Anatomy Exam One
1/183
Earn XP
Description and Tags
Babler's Anatomy at UT Austin 446L
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
184 Terms
What type of tissue is adipose tissue?
connective
What are the two types of adipocytes?
white and brown
what are the function of adipocytes?
to synthesize and store triglycerides
how does adipose tissue function as an endocrine organ?
It secretes Leptin, a hormone that binds to cells in the brain (hypothalamus) to signal satiety
what are the 3 places where fat comes from?
chylomicrons from the intestines, VLDLS from the liver, and synthesized in the cell from glucose
what are the 2 ways fat can be mobilized?
the autonomic nervous system + hormonal signalling, both cause lipase to break down triglycerides
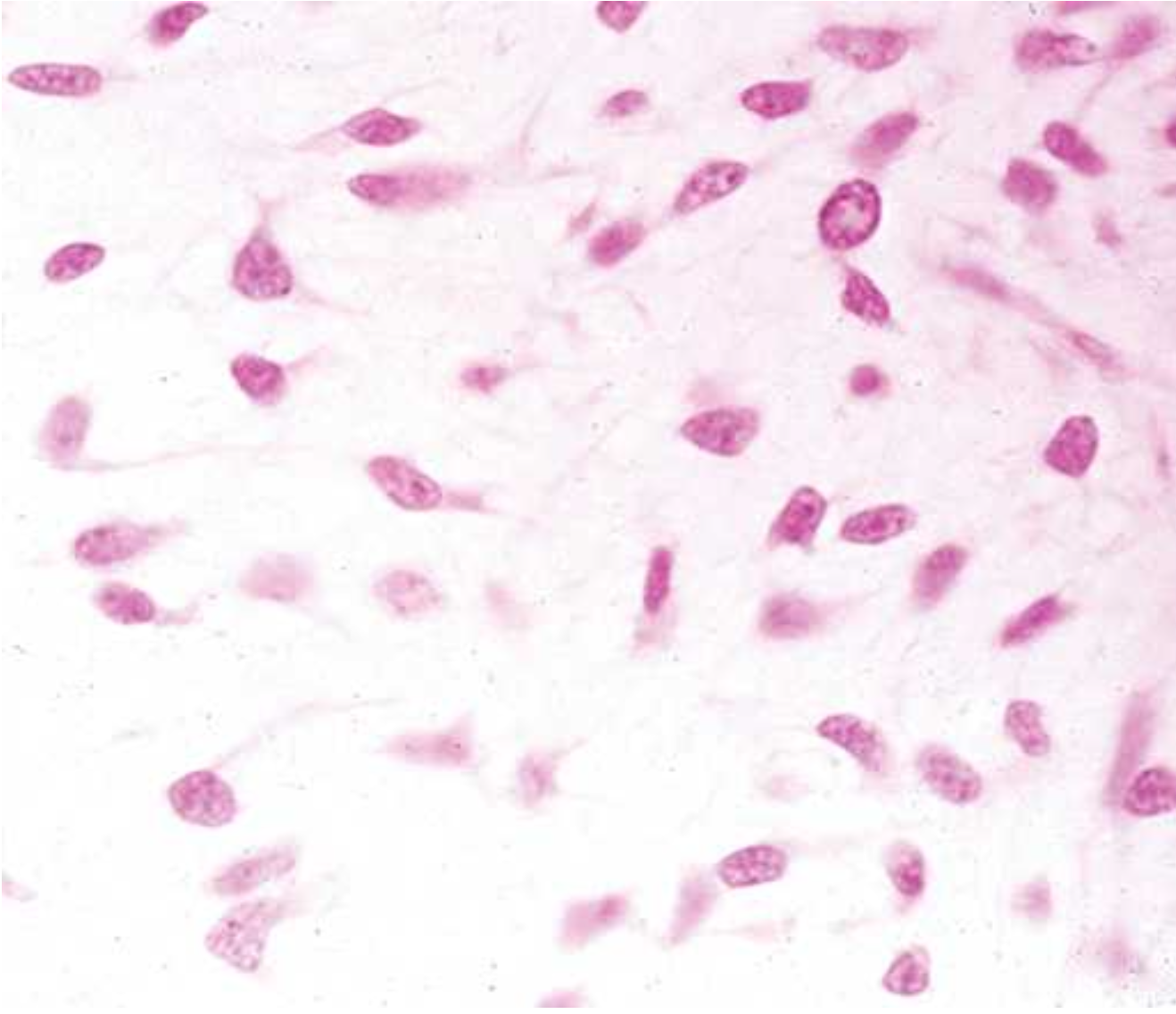
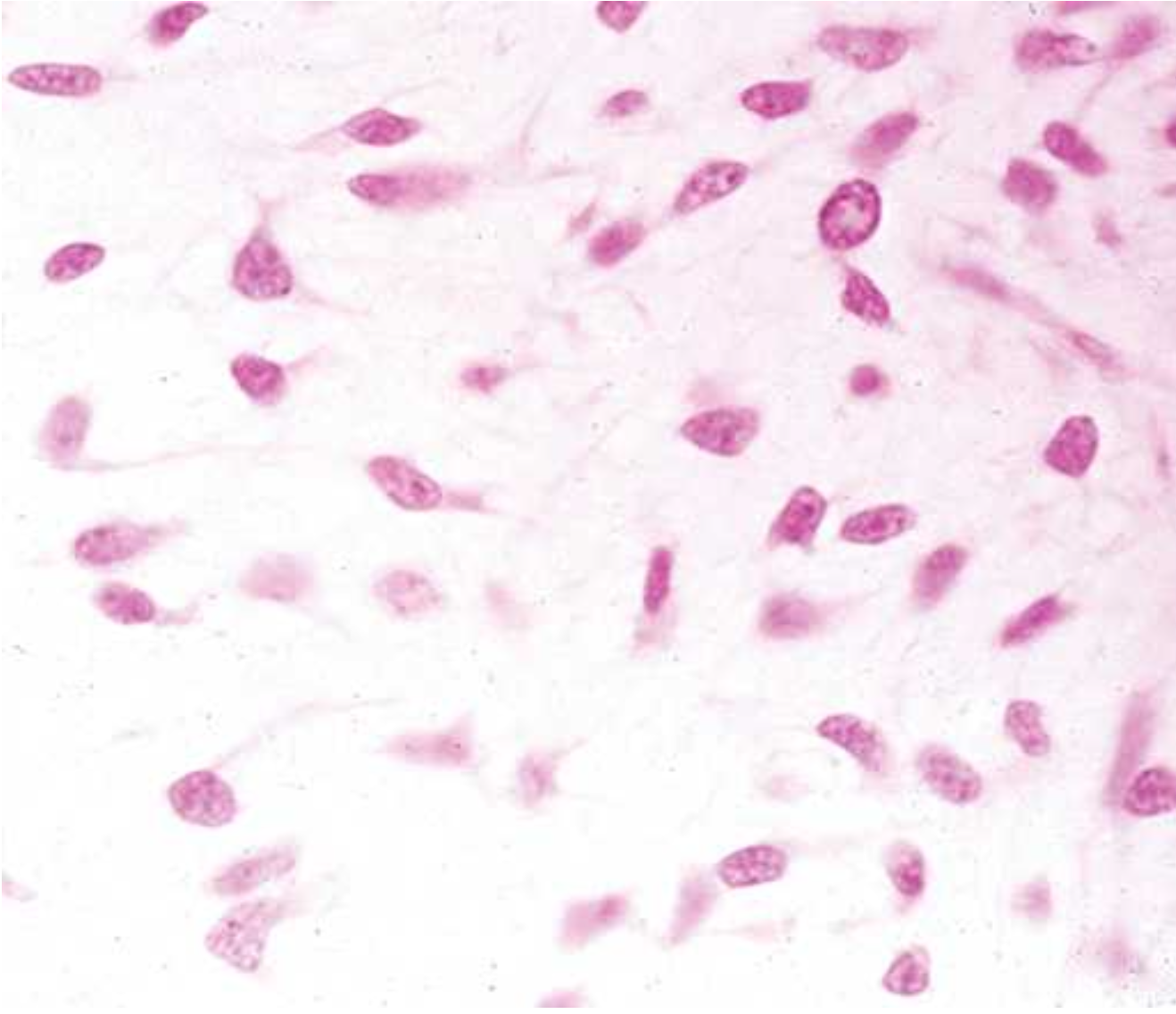
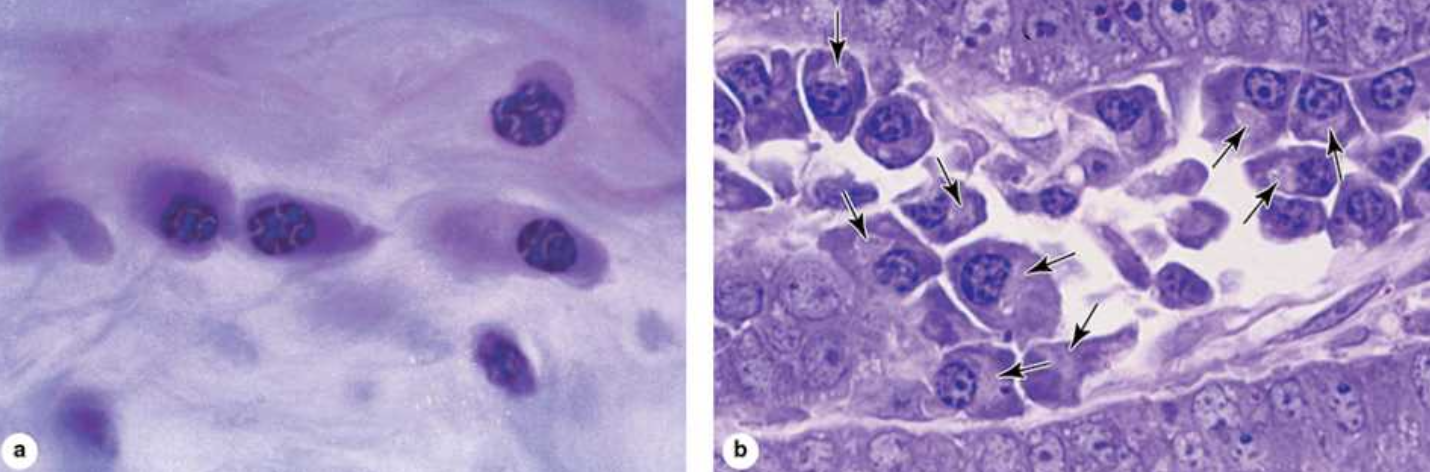
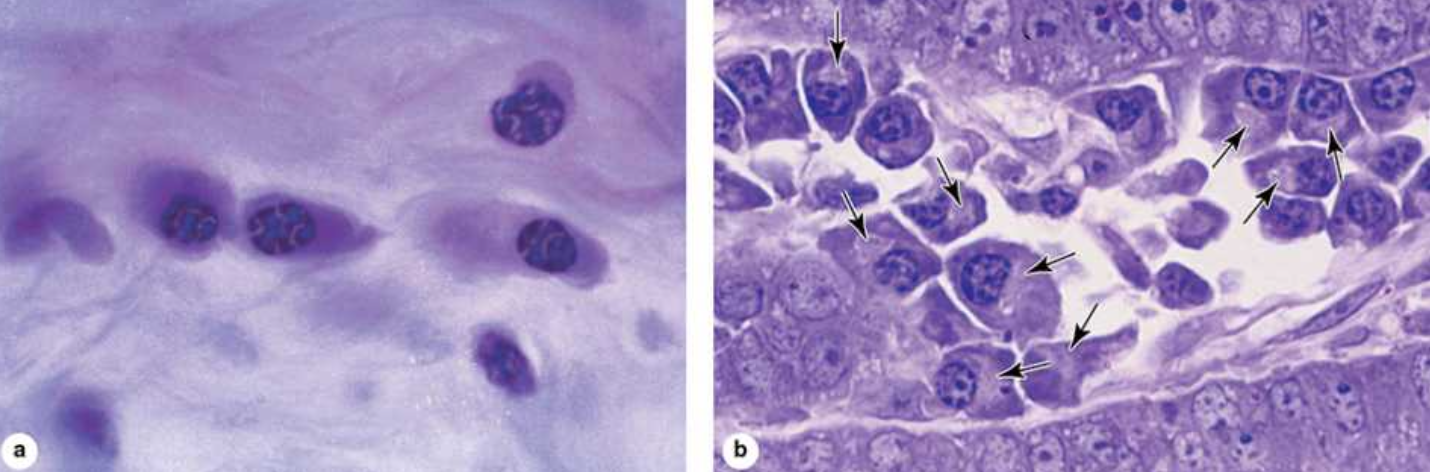
what are the characteristics of white adipose tissue?
unilocular, nucleus against membrane, energy storage site, synthesize and store triglycerides
what leads to the redistribution of white adipose tissue?
puberty/sex hormones
what are the characteristics of brown adipose tissue?
multilocular, smaller with many droplets of fat, central nuclei, for heat production, with many mitochondria
at what life stage do humans carry the most brown fat?
infancy
what condensation leads to the formation of cartilage bone models?
mesenchyme
what differentiates from the mesenchymal cells?
chondroblasts
progenitor cells can become either or
osteoblasts or chondroblasts
when does bone start to develop?
when the progenitor cells become osteoblasts
where is the primary centre of ossification?
the diaphysis of a developing bone
as the cartilage matrix begins to calcify, what happens to the cartilage cells?
they become hypertrophic and die, forming a cavity
what migrates into the cavity formed by dying cartilage cells?
periosteal cells
what is syndactyly?
digits are not formed normally
what is Apert's syndrome?
one disease that causes syndactyly
what kind of tissue is cartilage?
connective
cartilage consists of ___blasts which start to produce ___
"chondro", ECM
what is a lacunae
a cell nest
where do chondrocytes reside?
lacunae
95% of cartilage is made of?
ECM
what is in the ECM in cartilage?
ground substance (proteoglycans, glycosaminoglycans), collagen, and elastic fibres
cartilage is vascular/avascular
avascular
cartilage is innervated/not innervated
not innervated
what is the perichondrium?
a sheath of dense connective tissue
what are the two layers of the perichondrium?
inner layer which is chondrogenic and the outer layer which is fibrous
the inner layer of the perichondrium is the source of
cartilage cells
the outer layer of the perichondrium is the source of
fibroblasts which produce collagenous fibres and blood vessels
what are the two functions of the perichondrium?
growth and repair of cartilage
where is the perichondrium found?
the perimeter of elastic cartilage and hyaline cartilage
what two cartilage lack perichondrium?
fibrocartilage and articular cartilage
what are the three types of cartilage?
hyaline, elastic, and fibrocartilage
what is hyaline cartilage?
most common and mostly type 2 collagen, bone development and growth at the epiphyseal growth plate, also the site of interstitial growth
where is hyaline cartilage found?
trachea, bronchi, larynx, nose, ends of ribs, long bones
what is the epiphyseal plate?
where bone growth occurs
what is endochondral ossification?
growth at the proximal and distal ends of long bones
what is elastic cartilage?
elastic fibres and lamellae which does not calcify
where is elastic cartilage?
external ear, eustachian tube, epiglottis, larynx
what do the chondrocytes in elastic cartilage look like?
large, hypercellular
what is elastic cartilage surrounded by?
perichondrium
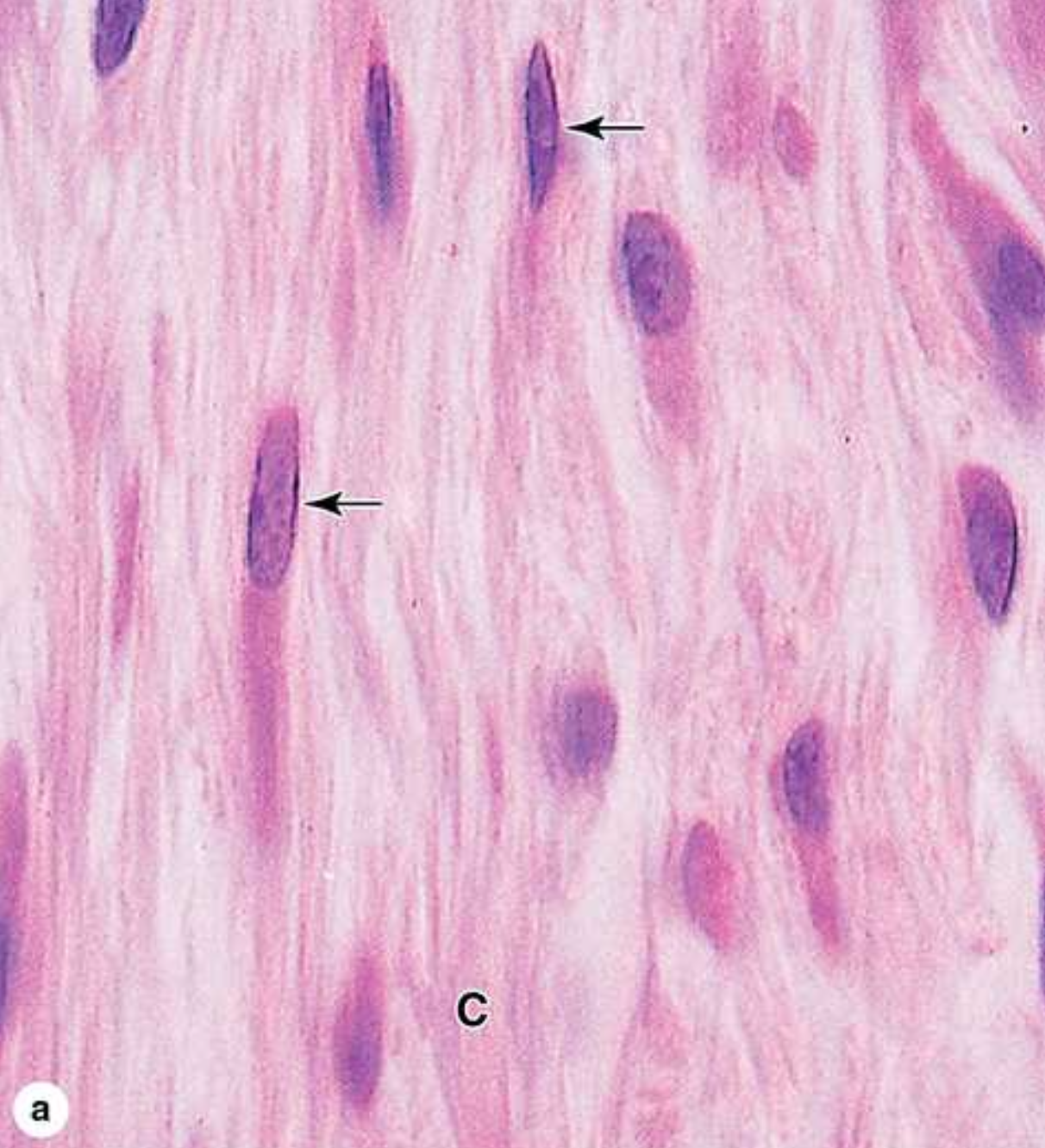
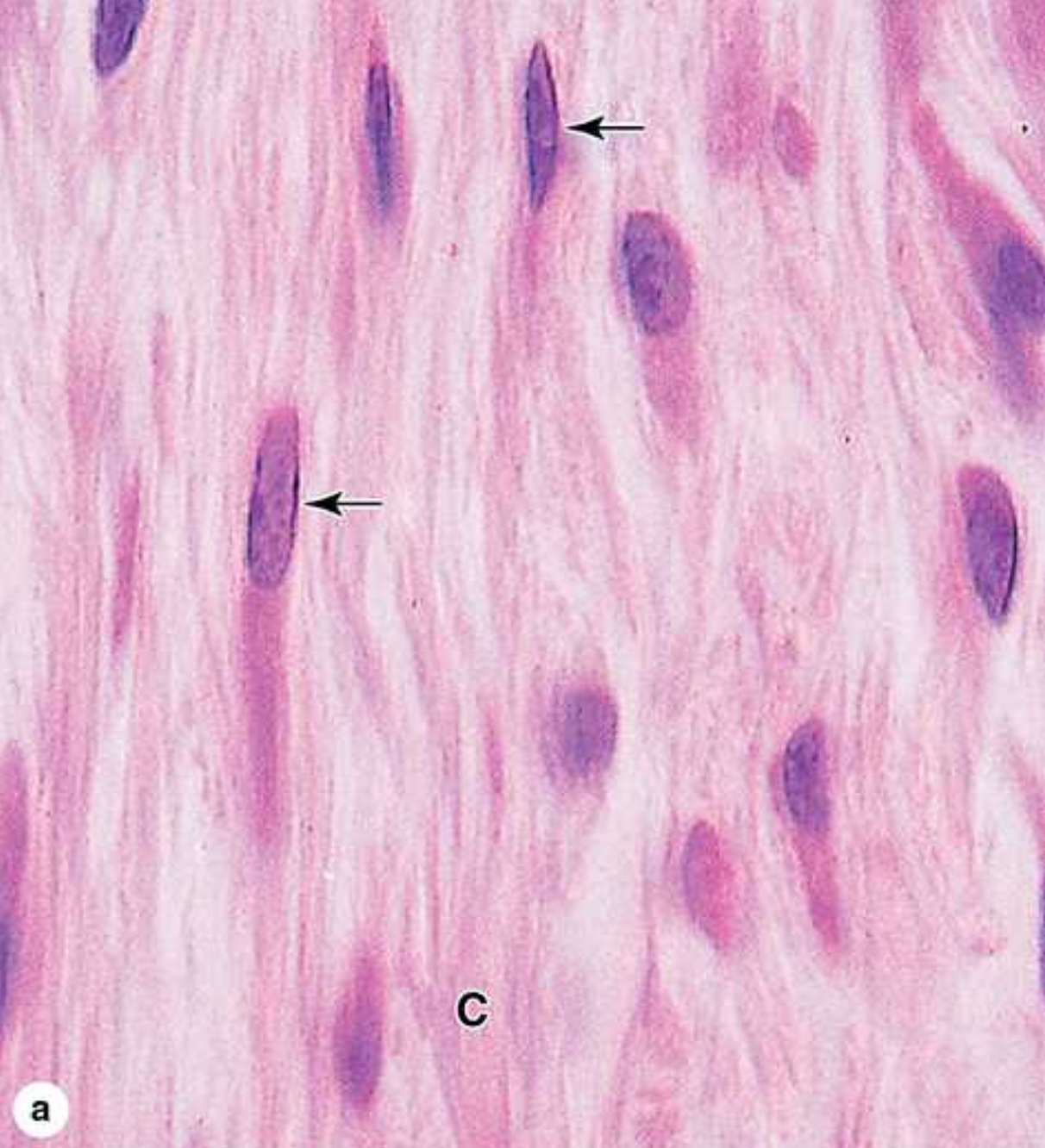
what is fibrocartilage?
in dense CT and mostly type 1 collagen
fibrocartilage has more/fewer chondrocytes
fewer
fibrocartilage is a mix of ____ and ____
fibres and hyaline cartilage (type 1, 2)
what is the main purpose of fibrocartilage?
shock absorber
what are the two forces that fibrocartilage withstands?
compression and shear force
examples of areas that have fibrocartilage
intervertebral discs, mandibles, pubic bone, sternum, knee
what happens at the epiphyseal growth plate?
chondrocytes undergo hypertrophy, die, become calcified, and osteoblasts lay down a new layer of bone, the plate is displaced away from the centre of the diaphysis and the length of the bone increases
the perichondrium
a sheath of dense connective tissue surrounding most cartilaginous structures, forms an interface between the cartilage and tissues supported by the cartilage, carries blood supply and some nerves
what is the structure of bone?
bone tissue + fat + hemopoietic tissue + blood vessels + nerves + hyaline cartilage
what does hemopoietic mean?
making blood
what is bone tissue made of?
calcified bone matrix or ECM and 3 bone cells
what are the two bone tissue layers?
compact cortical bone which is dense and spongey cancellous or trabecular bone
_blast
active and producing
_cyte
maintenance
_clast
breaking down
why is bone spongey?
to increase surface area to quickly add or remove calcium
what are the four functions of the bone?
mechanical support, protection, mineral homeostasis, and haematopoiesis
the function of cortical bone is
mechanical and protective
the function of trabecular bone is
metabolic
how do you make bone matrix?
collagen and ground substance are calcified
what is the major mineral?
calcium phosphate in the form of hydroxyapatite crystals
osteoblasts
secrete type 1 collagen and osteoid, promotes calcification by secreting alkaline phosphatase
what is osteoid?
initial unmineralized matrix
what shape is an active osteoblast?
cuboidal
osteocytes
trapped osteoblasts which occupy lacunae and make dendritic processes through canniculi and communicate with others, they secrete growth factors and stimulate other cells, live for ~10 years
osteoclasts
form giant multinucleated cells in contact with the surface of the bone and are differentiated from progenitor cells, more similar to macrophages (not true bone cells), they enhance Ca2+ release and break down old or damaged bone, they reside in resorption bays or Howship lacunae, produce a ruffled border while active
periosteum
surrounds bones, provides components for healing and repair, has 2 layers
what are the two layers of the periosteum?
outer layer is dense fibrous Ct, which is vascularized and innervated and the inner layer is the source of osteoprogenitor cells
how are collagen fibres of the periosteum arranged to the surface of the bone?
the ligaments and tendons enter the matrix at an angle (perforating or Sharpey's fibres)
what is the endosteum?
a single layer of osteoprogenitor cells and osteoblasts, small amount of CT, thinner than periosteum only one cell layer, the point of contact with the bone marrow > bone formation!
cartilage vs bone
cartilage contains chondrocytes embedded in the ECM and mostly type 2 collagen, while bone contains osteocytes and has a mineralized ECM and mostly type 1 collagen; both have perichondrium/osteum of two layers
at the microscopic level, what are the two types of bone?
primary/woven/immature and secondary/lamellar/mature
what is the woven bone?
the first to appear in development and fracture repair but the collagen fibres are disorganized and less mineralized
what is the lamellar bone?
replaces primary bone and is more organized (more communication between osteocytes) and has more perforating canals (increases blood vessels and contact with periosteum)
what is bone remodelling?
old osteons are resorbed by osteoclasts which form tunnel like cavities through old bone, those tunnels are invaded by osteoprogenitor cells and blood vessels which secrete new osteoid and form new lamellae; this traps osteocytes and eventually forms new osteon
what are the two mechanisms of osteogenesis?
endochondral and intramembranous bone
what is endochondral osteogenesis?
mesenchymal cells condense and form cartilaginous bone models which will be replaced by ossified tissue
what is intramembranous osteogenesis?
bone forms from condensed mesenchyme which differentiate into osteoblasts without a cartilage model (flat bones are formed this way)
where does the interchange of blood and bone calcium happen?
cancellous (compact) tissue
appositional growth
along the outer edge
interstitial growth
divides in existing areas
What is the ECM made out of?
The ___ contain different combinations of long protein fibers (collagen and elastic fibers) and ground substance, a complex of anionic hydrophilic proteoglycans, glycosaminoglycans (GAGs), and multiadhesive glycoproteins (laminin, fibronectin, and others).
What is mesenchyme?
a tissue developing mainly from the middle layer of the embryo, the ___derm. _______ consists largely of viscous ground substance with few collagen fibers.
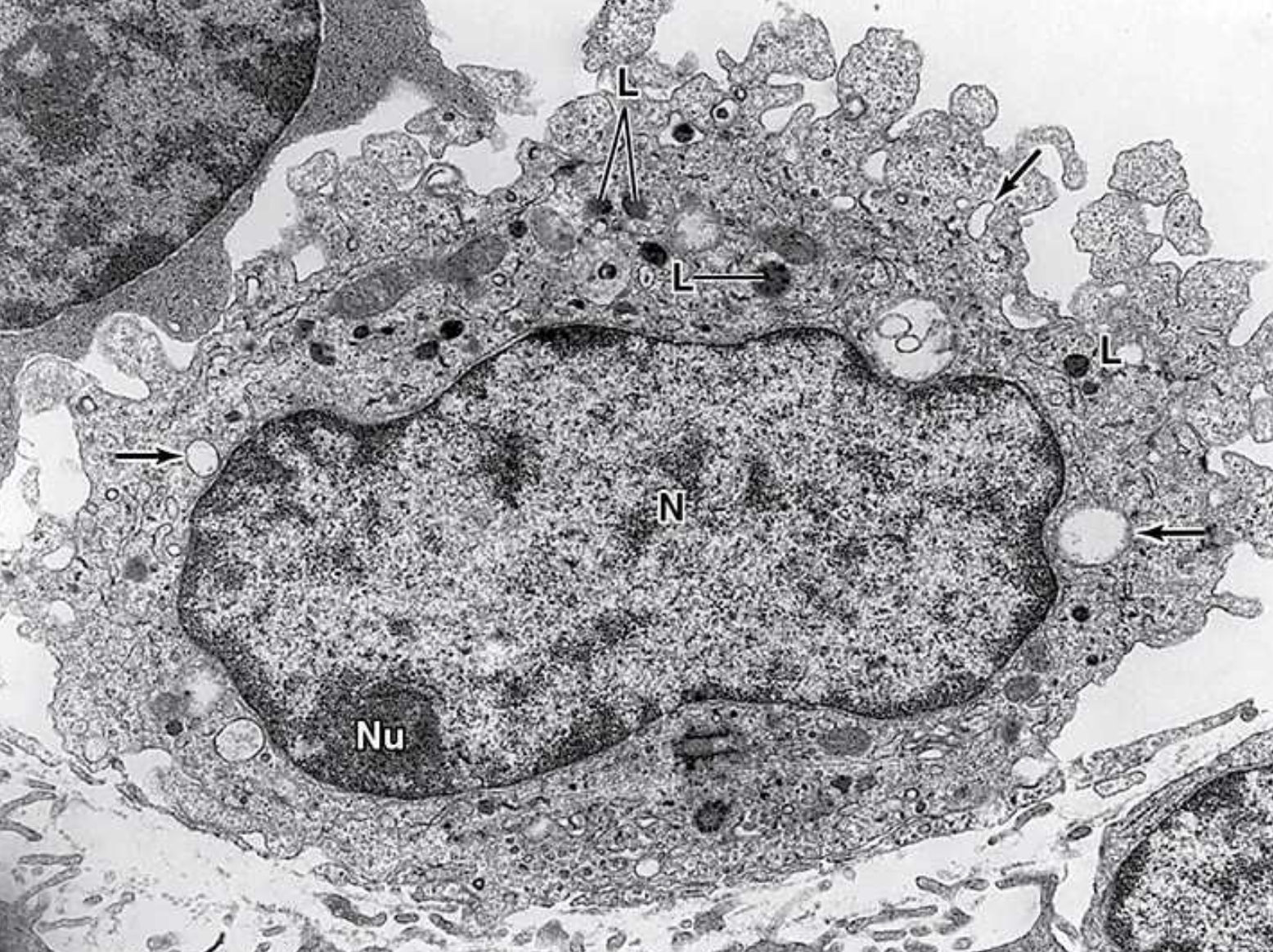
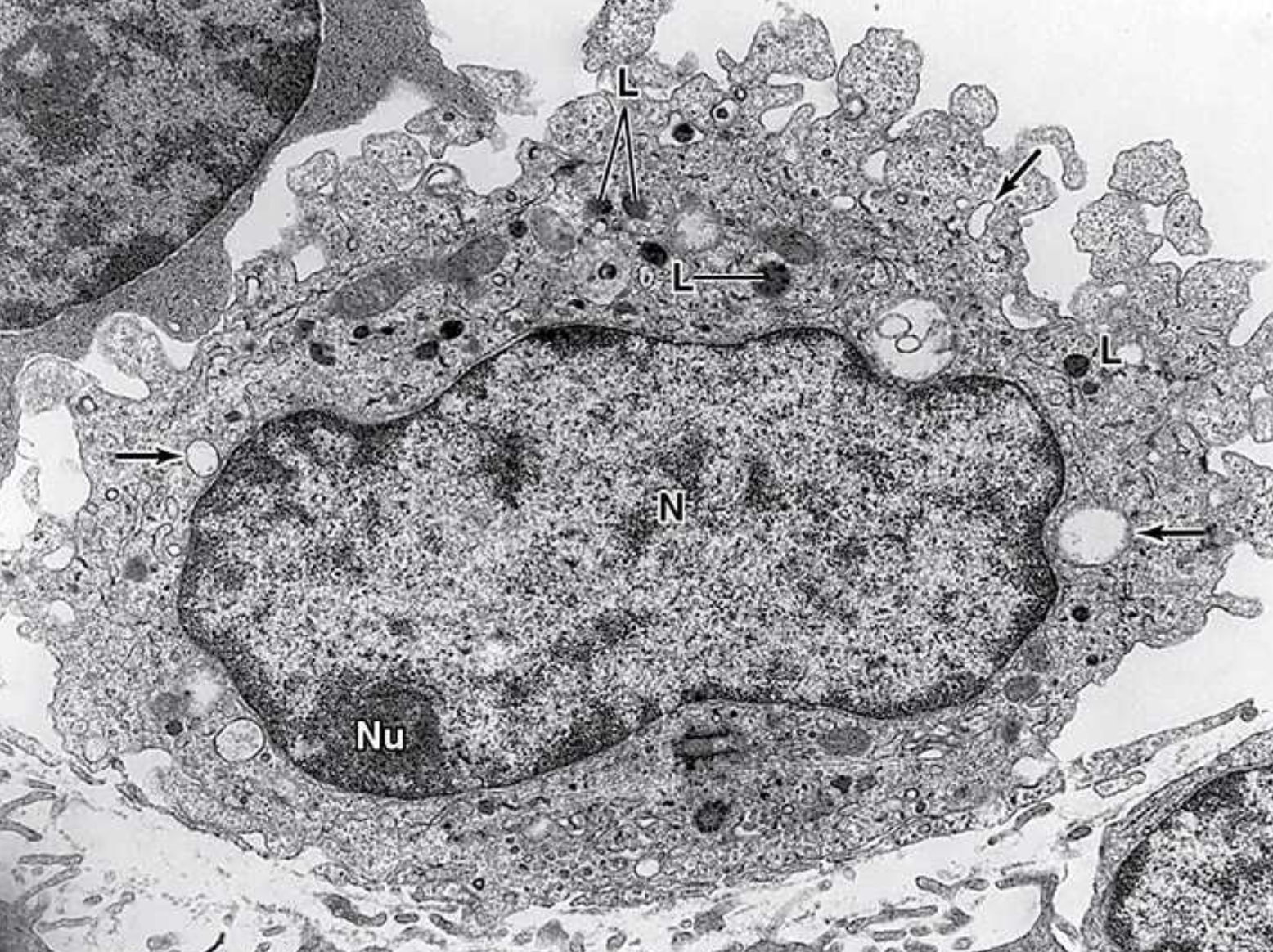
Mesenchymal cells have _____ nuclei with ____ chromatin and ____ nucleoli.
large, fine, prominent
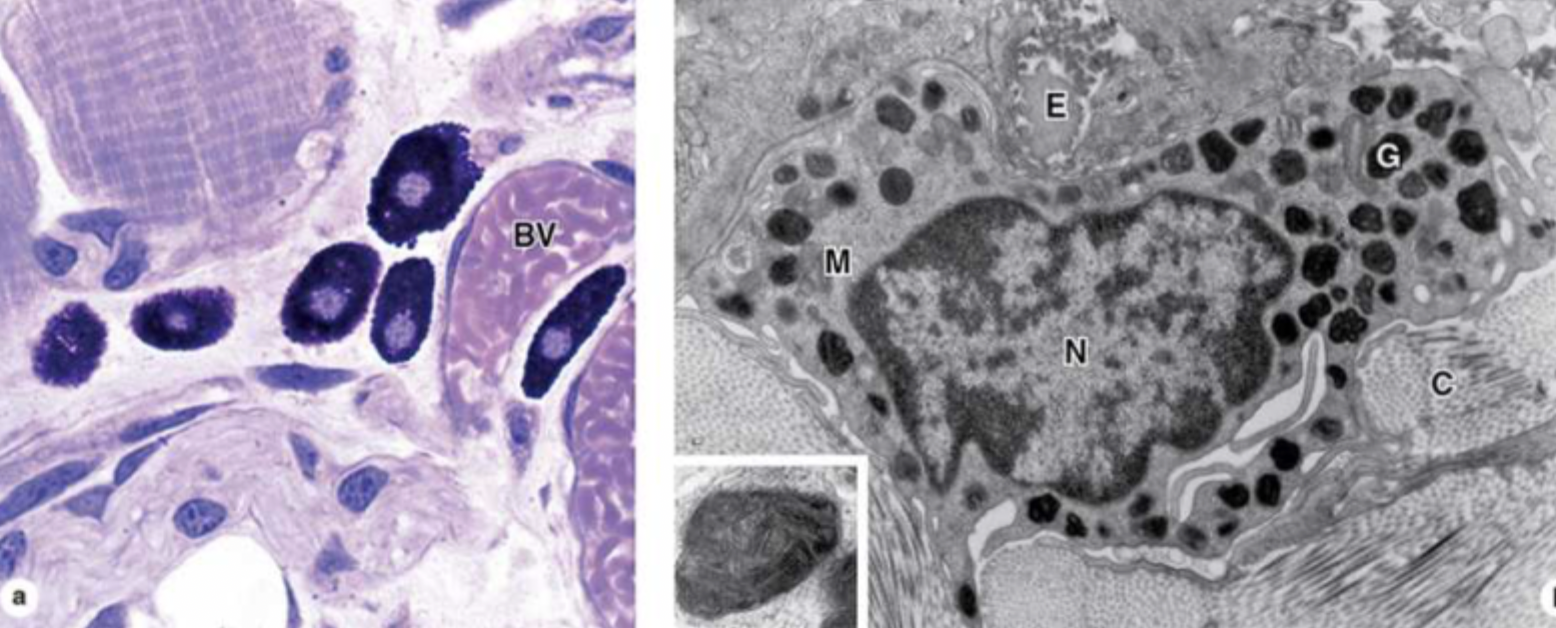
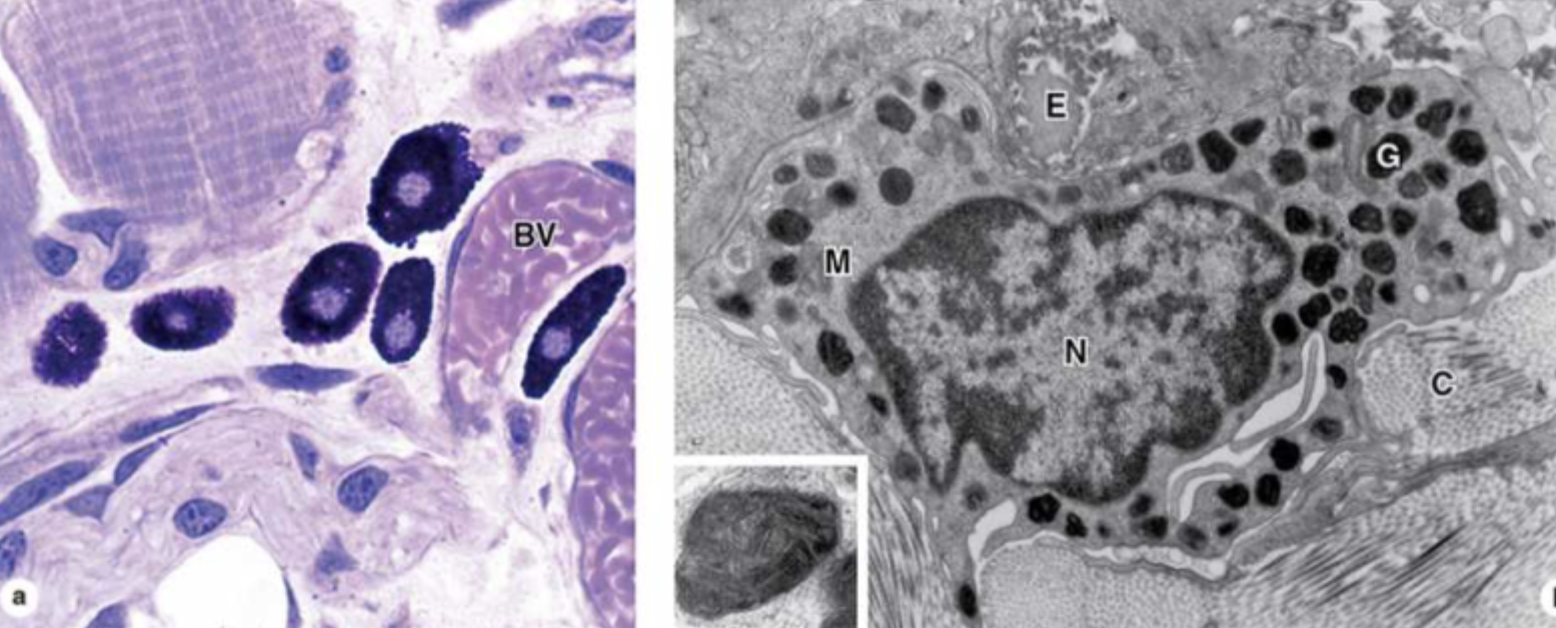
What are fibroblasts?
They are key cells in connective tissue proper.
What do fibroblasts do?
They synthesize and secrete collagen (the most abundant protein of the body) and elastin, which both form large fibers, as well as the GAGs, proteoglycans, and multiadhesive glycoproteins comprising the ground substance.
What do plasma cells do?
They make antibodies- y-shaped proteins that target antigens (toxins or bacteria).
What do eosinophilic leukocytes do?
They modulate allergic/vasoactive reactions and defend against parasites.
What do neutrophilic leukocytes do?
Phagocytosis of bactera.
What do macrophages do?
Phagocytosis of ECM debris, antigen presentation and processing, secretion of growth facotrs, cytokines (chemical messengers made of proteins), etc.
What do mast cells and basophilic leukocytes do?
They make pharmacologically active molecules like histamines.
What do adipocytes do?
They store neutral fats.
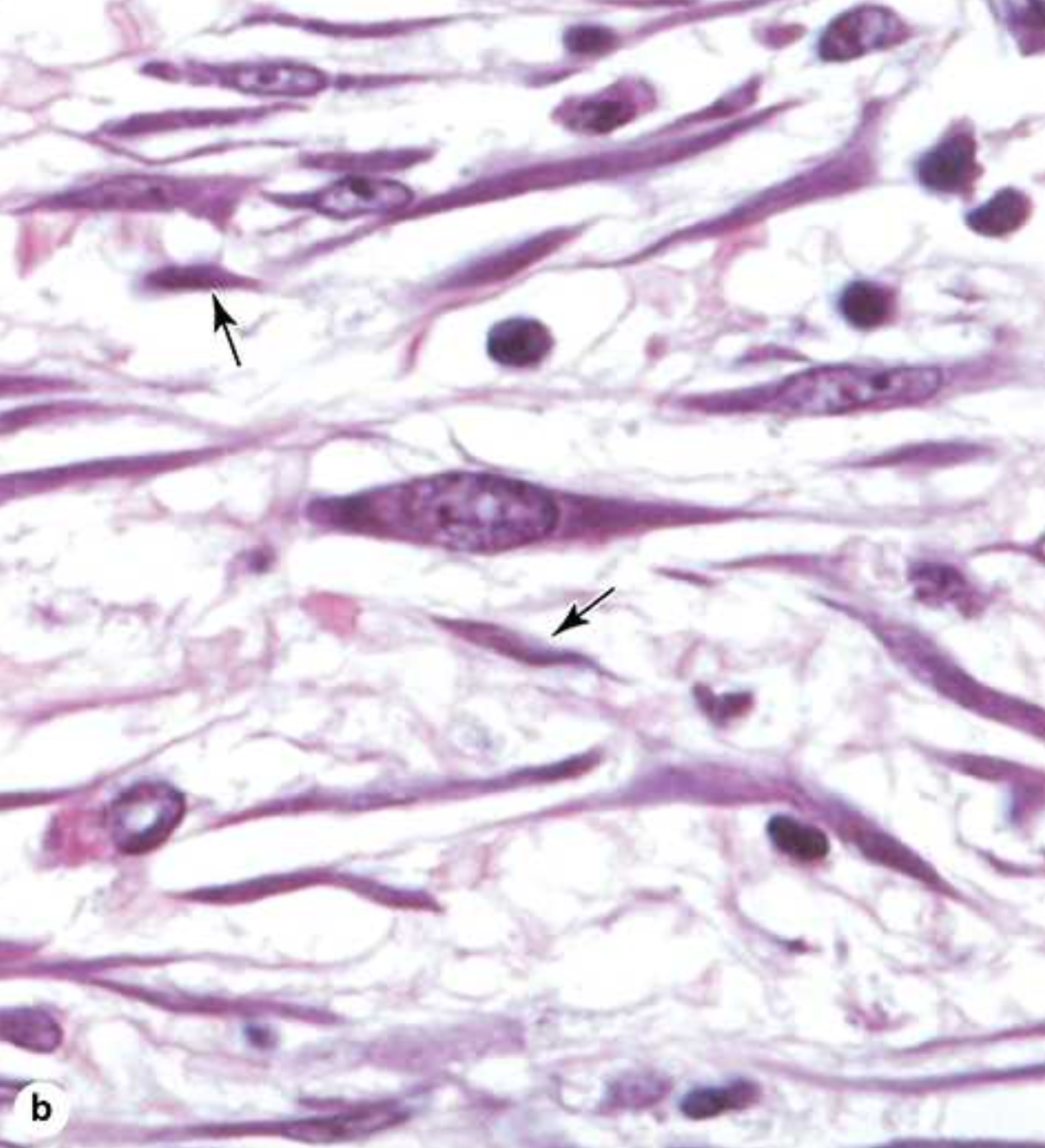
What is the difference between fibroblasts and fibrocytes?
Fibroblasts are highly active with high metabolic activity while fibrocytes are relatively inactive and “mature”.
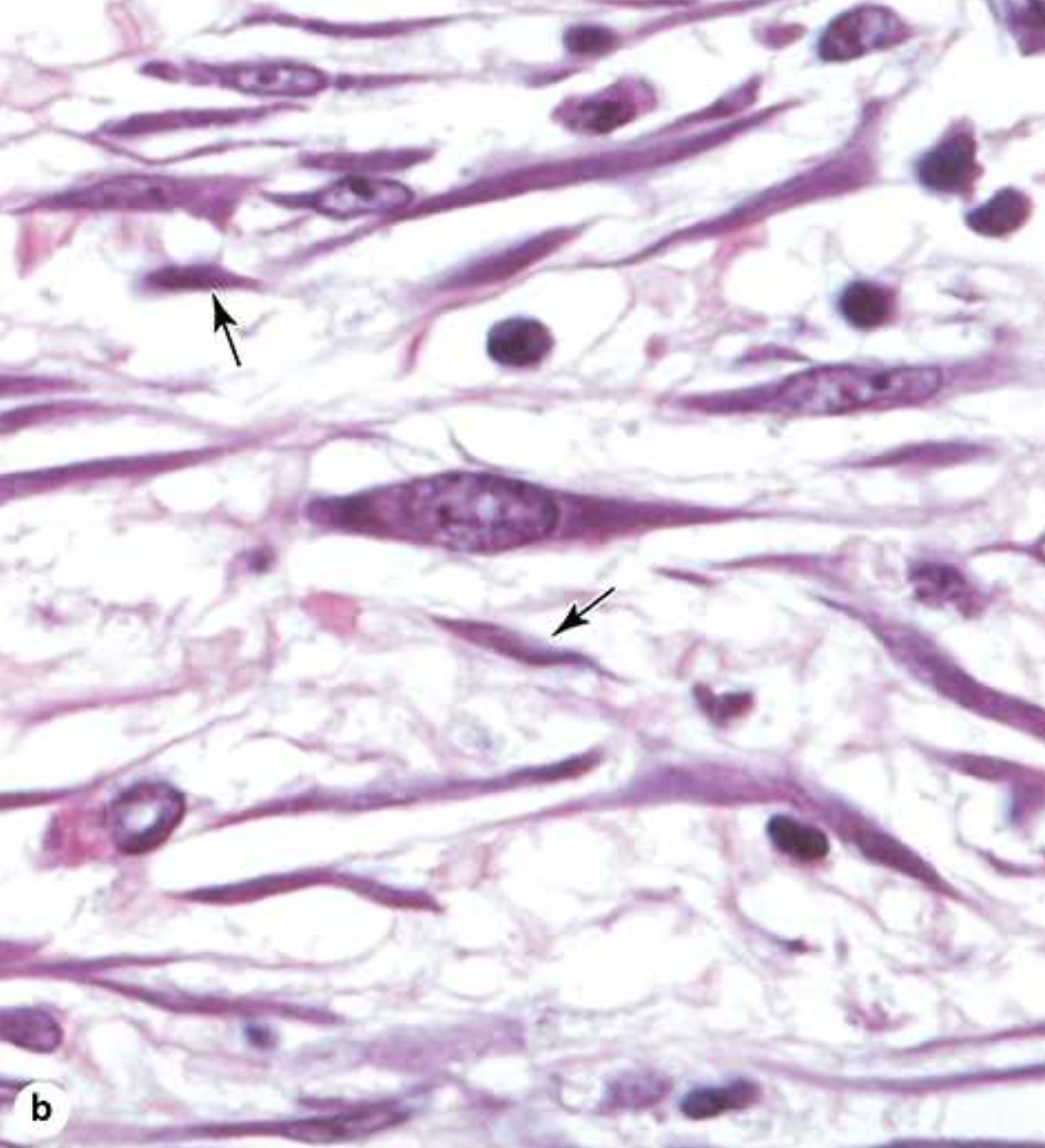
Active fibroblasts have more _____ and irregularly _____ cytoplasm. They have ____ rough endoplasmic reticulum and a ___-_______ golgi apparatus.
abundant, branched, much, well-developed.
What are growth factors?
They are a family of proteins which influence cell-growth and differentiation.
Myofibroblasts are involved in ___ ________. They have a form of ____ found in smooth muscle cells.
wound healing, actin
What is the purpose of adipose tissue?
It serves to cushion and insulate the skin and other organs. Made of cells specialized to store lipid as neutral fats or less commonly, to produce heat