A&P I- Chapter 6- Bones
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
Functions of Bones
support, protection, attachment point, storage, blood cell formation, and horomone production
What do bones protect?
CNS and visceral organs (thorax and upper absominal cavity)
How does skeletal muscle attach to bone?
tendon
What is hematopoiesis?
formation of blood cells in red bone marrow
What is osteocalcin?
regulates insulin release (stimulates pancreas), glucose homeostasis, energy expenditure
What does the embryo skeleton contain
mostly cartilage
Characteristics of cartilage
strength and resilience (return to original shape), high water content, no nerve supply, avascular, surrounded by perichondrium
What is perichondrium?
fibrous connective tissue, vascularized, limits to twisting
Hyaline Cartilage
Most abundant with collagen fibers- Example: Articular cartilage, costal cartilage (ribs to sternum), respiratory cartilage, nasal cartilage
Elastic Cartilage
Contains elastic fibers and some collagen- Example: external ear, epiglottis (above trachea)
Fibrocartilage
contains rows of chondrocytes (secreted cartilage) alternating with thick collagen bands, compressible and great tensile strength- Example: vertebral discs, knee, pubic symphysis
Appositional Growth
laying down new cartilage on old cartilage, cells under perichondrium deposit new matrix on top of old (tree ring), at surface of cartilage tissue
Interstital Growth
cells divide and secrete matrix within pre-existing cartilage, deeper in tissue, causes cartilage to grow in length (cartilage skeleton is the blueprint)
How are bones classified?
location and shape
Axial Skeleton
long axis of body, skull, vertebral column, ribs
Appendicular Skeleton
limbs and the girdles, pectoral and pelvic girdles, arms, legs, vital for movement
Long Bones
longer than they are wide, column shape- Example: arm and leg bones
Short Bones
cube-shaped- Example: bones in wrists and ankles
Sesamoid bones
bones that form in a tendon- Example: patella
Flat bones
thin, flat, curved- Example: sternum, scapulae, ribs, most cranial bones
Irregular bones
anything that does not fit in other categories- Example: vertebrae, os coxa
What are the layers of bones?
Compact (lamellar) bone and spongy (trabecular) bone
Compact (lamellar) bone
looks smooth and solid, no space
Spongy (trabecular) bone
open spaces with needle- like pieces of bone called trabeculae, open space filled with red or yellow marrow
Trabeculae
needle-like bone pieces, found in greatest concentration along lines of stress (where bone is pushed on) to give it more strength
Structure of flat, irregular, and short bones
thin plate of spongy bone covered by compact bone (spongy sandwich), no large cavities for bone marrow
Structure of Long bones
Diaphysis, Epiphysis, Membranes, Vascularization and Innvervation
Diaphysis
bone shaft, composed of compact bone “collar” with internal medullary cavity (contains bone marrow)
Epiphysis
bone ends, composed of compact bone externally and spongy bone internally, covered with articular cartilage, no cavity, location is where one bone articulates with another bone
Membranes
Periosteum and Endosteum
Periosteum
covers external bone surface except at epiphysis!! well vascularized and innervated, outside nerve covering
Endosteum
covers internal bone surfaces, trabeculae in spongy bone, cavities in compact bone, contain osteoprogenitor (generate into bone forming cells) cells
Nutrient artery and vein
serve diaphysis
Epiphyseal artery and vein
serve epiphysis
Osteon (of lamellar or compact bone)
structural unit of compact bone, helps bone withstand pressure and stress (change osteon, change bone function)
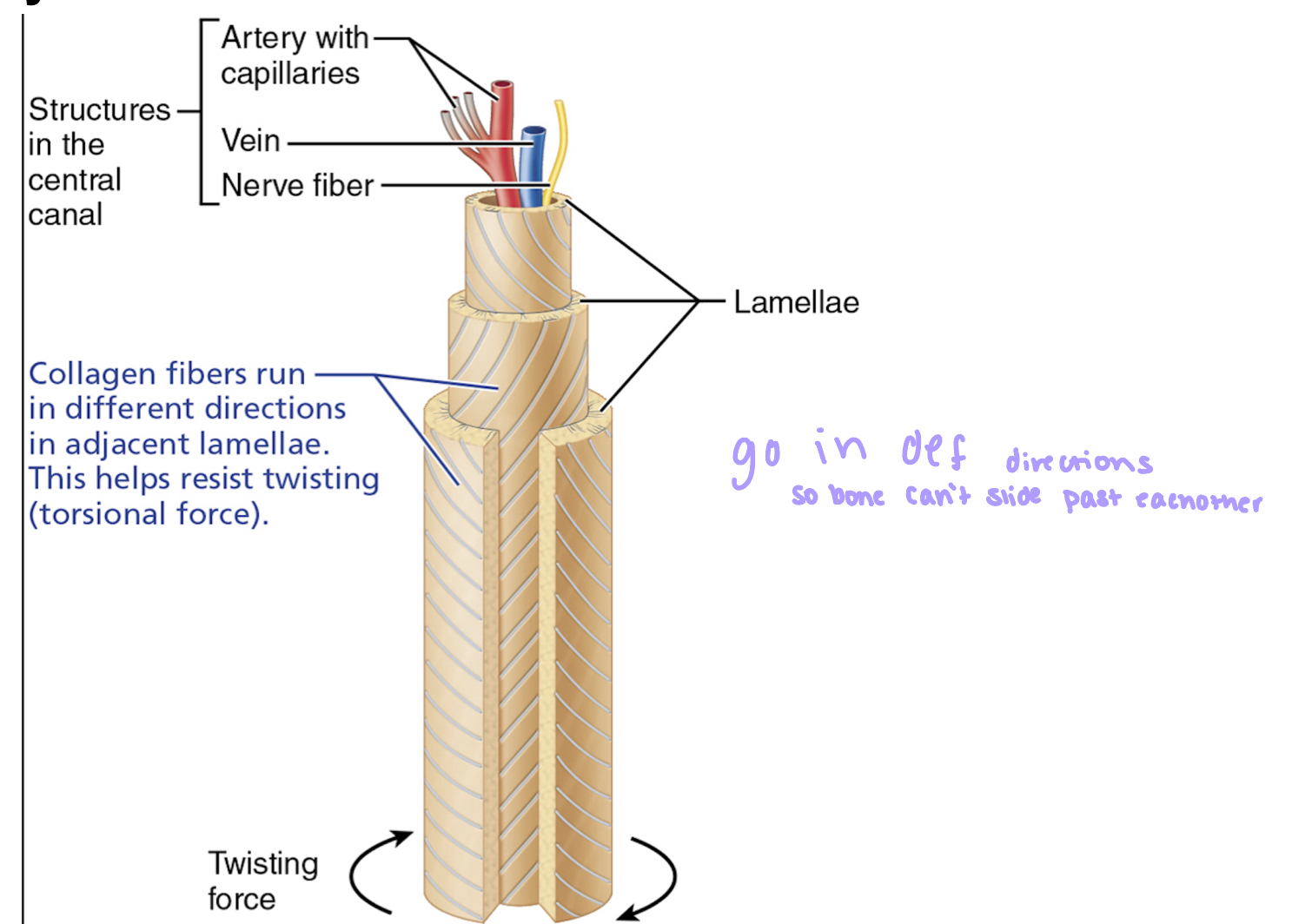
Central Canals (of compact bone)
run through center of each osteon, contains nerve and blood vessels
Perforating canals
extending from central canal, connect neighboring osteons and medullary cavity
Interstitial Lamellae
incomplete lamellae found in between complete osteons- Function: fill in gaps between osteons
Circumferential lamellae
found just deep to periosteum, extend around circumference of diaphysis- Function: resists twisting of long bone
Hematopoietic Tissue
tissue to form blood cells
Red bone marrow
produce blood cells, in adult skull, ribs, sternum, clavicles, scapula, vertebrae, and the heads of femur and humerus (only long bones with this)
Where is Red Bone Marrow found in Infants?
all of skeleton is filled with red bone marrow, limited in adult bony, not much growth
Yellow Marrow
in adult medullary cavity of long bones, contains more fat and less blood supply than red marrow, can be converted to red marrow when they hemmorage
4 Cell Types for Bone Growth
Osteoprogenitor (osteogenic cells), osteoblasts, osteocytes, osteoclasts
Osteoprogenitor (osteogenic) cells
stem cells, mitotically active, can differentiate to osteoblasts
Osteoblasts
bone-forming cells, secrete unmineralized matrix (osteoid) that forms bone tissue, secrete matrix until surrounded
What happens to osteoblasts when it is surrounded by matrix?
they mature and transform to osteocytes
What does “unmineralized" matrix mean?
soft, not yet hardened with mineral salts
Osteocyte
mature bone cell, they monitor and maintain bone matrix, respond to mechanical stress and calcium signals- Example: too many salts= too hard, arms communicate with other cell types
Osteoclasts
bone-degrading cells, maintain, remodel, and repair bones, stimulated when blood calcium homeostasis is low, produce collagenase
Collagenase
break down collagen fibers
Chemical Composition of Bone
Organic (cells and osteoid, matrix), and inorganic (mineral salts, calcium phosphate to make collagen fibers stiffer)
Osteomalacia (adults)
calcium deficiency, less mineral salts deposited in bone than normal, causes weak/soft bone, vitamin D deficiency (need for calcium to be absorbed)
Ricket’s (children)
weak/soft bone due to less mineral salts, skeleton is not done growing so permanent bone deformities, bowed legs and misshapen pelvic girdle, can wear a brace
Endochondral ossification
formation of ossified bone by replacement of cartilage with bone, happens below the skull, hyaline used as a blueprint (embryonic skeleton)- as ossified bone is laid done, hyaline cartilage is broken down
Endochondral Ossification Step 1: Formation of a Bone Collar
osteoblasts lay down bone matrix against cartilage surface to form a collar around the diaphysis cartilage to support, formation of primary ossification center (POC- where bone formation begins) after bone collar formation, POC is rigid and filled with cartilage, cells hypertrophy and harden
Endochondral Ossification Step 2: Cavity forms in diaphysis center
cells inside ossification center die off because they are not getting nutrients, cartilage inside POC break down and calcify, creating a cavity, cartilage outside continues to grow and elongates bone, bone collar prevents diaphysis from being bent/crushed
Endochondral Ossification Step 3: Formation of initial spongy bone in diaphysis
the periosteal bud invades cavity, bud contains nutrient artery/vein, nerve fibers, red marrow elements, osteoprogenitor cells, and osteoclasts, osteoblasts secrete matrix around calcified cartilage, initial formation of spongy bone is bone-covered cartilage trabeculae
Endochondral Ossification Step 4: Formation of medullary cavity and elongation of diaphysis
initial spongy bone is broken down by osteoclasts, forms medullary cavity, cartilage remaining in diaphysis is calcified, broken down, and replaces by bone, secondary ossification center forms in epiphyses
Endochondral Ossification Step 5: Secondary ossification continues in epiphyses
Similar to primary ossification except the spongy bone is retained (no medullary cavity), some areas still have some actively growing cartilage
How does a bone grow in length?
intersitital growth in pre-existing tissue, occurs at the epiphyseal plate (cartilage plate between epiphysis and diaphysis)
Process of Growth in Length
1) New cartilage laid down in epiphyseal plate
2) Cartilage cells at center of epiphyseal plate enlarge and cartilage is calcified (die off)
3) Calcified cartilage is broken down by osteoclasts and osteoblasts lay new bone tissue
What happens to bone growth at the end of adolescence?
cartilage production in epiphyseal plate slows and stops (determined by hormones), existing cartilage is calcified and replaced by bone- bone of diaphysis fuses with bone of epiphysis
How does a bone grow in width?
appositional growth occurs at the same time as bone lengthening (can’t have a skinny bone)
Process of bone growth in width
1) Osteoblasts secrete new matrix at the periosteum
2) Osteoclasts break down bone tissue at the endosteum
What difference in activity rate between the cells must there be for growth in width to occur
osteoblast cavity must exceed osteoclast, growth>deterioation
Growth hormone
controls activity at the epiphyseal plate, released by anterior pituitary gland in brain
What effect does growth hormone have on the epiphyseal plate?
when cells are exposed to growth hormone they are more active, hyposecretion = not enough hormone
Estrogen
causes growth spurt at pubery, in high levels it induces epiphyseal plate closure, causes feminization of certain parts of skeleton
Testosterone
Causes “masculinization” of certain parts of skeleton, no growth spurt but no stopping growing
What is the typical age at which males and females stop growing?
21 (M) and 18 (F)
What is involed in bone remodeling?
bone deposition (new osteoid from osteoblasts) and resorption (break down old bone with osteoclasts)
Maintenance of Ca2+ homeostasis
Ca2+ is essential for excitability of body cells (especially neurons and muscle cells), without Ca2+, neurons do not fire and muscle does not contract
Bone Health
Mechanical/gravitational forces activing on bone tissue drive remodeling, strengthens bone exactly where needed
Factors involed in Deposition and Resorption
Parathyroid homorone (PTH - released in response to decreasing blood Ca2+ levels), and Mechanical stress (Wolff’s law: bones will remodel to adapt to mechanical forces that may or may not be places on them)
Effects of increased PTH release
1) number of osteoclasts at bone increase
2) osteoclasts become more active in bone tissue
Once blood Ca2+ returns to normal, PTH release decreases and osteoclast number and rate of activity decreases
If continue low Ca2+ in blood, excessive PTH release and bone breakdown, it eats through the skeleton
What happens when more stress is placed on a bone?
1) the more trabeculae will be found at the location of loading
2) the thicker the compact bone will be at the location of loading
Example- weightlifters need stronger bones, astronauts have no stress on bones so they aren’t as think (prone to fracture)
Steps of Bone Repair
1) a hematoma forms- collection of blood outside of a blood vessel, clear out fracture with phagocytes, chondroblasts lay down fibrocartilage
2) fibrocartilaginous callus forms
3) bony callus forms
4) bone remodeling occurs