Hematologic system
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
What does the hematologic system consist of?
It consists of blood and the sites where blood is produced, including the bone marrow and the RES system
What does plasma contain?
Nutrients, hormones, electrolytes, waste, clotting factors proteins
What does blood contain: 55% of blood volume is plasma and 45% consists others
Blood
what are the 3 primary cell types
What is the process of hematopoiesis
Location?
differentiations?
Thrombocyopenia?
Thrombocytosis?
3 cells:
erythrocytes (RBC)
Leukocytes (WBC)
Thrombocytes (platelets)
Hematopoiesis: replenish blood cells - primary site is the bone marrow- stem cells begin the process of differentiation into myeloid or lymphoid cells
myloid cells - non-lymphoid WBC, RBC production and platelets
if not function properly can produce leukemia
Thrombocytopenia: low platelet count - risk of bleeding
Thrombocytosis: high platelet count - risk of blood clots
Erythrocytes (red Blood Cells)
primary weight by
responsible for
A condition caused by bleeding?
Consists primarily of hemoglobin, which is iron
oxygen readily binds to hemoglobin in the lungs and is carried as oxyhemoglobin in arterial blood - primary function
When the bone marrow releases immature RBC called reticulocytes, sometimes its a normal response for bleeding in disease states
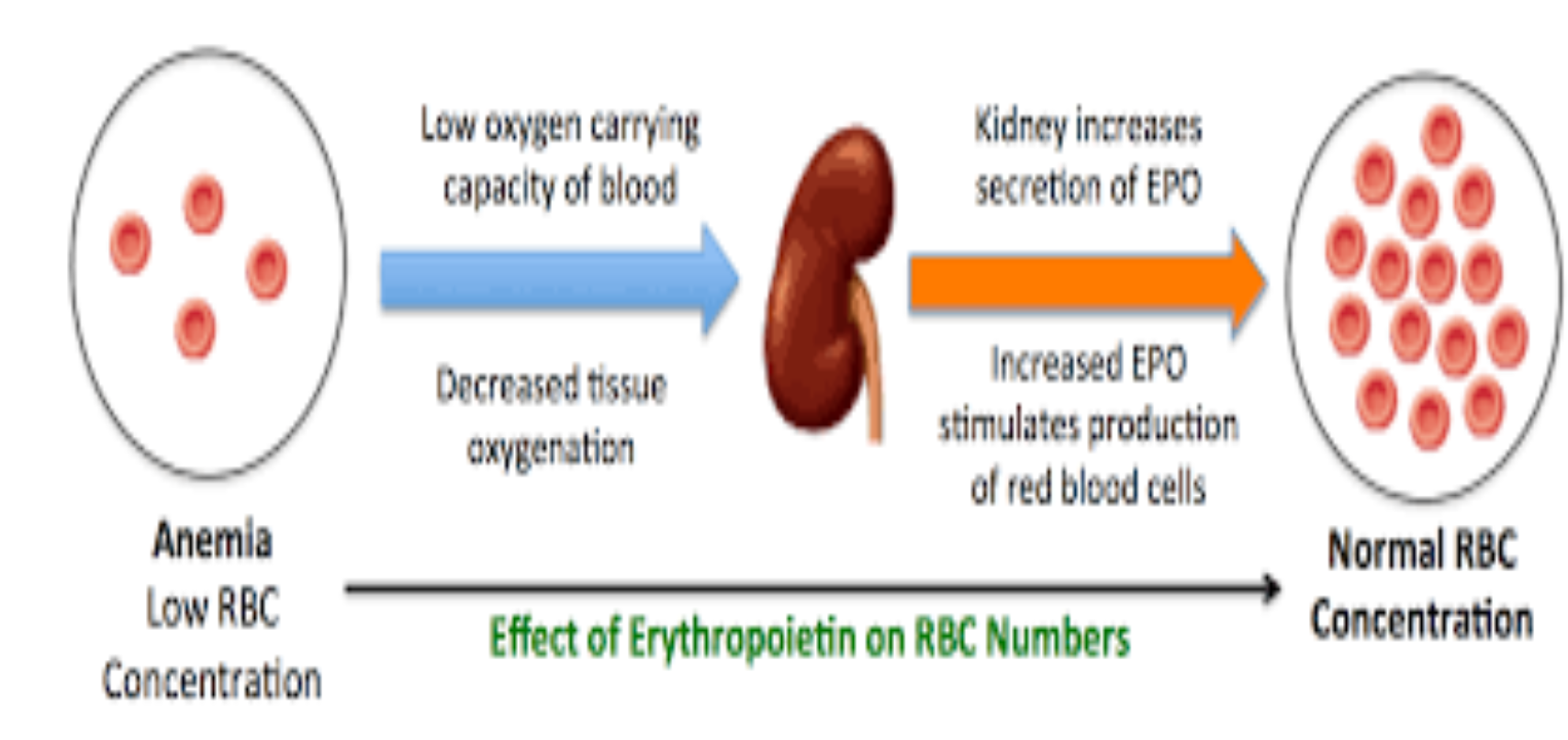
Erythroposisis
what is the process of forming RBC
How are old RBC removed
Myeloid stem cells in the bone marrow are activated for differentiation by stimulation of erythropoietin from the kidneys creating erythroblasts
Depending on supplies- folic acid, VB12, iron
Old RBC are removed from blood by reticuloendothelial cells - in liver and spleen
Iron Deficiency anemia
only .5 -1 mg is absorbed in Small intestine
What is the patho?
Microcytic anemia
what is
Patho: rapidly depleted bone marrow stores decrease hemoglobin syntheisis = small and low amount of erythrocytes
Microcytic anemia usually from blood loss from heavy menstruation or bleeding of the GI tract
older audlts = GI dx or colon
stool samples
Vitamin B12 and Folic acid
derived from?
required for DNA synthesis of RBC
derived from diet
must have a functional intestinal mucosa for absorption
B12 combines with. intrinsic factor produced in the stomach and absorbed in the distal ileum
Those with partial or total gastrectomy - limited intrensic factor so cat absorb B12
Luekocytes -WBC
2 types
what’s included in those 2 types
What are they used for
Which patient would be presnt with which dx?
Granulocytes: granules in cytoplasm - protect the body from invasion by bacteria or foreign body
Neutrophils (WBC)
band cells: increase with neutrophil demand (infection) - bandemia
rise with fever, tachy, systemic inflammatory response (RA, gout, ETC)
Eosinophils - parasitic and allergic reaction
basophils - released in exposure to allergens
Agranuloyctyes
monocytes: differentiate the tissue to macrophages
macorhpage- effective against fungi and viruses
Lymphocytes - in Bone marrow ad cortex of thymus
t-lymphocytes: release lymphokines to kill forgein cells and enhance phagocytic response
cellular immunity delays allergic reaction, rejection of foreign tissue, destruction of tumor cells
B-lymphocytes: humoral immunity
differentiate into plasma cells and produce atibodies called immunoglobulin
Platelets (thrombocytes)
role
Plasma and plasma proteins
contains
Contor bleeding - circulate in the blood in an inactive state - vascular injury = platelets collect at the site and are activated forming platelet plug
90% is water, plasma proteins and clotting factors - fibrogen
Plasma proteins = albumin and the globulins
albumin helps maintain the fluid balance in vascular system

Hemostasis
primary and secondary pathways
what dx would a person with defect in factor 5 and factor 12?
Activated through intrinsic or extrinsic pathway - reaction of the cascade forms fibrin
Factor 5 deficency- inc clotting risk
factor 12 deficnecy - inc bleeding risk
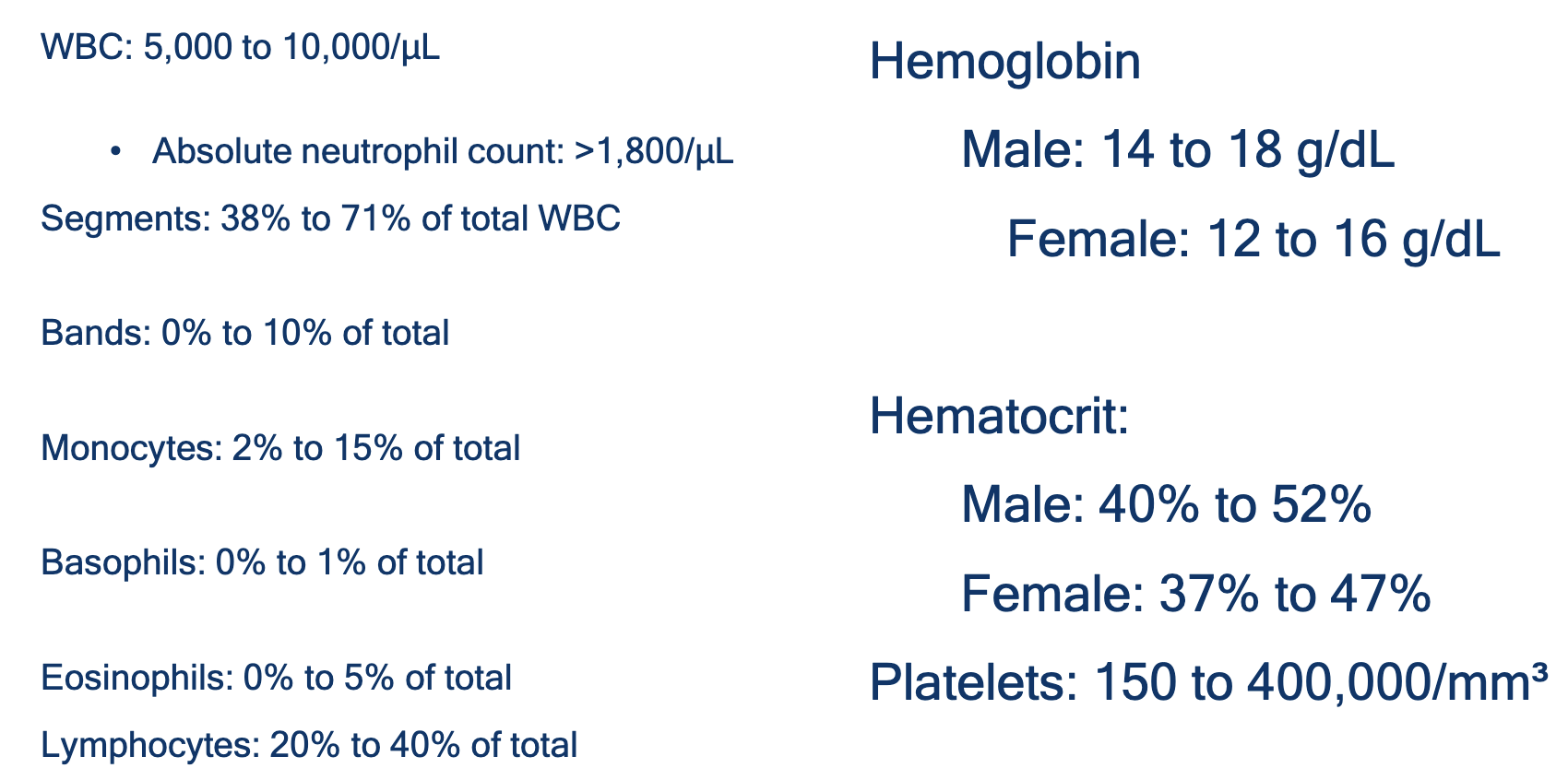
Complete Blood count with differentiation
WBC count
Hemoglobulin
Hemotacrit
Assessing the patient with low hemoglobin and hematocrit
Pallor - most common
fatigue, dyspnea, palpitations. poor activity tolerance, headaches, tinnitus, anorexia, indigestion, irratablity, difficulty sleeping, abnormal menstruation, impotence, loss of libido, chest pain
What is the difference between hemodilution and hemoconcentration
definition
what to do?
Hemodilution falsely low hematocrit
sx: weight gain, moist mucus, edema, HTN, crackles, S3 gallop, mitral valve, increased urine output, distended neck vein
fluid volume overload - RSHF
Diurusis patients - restrict/monitor I and O, daily weights, electrolytes
Hemoconcentration = falsely elevated hemotacrit
sx: weight loss, dry mucus, delayed skin turgor, orthostatic hypotension, decreased pulse pressure, dec urinary output, inc HR, dec BP
Isotonic hydration - inc plasma and oral hydration
Assessing the patient with low WBC count
ANC
Fever??
Neutropenic precautions
Assess absolute neutrophil count (ANC)
Severity is classified into:
ANC 1,500 - 1,000 =mild neutropenia
ANC 999 - 500 = moderate neutropenia
ANC less than 500 = severe neutropenia
Assessment of multisystem - because patients with neutropenia aren’t able to manifest the classic signs of infection - watch for fever above 100.4 fever
Neutropneic diet
masks
hygiene had wash
no florist or edible arrangments
What is the Nurisng Multisystemic Assessment
skin
oral mucosa
respitory
GI
neuro
Skin: tenderness, erythema, edema, breaks, moisture, central line
oral mucosa: moisture, lesions, color, pain, change in taste - swish and spit
Respiratory: cough, sore throat, tahypena pain on inspiration, ltne breath sounds, sputum color, consistent
GI: palpate abdomen ascultate assess for change in bowel pattern changes
nuero: headache, neck stiffness, visual disturbance, level of consciousness, orientation, behavior
How to assess the patient at risk for bleeding
History and Physical Examination for a patient with a hematologic disorder, emphasizing the need for a multi-systemic assessment and a focus on the integumentary system (skin).
Petechiae are the smallest type of bleeding spots under the skin.
Size: Pinpoint size
Appearance: Tiny, flat, non-blanching red, blue, or purple dots, often appearing in clusters
Significance: Petechiae are the classic sign of a primary hemostasis defect, problem with platelets or the capillary vessel walls.
Most Common Association: Severe Thrombocytopenia platelets responsible for sealing tiny breaks in capillaries too low in number or dysfunctional, allowing blood to leak out of the smallest vessels into the skin.
Purpura describes larger areas of bleeding into the skin.
Size: Larger spots Lesions larger than 1cm called ecchymoses (bruises).
Appearance: Flat, non-blanching macules or patches that are red, purple, or brownish-black.
Significance: Purpura can indicate a wider range of conditions
Thrombocytopenic Purpura: Occurs when purpura is caused by a low platelet count -Immune Thrombocytopenia (ITP),
Non-Thrombocytopenic Purpura: Occurs when the platelet count is normal, but the purpura is caused by vessel damage
Palpable Purpura: An important clinical finding where the lesions feel raised or bumpy. This often signals Vasculitis (inflammation of the blood vessels) and can be a sign of a serious underlying illness (e.g., Rocky Mountain spotted fever, meningococcemia, or autoimmune disorders)
What questions are u askin when asseing for the risks of bleeding?
Hx?
Labs you are assessing
Physical examination
nosebleeds, dental work, menstruation - iron replacement, childbirth - blood transfusion, surgery blood transfusions, early bruising, family
If at risk - no tubes rectal - no injection deep , fall risk
Labs: CBC, peripheral blood smear, PT/INR, PTT, Platlet function assay
Thrombocytopenia: low platelet count
<50,000 - bleeding precautions
Physical exam: petechiae, ecchymosis, bleeding at puncture site, hypotension, tachy, dizziness, epistaxis, hemoptysis, abdominal pain or back pain, hematemesis, abdominal distension, rectal bleeding, vaginal bleeding, headache, mental status change, blurred vision
What does PT/PTT/INR mesure
PT = time needed for factor VIIa to form a complex with tissue factor and clot - 11 to 13.5 seconds
porlonged PT = Factor 7 deficency
INR= standardized Pt times from several laboratories - used to monitor Warfarin - (2-3 if heparin)
PTT - elevated may indicate definceny infcator 7, 8, 11 (25 to 35 seconds )
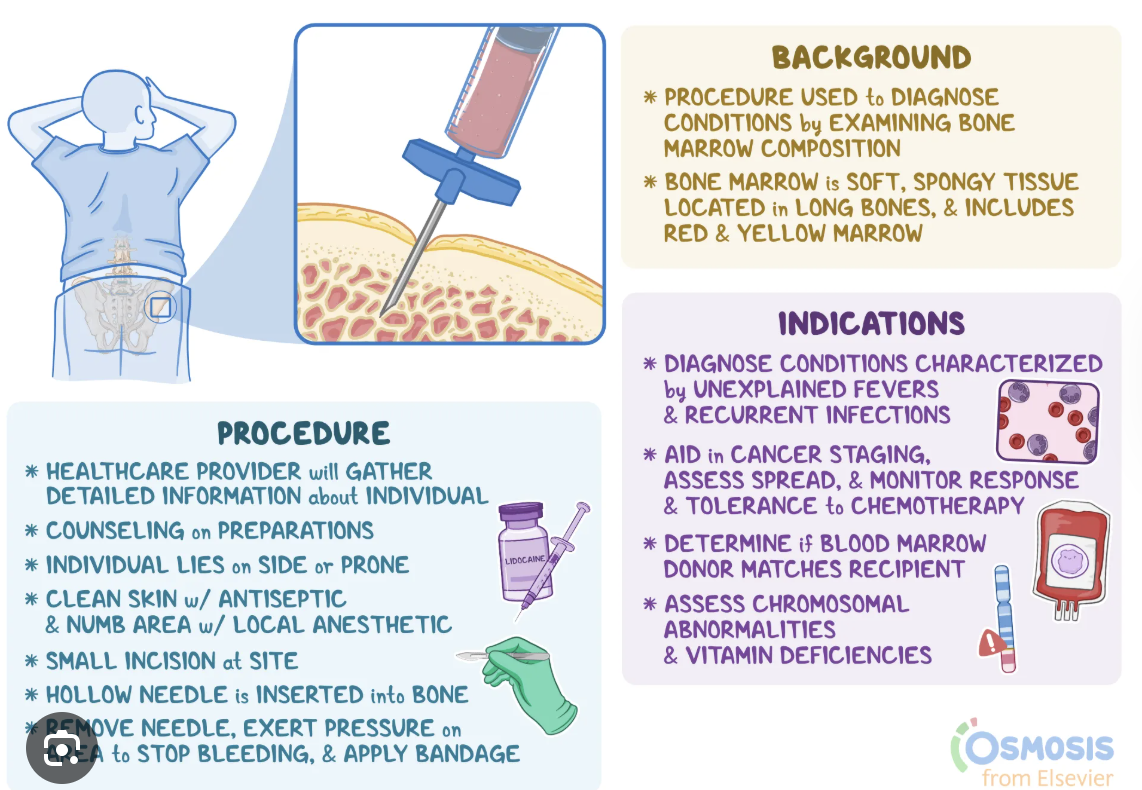
What is bone marrow aspiration and biopsy?
what’s it do
Nursing care?
Provides information to assess how a person's blood cells are being formed - assess the quantity and quality of each type of cell produced by marrow
procedure: informed consent - requires local anesthetia
Nursing care: pain, antianxiety meds, deep breathes, post-procedure education
Anemia - dec number of RBC
Classified as?
What is the medical management and nursing management?
Size:
Normocytic- normal average size RBC
macrocytic - larger than normal - iron
microcytic - smaller than normal
Color
Normochronic - normal in color
Hyperchromic: Darker cellular contents
Hypochromic: pale
Hypoproliferative anemias: the bone marrow cannot produce adequate numbers of erythrocytes
hemolytic anemias: involve premature destruction of erythrocytes
Nursing management: onset duration, metabolic requirements, concurrent medical conditions
Complications: heart failure, paresthesias and confusion
Nursing care focuses on: managing fatigue - can cause dec QOL
promote nutrition -iron B12, folic acid, avoid alcohol
maintain perfusion - transfusion or IV supplemnetal O2 monitor vitals
resolve the underlying cause
What are different types of anemia:
Iron deficiency
Renal Dx
Aplastic Anemia
Megaloblastic anemia - B12 or folic acid deficiency
thalassemua
immune hemolytic anemia
Iron deficency anemia
Patho
recognize cues - Sx
analyze cues
nursing education
meds
depletion of iron stores
Sx: fatigue, dizziness, pic, lightheadedness, palpations
Physical exam: circumoral pallow, conjunctival pallor, brittle nails, angular cheilitis, tachy, hypotension, murmurs
Labs: dec retics, iron, ferritin, iron saturation, increased TIBC
Medications: iron PO
Nursing education: food ditery considerations iron managment
Anemia of kidney dx
patho
dec kidney function - dec erthytopoetin production - concurrent iron deficiency due to dialysis
sx: fatigue, decreased activity tolerance
Physical exam: circumoral pallor, conjunctival pallor, brittle nails, angular cheilitis (cracks on side mouth), tachy, hypotension, murmurs
Labs: elevated creatine, low-normal MCV
Meds: ESA(erythropoetin stimulating agents) Epogen, Darbeoppotien
Nursing action: ESA stroke, VTE, HTN, titrate epo to the goal Hb
Vitamin B12 anemia is????
deficient in VB12 intake - poor Gi absorption, pernicious anemia
sx: beefy red sore tongue, fatigue, peripheral neuropathy
Physical exam: circumoral pallor, conjuctival palloe, brittle nails, tachy, murmur, hypotension
Labs: CBC - increased MCV, low B12 level, low reticulocyte
Meds: B12 replacement IM/mouth - life oloong for pernicious anemia
dietary counseling oral supplements frofied milk soy for vegans
Thalassemia what is it and nursing
Patho: heredity anemia - characterized by hypochromia, microcytosis hemolysis
sx: severity of major fatality in 1st few years
physical exam: circumoral pallor, conjunctival pallor, brittle nails, tachy, murmur, hypotension
Labs: low MCV and MCH, hemolysis markers
Solutions: beta Thalassmia- chronic transfusion therapy
Monitor for iron overload, elevated ferritin ue to chronic transfusions
Polycythemia: too many cells in the blood
POLYCYTHEMIA VERA: a myeloproliferative disorder in which the myeloid stem cells have escaped normal control mechanisms
Secondary polycythemia: caused by excessive production of erythropoietin
rare very thick blood can cause strokes, clotting increase hematocrit
Sickle cell anemia:
Assessment
Nursing diagnoses
interventions
Assessment:
inherited disorder → abnormal Hb (Hb S) → sickled RBCs.
Triggers: infection, dehydration, stress, cold, hypoxia.
Key findings: pain crisis, fatigue, jaundice, pallor, low H&H, ↑ bilirubin.
Watch for: stroke, acute chest syndrome, renal failure.
Nursing Diagnoses:
• Acute pain r/t tissue ischemia.
• Risk for infection r/t splenic dysfunction.
• Fatigue r/t anemia.
Interventions:
• Pain: Opioids, warm compresses, relaxation.
• Hydration: IV/oral fluids (3–4 L/day).
• Oxygen: Maintain O₂ >95%.
• Prevent infection: Vaccines, antibiotics, hand hygiene.
• Medications: Hydroxyurea, folic acid, transfusions.
• Education: Avoid triggers—cold, dehydration, high altitude, stress.
Evaluation:
• Pain controlled, oxygen stable, no crisis, patient verbalizes understanding.
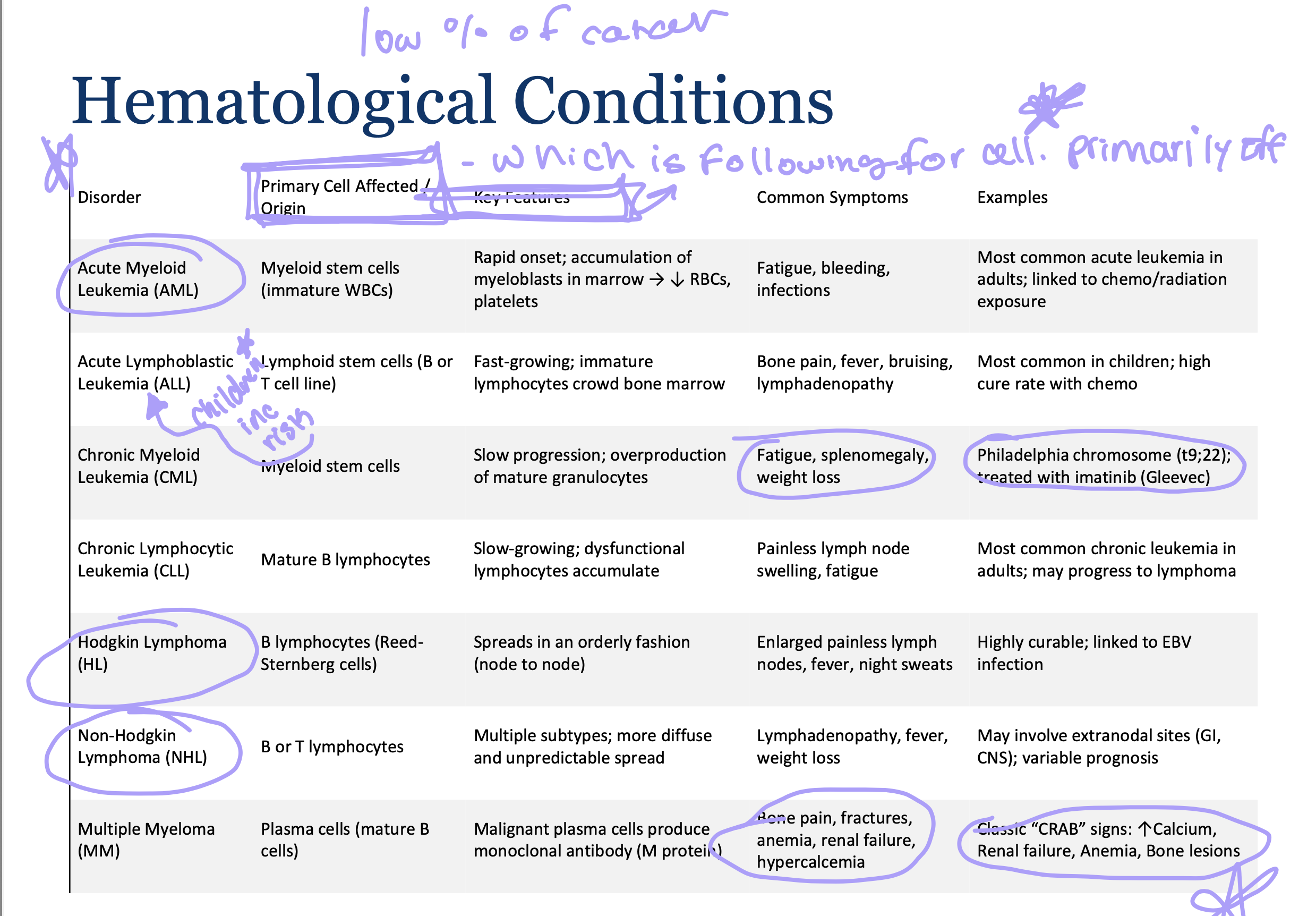
Leukemia:
what is it
neoplastic proliferation of one particular hematopoietic cell type: Leukemia is characterized by the rapid and uncontrolled production of abnormal, immature white blood cells (leukocytes)
unregulated proliferation of leukocytes in the bone marrow - classified according to the stem cells line involved, either lymphoid or myeloid
chronic or acute
Acute Myeloid leukemia
Results from a defect in the hematopoietic stem cell differentiation into myeloid cells
Symptoms result from insufficient production of normal red blood cells - bleeding and infection = complications
fever, infection, neutropenia, enlarged spleen, gum hyperplasia
Tx: aggressive administration of chemotherapy - neutropenia
Nursing intervention: infection prevention, promoting comfort, patient education
Acute lymphoid leukemia
results from the uncontrolled proliferation of immature cells from lymphoid stem cells
Normal hematopoiesis is inhibited, resulting in a reduced number of leukocytes, erythrocytes, and platelets
Tx: Induction therapy
Infections and viral infections are common
Nursing priorities: prevention of infection and bleeding managment sx nausea and pain
Lymphomas
Neoplasms of lymphoid tissue - derived from B lymphocytes
hodgkin lymphonma
non-Hodgkin lymphomas
Hodgkin Lymphoma
patho
Patho: malignant cell of Hodgkin lymphoma is the Reed-Sternberg cel a large tumor cell that is morphologically unique and is thought to be immature lymphoid origin - it is the pathological hallmark and essential diagnostic criterion for Hodgkin dx
painless enlargement of one or more lymph nodes, mediastinal mass on CXR, pruritus
Cues; cough, pulmonary infiltrates, jaundice, abdominal pain, bone pain and B-symptoms, fever, W/O chills, drenching sweats, unintentional weight loss
mild anemia, CBC, ESR, LDH, liver and kidney function
Tx: focused on cure, early stage cure, - chemotherapy, radiation therapy
outcomes - monitor for secondary cancers , hypothyroidism, CVD
Non-Hogkin Lymphoma
Patho: heterogeneous group of cancers that originate from the neoplastic growth of lymphoid tissue
involve malignant B lymphocytes and T lymphocytes
Cue presentations are variable
Analyze cues B Sx: recurrent fever, drenching night sweats, unintentional weight loss
Histopathology, immunophenotyping, cytogenetic analyzes of malignant dx
Radiation can be a treatment for T but chemotherapy
Outcome: reduce infection risk, patients receiving abdominal radiation therapy may experience nausea and diarrhea but not hair loss all patients experience fatigue
Multiple Myeloma
A malignant dx of the most mature form of B lymphocytes the plasma cell: results in production of high levels of ineffective immunoglobulins
Sx: bone pain
elderly: back pain and who has an elevated total protein level should be evaluated by possible myeloma
No cure but tx focuses on corticosteroids and chemotherapy
Hematological considerations keys
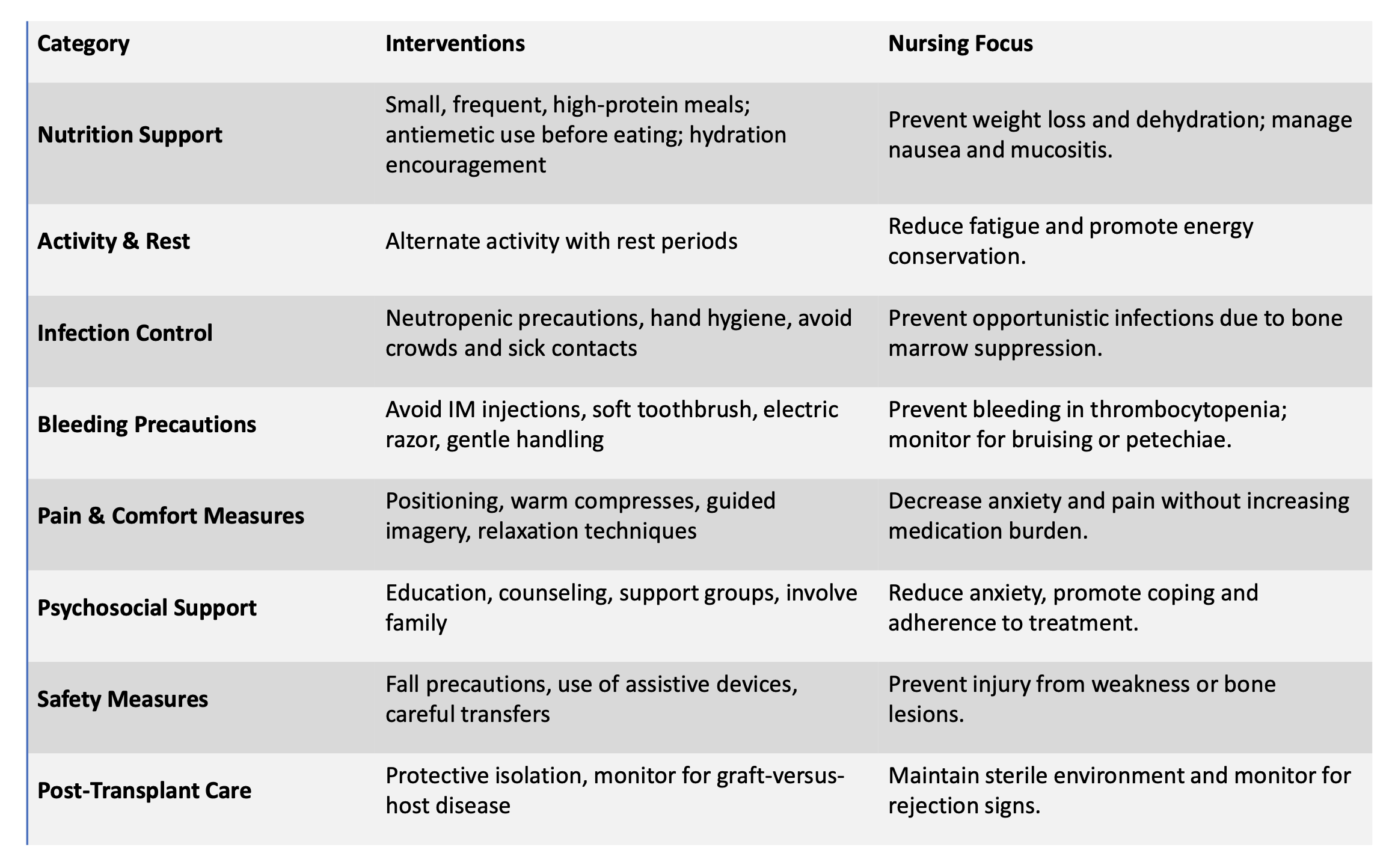
What are the nursing conditions for hematological dx
nursing diagnosis
Diagnosis
risk for infection - neutropenia
risk for bleeding - thrombocytopenia
fatigue anemia and Tx side effects
acute or chronic pain related to bone involvement or procedures
avoid large crowds
imbalanced nutrition
ineffective coping/anxiety related to cancer diagnosis and prolonged treatment
risk for injury related to weakened bones lesions or falls
What are the nursing conditions for hematological dx
nursing intervention
Intervention
neutropenic and bleeding precautions - avoid crowds, monitor for bleeding - use soft toothbrush and electric razor
monitor for signs of infection anemia and bleeding status
medications, accurate adequate nutrition and hydration - small frequent meals and oral care
encourage rest and energy conservation
emotional and psychological support, counseling education, coping
safety measures - prevent falls, handle gently, avoid invasive procedures
educate patient and family of signs of infection
What are the nursing interventions for hematological dx
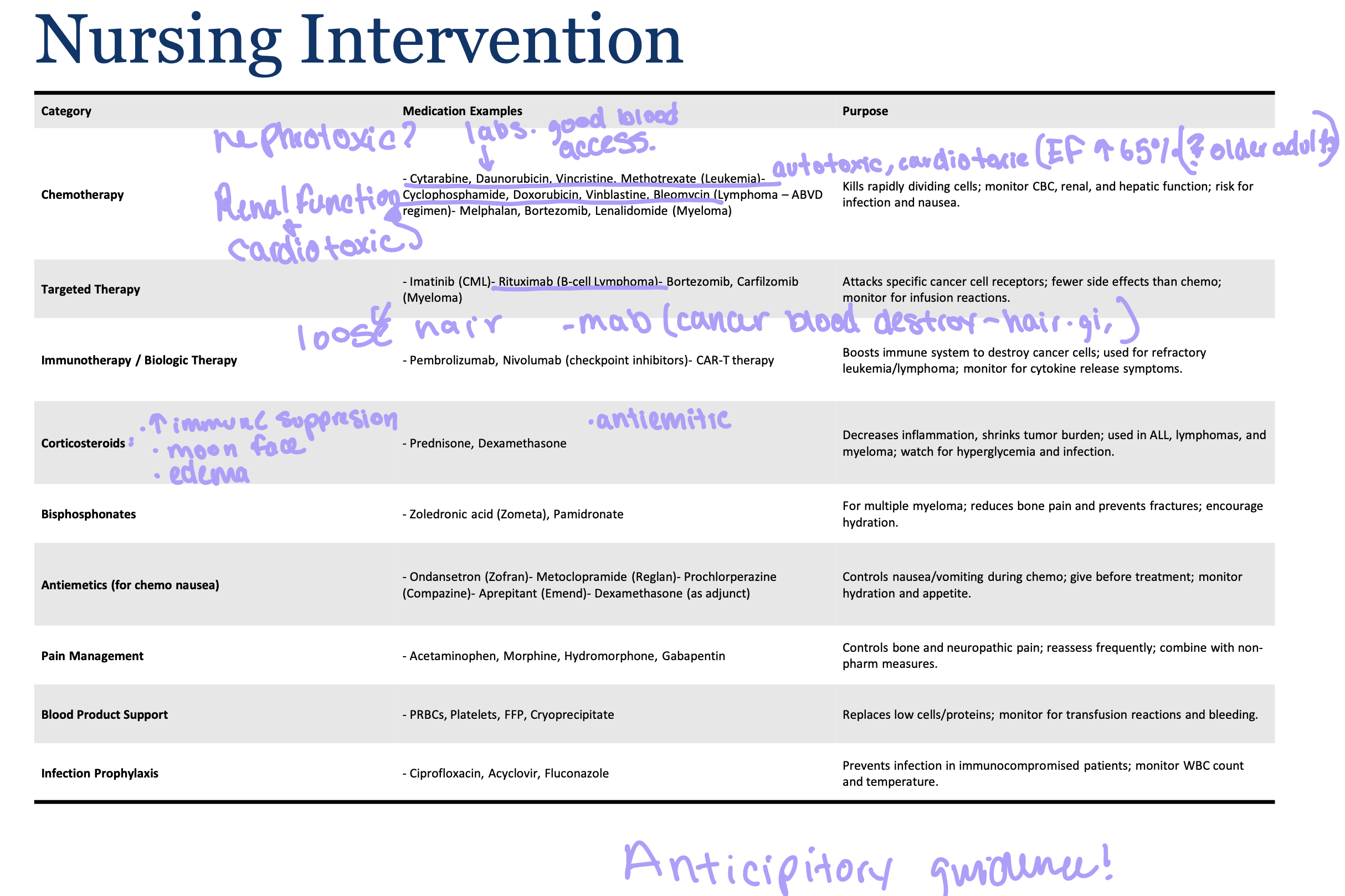
What are the nursing interventions for hematological dx
Disseminated intravasucalr cogulation
not a dx but a sign of an underlying condition
normal hemostatic mechanisms are altered so that a massive amount of tiny clots form in the microcirculation
Tx focuses on the underlying cause
monitor and manage potential complications
Leads to clotting and bleeding at the same time - liver brain and kidney damage
What are therapies for blood disorders
Splenectomy
Therapeutic apheresis: blood is taken from the patient and passed through a centrifuge to remove a specific component
Therapeutic phlebotomy: removal of a certain amount of blood under controlled conditions
Blood transfusions
Pretransfusion assessment, correct technique, and monitor for complications of transfusion
febrile nonhemolytic transfusion reaction
Acute hemolytic reaction - most dangerous and potentially life-threatening - when the donor’s blood is incompatible with the recipient
delayed hemolytic reaction - 14 days after transfusion, the antibody has increased to the extent that a reaction can occur - the hemolysis of the erythrocytes is extravascular via the RES and occurs gradually
Allergic reaction - Urticaria, generalized itch, rash, wheezing
Circulatory overload - TACO is the second leading cause of transfusion-related deaths - if to much blood is infused to quickly, hypervolemia may occur
Nursing action:
type and screen
premedicate
BP check
start transfusion
15 min BP check
reaction stop
emergency meds - epi, steroid, benedryl, pepticid, H2 blocker