Large Intestines
1/55
Earn XP
Description and Tags
Celiac Disease, IBD, colitis, toxic megacolon, IBS
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
Celiac Disease (Sprue, Celiac Sprue, Gluten enteropathy)
A permanent dietary disorder characterized by an inappropriate immunologic response to gluten that results in diffuse damage to the proximal small intestines with malabsorption of nutrients and extra-GI symptoms (close association with the human leukocyte antigen (HLA) DR3-DQ2 and/or DR4-DQ8 gene locus)
Diarrhea, steatorrhea, weight loss, abdominal distention, weakness, muscle wasting, growth retardation
Celiac symptoms for children under 2
chronic diarrhea, dyspepsia, flatulence, malasborption
Celiac symptoms for children and adults
Fatigue, rash, depression, iron deficiency anemia (pallor), osteoporosis (Vitamin D, calcium), short stature, delayed puberty, amenorrhea, reduce fertility, Easy bruising (vitamin K), loss of muscle/subcutaneous fat (calorie deficit), hyperkeratosis (vitamin A), peripheral neuropathy, ataxia, encephalopathy (B1, B12, Vitamin E)
Extra-intestinal symptoms of celiac
dermatitis herpetiformis
A pruritic, erythematous, maculopapular rash the forms over extensor surfaces of extremities, trunk, scalp, and neck associated with Celiac disease

IgA tTG (preferred), EMA-IgA, CBC, CMP, Endoscopic mucosal biopsy of proximal duodenum (confirmatory)
45 y/o female presents to the clinic for diarrhea. She states that it has been going on for about a month and she has lost some weight. On a physical exam you note dermatitis herpetiformis. What labs do you want?
3-12 months on a gluten free diet
While the IgA tests and the biopsy are great and all, when are you going to get false negatives
NO GLUTEN - ur done (if you relapse you get severe rebound symptoms); steroids and immunomodulators for refractory symptoms, Larazotide acetate (approved for accidental gluten exposure)
45 y/o female presents to the clinic for diarrhea. She states that it has been going on for about a month and she has lost some weight. On a physical exam you note dermatitis herpetiformis. Labs are as follows MCV low, MCHC low, Hct low, RBC low, Hgb low, Positive IgA-tTM and biopsy. What is your treatment plan?
intestinal lymphoma, cancers of the mouth, pharynx, and esophagus
Patients with celiac disease that aren’t gluten free OR have refractory symptoms have a higher risk for
Poor (5yr = 40-50% due to malabsorption issues)
For refractory celiac symptoms, how’s the prognosis?
IBS, IBD, gastroenteritis, milk intolerance, gastrinoma hypersecretion, carcinoid syndrome
DDx for celiac
Ulcerative colitis (UC), Crohn Disease (CD)
Types of inflammatory bowel disease (IBD)
15-40, 50-80
Age distribution of IBD
Genetics, FHx (25% have 1st degree relative with it), NSAID use, cigarettes (increase with crohns, decrease UC), diet high in processed, fried, sugary foods (CD), obesity (CD)
Risk factors for IBD
Crohn’s Disease (CD)
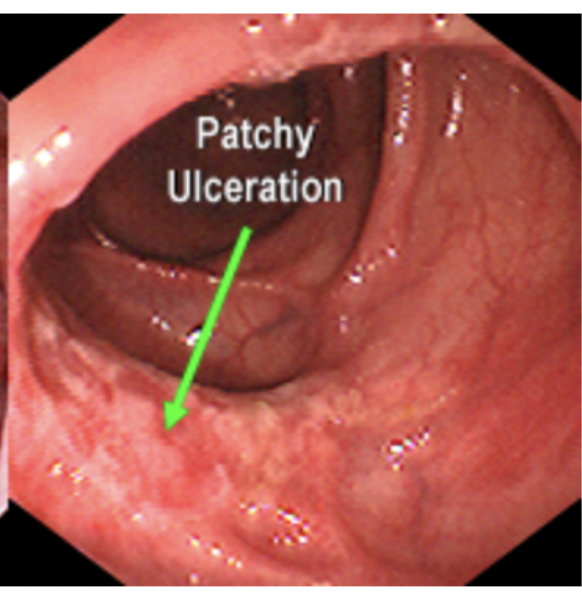
An insidious, chronic inflammatory conditions with transmural inflammation and SKIP lesions most commonly found in the ileum and proximal large intestine but can involve the mouth to anus
arthritis, uveitis, iritis, episcleritis, erythema nodosum, pyoderma gangrenosum, primary sclerosing cholangitis, thromboembolism, hypercoag, kidney stones, pulmonary complications
Extra intestinal manifestations of CD
abdominal pain, diarrhea (with or without gross bleeding - usually without), fatigue, weight loss
Cardinal Symptoms of CD
CMP (electrolytes), CRP and ESR (not specific but sensitive), Stool studies (show fecal leukocytes, calprotectin or lactoferrin), CBC (leukocytosis, anemia), Colonoscopy (1st line), CT or MR enterography
35 y/o female presents to the clinic for chronic diarrhea and abdominal pain. She notes that she has been so tired lately and canceling plans because she is worried about making it to the bathroom. She also reports that she has lost 10 lbs in the last few weeks. On physical exam, you note the RLQ is tender, wheezing in both the lungs, bilateral eye redness, and red nodular areas on the shin. What diagnostics you want?
severe, acute cases (no perf in this house)
When are we NOT doing a colonoscopy in CD or UC
Small, frequent meals that aren’t fatty, maintain proper hydration
Diet for Crohn’s Disease
Start with PO budesonide (or mesalamine), Maintain with PO mesalamine
35 y/o female presents to the clinic for chronic diarrhea and abdominal pain. She notes that she has been so tired lately and canceling plans because she is worried about making it to the bathroom. She also reports that she has lost 10 lbs in the last few weeks. On physical exam, you note the RLQ is tender, wheezing in both the lungs, bilateral eye redness, and red nodular areas on the shin. Colonoscopy demonstrates skip lesions of transmural inflammation of the ileum and proximal colon. Let’s say its mild to moderate - what is your treatment plan?
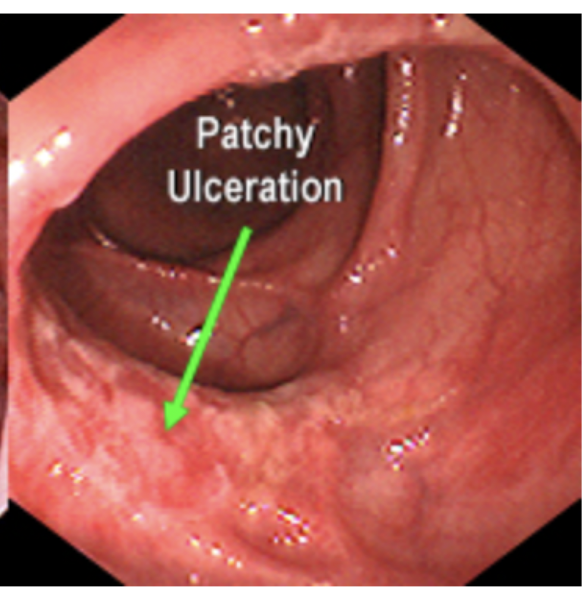
Start with PO prednisone (or PO sulfasalzine), maintain with sulfasalzine
35 y/o female presents to the clinic for chronic diarrhea and abdominal pain. She notes that she has been so tired lately and canceling plans because she is worried about making it to the bathroom. She also reports that she has lost 10 lbs in the last few weeks. On physical exam, you note the RLQ is tender, wheezing in both the lungs, bilateral eye redness, and red nodular areas on the shin. Colonoscopy demonstrates skip lesions of transmural inflammation of the left colon. Let’s say its mild to moderate - what is your treatment plan?
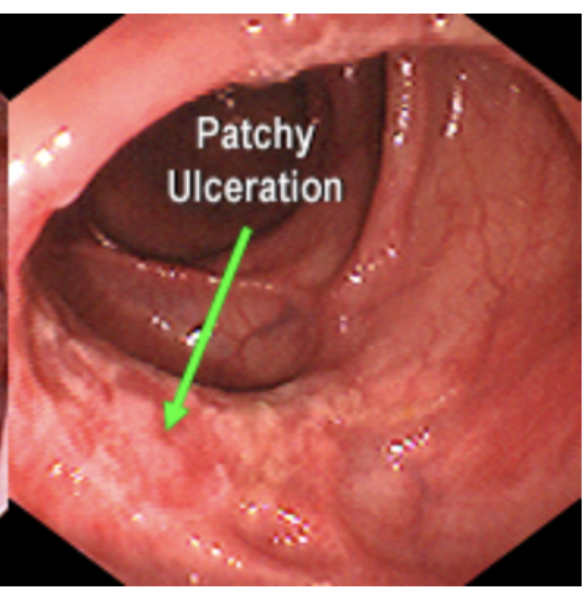
Start with Infliximab (anti-TNF) + methotrexate maybe prednisone; Maintain with Infliximab, maybe surgery
35 y/o female presents to the clinic for chronic diarrhea and abdominal pain. She notes that she has been so tired lately and canceling plans because she is worried about making it to the bathroom. She also reports that she has lost 10 lbs in the last few weeks. On physical exam, you note the RLQ is tender, wheezing in both the lungs, bilateral eye redness, and red nodular areas on the shin. Colonoscopy demonstrates skip lesions of transmural inflammation of the large intestine. Let’s say its moderate to severe - what is your treatment plan?
refractory symptoms, abscess formation, massive bleeding, fistulas, obstruction
Indications for surgery in CD - 60% recurrence rate within 1 yr
IBS, UC, Gastroenteritis, diverticulitis, appendicitis, colitis, proctitis, ischemic bowel, food intolerance, cancer
DDx for CD
Ulcerative colitis (UC)
Chronic inflammatory condition limited with relapsing and remitting inflammation limited to the mucosal layer of the colon (involves rectum and extends proximally)
CBC (anemia), ESR, CRP, CMP (albumin, electrolytes - dehydration), Stool studies (Fecal leukocytes, calprotectin, lactoferin), Colonoscopy (1st line), Sigmoidoscopy
45 y/o female presents to the ER for blood diarrhea and abdominal cramping. She also notes that she has had a hard time making it to the bathroom. On physical exam you note LLQ tenderness and gross blood on DRE. Vitals are stable with the exception of 104 bpm, 104/74, and 99.8 temp. What diagnostics you want?
Topical and PO mesalamine → if fail steroids → if fail anti-TNF
45 y/o female presents to the ER for blood diarrhea and abdominal cramping. She also notes that she has had a hard time making it to the bathroom. On physical exam you note LLQ tenderness and gross blood on DRE. Vitals are stable with the exception of 104 bpm, 104/74, and 100.8 temp. Labs are as follows HCT low, ESR up, albumin Low. Colonscopy demonstrates diffuse mucosal inflammation that looks like cobblestones. She’s moderate at least so what’s your treatment plan?

Topical mesalamine
45 y/o female presents to the ER for blood diarrhea and abdominal cramping. She also notes that she has had a hard time making it to the bathroom. On physical exam you note LLQ tenderness and gross blood on DRE. Vitals are stable - 95 bpm. Labs are as follows ESR up. Colonscopy demonstrates diffuse mucosal inflammation that looks like cobblestones. She’s mild at least so what’s your treatment plan?

perforation, colon infection, toxic megacolon, colon cancer
Complications for UC
total proctocolectomy (requires ileostomy)
What can cure UC?
CD, IBD, Gastroenteritis, diverticulitis, appendicitis, colitis, proctitis, ischemic bowel, food intolerance, cancer
DDX for UC
Colitis
A over-arching general term used to describe infections and/or inflammation of the colon (includes CD, UC, and infectious etiologies)
Immunocompromised (HIV, IBD, steroid use), Recent Abx usage (C. Diff), ingestion of undercooked or incorrectly prepared foods, traveled to endemic areas (giardiasis), receptive rectal intercourse
Risk factors for infectious colitis

CBC (WBCs), Stool studies (leukocytes, C. diff toxins, cultures, PCR), STI related labs (herpes IgM, infectious swab)
26 y/o male presents to the ER for loose diarrhea and abdominal pain. He states that he is currently taking clindamycin for his acne. Physical exam reveals abdominal tenderness. What diagnostics do you want queen?
Oral Vanc/Metro/fidaxomicin(if you got money)
26 y/o male presents to the ER for loose diarrhea and abdominal pain. He states that he is currently taking clindamycin for his acne. Physical exam reveals abdominal tenderness. Labs are as follows leukocytosis (15K) and stool is positive for C. Diff (but your nurses already knew that). What is your treatment plan?
treat the underlying so Abx, antivirals, STI precautions, discontinue any contributory medications
Game plan for infectious colitis - general
Toxic megacolon
A potentially life-threatening complication of IBD or infectious colitis that results in ileus, dilation, and sepsis
hypokalemia, Meds (anti-motlity agents, anticholinergics, opiates, antidepressants), barium enemas, colonoscopy
Etiology of toxic megacolon
Colon dilates → blood supply is limited → Susceptibility to infection increases
Pathogenesis of toxic megacolin
CT scan, abdominal xray series, DO NOT DO A COLONOSCOPY OR SIGMOIDOSCOPY, CBC, CMP, FOBT
58 y/o male presents to the ED for AMS. His wife reports that he has had diarrhea all day and she thinks she saw blood in the toilet. The patient is clutching his abdomen and screaming when you hip check the bed, he screams louder. The abdomen is distended. Vitals are as follows 103.6 rectal temp, 145 bpm, 98/60. What diagnostics you want?
NPO with IV hydration (maybe TPN), NG decompression, roll patient from side to side, Abx, surgery histamine-2 blockers or proton pump inhibitors for ulcer prophylaxis
58 y/o male presents to the ED for AMS. His wife reports that he has had diarrhea all day and she thinks she saw blood in the toilet. The patient is clutching his abdomen and screaming when you hip check the bed, he screams louder. The abdomen is distended. Vitals are as follows 103.6 rectal temp, 145 bpm, 98/60. Labs reveal leukocytosis and anemia, FOBT is positive. What is your treatment plan?
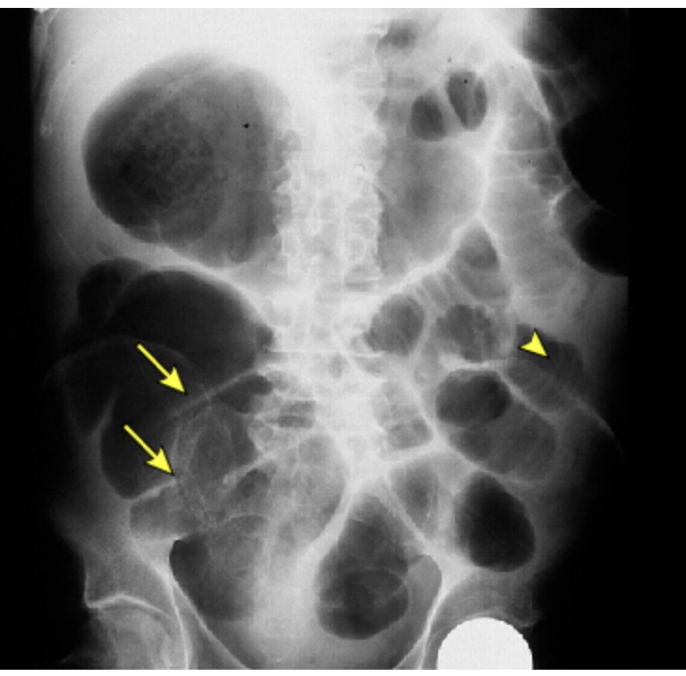
uncontrolled bleeding, perforation, worsening toxicity or dilation, necrosis, or full-thickness ischemia, intra-abdominal hypertension or abdominal compartment syndrome, clinical signs of peritonitis or worsening abdominal examination despite adequate medical therapy, and end-organ failure
Indications for Surgery with toxic megacolon
Radiographic evidence of colonic dilation (6 cm+), + 3 of these: fever, tachycardia over 120, PNMs over 10,500, anemia + 1 of these: dehydration, AMS, electrolyte disturbances, hypotension
Diagnostic Criteria for Toxic megacolon
Irritable Bowel Syndrome (IBS)
An idiopathic, functional GI disorder that is characterized by chronic or recurrent symptoms with no evidence of structural or biochemical abnormalities
3+ months of abdominal pain/discomfort at least once a week + 2 of these: relief of symptoms with bowel movements, change in stool frequency, change in stool form
Diagnostic criteria for IBS
abnormal motility, visceral hypersensitivity, enteric infection, psychosocial
Etiology of IBS
NOTHING - clinical diagnosis
25 y/o female presents to the clinic for chronic abdominal cramping in the lower abdomen. She states that it has not disrupted her sleep but she is taking laxatives multiple times a week to help with bowel movements. She is kinda tender on exam but nothing serious. What diagnostics do you want?
W/diarrhea, W/constipation, Mixed
IBS classifications
Nocturnal diarrhea, hematochezia, weight loss, reported fever, FHx of cancer, IBD, or celiac, onset of symptoms 40+
Red flags for IBS which mean we need labs and a colonoscopy
Exercise and increased dietary fiber (1st line), reassurance, education, support, Lubriprostone or linaclotide, probiotics
25 y/o female presents to the clinic for chronic abdominal cramping in the lower abdomen. She states that it has not disrupted her sleep but she is taking laxatives multiple times a week to help with bowel movements. She is kinda tender on exam but nothing serious. What is your management plan?
TCAs, SSRIs
Second line for IBS
Avoid fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs)
Recommended diet for IBS
rifaximin
Diarrhea specific management of IBS
IBD, gastroenteritis, cancer, hyper/hypothyroidism, parasites, malabsorption syndrome
DDx of IBS
Most learn to cope, no long term sequalae
Prognosis for IBS