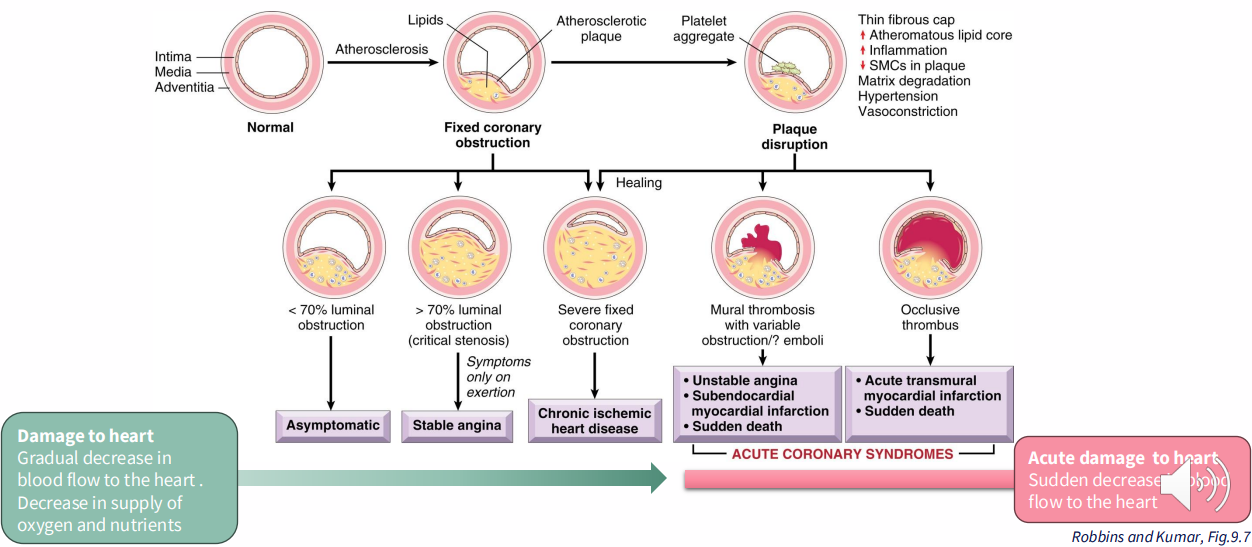
Coronary Artery Disease (CAD)/Ischaemic Heart Disease (IHD)
- damage to heart: gradual decrease in blood flow to the heart. Decrease in supply of oxygen and nutrients
- acute damage to heart: suden increase in blood flow to the heart
.
- diagram important to understand
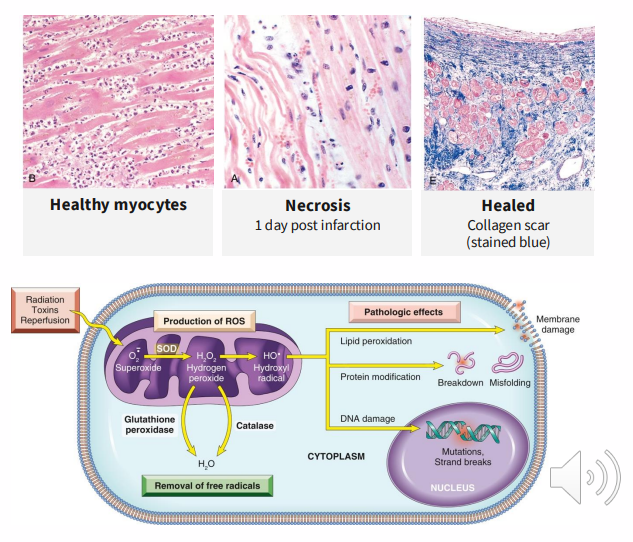
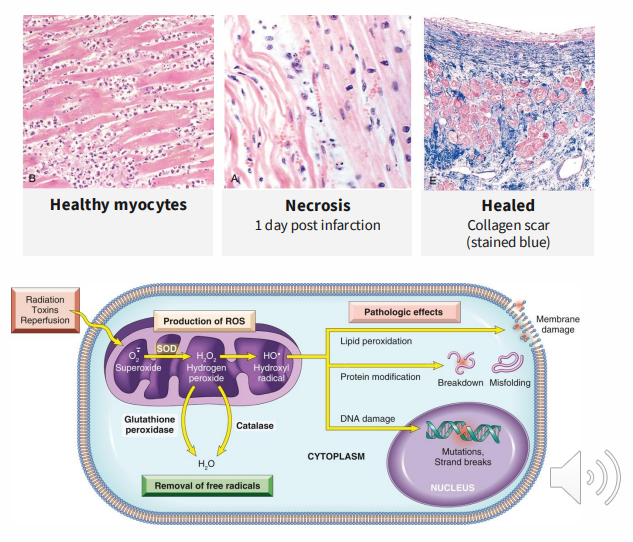
Ischeamic Heart Disease: Myocardial Infarction (Heart Attack)
MECHANISMS OF DAMAGE:
Ischaemia:
- waste not removed
- mitochondrial damage
- leaking of proteolytic enzymes
.
Ischaemia reperfusion injury:
Oxygen restoration:
- more free radicals, reactive oxygen species -> damage
- Calcium overloading -> arrhythmias, apoptosis
- Exaggerates inflammation
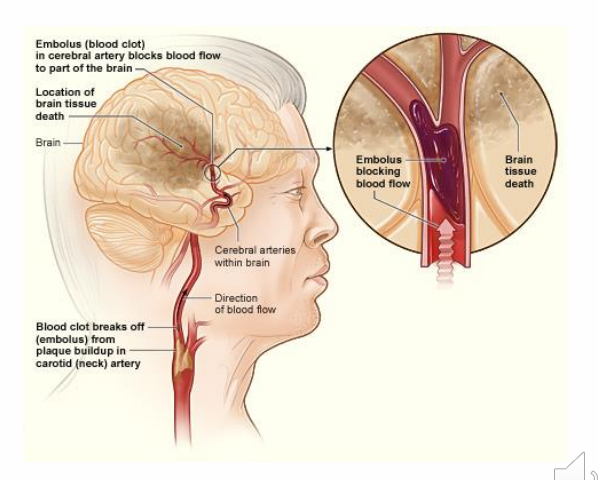
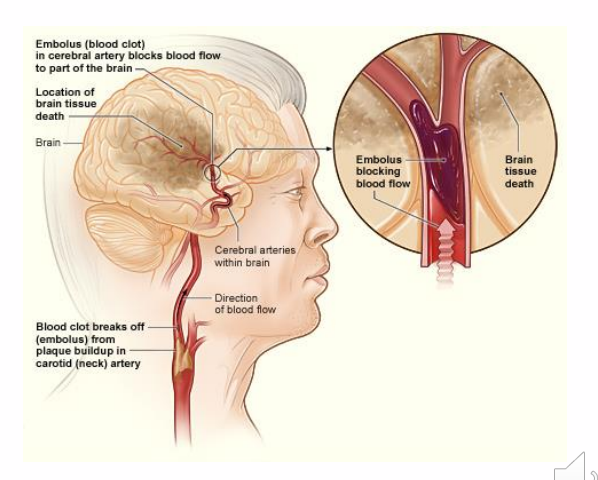
Ischaemic Stroke
ISCHAEMIC STROKE: blood supply to brain affected
.
Embolisms block blood flow:
- Thrombus formation in atherosclerotic cerebral blood vessels
- small vessel disease in brain (very small atherosclerotic plaques)
- thrombi which form in other organs (e.g heart) travel to brain through blood vessels
Haemorrhagic Stroke
HAEMORRHAGIC STROKE: due to blood vessel rupture
.
- Aneurysm (swelling in vessel wall)
- can be cauesd by uncontrolled high blood pressure
- Atherosclerosis can increase blood pressure
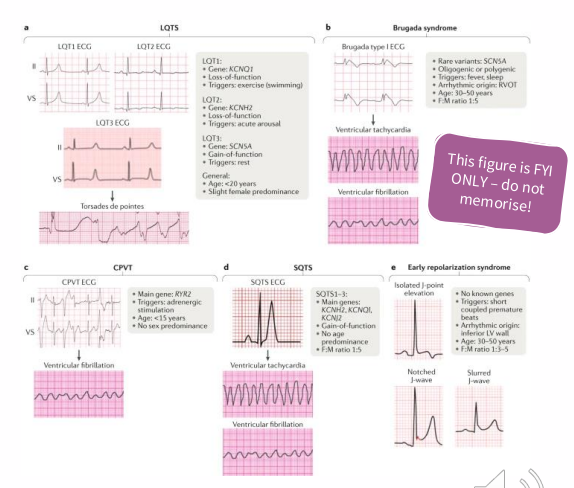
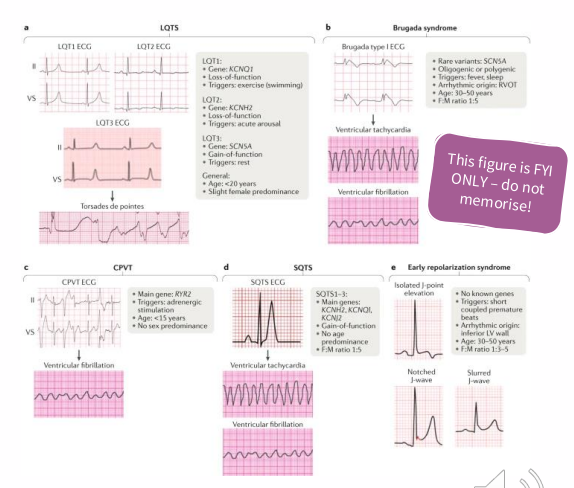
Cardiac Arrhythmia
- Heartbeat originates as an electrical impulse, causes synchronised contraction of the ventricles of the heart
- Abnormal electrical activity causes cardiac arrhythmia (too fast, too slow, regular, irregular)
- can lead to deterioration in the mechanical function of the heart
.
AETIOLOGIES: genetic (rare) or ischemic injury (common)
Sudden Cardiac Death
- Cessation of normal cardiac electrical activity, heart stops pumping blood
CAUSES:
5-10% are due to arrhythmias
- note - not all arrhythmias will be rectified by defibrillation
.
10% are due to structural heart disease
- congenital coronary artery abnormalities
- myocarditis (inflammatory cardiomyopathy)
- hypertensive heart disease
- myocardial hypertrophy
.
15-20% are non-cardiac causes
- e.g trauma, aortic rupture, poison
.
65-70% - coronary heart disease (age 35+)
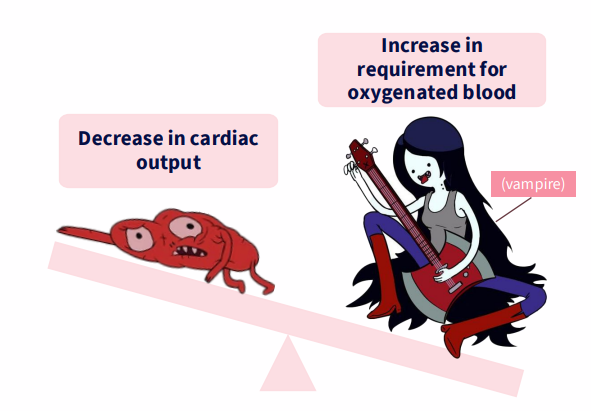
Congestive Heart Failure (CHF)
HEART CANNOT PROVIDE ADEQUATE PERFUSION TO MEET METABOLIC REQUIREMENTS OF PERIPHERAL TISSUES
.
- "Congestive" - congestion of venous circulation
.
Decrease in cardiac output is more common
- gradual, progressive onset (age, chronic work overload)
- acute (myocardial infarction, acute valve dysfunction)
.
- imbalance between output and requirement (anaemia, hyperthyroidism)
Congestive Heart Failure (CHF) Mechanisms
- ventricle cannot relax, fill with blood (diastolic failure)
- ventricle cannot contract, eject blood (systolic failure)
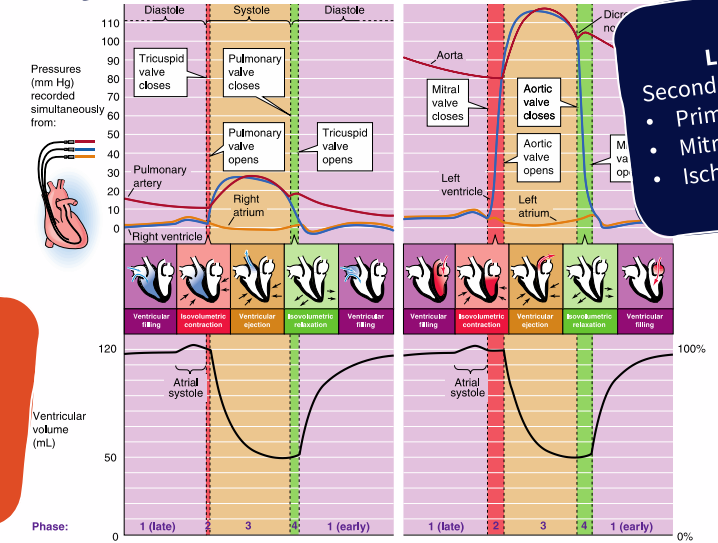
Congestive Heart Failure (CHF): Secondary to other conditions
LEFT-SIDED FAILURE:
- Secondary to: Primary myocardial disease, mitral or aortic valve disease, ischaemic heart disease
.
RIGHT-SIDED FAILURE:
- Secondary to: left sided heart failure, Primary pulmonary disorders (rare)
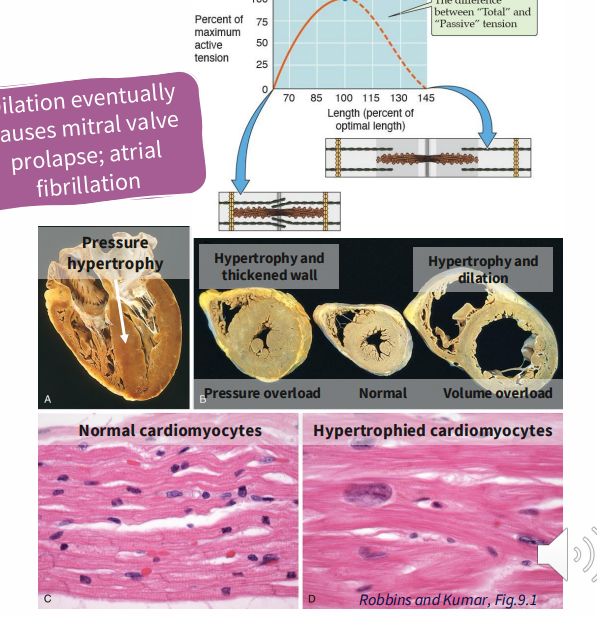
Congestive Heart Failure: Compensation
- Sympathetic nervous system activation e(e.g adrenaline increases heart rate, contractility)
.
FRANK-STARLING MECHANISM:
- larger volume pumped, dilates heart
- increased contractility, stroke volume
- actin-myosin cross-bridges at optimal length generate greater force
.
STRUCTURAL CHANGES:
- hypertrophy
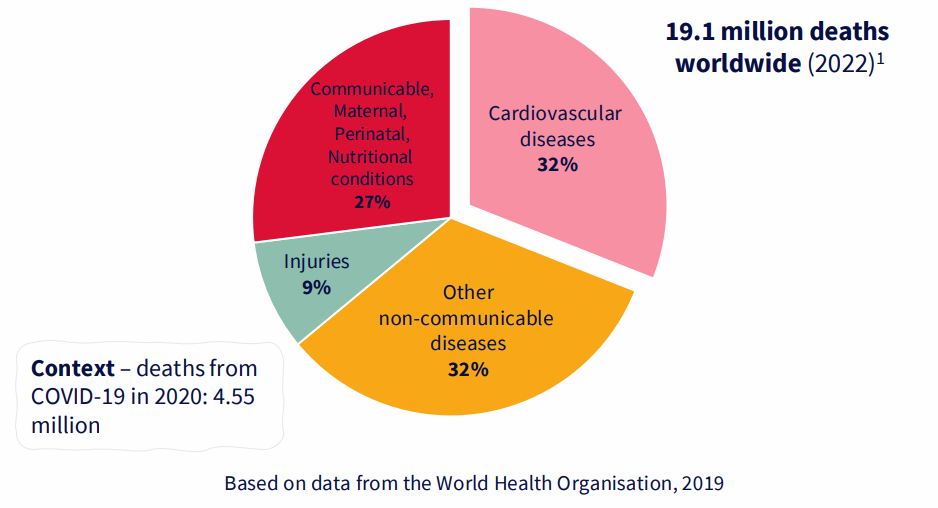
CVD is the leading cause of death in the world
DIAGRAM ON SLIDE 28
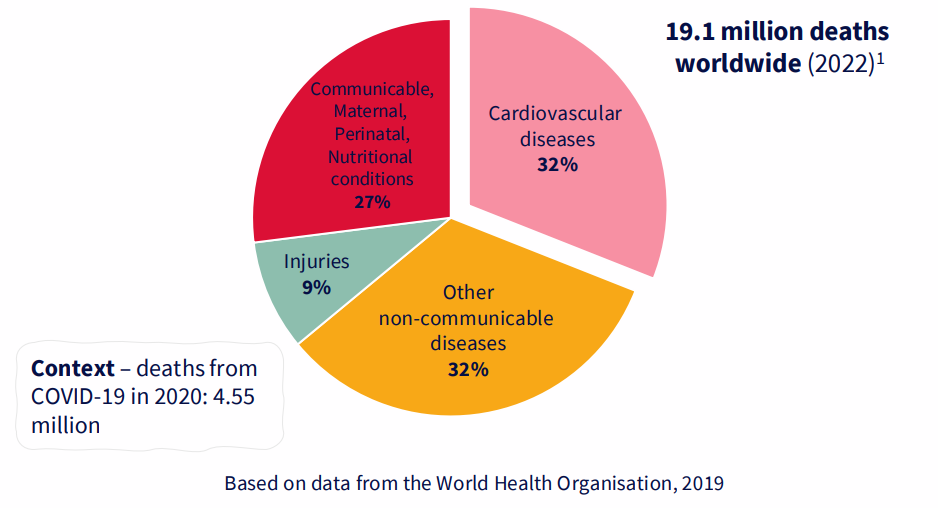
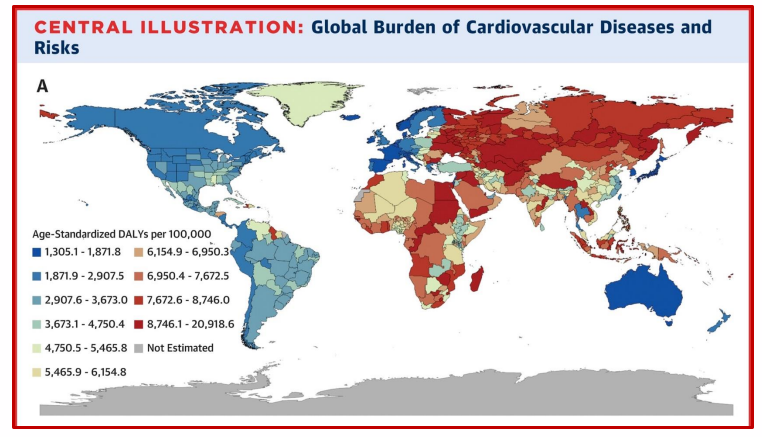
Major cause of morbidity and mortality globally
- 75% in low and middle income countries
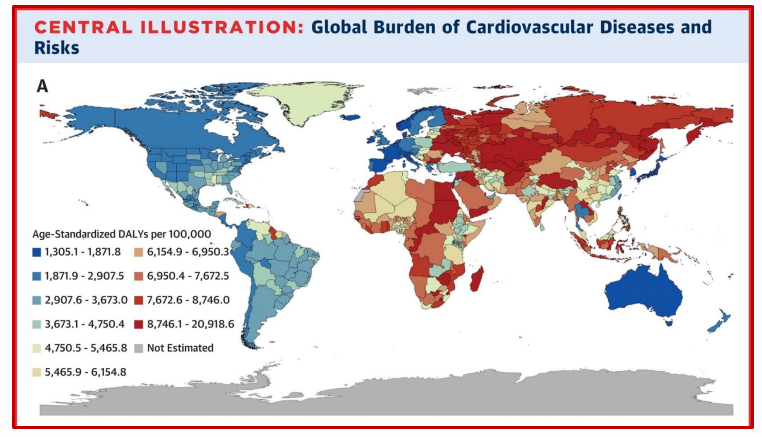
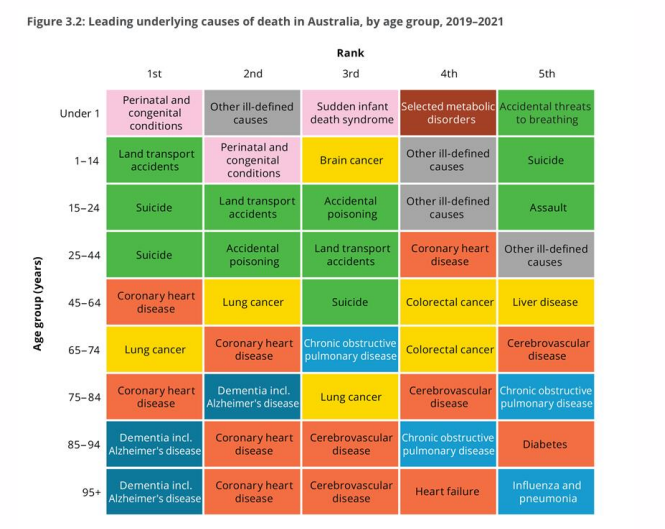
Mortality due to CVD increases with age
DIAGRAM ON SLIDE 30
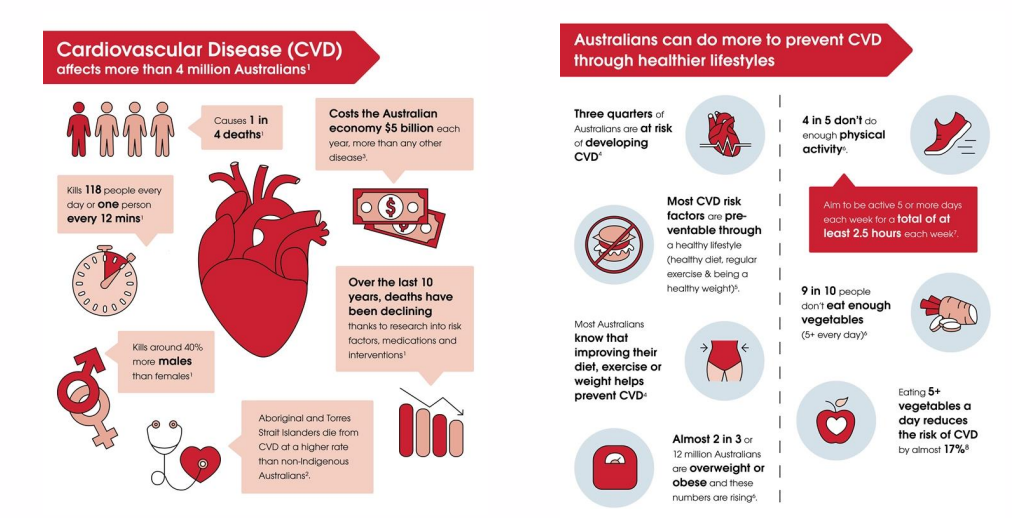
Cardiovascular disease in australoa
DIAGRAM ON SLIDE 31
About 90% of CVD is preventable
THE RISK FACTORS CAN BE AVOIDED:
- high blood pressure
- smoking
- type 2 diabetes
- lack of exercise
- obesity
- hyperlipidaemia
- high blood cholesterol
- excessive alcohol consumption
.
ALL SHARED CAUSATIVE FACTORS WITH:
- heart disease
- stroke
- cancer
- diabetes
- respiratory disease
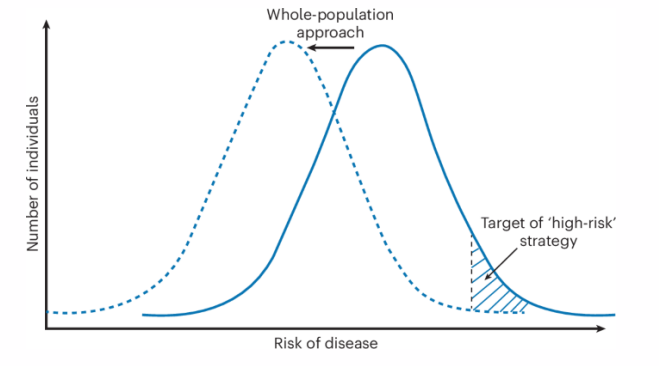
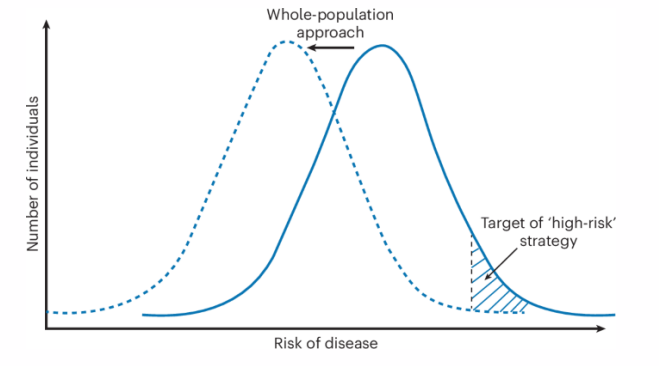
CVD and public health
- Target population at as whole, and high risk populations with appropriate strategies
- overall aim is to shift population out of the high risk category
Prevention of CVD through reducing modifiable risk factors
- the rates of ischemic heart disease have been decreasing dramatically since the 1980s
EXAMPLE: in the UK:
- 42% decrease is due to treatment (11% secondary prevntion (catching it early), 13% heart failure treatment, 8% initial treatment of acute myocardial infarction and 3% ypertension treatment)
.
- 58% is due to population-wide risk factor reductions
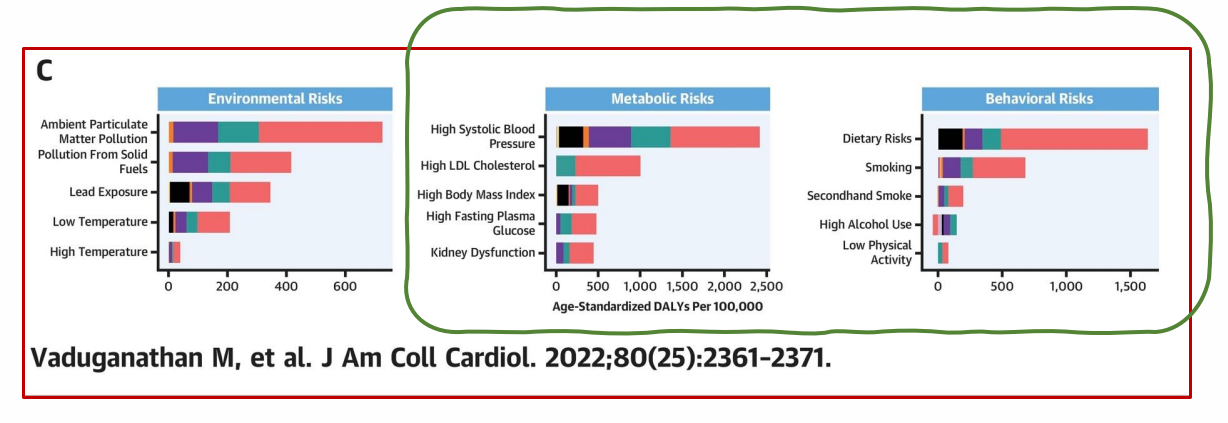
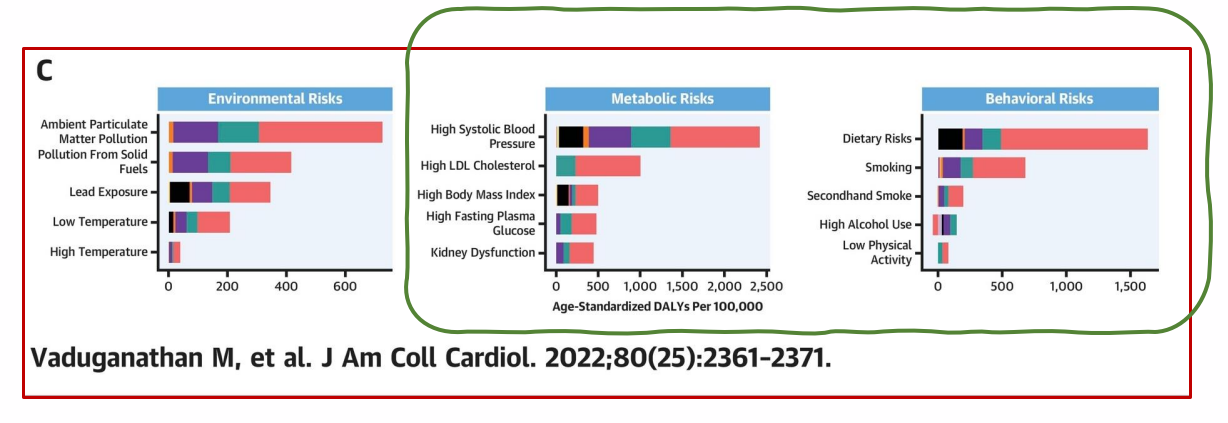
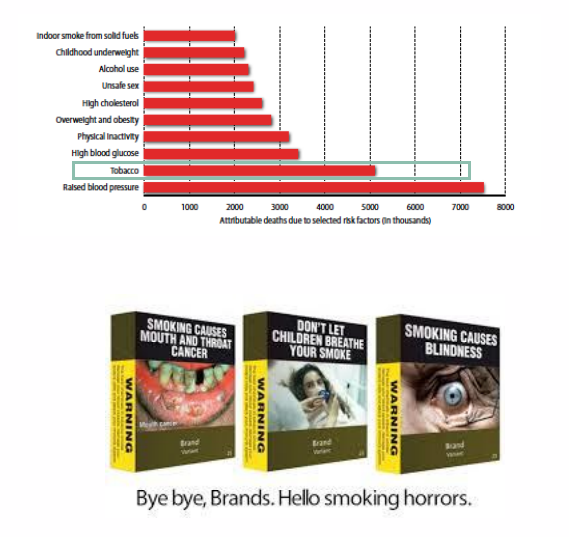
Risk factors for CVD
DIAGRAM ON SLIDE 35
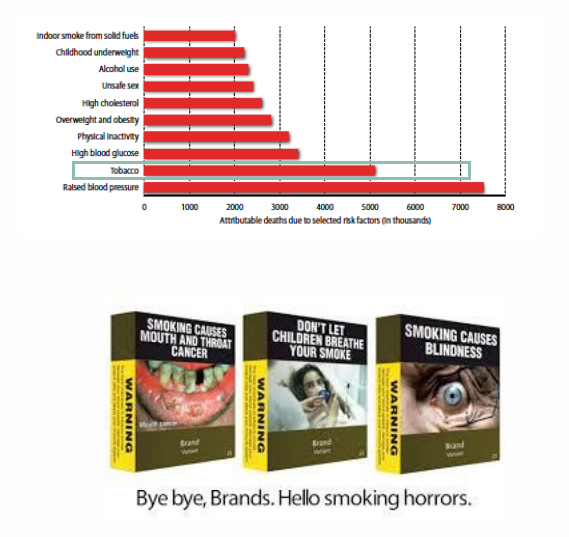
Tobacco use is an avoidable risk factor
CONTRIBUTES TO:
- myocardial infarction
- stroke
- sudden death
- heart failure
- aortic aneurism
- peripheral vascular disease
.
AIMS:
- reduce smoking and reduce second-hand smopke
Alcohol and CVD
- 14% of alcohol attributable deaths are due to CVD and diabetes mellitus
- direct casual relationship between level, patterns of alcohol consumption and CVD
- binge (episodic) drinking associated with increased risk of CVD
- damage heart msucle - risk of stroke, cardiac arrhythmia
Physical Inactivity and CVD
- insufficient physical activity is the 4th leading risk factor for mortality
- 3.2 million deaths each year attributed to insufficient physical activity
- 20-30% increase risk of all-cause mortality vs those who engage in 30 min of moderate activity
.
MECHANISM: improves endothelial function
- enhances vasodilation, vasomotor function in blood vessls
- effect on CVD partially through intermediate risk factors (glycaemic control, improved BP, lipid profile, insulin sensitivity)
CVD, atherosclerosis and modifiable risk factors (SUMMARY)
DIAGRAM ON SLIDE 40