PSYCH 257 (Psychopathology) EXAM 1
1/97
Earn XP
Description and Tags
Weeks 1-4
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
Etiology
origins, causes of something (disorders) - The origins are most commonly:
Supernatural
Biological
Psychological
Social
How does etiology effect the way that we view mental illness
Over history, theories about etiology = treatment of mental illness AND vice versa
eg., if antidepressants treat depression does that mean depression is biological? aka a chemical imbalance - no bc you can treat depression without understanding the root cause
Supernatural causes of mental health issues + treatment methods (Trephination)
Used to be the dominant theory of disorders
Causes: Spirits, demons, divine punishment, witchcraft
Treatment methods:
Exorcisms: rituals that expel spirits
Trephination: Drilling holes into the skull to release the evil spirits
Prayer and other religious rituals: EG appealing to divine intervention (miracles)
Hippocrates:
Considered Father of Western Medicine
One of the first to propose that disease (including mental illness) was due to natural no supernatural causes
Origins of biopsychosocial (using social, biological and psychological factors) view over supernatural views
Middle ages understanding of Mental Illness (Greece) - asylum model
Biological Understanding - mental illness is a physical issue in the body or the brain
This resulted in the “asylum model”: Blood letting, squalid conditions, chaining to walls
What did St.Vincent de Paul purpose in the middle ages as a result of asylum model
Natural environment
People shouldn’t be locked up – the more connected people were with their environment the better they would heal
Enlightenment period: understanding of mental Illness (Psychogenic)
Psychogenic Model: psychological factors like stress, trauma or emotions were seen as a possible cause not just biological/supernatural
This led to the hospital model: placed in hospitals rather than asylums and treatment is more scientific - observation, etc
Continue to advocate for humane treatment of patients
Wilhelm Wundt & Lightner Witmer (his student)
Experimental psychologist who founded the first psychology laboratory in Germany
Focused on specifically perception and sensation laying groundwork for clinical interventions
Lightner Witmer: Student who founded first psychology clinic
Emphasized the application of psychological principles for treatment purposes
World Wars I & II effect of Psychology
Pressing need to treat veterans with trauma from wars – only rly bad cases were treated
Better diagnostic methods and therapeutic approaches - increased PTSD
The U.S. Army's use of psychological testing (clinical assessments) (psychologically fit)
Psychotherapy Emerges – talk therapy
Francis Sumner: Father of “Black Psychology”
Albert Sidney Beckham: school psychology
Francis Sumner
First Black man to earn a PhD in Psychology (1920)
Black Psychology: Focuses on understanding and addressing the mental health and experiences of Black people through a culturally relevant and empowering lens
Advocated for addressing racial bias in psychological research and promoting diversity in education - How does marginalization effect mental health
Albert Sidney Beckham
Established the first psychological clinic in a public school (guidence councilors are there bc of him)
social, emotional, and environmental factors on academic performance
Inez Beverly Prosser: First Black woman to earn a PhD in Psychology
Braulio Alonso: Counseling psychology for Latinx student
Inez Beverly Prosser:
Studied the impact of segregated vs. integrated schools on Black children’s self-
esteem and academic achievement
Advocated for safe and nurturing educational spaces to support Black students' mental health and development
Braulio Alonso:
Advocated for educational equity and increased mental health access for marginalized and underserved communities
Emphasized the need for culturally competent counseling approaches to address systemic inequalities in education
Psychoanalytic Theory (Freud and Breuer)
Focused on the unconscious mind and how hidden conflicts shape behavior - repressed memories and unsolved conflicts
Etiology: Unconscious, Intrapsychic conflicts between different structures of mind
The things that you do are driven by underlying traits not from our own agency
Treatment:
Hypnosis
Free Association: whatever comes to mind without filtering (finding repressed memories)
Catharsis: Reliving and releasing repressed traumas or emotions
Freud’s view of the human mind - Mental Iceberg and egos
He said that mental disorders were cause by conflicts between different parts of the mind (Id: Primal desires like pleasure, Ego: Balances id and superego, Superego: Moral values and societal expectations)
His view of the mind: *not fully in control of your actions
conscious: thoughts and perceptions
subconscious: memories and knowledge
unconscious mind: fears, unacceptable sexual desires, immoral urges, selfish needs
Carl Rogers: Humanistic theory (UGE)
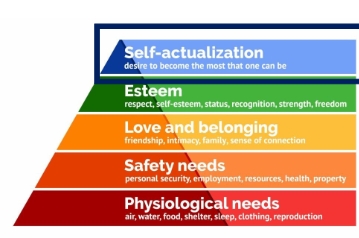
This draws on maslow’s higharchy of needs: humans have a natural drive toward self-actualization (becoming the best version of themselves)
Opposite of Freud: The client is the expert, they just need support
Treatment: Person centered
Unconditional Positive Regard: Accept client no matter what so they feel safe and valued
Empathy: Validate feelings
Genuineness: Be sincere (not overly clinical)
You are a humanistic therapist who practices in the style of Carl Rogers. You are in a session with a client who is reporting an increase in anxiety over the past week. The most likely therapeutic statement you would make to the client is:
It sounds like it’s been a really hard week, I can understand how that would be distressing for you.
Behavioral Model - Skinner and Watson
Says that all behaviours are learned through interactions with environment and disorders are the result of learned behaviour
EG: being afraid of dogs bc you associated dogs with getting bitten
Operant conditioning (skinner)
Behaviors are shaped by reinforcement (punishment and reward)
Positive reinforcement strengthens behaviors, while punishment discourages unwanted behaviors.
Observational learning
watching and imitating the behavior of others (Daughter immitating bahaviours of grandfather bc she sees that he succeeds)
Classical conditioning (Pavlov)
Creating associations between stimuli can lead to learned responses (Dog & metronome)
Key Point: Behavior is learned through repeated associations between stimuli
Mind is considered a “black box” all we have to do is condition we can manipulate learning despite what is happening in the brain
Neg reinforcement (alarm clock in the morning)
Unconditioned stimulus and response vs neutral and conditioned stimulus and response
Unconditioned Stimulus (e.g., food) naturally triggers
Unconditioned Response (e.g., salivation – naturally occurring)
Pairing Stimuli: A Neutral Stimulus (e.g., bell) is repeatedly paired with the Unconditioned Response (e.g., offer dog food and ring bell at the same time triggering salivation)
Eventually the Neutral Stimulus (e.g., bell) becomes a Conditioned Stimulus
The Conditioned Stimulus (e.g., bell) now triggers a
Conditioned Response (e.g., salivation) now triggers a...
Unconditioned Stimulus (e.g., food) present
Classical conditioning in mental health
Development of phobias
Claustrophobia:
Child goes on an elevator with parent (NS) = parent is fearful and has a panic attack on elevator, inciting fear in the child (US) = Child now afraid of elevators (CR)
Dog Phobia:
Child takes dog for a walk (NS) = Dog sees squirrel and drags child down street (US) = Child now afraid of dogs (CR)
Extinguishing/extinction
A treatment using the behavioral model:
Unpairing a conditioned stimulus (dogs) with an unconditioned stimulus (being dragged down the street) to lessen conditioned response (fear)
The more that you are exposed to dogs and not injured the less scared they will be
alcoholics and the pill that takes away euphoria
Systematic desensitization
Slowly introducing stimulus to reduce intensity of response
Treatment example: Spider phobia
You post a picture on Instagram and get a lot of likes from your followers. This makes you
want to post more pictures. What type of conditioning is this
Operant
Cognitive disortions
• Interpretations of events that are not realistic or accurate (Thinking of the worst outcome)
Disorders are a result of biased/distorted thoughts
Treatment
• Identify biased thoughts and challenge them with evidence
The 3 D’s for Defining psychological abnormality
*all three must be present* - what is normal?
Dysfunction: cognitive (thinking), emotional (feeling), or behavioral (acting) processes are disrupted *impacts their ability to function effectively in daily life. (dieting vs eating disorder)
Distress/Impairment: Feeling upset about the problem (may not always occur aka narssistic personality disorder) and interfering with functioning
Deviance: Response is not typical or culturally accepted - deviating from the norm (these are different depending on the culture)
Syma’s mood has been low for the past month. She has been thinking that she has no positive qualities and will never amount to anything in life. Which of the 3 D’s does Syma’s thinking illustrate?
Dysfunction
Disorders are never…
Unidimensional (people thinking that one specific thing leads to a disorder)
Critical mothering causes anorexia
Lack of self-control causes substance abuse problems
Chemical imbalances cause depression
Genes cause schizophrenia
Video games cause violent behaviour
Coddling children causes narcissism
Interconnections and feedback loops
Results of socital stressors
• Poor familial relationships > feeling shameful about self, not good enough
• Low self-esteem > not socializing
• Not Socializing > added grief over best friend, increased isolation
• Grief and loneliness > reduced focus at work, academic and financial stress
The biopsychosocial model
Holistic approach to understanding mental and physical health:
Biological factors: Genes, Brain structures, Neurotransmitters
Psychological factors: Thoughts, emotions, behaviors
Social factors: Relationships, Interpersonal (childhood), social structures like poverty and discrimination
Mental illness is a system of complex interactions (you cannot consider one in isolation)
Treating one component of the system will likely influence the others (Improving self-esteem = wanting to spend more time with others)
Biological Treatment Implications
Asses medical contributors like hormonal imbalances or liver problems
Explore the use of medications like SSRIs
Encourage general physical health - regular physical activity improving mood
Psychological Treatment Implications
Therapy, support groups - guidance:
Increase daily pleasurable activities
Challenge negative thinking about self and develop self-compassion
Develop problem-solving strategies to manage academic and job-related stress
Social Treatment Implications
Gradually reconnect with friends to foster supportive relationships
Engage with a broader community to find others with common interests
Gene studies with twins
The influence of genes on mental illnesses were measured on twins as they share all genes:
If one twin has a disorder there is roughly 50% chance the other will as well
Environmental factors influences the expression of different genes – may lay dormant even if they have the predisposition for a illness
Disorders are polygenetic
no individual genes have been identified relating to any major psychological disorders (exception - Alzheimer’s)
Diathesis-stress model
Environmental stress interacts with genetics to predict whether a person will experience a psychological disorder
Genetic vulnerability (diathesis) x stress = psychological disorders
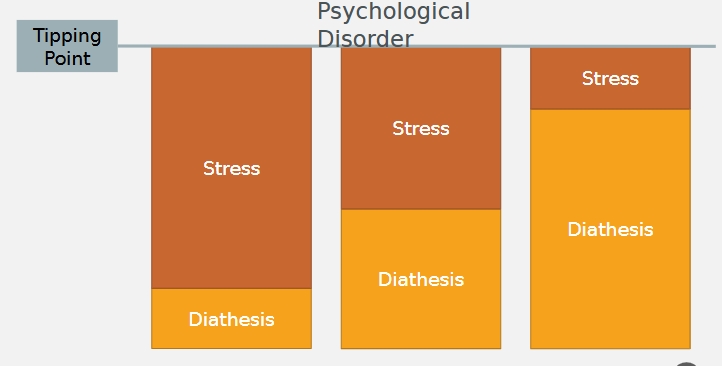
Predisposing vs precipitating stress
Predisposing Stress (Long-Term Risk) – Makes someone more vulnerable over time.
A child who grows up in a stressful home (neglect, abuse) may be more likely to develop anxiety or depression as an adult.
Precipitating Stress (Immediate Trigger) – Directly causes a mental health issue to appear.
A soldier returning from war might develop PTSD after a single traumatic event.
How do genes and environmental factors interact to influence the development of mental disorders?
Diathesis-stress model
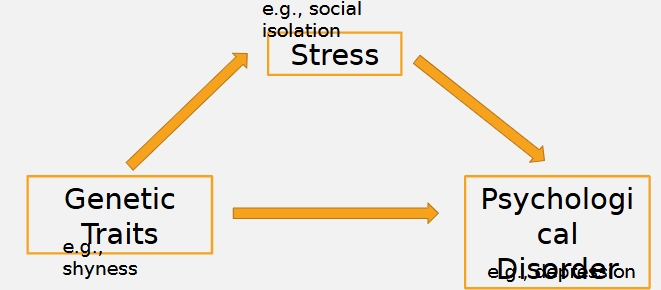
Are diathesis and stressful environment independent?
No, they work together
Reciprocal Gene-Environment Model
Genes shape our environment which then reinforces genetic tendencies
Genes influence personality and behavior → This makes people more likely to experience certain stressful situations.
genetic traits might cause more stress or experience things as more stressful (shyness)
Epigenetics
Environmental factors can modify the traits we pass along to our offspring, even if the genes themselves do not change
Genes are turned on/off by cellular material outside of genome (“epi”)
Passed down to next generation(s) - Biological evidence of the effect of generational trauma
Stress from previous generations is passed down to future generations through the epigenome
Your child or grandchild can have similar epigenomes
Imagining epigenetics as a recipe book
Epigenetics is like adding sticky notes to the book that say things like, 'Add more sugar!' or 'Leave out the salt!'
These sticky notes don’t change the recipe itself but change how it’s followed
Stressful experiences, like feeling scared or sad a lot, can add sticky notes to DNA that say, 'Be extra alert!' or 'Stay cautious!'
sticky notes can be passed down through generations, affecting how children’s DNA is read, even if they didn’t experience the same stress
Frontal Lobe and its dysfunctions
Not fully developed until ~25 years old!
Executive functions: Planning, problem-solving, organizing thoughts. (lower with alcohol)
Decision-Making
Short-Term Memory
Impulse Control – (like stopping yourself from saying something rude).
Emotional Regulation – Keeps emotions in check so you don’t overreact.
Dysfunctions:
Dysfunctions linked to depression, anxiety, ADHD, and other mood disorders.
Lymbic System
“emotion center”
Includes structures like the amygdala, hippocampus, and hypothalamus.
Central to emotional regulation, fear response, and memory formation, phobias = overactive limbic system specifically amygdala.
Imbalances associated with anxiety disorders, PTSD, and depression.
Serotonin
Regulates mood, appetite, and sleep.
Low levels often associated with depression
Dopamine
• Involved in reward, motivation, and pleasure systems.
• Dysregulation linked to schizophrenia, addiction, and Parkinson's disease.
Norepinephrine
Influences alertness, arousal, and the stress response.
Imbalances can contribute to anxiety disorders and depression.
Neuroplasticity
Brain's ability to adapt, rewire, and change in response to experiences, learning, and injury. It means that the brain is not fixed
“rewire the brain”
Wiring is “plastic”
How do psychological interventions change the brain?
Change Negative Thought Patterns – Therapy can help create new brain pathways that replace negative thinking with healthier thoughts.
Strengthen the Prefrontal Cortex – This part of the brain helps with self-control and decision-making. Strengthening it improves emotional regulation.
Calm the Amygdala – The amygdala controls fear and stress responses. Therapy can reduce its overactivity, leading to less anxiety and stress.
SSRIs
(Selective Serotonin Reuptake Inhibitors) can increase serotonin levels, affecting mood and anxiety regulation.
Antipsychotic Drugs
modulate dopamine activity, essential for schizophrenia treatment.
Stimulants
used for ADHD to increase dopamine and norepinephrine in the brain
Benzodiazepines
fast-acting anxiety medications that enhance the effect of GABA, a neurotransmitter that inhibits brain activity.
A parent shows intense pride and joy toward her child when she performs well on an exam, but ignores her child and treats her coldly when she does not perform well. According to Rogers, this child’s needs would be thwarted because the parent showed
Conditional regard
Which model of psychopathology suggests that individuals with certain genetic predispositions (e.g., shyness) might experience more stressful situations, which in turn contributes to their likelihood of developing a psychological disorder?
The reciprocal gene-environment model
Why do we use a classification system for psychological disorders
Humans tend to categorize and classify our experiences to make sense of the world
Classification is a central element of all branches of science
Allows us to organize, describe and relate subject matter of our discipline
Pros and Cons of labeling experiences only as normative or disordered
Pros:
Taxonomy: Organizes presentations into meaningful groups - we have some sort of organization – this isn't just mental illness this is ______
Helps with communication – people will understand what it means to be on the spectrum (nomenclature)
Treatment and insurance, Social: Understanding of severity of difficulty (you can say you have depression and it is considered severe enough to get coverage
Cons: Labeling/stereotyping, Stigma-based discrimination
Not being allowed to reach their goals
Naming psychosis as “violent”
Stigma in work places and school
Categorical pros and cons - heterogeneity issues and boundary and threshold issues
Pros:
Simplifies communication
Easy research participant classification
Ease of administration in hospital settings – medical model says that you either have cancer or don’t and often people are diagnosed in this way with mental health but that is not good (needed for insurance)
Cons:
Heterogeneity issues: E.g., Depression may look very different for two different people (we cannot make that many general assumptions because it looked different)
Loss of important clinical information: Severity of symptoms (maybe someone has treatment resistant depression vs someone who is in their first episode and treated)
Boundary and threshold disputes: Arbitrary timelines/thresholds (“excessive worry” is up for subjective interpretations)
Dimensional Approach Pros and Cons - diagnostic reliability
Psychopathology is assessed using scales or dimensions (e.g., level of mood dysregulation, impulsivity)
Recognizes that different disorders often share overlapping symptoms
Focuses on the unique combination of symptoms and their intensity for each person
Pros: Diagnostic reliability & stability (problem)
Clinicians may disagree about whether diagnosis is present
Dimensional approach gives more leeway – can still describe someone’s symptoms without labelling
Eliminating boundary disputes (DBT being used for many different issues)
Cons:
Still requires cut-off points? - A problem for insurance uses and understandings
Still necessary for us to know the point at which someone needs help
Lack of agreement on dimensions
The DSM Approach (Prototypical appraoch)
Strengths:
Provides common language
Increases consistency across clinicians
Creates something that can be studied
Not biased towards one theory
Essential characteristics and non-essential variations (EG must have 3 our of the 5 symptoms)
Differential diagnosis – shows you the difference in overlap
Critisisms of the DSM 5 TR (test revision)
• Not consistent with scientific advances (changes to the side effects of ADHD)
• Over-influenced by drug industry
• Does not take whole person into account
• Limited use for psychotherapy
The DSM appropriates the medical model meaning there may be too much symptom focus
Uses categories (you either have it or you don’t)
Diagnosis can vary between doctors bc of overlapping symptoms
Text revisions to the DSM (Prolonged grief disorder)
Prolonged Grief Disorder: Intense and persistent longing or preoccupation with the deceased, causing significant distress and impairment in daily functioning, lasting for an extended period post-loss (couldn’t get a depression diagnosis if you were going through grief)
Inclusion of culturally sensitive language: Addresses issues like racism and discrimination in the context of mental health
Updated criteria for various disorders
Why do we conduct clinical assessments
Research reasons
Formulate diagnosis
Understand individual and Predict behaviour
Plan and narrow treatment
Evaluate treatment outcome
Help client understand, feel less ashamed
What does it mean when someone’s treatment makes them worse
Often this is a sign that it is working - its going to get worse before it gets better
Assesment tools: Relibility (inter-rater and test-retest)
Reliability – measurement consistency – two different types of reliability
Inter-rater: different observers should agree that a person’s behaviours/symptoms fits a certain diagnostic class – if two people were observing the same situation would diagnose the same thing
Test-retest: Taking a test multiple times should produce same results – if someone takes a test multiple times and get a similar score
Assessment tools: Validity and standardization
Validity – measurement accuracy
Degree to which a diagnosis accurately conveys to us something clinically meaningful about the person whose behaviour fits the category
Standardization - Guidelines for use, scoring, and interpretation of a psychological test that help ensure consistency – given to every person in the same way and rated in the same way
Assessment tools (physical exams, psychological tests, behavioural assessment, Psychophysiological Assessment , neuropsychological testing, Neuroimaging, clinical interviews)
Physical Exams – is the source of the issue a thyroid condition
Psychological Tests – asking friends or family to comment
Behavioural Assessment – have them do something and watch how they do it (often common in adhd and autism) - or having interactive conversations (look over there)
Psychophysiological Assessment – Examining how much someone is sweating or how fast their heart rate is going (when couples are having arguments)
Neuropsychological Testing – cognitive assessments like memory impairment or motor movements
Neuroimaging – MRI, Brain scans, CT scans done by clinical neuropsychologists
Clinical Interviews (patient, family) - having conversations with families – sticking to key points but letting conversation flow
Critiques of the example clinical interview (Anorexia)
Asking about particular numbers is a problem – asking about her period (must ask about how this effects the person)
Not checking on state of mind – only looking at problems specific to the disorder, what else was going on?
What is a diagnosis?
A clinical judgment about an individual's mental health condition based on observed symptoms, behaviors, and history
Purpose: Provide a common language for professionals and guide treatment
Identifies and labels psychological disorders using established criteria (e.g., DSM-5-TR, ICD-11)
Why are diagnosis a controlled act? Who can diagnose
Controlled Act: A task or procedure that is legally restricted to certain regulated professionals due to its potential for harm if performed incorrectly
requires specialized knowledge, training, and judgment
Psychiatrists, Clinical Psychologists, Nurse Practitioners, Physicians
How do psychologists determine a diagnosis?
Compile all collected data from various assessments
Synthesize Data: Identify patterns and cluster symptoms that may fit a condition
Compare to DSM 5 TR
Differential Diagnosis
Evaluate overlapping symptoms to rule out disorders that may present similarly (e.g., distinguishing between depression and bipolar)
Competence and volunteerism in research ethics
Competence: Must ensure participants have capacity to provide consent
Volunteerism: must ensure lack of coercion
Full Disclosure and Comprehension in Research ethics
Full disclosure: must provide all necessary information to enable participants to make an informed decision
Comprehension: must ensure that participants understand all possible risks and benefits of participation
Independent and Dependent Variable
IV = X
DV = Y
What is the impact of studying (IV) on test grades (DV)
Hypothesis:
• Researcher’s supposition about probable link between variables
• Starting point for further investigation
________ avoids sampling bias, experimenter bias, self selection bias and attrition bias (define all)
Random selection avoids
Sampling bias: When the sample doesnt represent that entire population
Experimenter bias: When a researcher unintentionally influences the results of a study due to their expectations or beliefs.
Self Selection bias: When participants choose to be part of a study (sampling bias)
Attrition Bias: certain participants drop out of a study in a way that affects the results.
Correlational Designs - r
Measuring the relationship between two variables without manipulating them
Measures Linear association
R tells us how well the variables move together: 1.0 = perfect positive correlation and -1.0 = perfect negitive correlation, 0 = no correlation
CORRELATION DOES NOT MEAN CAUSATION
Positive vs negative correlations - scatter plot graphs
Positive correlation: Line will point upwards to the right
Negitive correlation: Line will point upwards to the left
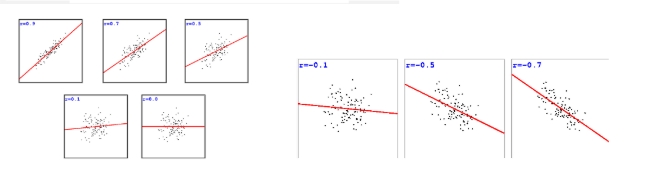
Non-linear association
Curved line - Correlations cannot meaningfully describe nonlinear relationships between relationships (weak or no r)
Manipulating the IV (experimental research) and control groups
IV: allows researchers to study cause-and-effect relationships, but ethics play a critical role in ensuring participant safety and avoiding harm. (cant have a child isolated)
Control groups: help with comparison but also must consider ethical responsibility - placebo groups - cant with-hold effective treatments from those who need it
Weaknesses and Strengths of experimental research
Pros: Allows for conclusions about causality (can show a cause and effect relationship)
Cons:
You need to make sure you achieve internal and external validity
Sometimes it is impossible or unethical to study certain things (testing effects of trauma)
Genie (Feral Child) is an example of what kind of study
Case study - possible third variables
Often results in many confounds
Foundation of early historic developments in psychopathology
Cross sectional studies and cohort effect
Observational research where data is collected from different participants at one point in time. (across things like age)
Cohort effect: people in the same cohort (e.g., people born in the same year or who lived through the same historical event) might share similar experiences that shape their perceptions and behaviors in ways that differ from other cohorts.
Difficult to generalize findings : if a study on technology use is based on people who grew up with the internet, it may not reflect how older generations, who didn’t have the same experiences, interact with technology.
Longitudinal studies (cross-generational effect)
Measuring the same individuals over time
Damands lots of resources (time money and effort)
Takes a long time
Attrition
Cross-generational effect says that people from different generations will experience certain things differently (differences in skills of technology)
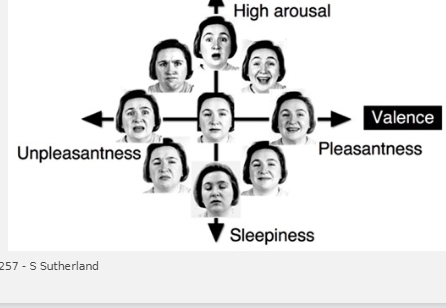
When is anxiety helpful vs harmful
Helpful: • Prepares us to take action (e.g., study for a test, get up to go to work)
• Helps us escape danger • Exists in moderate amounts
Harmful: • Excessive levels relative to “threat”• Interferes with functioning
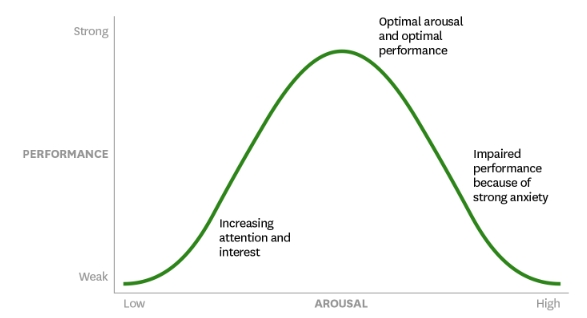
Where does anxiety come from? (Evolved threat system)
People with anxiety disorders have a highly sensitive “threat system”
Activated in response to dangers in the external environment In humans, activated by dangers that are:
Not just physical
Real or imagined
External or internal
(fire alarm in the kitchen that goes off) it is good to have but you also get a lot of false alarms
Generalized Anxiety Disorder (GAD)
Generalized means anxiety across the board (not just specific to one thing across many different things) - when people say anxiety disorders it is often this
*NEED TO HAVE 3 of the 6 symptoms in the DSM
Chronic worry (what if thinking)
Excessive worry and about a range of events or activities – trouble refocusing (talking with people while in an episode)
6 months or more – different than being in an acute stressful situation
Significant distress or impairment
Despite a person thinking about the things that can go wrong they aren’t doing something about it
Biological and Learning factors of GAD
Learning
Early stressful experiences – we learn how to be anxious (traumas like instability or poverty cause them to worry more)
Always looking for the key word “excessive” when diagnosing
Modelling from others: Learn that the world is dangerous and that you cannot cope “dont ever drive a car” “people are dangerous” - big reactions from caregivers
Biological
Inherited tendency to be tense and reactive
Genetic predisposition to be more sensitive (you can even see this in the behavior of babies)
Highly sensitive nervous system
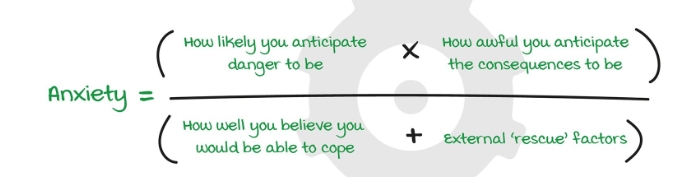
Cognitive factors of GAD
Belief that worrying is helpful
Difficulty tolerating uncertainty
Cognitive avoidance – Lost in mind, avoid engaging with reality
Attention – biased toward threatening information
Anxiety Equation
Treatment of GAD
Medication
Benzodiazepines: short-term relife, bad side effects, dependence
Anti-depressants: Safe long term, fewer side effects, less dependence
Psychotherapy *has the most research behind it
As effective as medication short-term - More beneficial long-term
CBT: Relaxation techniques - breathing (giving messages to the rest of the body that you are ok)
OCD - (obsessions vs compulsions)
OCD: Recurrent obsessions and/or compulsions
Obsessions: intrusive and nonsensical thoughts, images, or urges that one tries to resist or eliminate
Compulsions: repetitive actions meant to suppress thoughts & provide relief
The obsessions and/or compulsions are time- consuming (e.g., taking more than one hour per day) or cause significant distress or impairment in social, occupational, or other important areas of functioning
Not Due to a Substance, Medical Condition, or other psychological disorder
Can present as hoarding
It can be difficult to decipher between OCD and __________
OCD and autism spectrum disorder
What is considered impairment
Disrupts daily life (work, relationships, self- care)
Causes intense anxiety if rituals aren't performed
Consumes significant time
Triggers avoidance of situations, places, or people
Lack of rational control over compulsions
DSM Specifiers: Insight in OCD
With good or fair insight – person understands behaviors are not true or irrational
With poor insight – person believes that they are somewhat justifiable
With absent insight/delusional beliefs – believes they are completely true
“not just right compulsion”
Causes of OCD
Genes: Moderately heritable
Brain/Cognitive function
Structural abnormalities in the caudate nucleus
Low serotonin
Attention drawn to disturbing material
relevant to obsessive concerns
Early learning: Taught that some thoughts are dangerous/unacceptable - you are going to become whatever you are thinking about
Thought action fusion and suppression
Maintenance Factors in ODC
Thought-action fusion makes people feel their thoughts are dangerous.
Suppressing thoughts often makes them worse.
Inflated responsibility and guilt lead to compulsive actions to try to prevent imagined harm. These factors keep the cycle of OCD going and make it harder to break the pattern.
OCD Treatments
Antidepressants (e.g., SSRIs)
Severe cases: Psychosurgery (cingulotomy – incision to cingulate gyrus)
Psychological Treatment: CBT: Exposure & Response Prevention (ERP)